Abstract
While chemokines are clearly important in the generation of protective immunity, the role of individual chemokines in the control of bacterial infection is still poorly understood. In this study, we investigated the role of macrophage inflammatory protein (MIP)-3α/CCL20, a chemokine that attracts activated T and B lymphocytes and immature dendritic cells, in host responses to bacterial infection. CCL20 production was induced in subcutaneous tissue in the BALB/c mouse in response to Salmonella enteritidis, Staphylococcus aureus and zymosan, with S. enteritidis being the most potent. S. enteritidis induced CCL20 production in the spleen following either oral administration or injection into the peritoneal cavity. In contrast, no increase was observed in the Peyer's patches. In this model, following intraperitoneal injection, dose-dependent colonization of the spleen and Peyer's patches by S. enteritidis, expression of IFNγ and IL-4, and production of antibodies against the S. enteritidis surface antigen SefA were observed. Prior treatment with neutralizing antibodies against CCL20 enhanced bacterial dissemination to the spleen and Peyer's patches and strongly biased the IFNγ/IL-4 ratio towards a type 2 profile in the spleen, while the humoral response was unaffected. In contrast, treatment with neutralizing anti-MIP-1α/CCL3 antibodies enhanced the bacterial burden in the Peyer's patches but not in the spleen, had no significant effect on the cytokine ratio, but significantly inhibited anti-SefA production. Together, these results demonstrate an important role for CCL20 in the control of bacterial infection and more specifically in the regulation of cell-mediated immunity against intracellular bacteria such as S. enteritidis.
Similar content being viewed by others
Main
Infection by pathogenic bacteria triggers a cascade of events aimed at clearing the pathogen. This not only includes activation of elements of the innate immune system, but also the migration of antigen-presenting cells from the tissue to local draining lymph nodes where clonal selection of lymphocytes may occur, followed by the subsequent migration of antigen-specific lymphocytes towards the site of infection. The chemokines, a family of chemotactic cytokines, play an early and pivotal role in these processes via their ability to direct migration of various effector cells of the immune system.1 They are classified based on their functional expression as homeostatic/constitutive or inflammatory/inducible. Homeostatic chemokines are expressed constitutively within lymphoid tissues and appear to be responsible for movement of thymocytes through the thymus during selection2, 3, 4 and for the physiological trafficking of cells including lymphocytes and dendritic cells (DC) into secondary lymphoid organs, under normal conditions or during immune responses. On the other hand, inflammatory chemokines are upregulated at sites of inflammation, and play a key role in the recruitment of effector leukocytes to peripheral tissues in response to immunological challenge.1, 5, 6, 7
MIP-3α/CCL20 is a CC chemokine that appears to display expression characteristics of both constitutive and inflammatory chemokines. For instance, messenger RNA (mRNA) for CCL20 has been found to be constitutively expressed at mucosal interfaces and in gastrointestinal lymphoid tissues, but its production can also be induced in several cell types including many types of leukocytes.8 In the context of the host response to bacterial infection, CCL20 is potentially important for several reasons. First, it has the capacity to attract activated and memory CD4+ and CD8+ T cells, B cells, and immature DC, at least in vitro.9, 10, 11, 12 Second, CCL20 mRNA is expressed at immunological barriers such as the gastrointestinal tract and the skin,13 and this expression is increased by inflammatory stimuli including bacterial lipopolysaccharide (LPS) or the proinflammatory cytokines tumor necrosis factor alpha (TNFα) or interleukin (IL-1).9, 14 Third, studies using mice in which CCR6, the only known receptor for CCL20, has been deleted by homologous recombination, display an absence of CD11c+ CD11b+ myeloid-derived DC in the Peyer's patches and an increase in CD4 and CD8 T-cell subpopulations within the mucosa in the small intestine. This is associated with an impaired ability to mount a humoral response against keyhole limpet hemocyanin (KLH) and rotavirus15 and alterations in cell-mediated immunity.16 Finally, an increased production of CCL20 was demonstrated in human intestinal xenografts in SCID mice infected with Salmonella dublin and Escherichia coli, and CCL20 mRNA was upregulated in gastrointestinal tissue in a murine model of Helicobacter pylori infection where it correlated with the influx of myeloid DC.17, 18
While the characteristics of its expression and its target cell spectrum suggest that CCL20 is likely to play an important role in the adaptive immune response to bacterial infection, unequivocal data supporting this notion have yet to be obtained. The role of various cellular and molecular components of the immune system have been examined in the mouse using a range of bacteria including species of Salmonella, an example of which is S. enteritidis. During S. enteritidis infection, bacteria ingested with contaminated food or water enter the membranous epithelial cells (M cells) within the Peyer's patches. The bacteria can then be transported by macrophages to other tissues such as regional lymph nodes, spleen and liver, and will multiply in all these target organs as well as within the Peyer's patches. In this study, we have therefore investigated CCL20 production at sites of infection in vivo and then used S. enteritidis infection in the mouse to investigate the role of CCL20 in the control of bacterial dissemination to secondary lymphoid target organs such as the spleen and Peyer's patches. We also evaluated the role of CCL20 in the activation of the two arms of the adaptive immune response by monitoring antigen-specific humoral immunity and the production of the type 1 cytokine interferon-γ (IFNγ) and type 2 cytokine IL-4 in target organs as an indication of the cell-mediated immune response. In addition, the role of CCL20 was compared with that of the closely related but better characterized CC chemokine macrophage inflammatory protein (MIP)-1α/CCL3.
Materials and methods
Animals
Female BALB/c mice, 6–8 weeks old, were obtained from the Central Animal House at the University of Adelaide, South Australia. Animals were housed in conventional mouse rooms at Adelaide University where they were provided with food and water ad libitum. Animals were handled according to the guidelines of the University of Adelaide Animal Ethics Committee.
Reagents
The anti-CCL20 and anti-CCL3 antibodies (Abs) used in this study were protein-A-purified from polyclonal antisera raised in rabbits against full-length synthetic murine CCL20 and murine CCL3 respectively.19, 20, 21 S. enteritidis strain 11RX and Staphylococcus aureus22 were obtained from stocks within the School of Molecular and Biomedical Science at the University of Adelaide. Zymosan was obtained from the Sigma Chemical Co. (St Louis, MO, USA). SefA protein was purified from S. enteritidis strain 11RX as previously described.23
Formation of Subcutaneous Air Pouches
Air pouches were raised on the dorsum of BALB/c mice by subcutaneous injection of 2.5 ml of sterile air as previously described.20, 21 Agonists were introduced into the air pouch in a 1 ml volume of sterile PBS, and exudates collected after 2 h. Exudates were centrifuged at 100 g for 10 min and the supernatants were retained for ELISA.
Gavage of Mice with S. enteritidis
BALB/c mice were given 2 × 109 colony forming units (cfu) S. enteritidis 11RX in endotoxin-free PBS by the oral route. The Peyer's patches and spleen were surgically removed, washed, and immediately homogenized on day 5 after gavage. The homogenates were passed through a cell dissociation sieve (Sigma, St Louis, MO, USA), centrifuged for 5 min at 3000 rpm, and supernatants were retained and adjusted to a final volume of 1 ml with PBS for detection of CCL20 and CCL3 by ELISA.
S. enteritidis Infection in the Peritoneal Cavity
A range of S. enteritidis 11RX doses (104, 3 × 104, 105 and 3 × 105 cfu) or diluent (endotoxin-free PBS) was injected into the peritoneal cavity of BALB/c mice as previously described.22 On day 5 after infection, spleens were collected from the animals and processed as described above for CCL20 and CCL3 ELISA. For each animal, 4–5 Peyer's patches were also collected and processed as described above. In the experiments involving anti-chemokine antibody treatment, 500 μg of rabbit polyclonal anti-mouse CCL20, anti-mouse CCL3, or normal rabbit immunoglobulin G (IgG) control were injected intraperitoneally 24 h prior to bacterial infection with a dose of 3 × 105 cfu S. enteritidis.
Viable Bacterial Counts
Serial dilutions of the homogenates from the spleen and Peyer's patches were performed in Luria Broth (LB) media, and assayed for colony forming units on LB solid agar from growth at 37°C overnight.
Enzyme-Linked Immunosorbent Assay
Murine CCL20 and CCL3 ELISAs were conducted as previously described.19, 21 Briefly, for CCL20, Costar high-binding 96-well trays (Corning, Corning, NY, USA) were coated with 100 μl of polyclonal capture Ab, diluted in 0.1 M NaHCO3. Plates were incubated at 4°C overnight, then washed with phosphate-buffered saline (PBS)/Tween and blocked with PBS/3% BSA for 2 h. The plates were washed again before standards and samples were added and incubated for 90 min. The plates were washed again and incubated with biotin-conjugated anti-CCL20 diluted in PBS/1% BSA for 45 min, then washed prior to adding streptavidin-peroxidase conjugate (Rockland, Gilbertsville, PA, USA) and Fast OPD substrate (Sigma) according to the manufacturer's recommendations. Murine IFNγ and IL-4 enzyme-linked immunosorbent assays (ELISAs) were performed using matched-pair antibodies obtained from Pharmingen (Becton Dickinson, Franklin Lakes, NJ, USA) and streptavidin-peroxidase conjugate (Rockland) and Fast OPD substrate (Sigma) according to the manufacturer's recommendations. It should be noted that while the values presented for the spleens correspond to whole organs, the values for Peyer's patches have been normalized to the quantity of tissue retrieved during microdissection. On average, this corresponded to 16.3±4 mg (ie 4–5 Peyer's patches/animal). Detection of anti-SefA antibody in sera was performed using a direct ELISA protocol. Sera were collected at day 5 after infection and stored at −20°C until analyzed. Briefly, Costar (Corning, Corning, NY, USA) high-binding 96-well trays were coated overnight at 4°C with 3 μg/ml purified S. enteritidis SefA and blocked with PBS containing 1% BSA 5% sucrose for 2 h. Dilutions of the samples in PBS containing 0.1% BSA were incubated for 2 h. Peroxidase-conjugated goat anti-mouse IgM (Rockland), goat anti-mouse IgA (Zymed, San Francisco, CA, USA), rabbit anti-mouse IgG1 or rabbit anti-mouse IgG2a (Zymed) antibody was then added (Rockland) for 2 h and the reaction was developed using Fast OPD substrate (Sigma). For each isotype, the mean optical density value for naïve noninfected mouse serum (n=3) was substracted to each individual data obtained.
Statistical Analysis
Statistical analysis was performed using the Student t-test for all experiments, except for bacterial burden evaluation where the nonparametric Mann–Whitney U-test was used. The level of statistical significance attained is indicated in the figure legends.
Results
Expression of CCL20 at Different Sites In Vivo in Response to Microbial Challenge
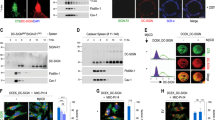
To determine the levels of CCL20 produced in vivo during infection, a specific sandwich ELISA was developed (Materials and methods). Production of CCL20 was initially examined in the skin using the acute subcutaneous air pouch model. Little or no CCL20 was detected in control air pouches; however, injection of either the Gram-negative bacterium S. enteritidis, the Gram-positive bacterium S. aureus, or the yeast cell wall component zymosan, into the air pouch for 2 h led to the accumulation of CCL20. This effect was dose-dependent (Figure 1a) and time-dependent, with maximal accumulation occurring at 2 h poststimulation. In response to S. enteritidis, CCL20 was first detected at low level 30 min after injection, was almost maximal by 1 h, and had decreased by 24 h postinjection (data not shown). Production of the closely related chemokine CCL3 followed a similar pattern, although CCL3 production was induced more effectively at lower doses of the bacteria and no clear dose-response to zymosan was observed.
Production of CCL20 and CCL3 in vivo in response to microbial stimulation. Production of CCL20 and CCL3 was measured by sandwich ELISA (a) in subcutaneous air pouch exudates collected 2 h after injection of either PBS, or the indicated doses of S. enteritidis, S. aureus, or zymosan; (b) in homogenates of the spleen and Peyer's patches either before exposure (day 0) or 5 days following oral gavage with 2 × 109 cfu S. enteritidis; (c) in peritoneal cavity exudates, or homogenates of the spleen or Peyer's patches either before exposure (day 0) or 5 days following peritoneal injection of with 3 × 105 cfu S. enteritidis. Data represent mean±s.e.m. from at least six mice. Significantly different from PBS control or day 0 value at *P<0.05 Student's t-test.
Based on its more potent stimulatory activity, further experimentation was conducted on S. enteritidis to observe CCL20 production in the gut and spleen during systemic infection. Mice received S. enteritidis either orally or via intraperitoneal (i.p.) injection and the level of CCL20 was determined in the spleen, the Peyer's patches and in the peritoneal cavity (the latter only following i.p. injection of S. enteritidis). CCL20 production was induced approximately three-fold over control levels in the spleen following oral feeding with S. enteritidis (Figure 1b). However, there was no alteration in the level of CCL20 observed in the Peyer's patches. This contrasted somewhat to production of CCL3, which while being induced in the spleen, was also induced in the Peyer's patches.
CCL20 expression followed a similar pattern in the spleen and Peyer's patches following i.p. administration of S. enteritidis, and was also elevated in the peritoneal cavity (Figure 1c). As observed above with respect to oral administration, CCL3 production following i.p. administration of S. enteritidis was elevated in both the spleen and Peyer's patches, and like CCL20, was also increased in the peritoneal cavity. It is interesting to note that the production of CCL20 and CCL3 in the spleen of infected animals at day 5 followed a dose-response pattern, with higher chemokine concentrations measured in response to higher bacterial doses injected into the peritoneal cavity. This pattern was also found in the Peyer's patches for CCL3, but no alteration in the level of CCL20 was observed compared to noninfected controls for any of the bacterial doses injected (ranging form 104 cfu to 3 × 105 cfu) (data not shown).
Bacterial Dissemination in the Spleen and Peyer's Patches
Upon completion of the experiments outlined above, the role of CCL20 in the host response to bacteria was explored further. To achieve this, the host response following i.p. injection of S. enteritidis was characterized. This route of administration was chosen because the systemic pattern of CCL20 production was similar to that observed following oral administration but i.p. administration led to more reproducible results (data not shown). A range of bacterial doses was injected into the peritoneal cavity and survival and dissemination of the bacteria to the spleen and Peyer's patches, two major target organs, was monitored. All infected animals displayed splenomegaly that followed a dose–response pattern—the higher the infective dose, the greater the weight of the spleen (data not shown). Bacterial burden at day 5 in spleen (Figure 2a) and Peyer's patches (Figure 2b) followed a clear dose-dependent pattern with the greatest bacterial burden being observed following infection with 3 × 105 cfu, the highest dose of bacteria used. Doses higher than this were found to be lethal when administrated via intraperitoneal injection.
Recovery of S. enteritidis from the spleen and Peyer's patches following infection. Mice were inoculated by intraperitoneal injection with the indicated infectious doses of S. enteritidis and the number of colony-forming units recovered from (a) the spleen and (b) the Peyer's patches was determined 5 days later. Data are plotted as values from individual mice. The bars represent the median value.
Cell-Mediated and Humoral Responses to Infection with S. enteritidis
The effect of infection of mice with S. enteritidis on two key parameters of the adaptive immune response, IFNγ and specific antibody production, were monitored at day 5 post i.p. injection. As shown in Figure 3a, bacterial infection strongly induced production of IFNγ in the spleen. Of note, the highest bacterial doses (105 and 3 × 105 cfu) resulted in a comparatively more moderate increase compared with the smallest dose (104 cfu). In contrast, the levels of IFNγ in the Peyer's patches of infected animals showed no significant variation compared to the noninfected control group (Figure 3b).
The cell-mediated and humoral immune responses to S. enteritidis infection. Mice were inoculated by intraperitoneal injection with the indicated infectious doses of S. enteritidis and the level of IFNγ was measured in homogenates of (a) the spleen and (b) the Peyer's patches at day 5 postinfection. Control=PBS-injected animals. In parallel, the effect of increasing doses of bacteria on the level of serum antibody against the bacterial surface antigen SefA was assessed at day 5 after infection (c). Data represent mean±s.e.m. from at least seven mice. ns, not significant. Significantly different from control value at ***P<0.0001 Student's t-test.
In parallel, the sera of the animals were assessed by direct ELISA for S. enteritidis-specific antibody production at day 5. As shown in Figure 3c, infection with S. enteritidis led to a dose-dependent increase in anti-SefA (SefA is the major surface antigen of S. enteritidis 11RX) antibodies in the serum. While the level of anti-SefA antibodies in the 104 cfu-infected group was close to the lower limit of detection, this level increased with increasing bacterial dose, and the 3 × 105 cfu-infected group displayed a strong specific antibody titre.
CCL20 Regulates Bacterial Burden
The role of CCL20 in control of bacterial burden in both the spleen and Peyer's patches was investigated using a specific, neutralizing polyclonal rabbit antibody previously developed in our laboratory.19 In these experiments, we also examined the effect of neutralization of CCL3 for comparison. Mice were treated with the neutralizing antibodies or a control normal rabbit IgG (NRIgG) prior to bacterial infection and bacterial burden in the target organs was monitored. Prior treatment with either anti-CCL20 or anti-CCL3 antibodies had no effect on the splenomegaly in response to infection with 3 × 105 cfu S. enteritidis (data not shown). However, neutralization of CCL20 led to a significant increase in the number of bacteria in both the spleen and the Peyer's patches (Figure 4a). Neutralization of CCL3 failed to alter the bacterial burden in the spleen, but led to a significant increase in the number of bacteria recovered from the Peyer's patches (Figure 4b). Of note, at day 5 postinfection, neither anti-CCL20 nor anti-CCL3 treatment altered the level of CCL20 or CCL3 measured in the spleen or Peyer's patches, compared with control mice treated with NRIgG (data not shown).
CCL20 and CCL3 regulate bacterial burden in the spleen and Peyer's patches. Mice were pretreated with 500 μg of Protein A-purified Normal Rabbit (NR) IgG, anti-CCL20 or anti-CCL3 the evening prior to intraperitoneal injection of 3 × 105 cfu of S. enteritidis. The number of cfu recovered from (a) the spleen and (b) the Peyer's patches was determined 5 days later. Data are plotted as values from individual mice (n=10–12 for spleen, n=7–9 for Peyer's patches) from two independent experiments. The bars represent the median value. Significantly different from NRIgG values at *P<0.05 Mann–Whitney U-test.
CCL20 and CCL3 are Involved in the Adaptive Immune Response to S. enteritidis
To characterize the potential role of CCL20 and CCL3 in the development of the adaptive immune response against S. enteritidis, the effect of prior treatment with neutralizing antibodies on IFNγ production in target organs was determined. Mice were treated 1 day prior to bacterial infection with either a neutralizing anti-CCL20 or anti-CCL3 antibody, or with nonspecific normal rabbit IgG (NRIgG). A strong increase in IFNγ production in the spleen as compared with uninfected controls was observed in animals treated with NRIgG (Figure 5a). Treatment with anti-CCL20 antibody significantly reduced the level of IFNγ production in the spleen compared with the NRIgG-treated group. This result is in contrast with the anti-CCL3-treated group, which showed no difference in the level of IFNγ produced in the spleen compared with the NRIgG group. In parallel, expression of IL-4 in the spleen was evaluated. As shown in Table 1, anti-CCL20 treatment induced a strong increase in IL-4 production. Anti-CCL3 treatment had a milder and nonstatistically significant effect (data not shown). As a result of both decreased IFNγ and increased IL-4 production in the spleen, the resulting IFNγ/IL-4 ratio was dramatically decreased in anti-CCL20-treated animals (Table 1). In the Peyer's patches (Figure 5b), all infected animals exhibited a small and statistically nonsignificant increase in IFNγ expression, and there was no difference between the NRIgG-treated group and the anti-CCL20- or anti-CCL3-treated groups in this respect.
CCL20 regulates the cell-mediated immune response to bacterial infection. Mice were pretreated with 500 μg of Protein A-purified NRIgG, anti-CCL20 or anti-CCL3 the evening prior to intraperitoneal injection of 3 × 105 cfu of S. enteritidis. After 5 days, the level of IFNγ in homogenates of (a) the spleen and (b) the Peyer's patches was determined. Control=PBS-injected mice. Data represent the mean±s.e.m. (n=10–12) from two independent experiments. Significantly different from control values at **P<0.01 Student's t-test.
Finally, the potential involvement of CCL20 and CCL3 in regulation of the humoral immune response to bacterial infection was evaluated. The level of specific anti-SefA antibodies in the sera of the animals treated with neutralizing antichemokine antibodies was therefore assessed. Infected animals treated with the control NRIgG displayed a strong anti-SefA IgM response (Figure 6). Treatment with the anti-CCL20 antibody did not have any effect on the level of anti-SefA generated. However, treatment with the anti-CCL3 antibody induced a significant decrease in anti-SefA IgM titres compared to the NRIgG-treated control. In contrast, no statistically significant difference was detected for the other antibody isotypes analyzed (Figure 6).
CCL3 regulates the humoral immune response to bacterial infection. Mice were pretreated with 500 μg of Protein A-purified NRIgG, anti-CCL20 or anti-CCL3 the evening prior to intraperitoneal injection of 3 × 105 cfu of S. enteritidis. After 5 days, sera were collected and the level of SefA-specific Ig isotypes was determined. The bars represent the median value (n=6–8) from two independent experiments. Student's t-test value significant for IgM between NRIgG-treated group and anti-CCL3-treated group (at **P<0.01). P>0.05 for the remainder.
Discussion
In this study, we provide several novel pieces of information regarding the biological role of the CC chemokine CCL20. We provide the first in vivo quantitation of CCL20 protein levels expressed during both innate and adaptive immune responses to bacteria, and we demonstrate an important role for this chemokine in cell-mediated immunity against the Gram-negative, intracellular bacterium S. enteritidis. These in vivo data pave the way for further investigations into the biological role of this chemokine, particularly in antibacterial responses.
Chemokines were originally classified into four subfamilies based on the arrangement of a signature cysteine motif present in their predicted primary amino-acid structure.1, 5 However, with the discovery that the superfamily comprises more than 40 members, and the fact that the structural classification did not provide any indication of the functional role of the various chemokines, an alternative system that relates expression to function was introduced.4 In this context, the homeostatic/constitutive chemokines (such as SDF-1/CXCL12 or ELC/CCL19 and SLC/CCL21) are involved in the homeostatic function of the immune system, regulating lymphocyte movement in primary and secondary lymphoid organs, and the inflammatory/inducible chemokines (such as CXCL9-11, CCL3, RANTES/CCL5 or MCP-1/CCL2 among many others) are involved in recruitment of effector cells to peripheral tissues.4
Our data, quantifying the levels of CCL20 protein generated at different sites in the body following immune response induction, clearly indicate that CCL20 spans both the homeostatic and inflammatory classes: CCL20 was induced in subcutaneous tissue, the peritoneal cavity and the spleen in response to microbial challenge. However, it was constitutively expressed in the spleen and the Peyer's patches, but was not induced in the Peyer's patches. These observations are supported by previous data indicating constitutive expression of CCL20 mRNA at mucosal surfaces and in the Peyer's patches15 and detection of CCL20 protein in inflammatory pathologies such as psoriasis and rheumatoid arthritis.24, 25, 26 While the source of CCL20 was not formally identified in this study, it is likely to be produced by epithelial cells and/or resident or infiltrating granulocytes such as neutrophil, as these cells have previously been shown to produce CCL20. The inducible nature of CCL20 expression is further supported by data obtained at the mRNA level, showing an increase in CCL20 transcripts in vitro and in vivo after exposure to LPS.9, 27, 28 This combined constitutive/inducible profile is relatively unique among the chemokines, which, in turn, suggests a unique role for CCL20 in immune surveillance15 and inflammation, as indicated by its upregulation in response to LPS.29, 30 and during infection (the present study).
CCL20 binds with high affinity to only one known receptor, CCR6. Moreover, CCL20 is the only known chemokine ligand for CCR6. This is also relatively unique among members of the chemokine gene superfamily, where most ligands bind to multiple receptors, and most receptors have multiple ligands. Two separate groups have generated muCCR6 knockout mice by gene targeting in order to study the biological role of this molecule in vivo.15, 16 These mice exhibit defective humoral immunity and cell-mediated immunity following challenge. However, the immune system of CCR6−/− mice exhibits a developmental defect in the Peyer's patches where myeloid-derived DC and lymphocyte subsets are abnormal. These primary defects make it difficult to interpret the precise role of CCL20 and CCR6 in inflammatory responses during infection, particularly those involving the gastrointestinal tract or mucosal surfaces. Therefore, while studies in the CCR6−/− mouse demonstrate the effect of genetic deficiency on immune responses mediated by this receptor/ligand interaction, they do not indicate the effects of blocking responses in a normal, fully developed immune system, unlike the specific neutralizing antibodies used in this study. Furthermore, while CCL20 is the only known chemokine ligand for CCR6, it is not the only ligand. Recent studies indicate that β-defensins also interact with CCR6.31, 32 Because such an interaction is likely to play a role in immunity against bacteria, the use of neutralizing antibodies against CCL20 rather than CCR6-deficient mice is the most direct way of specifically examining the role of CCL20 in models of bacterial infection.
In this study, treatment of mice with neutralizing anti-CCL20 antibodies prior to primary infection resulted in recovery of enhanced levels of the bacteria in the spleen and the Peyer's patches, indicating an important role for endogenous CCL20 in the immune response against S. enteritidis. Previous investigations with this bacterium indicate that both cell-mediated and humoral immunity is required for mice to clear this infection.33 Neutralization of CCL20 had no influence on production of anti-SefA (the major surface antigen on S. enteritidis) antibodies; however it significantly reduced IFNγ levels in the spleen. To our knowledge, this is the first demonstration of a role of CCL20 in IFNγ production during the immune response, although other chemokines have been implicated in the regulation of IFNγ production. For instance, the level IFNγ in the serum, and of IFNγ mRNA in the liver in an hepatic granuloma model are significantly reduced in CCR2−/− mice.34 Moreover, decreased recruitment of CD4+ and CD8+ lymphocytes into the brain, reduced levels of IFNγ in the brain and decreased numbers of virus-specific IFNγ-secreting CD8+ cells in the spleen were observed in IP-10/CXCL10-deficient mice infected with MHV.35
CCL20 neutralization inhibited IFNγ production and enhanced the level of IL-4 produced in the spleen during the infection, shifting the ratio of IFNγ/IL-4 from 20.2±0.06 to 4.64±1.39, and indicating that CCL20 plays an important role in shaping the type 1 immune response against S. enteritidis. In this respect, it is interesting to note that while immune deviation towards a type 2 profile occurred in the spleen, no such trend was observed in other secondary lymphoid organs including the inguinal lymph nodes (data not shown) and the Peyer's patches, where anti-CCL20 treatment had no significant effect on IFNγ or IL-4 levels. The mechanism for this immune deviation upon neutralization of CCL20 is unclear. CCL20 is clearly expressed in secondary lymphoid organs during infection or during autoimmunity (present study and Kohler et al19), and CCR6, the only known receptor for CCL20 is upregulated on Th1 cells during clonal selection.36 Several previous observations support the theory that CCL20 contributes directly to the differentiation of Th1 cells. First, homeostatic levels of myeloid-derived DC are dramatically reduced in the Peyer's patches in CCR6−/− mice compared with their wild-type controls,15 and CCL20/CCR6 has been implicated in DC trafficking in the lung and the skin.24, 37, 38 It is therefore possible that neutralization of CCL20 interferes with the ability of Th1-regulating DC to perform their normal function in secondary lymphoid organs.39 Second, neutralization of CCL20 with the same antibody as that used in the present study, inhibited the development of experimental autoimmune encephalomyelitis (EAE) by inhibiting the priming phase of the disease.19 In that case, the inhibition of EAE, a Th1 immune response, was due to decreased sensitization of the Th1 cells to proteolipid protein (PLP139–151) and a delay in the exit of encephalitogenic T cells from the lymph nodes. Finally, because activated neutrophils are a major source of IFNγ in the spleen after primary infection with Salmonella40 and can express functional CCR6,41 CCL20 may also be involved in the establishment of a type 1 environment during infection by regulating recruitment of such IFNγ-producing effector cells to sites of infection.
The question arises as to how inhibition of CCL20 activity leads to increased numbers of bacteria in the Peyer's patches even though there is no effect on the level of IFNγ production at that location. Low constitutive levels of both CCL20 and IFNγ were detected in the Peyer's patches and these were not altered during the course of bacterial infection. This suggests that local production of these two molecules does not contribute to the antibacterial response in the Peyer's patches. This is in contrast to that occurring in the spleen where both CCL20 and IFNγ expression are strongly induced and neutralization of CCL20 inhibits IFNγ production. Therefore, at least during the acute phase of Salmonella infection (day 5 postinfection), the most likely explanation is that the number of bacteria in the Peyer's patches is dependent on the antibacterial response occurring in the spleen.
While our data indicate that CCL20 plays an important role in the antibacterial response by promoting IFNγ production and a type 1 immune response in the spleen, an additional mechanism by which CCL20 may regulate bacterial dissemination is via direct antimicrobial activity as part of the innate immune system. Although it must be stated that this has not yet been clearly demonstrated in vivo, many chemokines, including CCL20, have recently been demonstrated to have significant in vitro antimicrobial activities, particularly against Gram-negative bacteria.32, 42, 43
In this study, we compared expression and function of CCL20 with that of the closely related chemokine CCL3. In contrast to that observed with CCL20, CCL3 protein was induced at all of the locations examined, in keeping with its classification as an inflammatory chemokine. The cellular source of CCL3 can be quite diverse, ranging from structural cells such as fibroblasts, to epithelial cells, lymphocytes or resident and recruited macrophages. In further contrast to that observed with CCL20, while neutralization of CCL3 also led to an increase in bacterial burden, particularly in the Peyer's patches, it had no effect on the level of IFNγ production in target lymphoid organs, but instead inhibited the humoral response directed against the bacteria. While previous data support a role for CCL3 in the orientation towards type 1 immune responses,44 our data are supported by those from other studies examining bacterial infection in chemokine knockout mice. Indeed, a significant increase in bacterial burden was observed in CCL3−/− mice; however, there was no difference in either leukocyte recruitment or the level of type 1 cytokines produced, including IFNγ and IL-12.45, 46
In conclusion, the results of this study demonstrate an important role for CCL20 in the adaptive arm of the immune response to bacteria, more specifically in cell-mediated immunity against S. enteritidis, and the limitation of bacterial dissemination and/or multiplication. Our data demonstrate a similar role for the related CC chemokine CCL3 in the control of bacterial growth via effects on humoral immunity rather than cell-mediated immunity. Together with the results of previous in vivo studies that indicate a role for CCL20 in humoral immune responses in the mucosal epithelium15 and for CCL3 in cell-mediated immunity,45 our data further serve to illustrate the complex biology of the chemokine system where particular chemokines can affect different arms of the immune system depending on location and the nature of the immunogen. Future work will focus on establishing the role of CCL20 in immunity against a broader range of bacteria, including intra- and extracellular bacteria, as well as examination of the secondary immune response to bacteria.
References
Gale LM, McColl SR . Chemokines: extracellular messengers for all occasions? Bioessays 1999;21:17–28.
Annunziato F, Romagnani P, Cosmi L, et al. Chemokines and lymphopoiesis in human thymus. Trends Immunol 2001;22:277–281.
Ansel KM, Cyster JG . Chemokines in lymphopoiesis and lymphoid organ development. Curr Opin Immunol 2001;13:172–179.
Zlotnik A, Yoshie O . Chemokines: a new classification system and their role in immunity. Immunity 2000;12:121–127.
Baggiolini M . Chemokines and leukocyte traffic. Nature 1998;392:565–568.
Godessart N, Kunkel SL . Chemokines in autoimmune disease. Curr Opin Immunol 2001;13:670–675.
Luster AD . The role of chemokines in linking innate and adaptive immunity. Curr Opin Immunol 2002;14: 129–135.
Schutyser E, Struyf S, Van Damme J . The CC chemokine CCL20 and its receptor CCR6. Cytokine Growth Factor Rev 2003;14:409–426.
Tanaka Y, Imai T, Baba M, et al. Selective expression of liver and activation-regulated chemokine (LARC) in intestinal epithelium in mice and humans. Eur J Immunol 1999;29:633–642.
Krzysiek R, Lefevre EA, Bernard J, et al. Regulation of CCR6 chemokine receptor expression and responsiveness to macrophage inflammatory protein-3alpha/CCL20 in human B cells. Blood 2000;96:2338–2345.
Yang D, Howard OM, Chen Q, et al. Cutting edge: immature dendritic cells generated from monocytes in the presence of TGF-beta 1 express functional C-C chemokine receptor 6. J Immunol 1999;163:1737–1741.
Dieu MC, Vanbervliet B, Vicari A, et al. Selective recruitment of immature and mature dendritic cells by distinct chemokines expressed in different anatomic sites. J Exp Med 1998;188:373–386.
Varona R, Zaballos A, Gutierrez J, et al. Molecular cloning, functional characterization and mRNA expression analysis of the murine chemokine receptor CCR6 and its specific ligand MIP-3alpha. FEBS Lett 1998;440:188–194.
Fujiie S, Hieshima K, Izawa D, et al. Proinflammatory cytokines induce liver and activation-regulated chemokine/macrophage inflammatory protein-3alpha/CCL20 in mucosal epithelial cells through NF-kappaB [correction of NK-kappaB]. Int Immunol 2001;13: 1255–1263.
Cook DN, Prosser DM, Forster R, et al. CCR6 mediates dendritic cell localization, lymphocyte homeostasis, and immune responses in mucosal tissue. Immunity 2000;12:495–503.
Varona R, Villares R, Carramolino L, et al. CCR6-deficient mice have impaired leukocyte homeostasis and altered contact hypersensitivity and delayed-type hypersensitivity responses. J Clin Invest 2001;107: R37–R45.
Izadpanah A, Dwinell MB, Eckmann L, et al. Regulated MIP-3alpha/CCL20 production by human intestinal epithelium: mechanism for modulating mucosal immunity. Am J Physiol Gastrointest Liver Physiol 2001;280:G710–G719.
Nishi T, Okazaki K, Kawasaki K, et al. Involvement of myeloid dendritic cells in the development of gastric secondary lymphoid follicles in Helicobacter pylori-infected neonatally thymectomized BALB/c mice. Infect Immun 2003;71:2153–2162.
Kohler RE, Caon AC, Willenborg DO, et al. A role for macrophage inflammatory protein-3alpha/CC chemokine ligand 20 in immune priming during T cell-mediated inflammation of the central nervous system. J Immunol 2003;170:6298–6306.
Tessier PA, Naccache PH, Clark-Lewis I, et al. Chemokine networks in vivo: involvement of C-X-C and C-C chemokines in neutrophil extravasation in vivo in response to TNF-alpha. J Immunol 1997;159: 3595–3602.
Tessier PA, Naccache PH, Diener KR, et al. Induction of acute inflammation in vivo by staphylococcal superantigens. II. Critical role for chemokines, ICAM-1, and TNF-alpha. J Immunol 1998;161:1204–1211.
Attridge SR, Kotlarski I . Local transfer of delayed-type hypersensitivity after Salmonella infection in mice. Infect Immun 1985;50:807–812.
Ogunniyi AD, Manning PA, Kotlarski I . A Salmonella enteritidis 11RX pilin induces strong T-lymphocyte responses. Infect Immun 1994;62:5376–5383.
Dieu-Nosjean MC, Massacrier C, Homey B, et al. Macrophage inflammatory protein 3alpha is expressed at inflamed epithelial surfaces and is the most potent chemokine known in attracting Langerhans cell precursors. J Exp Med 2000;192:705–718.
Ruth JH, Shahrara S, Park CC, et al. Role of macrophage inflammatory protein-3alpha and its ligand CCR6 in rheumatoid arthritis. Lab Invest 2003;83: 579–588.
Chabaud M, Page G, Miossec P . Enhancing effect of IL-1, IL-17, and TNF-alpha on macrophage inflammatory protein-3alpha production in rheumatoid arthritis: regulation by soluble receptors and Th2 cytokines. J Immunol 2001;167:6015–6020.
Sierro F, Dubois B, Coste A, et al. Flagellin stimulation of intestinal epithelial cells triggers CCL20-mediated migration of dendritic cells. Proc Natl Acad Sci USA 2001;98:13722–13727.
Sugita S, Kohno T, Yamamoto K, et al. Induction of macrophage-inflammatory protein-3alpha gene expression by TNF-dependent NF-kappaB activation. J Immunol 2002;168:5621–5628.
Scapini P, Laudanna C, Pinardi C, et al. Neutrophils produce biologically active macrophage inflammatory protein-3alpha (MIP-3alpha)/CCL20 and MIP-3beta/CCL19. Eur J Immunol 2001;31:1981–1988.
Schutyser E, Struyf S, Menten P, et al. Regulated production and molecular diversity of human liver and activation-regulated chemokine/macrophage inflammatory protein-3 alpha from normal and transformed cells. J Immunol 2000;165:4470–4477.
Yang D, Chertov O, Bykovskaia S, et al. Beta-defensins: linking innate and adaptive immunity through dendritic and T cell CCR6. Science 1999;286:525–528.
Hoover DM, Boulegue C, Yang D, et al. The structure of human macrophage inflammatory protein-3alpha/CCL20. Linking antimicrobial and CC chemokine receptor-6-binding activities with human beta-defensins. J Biol Chem 2002;277:37647–37654.
Bao S, Beagley KW, France MP, et al. Interferon-gamma plays a critical role in intestinal immunity against Salmonella typhimurium infection. Immunology 2000;99:464–472.
Jinnouchi K, Terasaki Y, Fujiyama S, et al. Impaired hepatic granuloma formation in mice deficient in C-C chemokine receptor 2. J Pathol 2003;200:406–416.
Dufour JH, Dziejman M, Liu MT, et al. IFN-gamma-inducible protein 10 (IP-10; CXCL10)-deficient mice reveal a role for IP-10 in effector T cell generation and trafficking. J Immunol 2002;168:3195–3204.
Ebert LM, McColl SR . Up-regulation of CCR5 and CCR6 on distinct subpopulations of antigen-activated CD4+ T lymphocytes. J Immunol 2002;168:65–72.
Greaves DR, Wang W, Dairaghi DJ, et al. CCR6, a CC chemokine receptor that interacts with macrophage inflammatory protein 3alpha and is highly expressed in human dendritic cells. J Exp Med 1997;186:837–844.
Power CA, Church DJ, Meyer A, et al. Cloning and characterization of a specific receptor for the novel CC chemokine MIP-3alpha from lung dendritic cells. J Exp Med 1997;186:825–835.
Cella M, Scheidegger D, Palmer-Lehmann K, et al. Ligation of CD40 on dendritic cells triggers production of high levels of interleukin-12 and enhances T cell stimulatory capacity: T-T help via APC activation. J Exp Med 1996;184:747–752.
Kirby AC, Yrlid U, Wick MJ . The innate immune response differs in primary and secondary Salmonella infection. J Immunol 2002;169:4450–4459.
Yamashiro S, Wang J, Yang D, et al. Expression of CCR6 and CD83 by cytokine-activated human neutrophils. Blood 2000;96:3958–3963.
Yang D, Chen Q, Hoover DM, et al. Many chemokines including CCL20/MIP-3alpha display antimicrobial activity. J Leukoc Biol 2003;74:448–455.
Starner TD, Barker CK, Jia HP, et al. CCL20 is an inducible product of human airway epithelia with innate immune properties. Am J Respir Cell Mol Biol 2003;14:14.
Dorner BG, Scheffold A, Rolph MS, et al. MIP-1alpha, MIP-1beta, RANTES, and ATAC/lymphotactin function together with IFN-gamma as type 1 cytokines. Proc Natl Acad Sci USA 2002;99:6181–6186.
Lindell DM, Standiford TJ, Mancuso P, et al. Macrophage inflammatory protein 1alpha/CCL3 is required for clearance of an acute Klebsiella pneumoniae pulmonary infection. Infect Immun 2001;69:6364–6369.
Olszewski MA, Huffnagle GB, McDonald RA, et al. The role of macrophage inflammatory protein-1 alpha/CCL3 in regulation of T cell-mediated immunity to Cryptococcus neoformans infection. J Immunol 2000; 165:6429–6436.
Acknowledgements
This work was supported by a grant from the National and Health Medical Research Council of Australia.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fahy, O., Townley, S., Coates, N. et al. Control of Salmonella dissemination in vivo by macrophage inflammatory protein (MIP)-3α/CCL20. Lab Invest 84, 1501–1511 (2004). https://doi.org/10.1038/labinvest.3700176
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.3700176
Keywords
This article is cited by
-
B cells are required for tumor-targeting Salmonella in host
Applied Microbiology and Biotechnology (2011)
-
Regulation of the Psoriatic Chemokine CCL20 by E3 Ligases Trim32 and Piasy in Keratinocytes
Journal of Investigative Dermatology (2010)
-
An injected bacterial effector targets chromatin access for transcription factor NF-κB to alter transcription of host genes involved in immune responses
Nature Immunology (2007)