Abstract
Study design:
Prospective observational study.
Objectives:
To identify the epidemiological features specific to spinal injuries as a result of an earthquake.
Settings:
Rawalpindi, Pakistan in the months after the 8 October 2005 earthquake.
Methods:
In the month after the earthquake, the one established rehabilitation center was augmented with two makeshift spinal cord centers. Information on mechanism of injury, mode of evacuation, associated injuries was gathered, and a detailed clinical and radiological assessment was performed. Neurological status and functional outcome was determined after 10 weeks.
Results:
Of an estimated 650–750 spinal cord injuries, 187 were admitted to these centers, including 80 men and 107 women with a mean age of 28.3±12.4 years. Injuries occurred while standing in 57.8% of patients. Most (83.4%) who reached the spinal cord center were airlifted. A urinary catheter had been placed before admission in 91.5%. Most of the patients were paraplegic 89.3, with 50.8% incomplete injuries. Fracture or fracture dislocation was present in 70, and 75% underwent spinal fixation. Although pressure ulcers (28.9%) and urinary tract infections (39%) were common, deep venous thromboses (4.8%) and depression (5.8%) were seldom detected. At 10 weeks, 75% were continent or performing intermittent catheterization. There were no deaths and two births.
Conclusion:
After a disaster, evacuation of persons with a spinal cord injury to a specialized center results in low mortality. Response planning for disasters should include early aggressive medical rehabilitation.
Sponsorship:
None.
Similar content being viewed by others
Introduction
Disasters have inflicted pain, suffering, death, and disability on populations since the beginning of time. But recent incidents, including the Indian Ocean tsunami, the flooding of New Orleans, and our Pakistan earthquake have brought disaster preparedness to the forefront of international policy.
Management of disability after disaster has received little attention in disaster-planning circles. For example, a Medline search on the topics ‘spinal cord injury’ and ‘earthquake’ resulted in only eight articles, none of which pertained to epidemiology or management.
On 8 October 2005 at 8:52 PST, an earthquake measuring 7.6 on the Richter scale occurred in the northern areas of Pakistan and India, with an epicenter 100 km north–north east of Islamabad. Seventy-three thousand people lost their lives and 126 000 were injured.1, 2 It was the most devastating and debilitating natural disaster in the country's history, causing widespread destruction and loss of life and property. The task of managing so many casualties in a third-world country with a physician density of 0.74 per 1000 people3 was gigantic.
The disaster was a unique learning opportunity for the rest of the world. In the process of establishing and augmenting emergency spinal cord rehabilitation centers and caring for the victims, we obtained invaluable data on the nature of spinal cord injury (SCI) in an earthquake and a process of handling them.
Materials and methods
Medical setting
Before this event, rehabilitation in Pakistan was generally equated with ‘physiotherapy’, rather than the medical specialty of Physical Medicine and Rehabilitation and the concept of a multidisciplinary team. Thus, despite neurosurgical departments in nearly all major teaching hospitals, there existed no SCI unit and disaster planning did not include disability management. Only one dedicated rehabilitation medicine institute was functioning at the time of the disaster – the Armed Forces Institute of Rehabilitation Medicine (AFIRM), a 100-bed, tertiary-care hospital providing rehabilitation services to persons with SCI, stroke, amputation, musculoskeletal disabilities, and pediatric disabilities.
After the earthquake, all communications from the affected areas were cutoff, so a rapid response to the catastrophe could not occur. No disaster-relief plan existed to meet such a challenge. As the news spread out and aid started pouring in, an airborne operation including approximately 70 helicopters4 was launched.
This was a prospective observational study conducted at three centers in Rawalpindi: the established spinal rehabilitation unit at AFIRM, a makeshift Paraplegic Centre developed from a converted pulmonary ward at the District Headquarters Hospital (DHQ), and the converted Neurosurgical Ward at Holy Family Hospital (HFH). Rehabilitation medicine consultants and residents from AFIRM regularly visited these centers to follow up the patient's progress and to facilitate SCI rehabilitation.
No national SCI registry existed in the country, so exact number of SCI patients could not be determined with accuracy; but according to different estimates the number of SCI patients in this disaster was between 650 and 750.5, 6 A preliminary survey of SCI carried out in the third week post earthquake to assess the magnitude of the problem revealed that there were 300 diagnosed cases of SCI admitted in different hospitals of the city. Women were more commonly admitted (196 versus 104), but this was likely an artifact of the fact that one facility, ‘Melody Rehabilitation Center’, dedicated entirely to women, had 60 admissions.
Patients and methods
One hundred and ninety-five persons admitted to these three centers between 9 October 2005 and 9 November 2005 were enrolled in the study. Eight patients who left against medical advice or were transferred elsewhere were lost to follow-up, leaving 187 subjects. A detailed evaluation of the patients included a complete history, compilation of demographic data, time and mode of evacuation, identification of mechanism of injury, associated problems/injuries, level and nature of injury, and radiological evaluation (by X-rays in all cases and computed tomography and magnetic resonance imaging of the spine in selected cases). SCI was diagnosed on the basis of clinical findings and radiological evidence by the neurosurgeon, spinal surgeon, or rehabilitation medicine specialist, with severity determined by the American Spinal Injury Association (ASIA) classification.7
The patients were assessed in detail every 2 weeks for improvement in the clinical status and development of secondary complications of SCI; with emphasis on detection of deep vein thrombosis, pressure ulcer formation, urinary tract infections (UTIs), depression, and neuropathic pain. Only approximately 10–12% received thromboprophylaxis in the form of compression stockings, unfractionated and low molecular weight heparin. Patients were observed for development of clinical signs and symptoms suggestive of DVT (swelling, pain, redness, and tenderness of the calf), and in case of clinical suspicion underwent duplex ultrasound scan at the affiliated radiology department to confirm or refute the diagnosis of DVT.
Patients were followed up for 10 weeks. Stable patients with SCI ASIA-E discharged earlier were asked to follow-up in the outpatient department on a monthly basis. The final assessment was carried out in the last week of January.
Oral informed consent was obtained from the patients or parents/guardians as appropriate at the start of the study. Data were entered on forms designed specifically for the study and the record was maintained on two separate computers. Data were compiled and results were analyzed using SPSS V 11.
Results
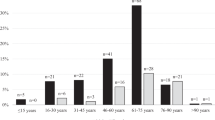
This study group of 187 patients had a mean age 28.3±12.4 (range 3–75) years (see Table 1). The majority of victims (57.2%) were women, and they were slightly younger than the men, with mean ages of 26.5±11.9 and 30.75±12.8, respectively. Of the women, 67% were housewives, 18% were students, 12% were unemployed, and 3% were employed, all by the government. An equal number of both sexes were married (65%).
Most of the injuries (108, 57.8%, 54 men and 54 women) were sustained by people while they were standing or running about to save themselves from falling rubble. Fifty-four (28.9%) of the patients were injured in the sitting position as roofs collapsed (43 women and 11 men), 24 sustained injuries while lying (nine women and 15 men), and one was injured in a jump from the second floor of a house. The majority of the patients (83.4%) were air-lifted from the affected zone by helicopters, 15.5% were evacuated by road, whereas two (1.1%) utilized both modes.
Nature of injuries
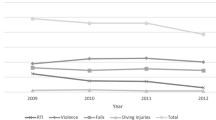
At the time of admission, 86 (46%) patients had incomplete paraplegia, 81 (43.3%) had complete paraplegia, nine (4.8%) had incomplete tetraplegia, and 11 (5.9%) had no neurological deficit. Incomplete paraplegia was the most common presentation in women whereas complete paraplegia was the dominant presentation in men. There was no case of complete tetraplegia (see Table 2). Out of the 95 patients who had incomplete injury, 46 were in ASIA B, 41 were ASIA C, and eight were ASIA D (see Figures 1 and 2).
Radiologically 68 (36.4%) patients had vertebral fractures, whereas 62 (33.2%) had fracture dislocation (see Table 3). Surgical intervention was not available in many cases, but most (75.4%) underwent spinal fixation. The main criteria for fixation was unstable spine or, in late cases, intractable pain. Nearly all spinal fixations were carried out via the posterior midline approach.
Six women sustained traumatic brain injuries, three men and seven women sustained pelvic fractures (total 5.3%), nine had abdominal injuries, and 11 had chest injuries. There were 24 fractures, of which 21 affected long bones. Twelve had deep lacerations and one had severe tissue loss in a leg. Significant pre-existing diseases included ischemic heart disease, hypertension, cholelithiasis, diabetes mellitus, multi nodular goiter, and pneumonia in one patient each, and tuberculosis in two patients.
Management and complications
Most of the patients (91.4%) had indwelling catheters in place at the time of admission. As described in Table 4, 57% of men learned clean intermittent catheterization whereas only 43% of women did so. Seventy-three (39%) patients developed UTIs, including 42 women and 31 men. Four male patients who were on clean intermittent catherization developed urethroscrotal fistulae.
Of 17 patients who were suspected clinically to have DVT, ultrasound was positive in nine (4.8%), with a higher incidence in men (6.2%) versus women (3.7%), and no difference in side of clot. All were of ages of 10–30 years. Five of these had complete SCI, three were ASIA B, and one was ASIA D, with one cervical, seven thoracic, and one lumbar injury. Five had undergone spinal surgery. None had any prophylaxis.
Most of the 28.5% of persons who had pressure ulcers (PU) were from the makeshift SCI centers. Seventeen percent of patients developed neuropathic pain, including 19 women and 13 men. Depression, assessed using the Beck Depression Inventory, was found in 5.8% of patients, including seven women and four men.
Discussion
This is the first study to specifically describe the epidemiology and management of SCI after an earthquake disaster. Disaster, defined as ‘any incident, involving large numbers of casualties which overwhelms the capacity of available resources to cope with it’,8 is predictable neither in time nor in place. It is certain that disasters will occur, however; therefore it is critical that the experiences from previous ones, including this earthquake, be understood. The findings should be discussed in light of past work, the qualitative observations should be shared, and implications for persons planning for future disasters should be laid out. Notable findings include:
Epidemiology:
-
a)
No survivors with complete tetraplegia, mostly paraplegics (89%).
-
b)
A significant pediatric population (17%).
-
c)
Predominant female victims (ratio of 1:1.3).
Patient care:
-
a)
Most patients were airlifted (83%).
-
b)
Most had spinal fixation (75%).
-
c)
Two births, not a single death in patients cared for by the physiatric team.
Management:
-
a)
Rehabilitation resources were scarce before the disaster.
-
b)
Disaster planning did not include SCI.
-
c)
The physiatrist-run makeshift rehabilitation units were successful.
Comparison to other experiences
Epidemiological studies of SCI in both developed and developing countries have consistently shown reported male:female ratios of between 3:1 and 8.3:1.9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21 In contrast, women were more likely involved in our earthquake. In our male-dominated society, men go out as the bread winners and women largely stay at home. So many women were at home at the time of the earthquake and others rushed in from the fields to their homes to save their children. In a Turkish disaster, it appeared that women were better off, because they were protected from outdoor dangers.14 Large numbers of people were injured while standing or running around. This confirms to the study by Marou and Matumotto,22 which demonstrated that the majority of spinal fractures in the Kobe, Japan earthquake were sustained when people tried to sit up or stand on their traditional futon mattresses without bed frames. We conclude that both the nature of the dwellings and societal customs may be taken into account in preparing for different sex ratios in disaster.
The ages of our victims varied from 3 to 75, but the mean age was 28. Elsewhere the mean age appears to be older, ranging from 32 to 50 years.12, 16, 17, 20, 21, 23 This age group represents the main economic and social fabric of our community. Only adequate rehabilitation will guarantee their successful reintegration into the society as useful and productive members of society.
In other health-care situations, the percentage of persons with complete tetraplegia ranges from 8.1 to 54%.12, 13, 16, 18, 19, 23, 24, 25 There were none in our study. This may have to do with the available evacuation modes and local settings.26 The air evacuation chain effectively evacuated a large number of casualties and possibly was responsible for reduced morbidity and mortality in SCI patients.24 But air evacuation was not available to all. Kashmir is a mountainous area. Many people were buried for almost 12 h. The local population did not know how to handle a suspected SCI. Many victims were carried for miles on shoulders and charpoys. Those who were evacuated by road travelled in all types of vehicles inadequate for SCI patient transport. Even when they reached air evacuation sites SCI casualties had to wait, as priority was given to acute life-threatening injuries. It is highly unlikely that many people with complete tetraplegia would survive in these conditions.
Pediatric SCI is reported to be rare in the Western literature, ranging from 2 to 5%27, 28, 29, 30 but the incidence of pediatric SCI in this study is 16.5%. The earthquake struck at around 09:00 h in the morning when most of the children were in their classrooms. They could not get out as the earth shook and roofs collapsed trapping them under debris. Only two (6.45%) children had SCI without radiological abnormalities, much less than the 13–38% incidence quoted in previous studies.31, 32, 33
Qualitative observations
The main outcome was zero mortality in these 187 patients. This was made possible by accurate and early diagnosis, early detection, and prevention of complications responsible for high mortality in SCI patients. The majority of the UTIs and all of the urethroscrotal fistulae developed in patients being managed in temporary centers. The etiological factors are thought to be:
-
Inadequate fluid intake
-
Placement of indwelling catheters before admission at the site of disaster (where clean technique was not used)
-
Long-term placement of indwelling catheters
-
Poor perineal hygiene of patients
-
Repeated use of the disposable catheters.
Urethroscrotal fistulae developed in four male patients from the temporary spinal units and the etiology was wrong technique and forceful insertion of catheter.
Of the 54 patients with PU, three were admitted with PU and all of them had evacuation delayed for more than 15 days. Four patients at AFIRM and 47 patients at the Paraplegic Centre and HFH developed PU. The possible etiological factors could be:
-
Lack of knowledge regarding PU prevention on part of the doctors.
-
Inadequate change of posture.
-
Nonavailability of pressure-relief mattresses and cushions in the early phase.
-
Delay in identification of early signs of skin breakdown.
For over 30 years, it has been well established that multidisciplinary team management of disability is critical for success,34 and few would doubt the relative effectiveness of specialized SCI centers.35, 36 Our success demonstrates the importance of early involvement of rehabilitation specialists and multidisciplinary teams.
Policy implications
This disaster has highlighted the important role of spinal rehabilitation units. The lack of a national disaster management plan in the initial phase and absence of a national SCI registry in the rehabilitation phase was obvious and had important implications. Within the methodological limits of this study, and recognizing that circumstances in other disasters may differ from our experience, we believe that persons planning disaster response should take into consideration a number of lessons learned from this experience.
Disaster planners must assume that a large number of SCI will occur with earthquakes. They must develop plans to rapidly expand SCI centers under the direction of a Physical Medicine and Rehabilitation specialist. Plans should include identification and evacuation plans, staff training (in-service for inexperienced staff, patient education materials), space, equipment and supplies, quality monitoring, and chain of command.
Our success would not have been possible without the teams from WHO, Handicap International, South Africa, Canada, and Turkey. With fewer than 20 Rehabilitation Medicine Specialists in our country, we did not have sufficient resources to care for all injured persons. More people would have been served better if rehabilitation medicine had been adequately developed in our country before the disaster. Along with our own health policy leaders, medical professionals in industrialized countries have an important role in facilitating growth of rehabilitation medicine in countries such as ours, not only to prepare for emergencies, but also to sustain the social productivity of all persons.
Conflict of interests
None.
References
EM-DAT. The OFDA/CRED International Disaster Database. Brussels. Center for Research on the Epidemiology of Disasters. c 2006 [created 2006 April 27; cited 2006 April 30]. Available from http://www.em-dat.net/disasters/Visualisation/profiles/natural-table-emdat.php.
Pakistan Earthquake facts and figures sheet – 28 March, 2006. International Federation of Red Cross and Red Crescent Societies c 2005. [cited 2006 Oct 30]. Available from http://www.ifrc.org/Docs/pubs/disasters/pakistanearthquake/factsfigures0306.pdf.
World Health report 2006. World Health Organization. c 2006- [cited 2006 Oct 30]. Available from http://www.who.int/whr/2006/en/index.html.
Ahmad K . Saving lives in the aftermath of Pakistan's earthquake. Lancet 2005; 366: 1423–1424.
Health cluster bulletin. World Health Organization Pakistan. Islamabad. 2006 [cited 30 October 2006]. Available from http://www.whopak.org/pdf/Health_Cluster_Bulletin_South_Asia_Earthquake12.pdf.
Earthquake in Pakistan. Handicap International. UK [updated 2006 Feb 8; cited 2006 April 30] Available from http://www.handicap-international.org.uk/page_518.php.
Maynard FM et al. International standards for neurological and functional classification of spinal cord injury. Spinal Cord 1997; 35: 266–274.
Ambrose G . Disaster medical planning. In: Fulde GWO (ed). Emergency Medicine: The Principles of Practice, 2nd edn. Maclennan and Petty: Sydney 1992, pp 13–19.
Reneses JG, Cabrera RH, Monreno MM . Epidemiological study of spinal cord injury in Spain 1984–1985. Paraplegia 1991; 28: 180–190.
Sorenson FB, Pederson V, Clausen MD . Epidemiology of spinal cord lesions in Denmark. Paraplegia 1990; 28: 105–118.
Thurman DJ, Burnett CL, Jeppson L, Beaudoin DE, Sniezek JE . Surveillance of spinal cord injury in Utah-USA. Paraplegia 1994; 2: 665–669.
Martins F, Freitas F, Martins L, Dartigues JF, Barat M . Spinal cord injuries – epidemiology in Portugal's central region. Spinal Cord 1998; 36: 574–578.
Dincer F, Oflazer A, Beyazora M, Celiker R, Basgoze O, Altioklar K . Traumatic spinal cord injury in Turkey. Paraplegia 1992; 30: 641–664.
Karamehmetoglu SS et al. Traumatic spinal cord injuries in Istanbul, Turkey. An epidemiological study. Paraplegia 1995; 33: 469–471.
Lan C, Lai JS, Chang KH, Jean YC, Lien IN . Traumatic spinal cord injuries in the rural region of Taiwan: an epidemiological study in Hualien county, 1986–1990. Paraplegia 1993; 31: 398–403.
Maharaj JC . Epidemiology of spinal cord paralysis in Fiji: 1985–1994. Spinal Cord 1996; 34: 549–559.
Acton PA, Farley T, Freni LW, Ilegbodu VA, Sniezek JE, Wolleb JC . Traumatic spinal cord injury in Arkansas 1980–1989. Arch Phys Med Rehabil 1993; 74: 1035–1040.
Hart C, William E . Epidemiology of spinal cord injury: a reflection of changes in South African society. Paraplegia 1994; 32: 709–714.
Hoque MF, Grangeon C, Kylie Reed K . Spinal cord lesions in Bangladesh: an epidemiological study 1994–1995. Spinal Cord 1999; 37: 858–861.
Quinones M, Nassal M, Bader KIA, Muraikhi AE, Al Kahlout SR . Traumatic spinal cord injury in Qatar: an epidemiological study. Middle East J Emergency Med 2002; 2: 67–69.
Otom AS, Doughan AM, Kawar JS, Hattar EZ . Traumatic spinal cord injuries in Jordan an epidemiological study. Spinal Cord 1997; 35: 253–255.
Maruo S, Matumoto M . Spinal fractures resulting from the 1995 Great Hanshin Earthquake of the Kobe-Osaka area of Japan. Spinal Cord 1996; 34: 382–386.
Singh R, Sharma SC, Mittal R, Sharma A . Traumatic spinal cord injuries in Haryana: an epidemiological study. Ind J Community Med 2003; 28: 184–186.
Swain A, Grundy D . At the accident. In: Grundy D and Swain A (eds). ABC of Spinal Cord Injury, 4th edn. BMJ Publishing Group: London 2004, pp. 1–4.
Jackson AB, Dijkers M, DeVivo M, Poczateck RB . A demographic profile of new traumatic spinal cord injuries: change and stability over 30 years. Arch Phy Med Rehabil 2004; 85: 1740–1748.
Bernhard M, Gries A, Kremer P, Bottiger BW . Spinal cord injury (SCI) – prehospital management. Resuscitation 2005; 66: 127–139.
Durkin MS, Olsen S, Barlow B, Virella A, Connolly ES . The Epidemiology of urban pediatric neurological trauma: evaluation of, and implications for, injury prevention programs. Neurosurgery 1998; 42: 300–310.
Proctor MR . Spinal cord injury. Crit Care Med 2002; 30: S489–S499.
Reynolds R . Pediatric spinal injury. Curr Opin Pediatr 2000; 12: 67–71.
Augustis M, Abel R, Levi R . Pediatric spinal cord injury in a sub set of European countries. Spinal Cord 2006; 44: 106–112.
Brown RL, Brunn MA, Garcia VF . Cervical spine injuries in children: a review of 103 patients treated consecutively at a level 1 pediatric trauma center. J Pediatr Surg 2001; 36: 1107–1114.
Dickman CA, Zabramski JM, Hadley MN, Rekate HL, Sonntag VK . Pediatric spinal cord injury without radiographic abnormalities: report of 26 cases and review of the literature. J Spinal Disord 1991; 4: 296–305.
Turgut M, Akpinar G, Akalan N, Ozcan OE . Spinal injuries in the pediatric age group: a review of 82 cases of spinal cord and vertebral column injuries. Eur Spine J 1996; 5: 148–152.
Halstead LS . Team care in chronic illness: a critical review of the literature of the past 25 years. Arch Phys Med Rehabil 1976; 57: 507–511.
Illis LS . The case for specialist units. Spinal Cord 2004; 42: 443–446.
Ragnarsson KT . Restorative treatment of persons with spinal cord injury: current trends. J Rehabil Res Dev 1998; 35: 11–14.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Rathore, M., Rashid, P., Butt, A. et al. Epidemiology of spinal cord injuries in the 2005 Pakistan earthquake. Spinal Cord 45, 658–663 (2007). https://doi.org/10.1038/sj.sc.3102023
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3102023
Keywords
This article is cited by
-
Pulse article: survey of neurogenic bladder management in spinal cord injury patients around the world
Spinal Cord Series and Cases (2021)
-
International Spinal Cord Society (ISCoS) database: Asian Spinal Cord Network (ASCoN) Pilot Project [IDAPP]
Spinal Cord Series and Cases (2018)
-
Challenges in comprehensive management of spinal cord injury in India and in the Asian Spinal Cord network region: findings of a survey of experts, patients and consumers
Spinal Cord (2018)
-
Current and future international patterns of care of neurogenic bladder after spinal cord injury
World Journal of Urology (2018)
-
Descriptive study of earthquake-related spinal cord injury in Nepal
Spinal Cord (2017)