Abstract
Study design:
Prospective study of 100 consecutive patients.
Objective:
To evaluate the diagnostic usefulness of the urinary tract (KUB) radiograph routinely performed as part of spinal injury patient urinary tract screening with ultrasound (US) and the KUB radiograph.
Setting:
Orthopaedic and District General Hospital with spinal injuries unit, UK.
Methods:
Prospective study of the urinary tract of 100 consecutive routine follow-up spinal injury patients with KUB (kidneys, ureters, bladder) radiograph and US of the urinary tract. The percentage of the visualised area of kidneys and urinary bladder and relevant abnormal findings were recorded. Relevant patient history was recorded.
Results:
In all, 80 men 20 women were examined (average age 46 years, average time since injury 11 years). A total of 199 kidneys and 99 urinary bladders were examined. On average, less than 50% of the renal area and about 70–75% of the urinary bladder area were visualised. Five patients had renal stones identified on the KUB radiograph, and of these two were seen on US. There were no stones seen on US only. The patient history was not helpful to identify patients with renal stones. Significant further renal abnormalities were identified with US in 14 patients, and with the KUB radiograph in 0 patients. Significant urinary bladder abnormalities were identified with US in 20 patients, and with the KUB radiograph in 0 patients.
Conclusion:
On average, less than 50% of the kidney area is visualised on the KUB due to overlying bowel markings making the KUB radiograph a poor tool to assess the kidneys. The KUB radiograph and US are poor tools to assess urinary tract stones. In the absence of a therapeutic consequence, the KUB radiograph does not seem justified in the routine follow-up of the urinary tract in spinal injury patients.
Similar content being viewed by others
Introduction
Spinal injury patients with neurological deficit have the potential to develop urinary tract problems, which can go undetected clinically till late in the disease due to the impaired sensory of spinal injury patients. Especially, pyelonephritis, vesicoureteral reflux, hydronephrosis (due to reflux or impaired bladder emptying), stone formation and amyloidosis can damage the kidney and ultimately lead to renal insufficiency. Monitoring of the urinary tract and early intervention (such as spincterotomy or catheterization) can prevent life-threatening complications and significantly increase life expectancy.1, 2, 3, 4, 5 There is no agreed protocol for the follow-up imaging, but it is generally agreed that micturating cystourography, intravenous urography, KUB radiography, isotope studies and ultrasound (US) of the urinary tract all have a role.3, 4, 6, 7, 8, 9
In our institution, the KUB radiograph and urinary tract US are performed at the same sitting in the X-ray room to enhance patient care, but this decreases patient throughput. Furthermore, young patients are exposed to a potentially significant lifetime radiation dose. In addition, the KUB does not add useful information if the area in question is obscured by bowel markings.
This study was performed to evaluate the diagnostic usefulness of the KUB radiograph routinely performed as part of spinal injury patient urinary tract screening with US and the KUB radiograph.
Materials and methods
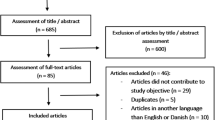
In this prospective study, 100 consecutive spinal injury patients attending for routine follow-up imaging of the urinary tract underwent a KUB radiograph and US. This represents the routine protocol in our institution (after initial assessment with i.v. urography and micturating vesicourograms, isotope studies when required) in the follow-up of asymptomatic patients. US was performed by a consultant radiologist or a senior registrar after the radiographs had been viewed.
On the radiograph, the percentages of visualised kidney and bladder were categorised as 0–25, 25–50, 50–75 and 75–100%. If less than 100% was visualised, the cause for nonvisualisation was recorded. Pathological findings were recorded.
The patient then underwent US examination. Any abnormalities, duration, severity (Frankel classification) and level of injury were recorded and a history of urinary tract problems, was taken, specifically whether there had been any urinary tract problems since the last examination. The method of urinary drainage was recorded.
Results
Of the 100 patients included in the study, 80 were male and 20 were female. The average age was 46 years and the average time since spinal injury was 11 years. One patient had undergone previous unilateral nephrectomy, and therefore 199 kidneys were examined.
The percentage area of kidney and bladder visualised is presented in Table 1. On average, less than 50% of the renal area was visualised (Figure 1) and about 70–75% of the urinary bladder area.
Clinically asymptomatic female patients. 18y at time of the first KUB radiograph (Figure 1a). Left-sided renal stones are seen (arrows). The majority of the left renal outline can be identified. On 1 year follow-up (Figure 1b), the left renal area is largely obscured, and the renal stones are no longer visualised
Nonvisualisation of renal areas was always due to overlying bowel markings. Nonvisualisation of the bladder was mainly due to bowel markings, but there was one case of a cystectomy and on one occasion the bladder was empty on examination.
There were five patients with renal stones identified on the KUB radiograph. In three patients, these stones were also identified on US, in two patients the stones could not be identified on US.
Of the two patients with renal stones not identified on US, one was clinically asymptomatic and emptied the bladder spontaneously, although with significant post micturitional volume; the other suffered from recurrent urinary tract infections (UTI) and emptied the bladder involuntarily by condom drainage.
In the three patients with renal stones seen on US, a nonfunctioning kidney was present in one case and occasional (one per year) UTI in the other two cases. The patient with known nonfunctioning kidney demonstrated a shrunken and distorted kidney on US with a staghorn calculus; urine drainage was via an indwelling urinary bladder catheter. The other two patients with renal stones identified on KUB radiograph and US emptied their bladders via intermittent self catheterisation, in one of the patients mild hydronephrosis was seen. Apart from the patient with incomplete bladder emptying, none of these patients had a urinary bladder wall abnormality.
US identified significant renal abnormalities in a further 14 patients. There were seven patients with renal scarring in eight kidneys. There were five patients with hydronephrosis in six kidneys; all cases were mild to moderate. There were two patients with a small kidney with thinned cortex.
US identified a number of other abnormalities. There was one patient with a duplex renal collecting system, one case of nephrectomy, one case of adrenal myolipoma, one situs inversus, one case of abnormally high echogenicity of the liver and two cases of gallstones. In one of these an additional gallbladder polyp was seen. One of the cases of gallstones was also identified on the KUB; all other abnormalities were not seen on the radiographs.
Abnormalities of the urinary bladder were seen in 20 cases. A total of 19 cases showed evidence of bladder wall hypertrophy, and one case of incomplete bladder emptying. There was one case of previous cystectomy and a neobladder. KUB did not identify any of these abnormalities.
Therefore, apart from the renal stones and one patient with gallstones, KUB did not identify any of the other abnormalities seen on US.
Discussion
On average, the visualised area of the kidneys on the KUB radiograph was less than 50%. Limited visualisation was always due to bowel markings. This has been recognised as a problem by a number of authors particularly in spinal injury patients,3, 4, 6 although it had not been quantified yet. The urinary bladder was relatively better visualised, approximately to 70–75%. Apart from five cases of renal stones and one case of gallstones, the KUB did not provide any useful information. These findings are in keeping with the findings of other authors.3, 4
US of the urinary tract demonstrated renal stones in three cases, missing two cases and other significant change to the kidney was seen in 14 cases. There were seven further cases with incidental sonographic abnormalities of the abdomen or kidneys. The ability of renal US to diagnose renal abnormalities and incidental findings has been well described previously.3, 4, 6, 10 In the urinary bladder abnormal findings were made in 20 cases, none of which were visualised on the radiographs.
The incidence of renal stones in spinal injury patients in this study was 5% and therefore higher than quoted by Kohli et al10 (about 1.3%) and lower than quoted by Rao et al (about 11%) or Chagnon et al (about 10%).6 In the general population of the UK, renal stones occur in about 3%.11
The previous study of Rao et al3 and Chagnon et al6 compared renal US and intravenous urography (IVU). Rao found that of 23 cases of renal calculi (in 202 patients), 18 were demonstrated by US and 20 by IVU with two false positive by US. Chagnon interestingly found that of 10 cases of renal calculi (in 50 patients), all 10 were seen on US against only eight of 10 with IVU. The study presented here found no case of renal stones seen only on US and not on KUB radiograph and in two patients, stones were seen only on the KUB radiograph but not on US. Knowing the result of the KUB radiograph when performing the renal US should have eased recognition of renal stones. The two cases where renal stones could not be identified even though they were demonstrated on the KUB radiograph emphasise that US is an imperfect tool for the diagnosis of renal stones.
Studies in the normal population have found that for the detection of renal calculi compared to IVU and the KUB radiograph, the sensitivity of US is about 37–68%; compared to CT the sensitivity decreases to about 24%.12 Similarly using CT as reference, KUB diagnoses 45–58% of renal stones.13
The previous, fairly small study of Brandt et al4 comparing renal US with IVU found no abnormality on IVU that was not also seen on US and US found additional abnormalities compared to the IVU. Solely for assessment of the ureters, IVU was felt to be superior. The latter view is not shared by Chagnon et al,6 who found US generally superior compared to IVU including the assessment of the ureters; however, some pathologies were not demonstrated on US.
Our study and the previous work of Rao et al3 and Morcos and Thomas7 suggest that some renal stones will be missed if the KUB is omitted from the routine follow-up of the urinary tract of spinal injury patients. Clinical symptoms or rather lack of clinical symptoms during the interval between examination was neither a reliable indicator to exclude renal pathology nor was spontaneous, controlled bladder emptying as the case of renal stones in an asymptomatic patient with controlled spontaneous bladder emptying demonstrates. In this patient, abnormal large residual bladder volume was found to be present.
However, as other studies suggest, KUB will miss approximately half of all renal calculi in the normal population. It is to be expected that this percentage is even higher in spinal injury patients where the renal outline is often markedly obscured. Four of the patients identified to have renal stones in this series did not undergo any treatment for renal stones, and one patient did not attend further but a urological opinion was suggested.
If the presence of renal stones does instigate treatment, then the KUB radiograph is a poor examination with only about 50% sensitivity,13 and if of no therapeutic consequence the radiation exposure by KUB is not justified.
Conclusion
On average, less than 50% of the kidney area is visualised on the KUB due to overlying bowel markings, making the KUB a poor tool to assess the kidneys. The KUB radiograph and US are poor tools to assess urinary tract stones. In the absence of a therapeutic consequence, the KUB radiograph does not seem justified in the routine follow-up of the urinary tract in spinal injury patients.
References
Scher AT . Changes in the upper urinary tract as demonstrated on intravenous pyelography and micturating cysto-urethrography in patients with spinal cord injury. Paraplegia 1975; 13: 157–161.
Lamid S . Long-term follow-up of spinal cord injury patients with vesicoureteral reflux. Paraplegia 1988; 26: 27–34.
Rao KG, Hackler RH, Woodlief RM, Ozer MN, Fields WR . Real-time renal sonography in spinal cord injury patients: prospective comparison with excretory urography. J Urol 1986; 135: 72–77.
Brandt TD, Neiman HL, Calenoff L, Greenberg M, Kaplan PE, Nanninga JB . Ultrasound evaluation of the urinary system in spinal-cord-injury patients. Radiology 1981; 141: 473–477.
Killorin W, Gray M, Bennett JK, Green BG . The value of urodynamics and bladder management in predicting upper urinary tract complications in male spinal cord injury patients. Paraplegia 1992; 30: 437–441.
Chagnon S, Vallee C, Laissy JP, Blery M . Ultrasonic evaluation of the urinary tract in patients with spinal cord injuries. Systematic comparison with intravenous urography in 50 cases. J Radiol 1985; 66: 801–806.
Morcos SK, Thomas DG . A comparison of real-time ultrasonography with intravenous urography in the follow-up of patients with spinal cord injury. Clin Radiol 1988; 39: 49–50.
Russell CD, Dubovsky EV . Reproducibility of single-sample clearance of 99mTc-mercaptoacetyltriglycine and 131I-orthoiodohippurate. J Nucl Med 1999; 40: 1122–1124.
Klingensmith III WC et al. Technetium-99m-MAG3 renal studies in spinal cord injury patients: normal range, reproducibility, and change as a function of duration and level of injury. Spinal Cord 1996; 34: 338–345.
Kohli A, Lamid S . Risk factors for renal stone formation in patients with spinal cord injury. Br J Urol 1986; 58: 588–591.
Kellet MJ . Calculi and urothelial disease. In: Grainger RG, Allison DJ, (eds) Diagnostic Radiology, 3rd edn. Churchill-Livingstone: New York 1997 pp 1391–1393.
Fowler KA, Locken JA, Duchesne JH, Williamson MR . US for detecting renal calculi with nonenhanced CT as a reference standard. Radiology 2002; 222: 109–113.
Sandhu C, Anson KM, Patel U . Urinary tract stones – Part I: role of radiological imaging in diagnosis and treatment planning. Clin Radiol 2003; 58: 415–421.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Tins, B., Teo, HG., Popuri, R. et al. Follow-up imaging of the urinary tract in spinal injury patients: Is a KUB necessary with every ultrasound?. Spinal Cord 43, 219–222 (2005). https://doi.org/10.1038/sj.sc.3101691
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101691