Abstract
This paper seeks to consider the validity and utility of two related terms in spinal and other injuries: complex regional pain syndrome (CRPS) and chronic pain syndrome (CPS). It is argued that the words chronic regional pain syndrome convey neither understanding of the condition nor of its mechanism. They simply redefine the clinical problem, but fail to establish specific diagnostic features or consistent primary pathogenesis. CRPS is best construed as a reaction to injury, or to excessive, often iatrogenic, immobilization after injury; but it is not an independent disease. The diagnosis of CPS groups together ill-defined symptoms under a convenient, but medically untestable and therefore inept label. Patients, lawyers and support groups commonly deny psychogenesis, with the sadly mistaken notion that this implies a bogus or spurious cause.
Similar content being viewed by others
Introduction
Spinal injuries are among the most common causes of chronic pain. In total, 65% of them have chronic pain, which itself constitutes a major impediment to effective rehabilitation.1
A multiplicity of alternative names and definitions for any disorder suggests a state of medical confusion. This paper seeks to reconsider the validity and utility of two related terms in spinal and other injuries:
-
1)
complex regional pain syndrome (CRPS) and
-
2)
chronic pain syndrome (CPS).
Complex regional pain syndrome (CRPS)
CRPS bears several synonyms: causalgia; shoulder–hand syndrome; reflex sympathetic dystrophy syndrome (RSDS); Sudeck's atrophy.2 It is defined
a chronic pain syndrome with two forms. CRPS 1 currently replaces the term ‘reflex sympathetic dystrophy syndrome’. It is a chronic nerve disorder that occurs most often in the arms or legs after a minor or major injury. CRPS 1 is associated with severe pain; changes in the nails, bone and skin; and an increased sensitivity to touch in the affected limb. CRPS 2 replaces the term causalgia and results from an identified injury to the nerve.3, 4
The terminology was changed because the pathophysiology of CRPS is not known with certainty. It was decided that a descriptive term such as CRPS was preferable to the term ‘reflex sympathetic dystrophy,’ which carries with it the outdated assumption that the sympathetic nervous system is important in its causation.
Pathophysiologically, many impute evidence for functional changes within the central nervous system and for involvement of peripheral mechanisms.3 The sympathetic nervous system is said to play a key role in maintaining pain and autonomic dysfunction in the affected extremity. After a primary central lesion, secondary peripheral changes in the paretic extremity are believed to be important in initiating a CRPS. There is no diagnostic gold standard.5
Stage 1 (lasts 1–3 months): severe burning, aching pain increasing with the slightest touch or breeze; swelling with warmth or coolness; skin becomes dry and thin, changes colour; increased nail and hair growth; pain may move further up or down the affected limb.
Stage 2 (lasts 3–6 months): swelling spreads; noticeable changes in skin texture and colour; decreased hair growth; changes in bone seen in X-rays; stiff muscles and joints.
Stage 3 (irreversible changes become evident): pain may exist in the entire limb; permanent tissue changes; muscle wasting; limited mobility in limb; contractions involving muscles and tendons.
Criteria for diagnosis6 have been proposed: at least four of the following must be present:
The essential symptom of CRPS is continuous, intense pain out of proportion to the severity of the injury (if an injury has occurred), which gets worse rather than better, often accompanied by
-
1)
‘burning’ pain
-
2)
increased skin sensitivity
-
3)
changes in skin temperature: warmer or cooler compared to the opposite extremity
-
4)
changes in skin colour: often blotchy, purple, pale, or red
-
5)
changes in skin texture: shiny and thin and sometimes excessively sweaty
-
6)
changes in nail and hair growth patterns
-
7)
swelling and stiffness in affected joints motor disability, with decreased ability to move the affected body.
An abnormal pattern three-phase bone scan is characteristic of CRPS.
However, investigation suggests that the internal validity of the IASP (International Association for the Study of Pain) CRPS criteria could be improved by separating vasomotor signs/symptoms; the criteria remain, to a large extent, arbitrary.7 Elements of the criteria exist in other conditions, notably immobility. It is agreed that diagnosing CRPS can be difficult. Often, the symptoms appear to be disproportionately severe in relation to the original injury. Results of treatment are unpredictable, but increasing mobility, by whatever means it is achieved, appears to be the common factor in improvement.
Mechanisms suggested
It is believed that CRPS is caused by an injury to the pain-sensitive C- and A-delta fibres that innervate the involved tissue. It is a progressive illness that spreads with time and may encompass large portions of the body. Proponents of CRPS deny psychological predisposition, but patients often seem depressed because of the constant pain, lack of sleep and complete disruption of their lifestyle. Proponents maintain that continuing pain is owing to central sensitization.8 The commonly observed autonomic dysregulation has a major central nervous system component Atrophy and dystrophy are partly owing to loss of blood supply of the affected tissues. The movement disorder is partly due to deficiency of GABAergic mechanisms; tremor is an exaggeration of the normal physiologic tremor. CRPS is said to be the result of changes to the somatosensory systems, which process noxious, tactile and thermal information; and to the sympathetic systems that innervate skin and affect the ‘somatomotor systems’. The changes suggest that the central neural representations of the systems have been altered. Patients with CRPS have peripheral oedema, inflammation, sympathetic-afferent coupling (to explain sympathetically maintained pain) and trophic changes that cannot be explained by central disturbances.9 It is now recognized that the traditional nerve blocks, often used diagnostically, are effective in only a small percentage of patients.
Validity of CRPS
-
1)
In most cases, CRPS is claimed to have three stages. Often, however, CRPS does not follow this progression. A minority remit spontaneously, some people go into the later stages almost immediately. Others remain in Stage 1 indefinitely. No explanation is apparent in the literature6 for this inconsistent clinical course.
-
2)
The actual words chronic regiotial pain syndrome convey no understanding of the condition. They provide neither mechanism for pain, nor for the associated symptoms and signs. The term simply redefines the clinical problem and suggests that it represents a defined disease, though it fails to establish any specific features or consistent primary pathogenesis. It is open to abuse and is often misapplied to ill-defined complaints of pain that do not readily fit into other more precisely defined diagnosable diseases.
-
3)
The reliability of accepted criteria has rarely been studied and is not established. When a small interobserver study was conducted involving 25 CRPS patients, interviewed and examined by six physicians and by structured questionnaries, observer agreement for these was calculated with kappa statistics. Physicians’ agreement in assessment of signs and symptoms in CRPS patients varied greatly. And there was poor observer agreement (kappa: 0.20). The authors concluded that, using current criteria systems, the diagnosis of CRPS is not reliable.10 Such lack of reproducibility scarcely justifies the designation of a syndrome, let alone a diagnostic entity. Further, a recent paper entitled: Can complex regional pain syndrome be painless? asserts this diagnosis in the absence of pain11 and illustrates the hopeless confusion.
-
4)
In almost all cases, the affected limb has been immobilized or its use restricted by pain, swelling, or by medical advice, often for many weeks or months. Many of the claimed diagnostic signs of oedema, colour change, altered sweating and sympathetic reflexes frequently occur in limbs immobilized by plaster of Paris or splints for fractures, in the absence of persisting chronic pain or other features of CRPS. The role of immobilization as an explanation or contribution to the observed signs is under-rated and has never been systematically explored. It is accepted that the outlook is better with early diagnosis in the first stage; it may remit and normal movement will return with lessening pain. However, if immobility persists changes in bone and muscle may develop rapidly and become irreversible.12 Again, this emphasizes the importance of immobility as a factor.
CRPS remains a mysterious condition of persisting pain with both peripheral and central neural mechanisms as secondary events. Immobility and disuse whether in response to an acutely painful disorder, iatrogenic, or consciously adopted by the patient is seldom absent. Is CRPS a disease? – According to the Washington State Department Labor Industries 1999 report on CRPS:
‘Many clinicians believe that CRPS can best be construed as a ‘reaction pattern’ to injury or to excessive activity restrictions (including immobilization) following injury. From this perspective, CRPS may be a complication of an injury or be iatrogenically induced, but it is not an independent disease process.’
Chronic pain syndrome
Definition
The IASP13 defines pain as ‘an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage’ (p 210). Pain progression is ‘sensory → cognitive → affective → illness behavior.’ Chronic pain syndrome (CPS) is often a pejorative descriptor.13 It has also been defined as
chronic anxiety and depression, anger and changed lifestyle, all with a variable but significant level of genuine neurologically based pain.14
Most authors consider ongoing pain lasting longer than 6 months as diagnostic of CPS. Some proponents suggest that any pain that persists longer than the reasonable expected healing time for the involved tissues should be considered chronic pain. CPS is a constellation of syndromes that frequently are intractable. The suggested pathophysiology of CPS is multifactorial, complex and is poorly understood. Some authors have suggested that CPS might be a learned behavioural syndrome that begins with a noxious stimulus that causes pain. This pain behaviour then is rewarded externally or internally and occurs without any noxious stimulus. Internal reinforcement comes from the relief afforded by society acknowledging the suffering or illness and diversion or relief from emotions such as guilt, fear of work, sex, responsibilities. External reinforcements15, 16 include such factors as attention from family members and friends, socialization with the physician, medications, compensation and time off work.17
Chronic pain is undoubtedly debilitating and demoralizing. A vicious cycle ensues between physical pain and psychological dysfunction, where each exacerbates the other. Patients with different psychological illnesses18 are prone to CPS. Comprehensive treatment of any chronic pain requires identification of the aetiology and management using pharmacological, physical and psychological techniques, as appropriate.19 It is conjectured that pain signals keep firing in the nervous system for weeks, months, or years; but facts are sparse.
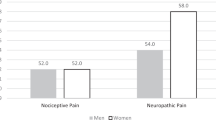
In some patients, there may be an unrelated continuing preinjury cause of pain such as arthritis, spondylosis or cancer. An analysis of 500 randomly selected households from a group family practice20 clinic showed 16% had experienced pain within the 2 weeks preceding the survey. The prevalence of those with persistent pain was twice that of those with temporary pain. More women than men reported both temporary and persistent pain. The lumbar spine, lower extremities, head and face were the most frequently affected. There may have been an initial illness, a spinal or chest, limb or pelvic injury or infection, from which the patient has apparently recovered. This initial insult may be severe, but more often is mild or trivial requiring no surgical intervention. However, many patients suffer chronic pain with minor or no identifiable injury, or other medical identifiable incident Medical advocates, with almost evangelical zeal tend to opinions rather than deductions based on factual observations.21 They declaim that such chronic pain is genuine, unrelenting and demoralizing. Pain itself is the problem. We recognize the associated complaints of weakness, fatigue, headaches, dizziness and apparent inability to work that become paramount but secondary features in many patients.
Patients may seek almost any available remedy. By the fact that they continue with symptoms it is evident that conventional pharmacological, surgical, physical and psychological approaches have failed to improve their condition. The evidence for many current treatments is still limited.1
The pain may lead to drug abuse and to a degree of dependency on family and friends that appears disproportionate to the identifiable illness or disease present at the onset of their condition. It drives others to demand and undergo repeated operations and resort to unqualified practitioners who promise quick and permanent ‘cures.’ But such desperation does not constitute evidence of the nature or severity of the complaint, as sometimes demanded by patient support groups.
There remains a core of clinical features as follows:
-
1
Patients have consulted many doctors.
-
2
They complain of pain persisting well beyond the expected time for the initiating event; pain that appears to be in excess of known pathology.
-
3
Symptoms frequently exceed objective signs on examination.
-
4
Investigations for the cause prove negative or equivocal.
-
5
There is minimal or no relief with analgesia and orthodox pain clinic treatments; symptoms may become worse after such treatments.
Acupuncture, transcutaneous electrical nerve stimulation, laser therapy, electrical nerve stimulation and neuroreflexotherapy are used in the management of chronic pain but in general, published trial results are deemed:
Contradictory or inadequate, reflecting poor study methodologies. No positive conclusion could be reached.22
Validity of CPS
The term describes a phenomenon, which is conceptually based on a behavioural, conditioning process. Published medical definitions point to a primary psychological illness (see above). Yet patients, lawyers and patient support groups21 commonly, strenuously deny psychogenesis, with the sadly mistaken notion that this implies a bogus or spurious cause. Patients' fear of aggravation or further injury impedes activity and independence. This is often iatrogenic. The resulting heightened state of arousal increases pain.
The definition of pain may be clarified by distinguishing (1) nociception, (2) pain and (3) suffering. Nociception is the activity produced in the nervous system by noxious (potentially tissue-damaging) stimuli. Clinically, nociception is inferred whenever tissue damage is identified. Pain is the perception of nociception.23 It follows that if there is no evidence of sufficient tissue damage, there is no organic demonstrable basis for continuing pain; nonorganic mechanisms may then pertain.
Overprotective attitudes to pain reduce mobility. Muscles become weak and may waste. To receive a reward for having pain is to reinforce it. Rewards can include attention and sympathy from family; exemption from domestic chores; avoidance of unpleasant work; and financial compensation through personal injury claims or disability payments. Regrettably, false labels, iatrogenic restriction of active lifestyle strongly conduce to a state of chronic invalidism coupled with both psychological and physical dependency.
The diagnosis of CPS allows ill-defined symptoms to be grouped under a convenient, socially respectable, but medically untestable and therefore inept label. With the medicalization now prevalent in society, defining something as a syndrome often gives it spurious legitimacy as a disease sui generis.
But a syndrome is not a disease since it does not have unique pathophysiological elements. Rather, it is an observation of frequently occurring features and behavioural responses categorized under a common title. Unfortunately, this is often based on relative and arbitrary features, for example, Battered Wife Syndrome, Sick Building Syndrome, Repressed Memory Syndrome. These labels may conceal undiagnosed organic pathology. More importantly, syndromes are often employed for their political and social utility in which the pathological affliction may be only in the eye of the beholder. In litigation, of course, the beholder is the claimant who needs definition for the perceived harm that has occurred.
There is no question that many suffering people have entered into a vicious cycle of pain leading to stress, leading to more pain and so on, as a result of an initial injury. Recruiting medical and psychological disciplines in a team approach may promise new hope for recovery, but more often leads to a restricted lifestyle based on iatrogenic disability and dependency.
The phenomenon of chronic pain must also be seen from a cultural and epidemiological perspective. In the latter half of the 20th century, chronic pain had grown to epidemic proportions. It is inextricably cleaved to the cultural concepts of pain. If something or someone can be impugned as the cause, then a degree of satisfaction or object for revenge may exist in individuals nurtured in the current ‘blame culture’. Back pain disability, for example, has increased 168% within a decade and pain from repetitive strain injury is a close second – and gaining annually. In a large prospective study at the Boeing plant in Washington, it was workers who did not enjoy their jobs, not those with poor physical stamina or heavy physical workload, who had a greatly increased risk of reported back symptoms.24
Lawyers recognize chronic pain as a frequent issue of litigation (see Oakes Marilyn T Certified Pain Practitioner21), in personal injury compensation claims. Chronic pain does not mean that patients are malingering, though this undoubtedly occurs25 in some claims. Terms such as malingering and compensation neurosis have been used pejoratively but are not always accurate. When there is a pre-existing psychological disorder, it is not merely a passive vulnerability worsened by the claimed injury, but it can be an active factor causing symptoms that express a psychological conflict. In other words, whether conscious or unconscious, the patient need the pain and may use it to solve a problem;26 the claimed injury is the opportunity for it to happen.
Many mental disorders are relevant to CPS. These are defined under the general rubric of Somatoform Disorders (see Diagnostic and Statistical Manual of Mental Disorders IV, American Psychiatric Association). Among them is Pain Disorder with psychological factors and/or a medical condition. Somatization Disorder, is also a chronic condition in which pain and other physical symptoms have gradually evolved from a psychosomatic predisposition. Undifferentiated Somatoform Disorder, is a nonspecific state in which the physical symptoms cannot be fully explained by any medical condition and may reflect personal, social or psychological problems. Review of the patient's history can identify the pre-existing issues and conflicts for which the physical symptoms are needed. In addition, many states of depression and anxiety can lead to pain. However, extensive Scandinavian studies have shown that where depression is seen in CPSs, it frequently precedes injury and pain, but is evident only when the life history is thoroughly explored.
Conclusions
1. CRPS: This term conveys no understanding of the condition. It provides no mechanism for pain, but simply redefines the clinical problem and misleadingly implies that it represents a defined disease. Yet it fails to establish any specific, testable, diagnostic features. It is open to abuse and is often misapplied to ill-defined complaints. Further, it may mask or conceal numerous other psychosocial variables: depression and anxiety states, pre-existing pain-prone personality, pre-existing life factors and work adjustment, history of the use of medical services, developmental and family histories and work records, absenteeism and occupational health issues.
It should be obvious that this requires more than a superficial interview and review of medical records by physicians and lawyers. The Medical Treatment guidelines, Washington State Department of Labor and Industries (1999 June, pp 3–19) stated:17
If a physician believes the CRPS condition is related to an accepted occupational injury, written documentation of the relationship (on a more probable than not basis) to the original condition should be provided. Treatment for CRPS will only be authorized if the relationship to an accepted injury is established.Most patients with widespread pain in an extremity do not have CRPS. Avoid the mistake of diagnosing CRPS primarily because a patient has widespread extremity pain that does not fit an obvious anatomic pattern. In many instances, there is no diagnostic label that adequately describes the patient's clinical findings. … CRPS may be a complication of an injury or be iatrogenically induced but it is not an independent disease process.
2. CPS is not a homogeneous condition: Even its proponents stress the importance of psychogenic factors. It is best seen as a divergent group of mainly psychogenic disorders often associated with poor motivation, social unhappiness, insecurity, or quest for financial gain. It seldom has an evident physical basis and sometimes no premorbid psychopathology. Although often deflected to nonmedical carers, the interplay of a medical training with clinical and therapeutic responsibility are, in my view, essential for the highest standards of diagnosis and prescription in patients with chronic pain. Overlooking the occasional organic pathology and aggravating or inducing disability by excessive zeal should be continual worries for therapists and support groups.
The Diagnostic and Statistical Manual of Mental Disorders (DSM-IV, 1994) of the American Psychiatric Association contains the closely related diagnosis ‘pain disorder,’ only as a diagnosis of exclusion.
We may agree with The American Society for Pain (IASP) task force, which omitted CPS as ‘a vague, often pejorative term.’27 The label has no clinical utility. Despite a legacy of poor-quality science, enthuasists continue to cite small, methodologically flawed studies purporting to show biologic variables for these syndromes. Despite a wealth of pain research, disciples continue to ignore the placebo effect, asserting a therapeutic hubris, although most studies admit a poor prognosis for CPS. The statement of Sir Francis Walshe comes to mind: the advocates of these syndromes are ‘better armed with technique than with judgment.’
References
Siddall PJ, Loeser JD . Pain following spinal cord injury. Spinal Cord 2001; 39: 63–73.
Sudeck PHM . Über die akute entzündliche Knochenatrophie. Arch Klin Chirur Berlin 1900; 62: 147.
Galer BS, Schwartz L, Allen RJ . Complex regional pain syndromes type I: reflex sympathetic dystrophy and type II: causalgia. In: Loeser JD, Butler SH, Chapman CR, Turk DC (eds). Bonica's Management of Pain. 3rd edn. Lippincott Williams & Wilkins: Philadelphia, PA 2000.
Wasner G, Schattschneider J, Binder A, Baron R . Complex regional pain syndrome – diagnostic, mechanisms, CNS involvement and therapy. Spinal Cord 2003; 41: 61–75.
National Institute of Neurological Disorders and Stroke. N1H Publication No. 04-4173. November 2003.
Harden RN et al. Complex regional pain syndrome: are the IASP diagnostic criteria valid and sufficiently comprehensive? Pain 1999; 83: 211–219.
Schwartzman RJ, Popescu A . Reflex sympathetic dystrophy. Curr Rheumatol Rep 2002; 4: 165–169.
Janig W, Baron R . Complex regional pain syndrome: mystery explained? Lancet Neurol 2003; 2: 687–697.
van de Vusse AC, Stomp-van den Berg SG, de Vet HC, Weber WE . Interobserver reliability of diagnosis in patients with complex regional pain syndrome. Eur J Pain 2003; 7: 259–265.
Eisenberg E, Melamed E . Can complex regional pain syndrome be painless? Pain 2003; 106: 263–267.
Greene A. http://www.nlm.nih.gov/medlineplus/ency/article/007184.htm.
Merskey H, Bogduk N . Classification of Chronic Pain: Descriptions of Chronic Pain Syndromes and Definitions of Pain Terms. 2nd edn. IASP Press: Seattle 1994.
Nicholson B, Verma S . Comorbidities in chronic neuropathic pain. Pain Med 2004; 5 (suppl 1): S9.
Singh MK, Patel J, Gallagher RM . Chronic pain syndrome. http://www.emedicine.com/pmr/topic32.htm#section~author_information.
Department of Labor and Industries. Medical treatment guidelines. Washington State Department of Labor and Industries: Washington State 1999 pp 1–19.
Covington EC . Psychogenic pain – what it means, why it does not exist and how to diagnose it. Pain Med 2000; 1: 287–294.
Weitz SE, Witt PH, Greenfield DP . Treatment of chronic pain syndrome. New Jersey Med 2000; 97: 63–67.
Crook J, Rideout E, Browne G . The prevalence of pain complaints in a general population. Pain 1984; 18: 299–314.
Oakes Marilyn T Certified Pain Practitioner. Countering Chronic Pain myths. http://www.oakes.org/webdoc5.htm.
Fargas-Babjak A . Acupuncture, transcutaneous electrical nerve stimulation and laser therapy in chronic pain. Clin J Pain 2001; 17 (4 Suppl): S105–S113.
Portenoy RK . Cancer pain: pathophysiology and syndromes. Lancet 1992; 339: 1026.
Bigos SJ et al. A prospective study of work perceptions and psycho-social factors affecting the report of back injury. Spine 1991; 16: l–6.
Chang JT, Szczyglinski JA, King SA . A case of malingering: feigning a painful disorder in the presence of true medical illness. Pain Med 2000; 3: 280–282.
Drukteinis AM . Chronic pain in litigation New England psychodiagnostics. http://www.psychlaw.com/nep/chronic.htm.
Merskey H, Bogduk N (eds). IASP Task Force on Taxonomy. IASP Press: Seattle 1994; 222pp.