Abstract
Study Design:
Case report.
Objective:
To describe the mechanism of injury in this case and its clinical features. Magnetic resonance (MR) images of hemorrhage in spinal cord injury due to stab wound are discussed.
Methods:
We describe the case of a 21-year-old woman who was stabbed in the right side of her neck and developed left-sided Brown–Séquard syndrome plus loss of bilateral proprioceptive sensation. Neither plain radiographs nor computed tomography of the cervical spine demonstrated any foreign bodies or fractures of the cervical spine. T2-weighted cervical MR images confirm spinal cord hemiresection at C5–C6.
Results:
MR imaging was performed serially at 4 days, 4 weeks, and 8 weeks after trauma. The signal pattern of the spinal cord at the site of injury varied iso, iso, and low on T1-weighted consecutive images. Meanwhile, high signal intensity on T2-weighted images was consistent during the 8 weeks after incidence of trauma. A T2-weighted sagittal image showed a tiny spot of low intensity in the high signal band at the site of penetration, demonstrating hemosiderin formation in the spinal cord. The patient was treated conservatively and, recovered from Frankel grade C to grade D.
Conclusion:
Spinal cord injuries (SCI) following stab wounds are rare. MR imaging is definitely useful for recording and monitoring the pathology of SCI.
Similar content being viewed by others
Introduction
With the exception of South Africa, reports of stab wounds which result in spinal cord injuries (SCI) are infrequent.1, 2, 3 The significant feature of SCI due to penetrating injuries is that a relatively high percentage of the patients present with incomplete paraplegia. Furthermore, half of those with incomplete motor lesions had a Brown–Séquard syndrome, which is a characteristic spinal cord injury syndrome that results from lateral hemiresection of the cord.3 However, only a limited number of patients demonstrate the ‘pure’ form of Brown–Séquard syndrome. Much more common is the Brown–Séquard-plus syndrome consisting of asymmetric paresis with hypalgesia more marked on the less paretic side.4
The usefulness of magnetic resonance (MR) imaging for the detection of spinal cord abnormalities is well described, especially in the acutely injured spine.5, 6 MR imaging can demonstrate several pathological features involving the spinal cord, including intraspinal hemorrhage, acute cord edema, and contusion of the spinal cord.7 The appearance of intraspinal hemorrhage at MR image varies through several forms as the hematoma ages.5, 8 We report a case of cervical spinal cord stab injury with Brown–Séquard-plus syndrome that was treated conservatively for more than 2 years.
Case report
The patient is a 21-year-old woman who had sustained a single stab wound in the right side of her neck while she was asleep in the prone position. She had bleeding with watery discharge possibly cerebrospinal fluid (CSF) from the neck wound. The moment she was assaulted, she felt an electric shock throughout her whole body and suddenly became unable to move both of her legs and her left arm. At the scene the patient was found to be awake and alert, and in no acute distress. She was taken to the local emergency hospital by ambulance and the wound was sutured primarily. The weapon used was not detected at the scene of the crime. Since the day of the admission, methylpredonisolone and antibiotics were administrated intravenously. At 6 days after injury, the patient was referred to Kansai Medical University Hospital.
Physical examination upon arrival revealed a 1-cm long, well-healed scar in the right side of her neck (Figure 1). The skin around the scar was slightly swollen, although nothing was palpable deep to scar.
Neurological examination revealed that motor function in both of her legs and in her left arm was impaired severely. Her left leg was completely flaccid, though her right leg could be moved slightly, and she was assessed as a grade C by Frankel classification.9 Joint position and vibration modalities were diminished up to the level of Th2 on both sides. There was a right-sided decrease in pain and temperature sensation below the C8 level. Sacral sensation was spared, although she developed urinary retention. A urinary catheter was inserted in the former hospital. The deep tendon reflexes were absent in the left leg with positive Babinski tests in her feet bilaterally. The patient had no significant past medical history or surgical history. The provisional diagnosis was that of a Brown–Séquard syndrome with the additional finding of a loss of proprioception on the right, secondary to a stab injury of the cervical spinal cord.
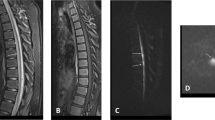
Neither plain radiographs nor a computed tomography of the cervical spine demonstrated any foreign bodies beneath the skin, nor a fracture of the spine. In order to confirm the diagnosis and to rule out an epidural abscess, MR imaging scan was performed. A right-sided parasagittal T2-weighted cervical MR image showed spinal cord hemiresection at the level of C5/C6 (Figure 2). The spinal cord was slightly swollen at the site of penetration. An axial T2-weighted MR image through the level of the lesion showed increased signal intensity indicative of edema in the swollen right side of the spinal cord. The linear area of increased intensity extending from the right dorsal to the left ventral aspect of the paraspinal muscle represents hemorrhage in the muscle along the trajectory of the weapon. Repeated MR studies performed 4 weeks later showed essentially the same findings as the initial images (Figure 3b and e). However, the MR images performed 8 weeks after the injury demonstrated a decreased signal on T1-weighted images at the level of C5/C6 (Figure 3c). Neither post-traumatic syringomyelia nor myelomaeracia was noted on this image. A spinal tap was performed to exclude pyogenic meningitis, because the patient complained of a persisting headache. The CSF was xanthochromic, with a glucose level of 117 mg/dl and a protein level of 84 mg/dl. No bacteria were detected on CSF culture.
A repeat sagittal T1-weighted study obtained 4 days (a), 4 weeks (b), and 8 weeks (c) after the trauma. A well-defined linear region of low signal intensity became evident on 8 weeks after injury (white allow). The sagittal T2-weighted scan performed 4 days (d), 4 weeks (e), and 8 weeks (f) after injury. The last image showed a tiny spot of low intensity in the high signal band in the spinal cord, demonstrating hemosiderin formation (black allow)
After 24 months of rehabilitation, the patient's motor strength returned to allow the patient to ambulate with the aid of a walker, though only for a few meters. She has been confined to a wheelchair for daily life. Proprioception and vibratory sense have improved up to the level of Th 10; by contrast, there is no recovery in sensation of pain and temperature. Grip power of her left hand has decreased by half of that noted on the right. Overall motor function was assessed as Frankel D at the time of the final evaluation.
Discussion
With the exception of South Africa, reports of stab wounds which result in SCI are relatively rare.1, 2 To the best of our knowledge, eight individuals with SCI due to the stab wounds have been reported in Japan since 1976. Lipschitz and Block1 reported 314 individuals with SCI caused by stab wounds. In all, 74% of the injuries were located in the thoracic spine followed by the cervical spine (18%) and the lumbar spine (8%). Peacock et al2 reported 450 patients who sustained stab wounds to the spine with ensuing SCI. He also reported that the most common site of the stab wound was in the thoracic spine (63%), followed by the cervical spine (30%) and lumbar spine (7%). By contrast, 75% of the cases in Japan were located in the cervical spine. The discrepancy of the injured level between South Africa and Japan is supposedly due to differences in socioeconomic status.
Lipschitz postulated three mechanisms of SCIs by penetrating injuries: (1) The weapon may damage the cord directly.1 Bone fragments may occasionally be driven into the spinal cord to produce damage. In this category of injury, the neurological deficits are supposed to be irreversible. (2) The vascular supply of the spinal cord may be damaged with resulting edema. The neurological disabilities associated with this type of injury will usually improve with the mitigation of edema. (3) Contrecoup spinal contusions or concussions may injure the cord. The penetrating knife blade causes local damage to the cord at the site of impact and, in addition, the force of the blow pushes the cord forward to impinge on the wall of the bony spinal canal. These types of disabilities may also have a chance to recover. Epidemiological studies of SCIs caused by stab wounds demonstrated that 50% of the patients with incomplete motor lesions had asymmetrical motor patterns indicative of a Brown–Séquard syndrome.3 The weapon usually enters the spinal canal via the interlaminar space along the anatomic gutter created by the spinous process in the coronal plane, and this serves to guide the weapon to only one side of the spinal cord, resulting in a Brown–Séquard syndrome.8 However, pure Brown–Séquard syndrome, characterized by ipsilateral hemiplegia and hypoesthesia and contralateral analgesia, has seldom been reported. Much more common is the so-called Brown–Séquard-plus syndrome consisting of asymmetric paresis with hypalgesia more marked on the less paretic side.10
In this patient, the stab injury took a lateral, almost horizontal, route between C5 and C6. Passing just behind the right lateral mass, the weapon perforated the ligamentum flavum allowing the blade's entrance into the spinal canal. In the neutral or extension position of the cervical spine, the laminae protect the spinal cord from penetrating injuries, thus, in this case, the patient was probably in the flexion position of the cervical spine when the stabbing occurred. The patient had left hemiplegia and loss of pain and temperature sensation on the right side, as well as loss of proprioception on both sides. This neurological finding indicates that the weapon had passed through the bilateral posterior columns and reached the right corticospinal tract and spinothalamic tract. The recovery of motor function indicates that the corticospinal tract was injured by a contrecoup contusion against the inside wall of spinal canal, rather than by a direct injury.
Accurate imaging studies are essential to explore the existence of a foreign body and to assess SCI. Standard radiographs and computed tomographic scans are strongly supported as the modalities for the assessment of vertebral fractures and foreign bodies but cannot detect spinal cord damage as MR imaging does. The greatest benefit of this modality is its ability to rule out a space-occupying lesion within the spinal canal, such as a hematoma or abscess, which may be amenable to surgery. However, MR imaging can be performed only after eliminating the possibility of a retained fragment. It is crucial to note that a retained foreign body with ferromagnetic properties may be dislodged and moved under the high magnetic field of MR imaging, and neurological deficit may be worsened.
To our knowledge, there are no reports presenting serial MR imaging studies of SCIs due to stab injuries. MR imaging was performed serially at 4 days, 4 weeks, and 8 weeks after injury in this patient. The linear area of high signal intensity on T2-weighted imaging at the level of C5/C6 demonstrated intraparenchymal hemorrhage of the spinal cord, which was incontrovertible evidence of the penetration of the weapon into spinal cord. The pattern of the MR images performed at 4 weeks after injury were essentially identical that noted in the early study. Intriguingly, a well-defined linear region of low signal intensity on T1-weighted imaging became evident on the last study. Furthermore, a T2-weighted sagittal image showed a tiny spot of low intensity in the high signal band at the site of penetration, demonstrating hemosiderin formation in the spinal cord. The appearance of intracranial hemorrhage on MR imaging which depends primarily on the age of hematoma is described by Bradley.11 As a hematoma ages, the hemoglobin passes through several forms (oxyhemoglobin, deoxyhemoglobin and methemoglobin) prior to red cell lysis and breakdown into hemosiderin. Methemoglobin is converted in hemosiderin after 2 weeks of hemorrhage.12 Hemosiderin is the final iron-containing product of hemoglobin degradation, which is produced by lysosomal degradation in macrophages. Although the speed at which hemoglobin degrades within spinal cord may not be the same as that applicable to the brain, the degradation of hemoglobin is supposed to proceed in the similar manner. It is a subject of great interest as to how the MR image appears in the late phase of SCI secondary to a penetrating injury. However, the patient did not consent to have further MR imaging studies.
The surgical treatment for SCIs due to the stab wounds is still controversial. Most surgeons advocate immediate exploration of the spinal cord wound when it is clear that a foreign body is present, a CSF leakage persists for several days, or there is progressive neurological deterioration.1, 2, 13 On the other hand, Simpson et al14 demonstrated no benefits from surgical treatment compared to conservative management in patients with penetrating spinal injuries. Based upon the indications for surgical intervention detailed by Lipschitz and Peacock, the patient in this report was treated conservatively.
References
Lipschitz R, Block J . Stab wounds of the spinal cord. Lancet 1962; 2: 169–172.
Peacock WJ, Shrosbree RD, Key AG . A review of 450 stabwounds of the spinal cord. S Afr Med J 1977; 51: 961–964.
Waters RL, Sie I, Adkins RH, Yakura JS . Motor recovery following spinal cord injury caused by stab wounds: a multicenter study. Paraplegia 1995; 33: 98–101.
Koehler PJ, Endtz LJ . The Brown–Sequard syndrome. True or false? Arch Neurol 1986; 43: 921–924.
Hackney DB et al. Hemorrhage and edema in acute spinal cord compression: demonstration by MR imaging. Radiology 1986; 161: 387–390.
Alkan A, Baysal T, Saras K, Sigirci A, Kutlu R . Early MRI findings in stab wound of the cervical spine: two case reports. Neuroradiology 2002; 44: 64–66.
Bondurant FJ et al. Acute spinal cord injury. A study using physical examination and magnetic resonance imaging. Spine 1990; 15: 161–168.
Kulkarni AV et al. Delayed presentation of spinal stab wound: case report and review of the literature. J Emerg Med 2000; 18: 209–213.
Frankel HL et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. I. Paraplegia 1969; 7: 179–192.
Taylor RG, Gleave JRW . Incomplete spinal cord injuries with Brown–Sequard phenomena. J Bone Joint Surg 1957; 39-B: 438–450.
Bradley Jr WG . MR appearance of hemorrhage in the brain. Radiology 1993; 189: 15–26.
Anzalone N, Scotti R, Riva R . Neuroradiologic differential diagnosis of cerebral intraparenchymal hemorrhage. Neurol Sci 2004; 25 (Suppl 1): S3–S5.
Rubin G, Tallman D, Sagan L, Melgar M . An unusual stab wound of the cervical spinal cord: a case report. Spine 2001; 26: 444–447.
Simpson Jr RK, Venger BH, Narayan RK . Treatment of acute penetrating injuries of the spine: a retrospective analysis. J Trauma 1989; 29: 42–46.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Takemura, S., Sasai, K., Ohnari, H. et al. Brown–Séquard-plus syndrome due to stab injury: a case report. Spinal Cord 44, 518–521 (2006). https://doi.org/10.1038/sj.sc.3101871
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101871
Keywords
This article is cited by
-
Pediatric arrowshot injury to cervical spinal cord-sagittal cord transection with no neurological deficit and good outcome: case report and review of literature
Child's Nervous System (2013)
-
The role of MRI in spinal stab wounds compared with intraoperative findings
European Spine Journal (2012)