Abstract
Study design:
A case report of intramedullary spinal cord teratoma with remote diastematomyelia in a female adult.
Objective:
To present a rare case of a dysembryogenic spinal tumor with concurrent split cord malformation and to define the importance of early surgical removal of the tumor.
Setting:
A department of neurosurgery in Greece.
Methods:
A 44-year old woman, presented with progressive lower limb muscle weakness, gait disturbances and dysesthesias in the trunk and lower extremity. She underwent plain radiographs, CT and MRI scan, which revealed an exophytic intramedullary spinal cord tumor at the level of T8–T10 and distant diastematomyelia in the upper lumbar spine (L2–L3). She underwent surgical intervention. The tumor was subtotally removed. No attempt was made to treat diastematomyelia.
Results:
Postoperatively, the patient's neurological status started to improve gradually. After 1 year she exhibited better strength in the lower limb muscles and improved sensation. The histological examination demonstrated mature spinal teratoma consisting of ectodermal, mesodermal and endodermal elements.
Conclusions:
In adult patients with intramedullary masses of possible dysembryogenic origin, the whole spine must be examined for additional dysraphic lesions. The choice and the timing of a surgical intervention are strongly dependent on the clinical picture.
Similar content being viewed by others
Introduction
Spinal intramedullary teratomas are unusual dysembryogenic lesions accounting for only 0.2–0.5% of all spinal cord tumors.1, 2 Their association with diastematomyelia is extremely rare, and very few cases are reported in the literature.3, 4, 5 We present a female adult with a thoracic intramedullary teratoma, coexisting with diastematomyelia in the lumbar spine. Furthermore, we discuss the importance of early diagnosis and surgical intervention of the responsible lesion.
Case report
A 44-year-old woman presented at the Neurosurgical Department of Thriasio General Hospital, Elefsis, Greece, with a 5-year history of progressive neurological deterioration. There was no history of trauma and recent illness. This woman experienced pain and paresthesias on the left side of the body from the level of the umbilicus and below radiating into the ipsilateral leg, which were followed by numbness of the left leg, progressive weakness of lower limb muscles and gait disturbances. Thus, she had difficulty in walking, and was able to stand and walk only with assistance. There was no family history for any neurological disorders or congenital anomalies in the spinal cord.
The physical examination revealed extended muscle weakness on the left leg, especially affecting the thigh flexors and adductors (about 2+/5 strength). Plantar flexion and extension were 3+/5 and 4+/5, respectively. Deep tendon reflexes (knee and ankle jerk) were both increased without producing clonus. ASIA (American Spinal Injury Association) motor score in the lower extremity was 24/25 for the right leg and 14/25 for the left leg. Pain arising from the level of the umbilicus had a zosteroid character and was more evident on the anterior part of the leg proximally. Sensory disturbances extended from the level of T8 on the left side to the distal limb, and were more prevalent on the anterior side. Moreover, the neurological examination at the contralateral side of the lower extremity demonstrated slight thermal changes and decreased sensation to light touch. Deep touch and proprioceptive changes were intact. The patient reported no changes in bowel and bladder function. ASIA sensory examination score was 89/112 for light touch and 86/112 for pin prick sensation. The examination of the right side of the body apart from thermal changes and light touch deficits was normal. The clinical picture resembled the Brown–Sequard syndrome.
Plain radiographs at the level of cervical and thoracic spine showed no evidence of vertebral body anomalies, scoliosis or decreased intervertebral disc height and no association with spinal dysraphism. On the other hand, plain X-ray films of the lumbar and sacral spine demonstrated decreased intervertebral height at the level of L2–L3, erosion of the pedicles, spina bifida and transitional L5 vertebrae.
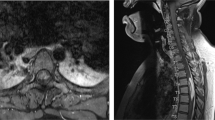
The patient underwent MR imaging of the thoracic and lumbar spine. In the lower thoracic spinal cord a heterogenous mass was visualized, extending from the T8 to T10 level with areas consisting of adipose tissue (Figure 1). According to the radiologists, these findings were compatible with a dermoid cyst. The MR imaging of the lumbar spine revealed a spinal canal divided into two sections (parts) at the level of L2–L3 vertebrae extending to the soft tissues. These findings were consistent with a diagnosis of diastematomyelia (Figure 2).
It was decided that the principle lesion was the teratoma, so the surgeons proceeded to remove the tumor and not to operate diastematomyelia. During surgery, a T8–T10 laminectomy was performed. The dura was opened through a midline incision revealing a pinkish–yellowish and irregular tumor suggesting teratoma. The tumor extended mostly between T8 and T9 vertebrae, was intramedullary in origin, but had also extramedullary–intradurally components. The intradural portion of the mass was totally removed. The operation proceeded via a postero-intermediate myelotomy, since the tumor emerged from this area of the spinal cord. The central part of the neoplasm was strongly adherent to the cord. A part of the intramedullary tumor was excised carefully by bipolar cauterization and ultrasonic aspiration. Intraoperatively, somatosensory-evoked potentials were used and, because they showed changes during the attempt of capsular resection, tumor capsule and an intramedullary component of the mass were left aside to avoid further morbidity. In this way a subtotal excision of the mass was accomplished with a portion of the tumor left on the inner aspect of the spinal cord around the central canal. The dura mater was closed primarily in a water-tight fashion.
Immediately postoperatively, after an initial deterioration in the motor signs, the patient experienced a slight improvement in the symptoms concerning sensory defects. After 2 days she was mobilized, got up and was able to walk with a solid cane wearing a waist support. The patient was discharged from the hospital 7 days postoperatively for further rehabilitation therapy, while corticosteroid administration discontinued.
By 6 months postoperatively, she gained some of her strength in her lower extremity, that is, thigh flexion and adduction 3+/5. ASIA motor score in the lower limb improved to 43/50 (25/25 for the right leg and 18/25 for the left leg). A year after the operation, proximal lower limb strength remained unchanged, but she demonstrated further improvement on the sensory deficits in terms of pain and paresthesias. ASIA sensory score was modified positively as well (93/112 for light touch and 90/112 for pin prick sensation). Moreover, by that time hip flexion and extension improved and she regained full strength in the distal lower limb muscles.
Thoracic and lumbar MR imaging were performed at 6 and 15 months postoperatively. A small amount of residual tumor was observed in the central spinal cord, which remained unchanged.
The tissue was processed in the conventional manner with formalin fixation followed by paraffin embedding. Grossly, the tissue consisted of multiple tan fragments with soft consistency. Histopathological examination revealed mature teratoma including three germ layers. It included keratinizing squamous epithelium overlaying neuroglial tissue (immunohistochemical detection of GFAP), aggregates of mucous secreting glands filled with abundant acidic mucins, mesonephric duct elements and tissues of mesenchymal origin (adipose, fibrous, as well as bone formation) (Figure 3a and b).
Discussion
Teratomas are uncommon intraspinal lesions, and their pathogenesis remains unclear. However, the most acceptable theory supports that they are derived from multipotential germinal cells which are misplaced during the early stages of embryonic development.6, 7 They account for 0.2–0.5% of all spinal cord tumors, and only 2% of all teratomas occur in the central nervous system.1, 2 According to the relevant literature, the most frequent site of intramedullary teratoma is the conus medullaris.8, 9
Teratomas belong to a group of tumors classified as inclusion tumors. Willis10 defined teratoma as a true tumor or neoplasm composed of multiple tissues of kinds foreign to the part in which it arises. True teratomas are histologically characterized by the presence of three germinal layers.7, 10, 11, 12 Tapper and Lack11 reviewed 256 teratomas in children, and only four were located inside the spinal canal. Sloof et al2 reported 301 intramedullary spinal cord lesions and distinguished only two cases of teratomas. In a review of the literature, Caruso et al8 described a total of 33 cases of intramedullary teratomas, including three with diastematomyelia.
Diastematomyelia or split cord malformation (SCM) is a form of spinal dysraphism referring to a congenital splitting of the spinal cord. It was first reported by Ollivier in 1837 and is usually accompanied by a number of other malformations.13 It is a rare condition and very few cases have been reported in adults.14, 15 According to Pang, two types of SCM exist: Type I is defined as two hemicords, each within a separate dural tube separated by a dural-sheathed osteocartilaginous medial septum. Type II consists of two hemicords within a single dural tube, separated by a nonrigid fibrous septum (diplomyelia).16, 17, 18 Our case was type I SCM. With the evolution and further accessibility of modern neuroimaging techniques, this entity is becoming more frequently diagnosed.19
In adults, intraspinal teratomas coexisting with split cord malformations have been rarely reported, especially those concerning the association of intramedullary teratomas with diastematomyelia.3, 4 Rosenbaum et al20 reported an adult case with both SCM and intradural teratoma. Interestingly, of the 12 cases with simultaneous presentation of SCM and intradural spinal teratoma described by Hader et al,4 only two were noted in adults. Elmaci et al3 presented a case of intradural spinal teratoma with diastematomyelia in a 42-year-old man, who was operated and demonstrated partial resolution of his symptoms one year after surgery.
Our case is unique because it does not only display the simultaneous appearance of intradural spinal teratoma and diastematomyelia, but also occurs in a female adult, has a history of 5 years from the onset of symptoms and the SCM exists at a remote site from the tumor. Additionally, the mass is intramedullary in origin with exophytic growth.
The treatment of diastematomyelia was considered not necessary because the patient did not manifest signs attributable to this pathology. On the other hand, the clinical picture implicated spinal cord compression at the level of T8–T10 due to teratoma. It must be emphasized that, postoperatively, signs attributable to L2 and below segments pathology showed improvement. Moreover, the postoperative improvement in hip flexion and extension justified the decision to remove the teratoma and not to treat diastematomyelia.
The aim of surgery should be radical extirpation of the mass whenever possible. In cases of intramedullary confinement of the tumor, this is almost impossible without some injury to the neural tissue. The reason is that the tumor is often strongly adherent to the surrounding nervous structures. Hejazi et al21 suggested that in order to prevent traumatizing adjacent spinal cord in cases where the teratoma tightly adheres to functional neurological tissue, an aggressive surgical attempt is not recommended. However, even in such cases, some late improvement might be expected under intensive physiotherapy. Total resection of extramedullary components is often feasible without undesirable consequences.
Intraoperative recording of somatosensory-evoked potentials provide further information regarding the neurophysiological status of the surgically manipulated neural tissue. In the present case, they were seriously taken into consideration since they demonstrated changes intraoperatively and drove the surgeons not to proceed to radical tumor excision. However, there are cases with somatosensory-evoked potentials changes, but with no neurological deterioration detected postoperatively.22
Surgery should be the first choice of treatment. Additionally, because of the benign behavior of these masses, a subtotal tumor resection can often provide acceptable results with no recurrence even for many years after the initial operation. On the other hand, in cases where parts of the nervous system are already injured irreversibly, as it occurred in our patient, the likelihood of complete recovery remains uncertain, even after a successful tumor resection.
Conclusions
In an adult presenting with a spinal teratoma, the whole spinal column must be evaluated to detect possible dysraphism. The probability of neurological deterioration and the establishment of permanent neurological deficits reinforce the aspect of early surgical removal. On the other hand, the surgeon has to rely more on his experience and the use of atraumatic manipulations, apart from the adjunct intraoperative neurophysiological facilities.
References
Austin G . The Spinal Cord. Basic Aspects and Surgical Considerations. CC Thomas: Springfield 1972, pp 335–346.
Sloof JL, Kernohan JW, MacCarty CS . Primary Intramedullary Tumors of Spinal Cord and Filum Terminale. WB Saunders: Philadelphia 1964, pp 1–20.
Elmaci I et al. Diastematomyelia and spinal teratoma in an adult. Case report. Neurosurg Focus 2001; 10: 1–4.
Hader W, Steinbok P, Poskitt K, Hendson G . Intramedullary spinal teratoma and diastematomyelia. Pediatr Neurosurg 1999; 30: 140–145.
Ugarte N, Gonzalez-Crussi F, Sotelo-Avila C . Diastematomyelia associated with teratomas. Report of two cases. J Neurosurg 1980; 53: 720–725.
Bucy PC, Buchanan DN . Teratoma of the spinal cord. Surg Gynecol Obstet 1935; 60: 1137–1144.
Sachus E, Horrax G . A cervical and lumba pilonidal sinus communicating with intraspinal dermoids. Report of two cases and review of the literature. J Neurosurg 1949; 6: 97–112.
Caruso R, Antoneli M, Cervoni L, Salvati M . Intramedullary teratoma: Case report and review of the literature. Tumori 1996; 82: 616–620.
Hamada H et al. Intramedullary spinal teratoma with spinal bifida. Child's Nerv Syst 2001; 17: 109–111.
Willis RA . The Borderland of Embryology and Pathology. Butterworth: London 1962.
Tapper D, Lack E . Teratomas in infancy and childhood. Ann Surg 1983; 198: 388–410.
Nonomura Y et al. Intramedullary teratoma of the spine:report of two adult cases. Spinal Cord 2002; 40: 40–43.
English WJ, Maltby GL . Diastematomyelia in adults. J Neurosurg 1967; 27: 260–264.
Ersahin Y, Mutluer S, Kocaman S, Demirtas E . Split spinal cord malformations in children. J Neurosurg 1998; 88: 57–65.
Prasad VS, Sengar RL, Sahu BP, Immaneni D . Diastematomyelia in adults. Modern imaging and operative treatment. Clin Imaging 1995; 19: 270–274.
Pang D, Dias MS, Ahab-Barmada M . Split cord malformations. Part I: a unified theory of embryogenesis for double spinal cord malformations. Neurosurgery 1992; 31: 451–480.
Pang D . Split cord malformations. Part II: clinical syndrome. Neurosurgery 1992; 31: 481–500.
Vaccaro A, Albert T . Mastercases: Spine Surgery. Thieme: Stuttgart 2001, pp 450–454.
Sheehan JP, Sheehan JM, Lopes MB, Jane Sr JA . Thoracic diastematomyelia with concurrent intradural epidermoid spinal cord tumor and cervical syrinx in an adult. Case report. J Neurosurg Spine 2002; 97: 231–234.
Rosenbaum TJ, Soule EH, Onofrio BM . Teratomatous cyst of the spinal canal: case report. J Neurosurg 1978; 49: 292–297.
Hejazi N, Witzmann A . Spinal intramedullary teratoma with exophytic components: report of two cases and review of the literature. Neurosurg Rev 2003; 26: 113–116.
Papastefanou S et al. Surface electrode somatosensory-evoked potentials in spinal surgery: implications for indications and practice. Spine 2000; 25: 2467–2472.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Tsitsopoulos, P., Rizos, C., Isaakidis, D. et al. Coexistence of spinal intramedullary teratoma and diastematomyelia in an adult. Spinal Cord 44, 632–635 (2006). https://doi.org/10.1038/sj.sc.3101886
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101886
Keywords
This article is cited by
-
Split cord malformation concomitant with spinal teratoma without open spinal dysraphism
Child's Nervous System (2022)
-
A comprehensive review of adult onset spinal teratomas: analysis of factors related to outcomes and recurrences
European Spine Journal (2020)
-
Adult-onset intradural spinal teratoma: report of 18 consecutive cases and outcomes in a single center
European Spine Journal (2017)
-
Split cord malformation types I and II: a personal series of 131 patients
Child's Nervous System (2013)