Abstract
Study Design:
Electromyographic study in complete and incomplete spinal cord injury (SCI).
Objective:
To examine the changes in the pattern of reciprocal inhibition between agonist and antagonist muscles in SCI.
Settings:
Sensory Motor Performance Program, Rehabilitation Institute of Chicago, IL, USA.
Methods:
Tendon taps were delivered manually with an instrumented hammer to the tendons of the tibialis anterior and soleus muscle in positions of full-ankle dorsiflexion and plantarflexion in eight subjects with complete SCI and eight subjects with incomplete SCI. Electromyographic activity (EMG) was recorded from ankle dorsiflexor and plantarflexor muscles. Tapping force was also recorded by a force sensor mounted to the tendon hammer, indicating the stimulus onset. Measures of reflex EMG magnitude and reflex latency were obtained for both agonist and antagonist muscles. The ratio of antagonist to agonist EMG was computed based on normalized EMG.
Results:
Substantial reflex responses occurred in both the stretched muscle and in its antagonist. The reflex in antagonist, which we term ‘reciprocal facilitation (RF)’, was most evident in subjects with incomplete SCI. The magnitude of RF was consistently greater than reflex responses in agonist muscles under all test conditions. The latency of the RF was comparable to that of monosynaptic reflex response.
Conclusions:
Following SCI, reciprocal organization of segmental reflexes at the ankle is often partially or completely suppressed, allowing reflex activation in antagonist muscles to be manifested. Possible mechanisms underlying these changes in neural organization are discussed.
Sponsorship:
This study was supported by Spinal Cord Research Foundation, the Paralyzed Veterans of America.
Similar content being viewed by others
Introduction
Following a cerebral motor or spinal lesion, the interruption of descending spinal pathways results in fundamental changes in the behavior of several spinal segmental circuits. One of the resulting outcomes is that reflex activation is observable in antagonist muscles.1,2,3,4,5
In patients with central nervous system disorders of early onset, it was previously shown that taps to the Achilles tendon and/or passive rotation of the ankle joint elicited electromyographic (EMG) responses in both agonist and antagonist muscles.3,4 These responses were especially pronounced in cerebral palsy. The altered reflex relationship between agonist and anta-gonist muscles was labeled ‘reciprocal excitation’ by the investigators. The pattern of ‘reciprocal excitation’ is a reversal of the well-established pattern – reciprocal inhibition, between a pair of agonist and antagonist muscles in the limbs.6
Using H-reflex technique, several investigators1,2,5 have reported that reciprocal inhibition is altered in patients with spasticity. Boorman et al1 compared the ability to suppress antagonist soleus H reflexes between control subjects and patients with spinal spasticity, and found that spastic patients showed reduced reciprocal inhibition. Suppression of reciprocal inhibition was also demonstrated in leg muscles of spastic patients with multiple sclerosis or hemiplegia.2,5
There are shared clinical manifestations among spastic conditions: cerebral palsy, hemiplegia, multiple sclerosis and spinal cord injury (SCI). However, little attention has been focused on patterns of reciprocal inhibition in SCI. The purpose of the present study was to explore whether SCI induced changes in the reciprocal relationship of reflex behaviors between agonist and antagonist muscles of the lower limbs. We examined these possibilities by investigating the relationship between reflexively induced agonist and antagonist muscle activity in response to tendon taps manually delivered to the ankle muscle tendons of individuals with SCI.
Methods
Subjects
Our subject population included eight adults with a complete SCI and eight adults with an incomplete SCI. Table 1 characterizes subjects' clinical presentation, including an impairment scale assessed by International standards for Neurological and Functional Classification of Spinal Cord Injury of the American Spinal Injury Association (ASIA),7 the modified Ashworth scale8 and medication. All subjects gave their informed consent prior to their participation. Experimental procedures were approved by the Institutional Review Board of Northwestern University, IL, USA, and were conducted in accord with the Helsinki Declaration of 1975.
Inclusion and exclusionary criteria
Inclusion criteria for the subjects were based upon: (1) age of 18 years or older; (2) an SCI history of at least 6 months; and (3) clinical signs of spasticity in one or both legs.
Exclusionary criteria included: (1) sitting tolerance less than 2 h; (2) a history of lower extremity fractures, skin breakdown, or an episode of autonomic dysreflexia within 2 weeks prior to participation; or (3) inability to give informed consent, understand training instructions or give adequate feedback.
No weaning from antispasticity medication was attempted. Subjects continued ongoing therapy and rehabilitation programs.
Experimental procedures
Each subject was seated upright on a custom-designed chair, with the trunk strapped to the chair. The subject's thigh remained horizontal and the knee joint was kept flexed at approximately 60°. The ankle joint was positioned, held and supported by one hand of the experimenter. Maintenance of a stable ankle position could therefore be readily achieved.
In order to examine how antagonist muscles respond to a stretch at both maximal length and minimal length, the ankle joint was positioned in either full dorsiflexion or plantarflexion and taps were then applied to either the tibialis anterior or soleus tendon, that is, the Achilles tendon. Thus, four experimental conditions were generated: (I) tibialis anterior (TA) tendon tapped under full dorsiflexion; (II) TA tendon tapped under full plantarflexion; (III) soleus tendon tapped under full dorsi-flexion; and (IV) soleus tendon tapped under full plantarflexion.
Each subject was instructed to relax completely and asked not to react to the taps. To identify the particular spot at which the tendon hammer should be applied, various positions along the tendon were tested until the resultant reflex response was consistently elicited in the agonist muscle. A self-adhesive rubber pad was then mounted at the spot that was identified. The pad was expected to transmit the tapping force more evenly to the tendon. To determine the tapping intensity delivered, the tapping force was increased progressively until an identifiable response was elicited in the agonist muscle. The tendon was then tapped at that level as closely as possible.
An instrumented tendon hammer, with a force sensor (Kistler Instrument Corp., NY, USA) mounted at the tapping site, recorded the tapping force applied to each tendon. Tapping force was used as an indicator of the stimulus onset and tapping strength. In all, 15 taps were delivered in each trial. Three trials were repeated in each condition, as determined by the tendon being tapped and ankle joint position. A 2-min interval was arranged between two consecutive trials.
EMG recordings
EMG activity was recorded from TA, medial gastrocnemius (MG) and soleus (SOL) muscles, using differential surface electrodes (DelSys Incorporated, MA, USA) with an interelectrode distance of 10 mm. Optimal electrode location was determined by following the guidelines of Perotto9 and confirmed with appropriate test maneuvers. For example, the electrode for TA muscle recording was positioned at the point of intersection 8 cm below the tibial tuberosity and 2 cm lateral to the tibial crest. Electrode location was confirmed with performance of ankle dorsiflexion. Prior to the placement of electrodes, the skin area chosen for electrode application was gently abraded using skin preparation pad, and then cleaned with alcohol in order to lower the electrical impedance. EMG signals were amplified ( × 10 K) and low-pass filtered (200 Hz) before being digitized at 500 Hz per EMG channel. Force signals, used to monitor the tapping intensity and the stimulus timing onset, were recorded simultaneously at the same sampling frequency.
Data analyses
Data were analyzed off-line using MATLAB software. EMG signals were full-wave rectified. Reflex magnitude and latency were calculated for agonist and antagonist muscles under each of the four conditions. Stimulus onset was determined as the onset of the sharply rising phase of the force trace, which was always clearly identifiable. Reflex onset was defined as the time at which the EMG amplitude first exceeded 95% confidence interval of the background muscle activity level (ie a 100 ms EMG average prior to the stimulus onset). Thus, reflex latency was the duration from stimulus onset to reflex onset. Reflex offset was defined following the same rule used to identify reflex onset, but based on the falling phase. Reflex duration covered window period from reflex onset to offset. Stimulus onset was measured for each tap, and EMG reflex onset was determined in individual muscles, separately.
The magnitudes of reciprocal facilitation (RF) and reflex response were computed as the integral of the resultant EMG response between reflex onset and offset, after subtraction of the background EMG activity level. It is the equivalent of the area enveloped by the EMG trace and background activity level within reflex duration. No EMG integral was computed for the taps that did not elicit an identifiable RF in antagonist.
The percentage of taps showing RF was computed. It was defined as number of taps evoking RF divided by the total number of taps (45) under each test condition for each subject. To compare RF of antagonist muscle with the reflex response of agonist muscle, EMG responses of agonist and antagonist muscles were normalized by dividing by the mean level of background activity, for taps eliciting identifiable RF. Mean ratios (normalized RF integral divided by normalized agonist reflex integral) were calculated for each of four conditions in all subjects who exhibited RF responses.
Individual Pearson's correlation coefficients were assessed for each test condition between RF and degree of spasticity, lesion level, time postinjury, and ASIA classification scale. Student's t-tests were performed to compare reflex latencies between agonist and antagonist muscles.
Results
Experiments were conducted on two groups of subjects with SCI: eight subjects with a complete injury and eight with an incomplete injury. Our overall findings were that RF occurred in six of eight subjects with an incomplete injury and in two of eight subjects with complete SCI. This phenomenon was most evident in test condition of tapping SOL tendon with ankle full dorsiflexion (Condition III) for both subject groups.
Table 2 shows the summary data for all participating subjects, with the proportion of taps generating an identifiable RF response in the antagonist, presented as a percentage of the total number of taps delivered. RF occurred in 12 instances in the incomplete SCI group but only three instances in the complete SCI group.
In addition, stratification of our data according to spasticity level, to lesion level, to time postinjury, and to ASIA classification scale showed that there was a limited correlation (r=0.47) between percentage of RF occurrences and spasticity level, and a casual link between RF and the ASIA scale, in test condition III only. But the correlations between the RF and the lesion level, and time postinjury were low.
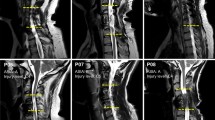
Spatial feature of RF elicited by tendon taps in SCI
Figure 1 shows an example of averaged EMG responses in antagonist muscles, resulting from tendon taps applied sequentially to soleus or TA muscle tendon of a subject (#9) with an incomplete SCI. Figure 1a demonstrates that a reflex response is observed not only in triceps surae, the muscle group being tapped, but also in the antagonist muscle, TA. Reciprocal facilitation for the antagonist muscle, TA, is 4089.54±661.14 millivolt*millisecond (mV*ms) expressed as mean±SEM (standard error of the mean), whereas the reflex response is 3602.82±571.20 mV*ms for MG and 1763.24±204.62 mV*ms for SOL.
Averaged EMG traces in three leg muscles in a subject (#9) with an incomplete SCI. (a) Average of 15 EMG sweeps when SOL tendon was tapped with the ankle dorsiflexed. (b) Average of nine EMG sweeps when TA tendon was tapped with the ankle dorsiflexed. Stimuli were applied at time zero, as indicated by an arrow S. Letter R shows the reflex onset in the muscle being tapped. Shadowed areas schematically illustrate measurements of reflex EMG integrals for both agonist and antagonist muscles
Figure 1b shows that when the TA tendon was tapped, a strong RF was recorded in the triceps surae. The integral of EMG response elicited in MG is 1223.04±224.02 mV*ms (mean±SEM), which is higher than that of the muscle being tapped (1079.16±212.66 mV*ms for TA). In both cases, EMG response is greater in the antagonist muscle than in the muscle receiving the tendon tap.
Figure 2 presents mean ratios of normalized RF to reflex responses of the agonist muscle in all subjects for both complete (Figure 2a) and incomplete (Figure 2b) SCI groups under four test conditions. Our results indicate that RFs were consistently stronger than reflex responses of agonist muscle under all test conditions in either subject group. Between the two groups, higher ratios were found in incomplete SCI group. Among all test conditions and subject groups, the highest ratio was associated with the incomplete SCI group in test Condition III.
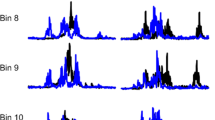
Temporal feature of RF elicited by tendon taps in SCI
The latency of RF ranged from 32 to 46 ms in the TA muscle when the SOL tendon was tapped, and from 40 and 52 ms in the SOL when the TA tendon was tapped. Figure 3 illustrates mean latency of RF in muscles SOL and TA, providing a comparison between the latency of reflex responses in muscles TA and SOL, when TA was tapped (I and II) and when SOL was tapped (III and IV). In test conditions I and II, the latency of RF was significantly (P<0.05) longer than latency of the reflex response.
Mean latency of RF (shadow bars) and reflex latency (blank bars) of agonist muscle in all subjects when TA tendon was tapped (I/II) and when SOL tendon was tapped (III/IV). Under test conditions I and II, the latency of RF was significantly (P<0.05) longer than the latency of reflex response in agonist muscle. Error bar: standard error of the mean. *Statistically significant P<0.05
Discussion
The main finding of this study is that the relationship between agonist and antagonist muscle activation is altered in SCI subjects. This alteration is reflected largely in the observation that the reflex response to muscle tap was also recorded in antagonistic muscle.
In this study, surface electrodes were used to record EMG activity from leg muscles. Therefore, EMG crosstalk was carefully considered with respect to data capture, information extraction and data interpretation. There has been a considerable controversy over whether the ‘reciprocal excitatory reflex’ recorded in the TA muscle truly represents a clinical sign of the neural response in the TA, or whether it was a spurious result of volume conduction.3,4,10 The arguments presented in favor of the latter were based upon: (1) the size of the SOL H-reflex was always significantly greater than that of the TA response; (2) a concomitant response in TA was reported to have a comparable reflex latency with SOL.10,11 Arguments against the proposition that reciprocal excitation can be accounted for by volume conduction were presented by Myklebust and Gottlieb.12
Results presented in this study support the view that the reflex response arising in the antagonist muscle is genuine. The distinctive features favoring such an RF response are reflected in both spatial and temporal parameters.
Firstly, the magnitude of RF was consistently greater than the magnitude of the reflex response in the muscles being tapped, whereas a key characteristic of crosstalk is that the spurious EMG records should show a significant reduction in amplitude, compared to the actual source.13 This reduction is broadly proportional to the distance from the detection surface to the active muscle fibers.
Secondly, in our results, the latency of the response in antagonist muscles was significantly longer than the latency of the response in agonist muscles in some test conditions (I and II), and the latency of the response in antagonist muscles was shorter than the latency of the response in agonist muscles in other test conditions. Again, this is inconsistent with passive signal propa-gation. The combination of these features provides convincing evidence that EMG crosstalk due to volume conduction can be ruled out in the present study.
Mechanisms underlying RF of antagonist muscles in SCI
There are several possible mechanisms to account for the manifestation of RF. Firstly, the most straight-forward one is a disruption of the descending pathways exciting the spinal interneurons that mediate the disynaptic reciprocal Ia inhibition of motoneurons.2,5,14,15 Ia inhibitory interneurons receive excitatory input from many descending systems, including corticospinal, rubrospinal and vestibulospinal tracts. In the event of spinal or brain lesions, this interruption could result in a reduction of excitability of these interneurons, producing decreased inhibition of motoneurons innervating the antagonist muscle.
The Ia inhibitory pathway has been widely investigated in both healthy and spastic populations, mainly using the H-reflex approach.1,2,5,16,17 Crone et al2 studied the soleus H-reflex in a large number of healthy subjects and in subjects with multiple sclerosis. They found that disynaptic Ia reciprocal inhibition was depressed in spastic patients. They suggested that the lack of Ia reciprocal inhibition is a result of an impaired descending control of the Ia inhibitory interneurons.
Yanagisawa and Tanaka5 examined reciprocal reflex activities in capsular hemiplegia and spastic paresis resulting from spinal cord lesions, including tumors, multiple sclerosis and other myelopathies. They also reported that the reciprocal Ia inhibition from the peroneal nerve to the triceps surae was weak. In contrast, there was a strong Ia inhibition from tibial nerve excitation to the TA muscle. Such an imbalance of reciprocal Ia inhibition between ankle dorsiflexor and plantarflexor was striking in capsular hemiplegia, whereas the phenomenon was not obvious in the spinal cord lesions.
Our results show that the prevalence of RF is greater in the TA muscle, indicating that Ia inhibition from SOL onto TA was weaker than from TA onto SOL. There are two possible explanations for the discrepancy between our study and the study reported by Yanagisawa and Tanaka.5 The present study was conducted in subjects with SCI, whereas the subject population in the previous study included individuals with capsular hemiplegia or spastic paresis due to nontraumatic spinal lesions. In addition, the techniques employed by the two studies also differed, although the mediation of neural circuits is essentially the same for tendon tap and H-reflex.
In agreement with the earlier studies, our findings in individuals with SCI suggest that Ia inhibitory mecha-nisms are likely to be disrupted in SCI, due to the disruption in descending commands.
Secondly, the pathways mediating the reflex circuits could well be abnormal resulting from a process of collateral sprouting of new connections from the intact nerve fibers. Evidence accumulated from experimental work has shown that, following a partial lesion in the nervous system, terminals with injured fibers degenerate and intact afferent fibers progressively sprout collaterally to occupy the evacuated regions.18,19,20,21,22
Reorganization of the nervous system comprises degenerative and regenerative changes in the afferent neurons distal to the lesion sites, disorganization and reorganization of the whole network, and ultimately the new growth.22,23,24,25,26,27,28,29 It is suggested that the process of degeneration, reorganization and sprouting results in an alteration of the ‘synaptic zone’, which is the very element of the nervous system transmitting information from one neuron to another, forming the basis of the reflex behavior.22,25 Furthermore, Merrill and Wall30 demonstrated that unmasking of synapses occurred where cells lost their normal inputs. Gradually, those cells developed novel inputs and began to respond to them. Therefore, unmasking may also contribute to the alteration of the synaptic zone.
Consequently, the pattern of the reflex responses is changed as a result of the alteration of the synaptic zone, as extensively and profoundly discussed by Illis.22,23,24,25,26,27 Besides, sprouting of the intact fibers and the unmasking of synapses, producing an altered nervous system, are considered to be factors responsible for clinical disturbances, including spasticity, following brain or spinal lesions.31,32,33,34
Following a partial lesion, the progress of the changes mentioned earlier may last several months before a final, stable equilibrium is reached. In our study, all subjects with SCI were at least 6-month postinjury, as shown in Table 1. The latency of RF suggests that RF is mediated by oligosynaptic short-latency pathways involving the Ia muscle afferents. We speculate that RF is mediated by abnormal reflex pathways arising through afferent sprouting, and that characteristics of the new afferent connections might induce some reflex delay in antagonist. There is other evidence that supports the existence of a sprouting mechanism. It was recently reported that electrical stimulation of a mixed peripheral nerve in the lower limb could evoke short latency, bilateral motor responses in the muscles of distal upper limbs in individuals with severe injuries to the cervical spinal cord.35,36 Such motor responses have been termed interlimb reflexes. Their findings showed that these interlimb reflexes did not appear until at least 8–9 months after SCI.37 They concluded that the regenerative sprouting best explained the appearance of interlimb reflexes in subjects with severe SCI.34,36
Thirdly, what remains to be established is the source of the reciprocal facilitation. It is conceivable that RF is mediated by an existing excitatory pathway that becomes more potent after the spinal lesion. Appropriate short-latency interneuronal Ia excitatory pathways have been discovered in reduced animal models. For example, earlier studies in animal models38,39,40 showed that Ib afferent excitation (from Golgi tendon organs) can evoke disynaptic excitation of motoneurons to antagonists. Thus, the term ‘inverse myotatic reflex’ was introduced, since its reflex action is opposite to the reflex actions of group Ia afferents. They also found a considerable proportion of interneurons mediating the inverse actions to be coexcited by group Ia and Ib afferents.
Some supportive evidence favoring the participation of such pathways has also been provided in earlier human studies,3,4 although the study findings were contested on technical grounds.10 Specifically, these studies reported that a mechanical stimulus to a muscle tendon evoked a short-latency excitatory reflex in the antagonist leg muscles in cerebral palsy. The authors attributed their findings to developmentally mediated reorganization of excitatory projections to antagonist motoneurons in the spinal cord.
Differential impact of complete and incomplete SCI
There are several differential features between complete and incomplete SCI. In complete spinal lesions, there are almost no descending commands retained. Often, there is a primary challenge associated with the regeneration of the lesioned fibers to reconnect two stumps of the spinal cord, whereas, in cases of incomplete spinal lesions, some sensory and motor information can still pass via the largely intact spinal circuit that is partially interconnected by the undamaged nerve fibers.41 However, the transmitted sensori-motor information is often fragmentary or distorted due to the alteration of the synaptic zone,22,25,31,32 leading to clinical complications such as pain or spasticity. Little et al42 reported that patients with incomplete lesions were more severely affected by spasticity with respect to functional mobility, sleep and pain, when compared to patients with complete lesions. Consequently, they displayed decreased range of motion either directly due to hypertonus or indirectly due to hypertonus-induced contracture.
In this study, we observed that decreased reciprocal inhibition is more prevalent in the incomplete SCI group (six subjects with incomplete SCI versus two subjects with complete SCI), and thus is likely due to maladaptive change associated with incomplete spinal lesions.
Conclusions
We conclude that the disruption of the descending control of spinal interneurons mediating the reciprocal Ia inhibition of motoneurons plays an important role in the manifestation of RF after SCI. In addition, we speculate that regenerative sprouting mechanisms, arising from segmental afferent or interneuronal projections, also contribute to the RF responses observed in this study. There is a large body of evidence from animal studies that supports this assertion. Further, latent excitatory pathways may be responsible for the manifestation of RF in spinal lesions.
References
Boorman GI, Lee RG, Becker WJ, Windhorst UR . Impaired ‘natural reciprocal inhibition’ in patients with spasticity due to incomplete spinal cord injury. Electroencephalogr Clin Neurophysiol 1996; 101: 84–92.
Crone C, Nielsen J, Petersen N, Ballegaard M, Hultborn H . Disynaptic reciprocal inhibition of ankle extensors in spastic patients. Brain 1994; 117: 1161–1168.
Gottlieb GL, Myklebust BM, Penn RD, Agarwal GC . Reciprocal excitation of muscle antagonists by the primary afferent pathway. Exp Brain Res 1982; 46: 454–456.
Myklebust BM, Gottlieb GL, Penn RD, Agarwal GC . Reciprocal excitation of antagonistic muscles as a differentiating feature in spasticity. Ann Neurol 1982; 12: 367–374.
Yanagisawa N, Tanaka R . Reciprocal Ia inhibition in spastic paralysis in man. Electroencephalogr Clin Neurophysiol Suppl 1978; 34: 521–526.
Lloyd PD . Integrative pattern of excitation and inhibition in two-neuron reflex arcs. J Neurophysiol 1946; 9: 439–444.
Maynard FM et al. International standards for neurological and functional classification of spinal cord injury. Spinal Cord 1997; 35: 266–274.
Bohannon RW, Smith MS . Interrater reliability of a Modified Ashworth Scale of muscle spasticity. Phys Ther 1987; 67: 206–207.
Perotto AO . Anatomical Guide for the Electromyographer: The Limb and Trunk. Charles C Thomas: Springfield, IL, USA 199 pp 141–171.
Turker KS, Miles TS . Cross-talk from other muscles can contaminate EMG signals in reflex studies of the human leg. Neurosci Lett 1990; 111: 164–169.
Hutton RS, Roy RR, Edgerton VR . Coexistent Hoffmann reflexes in human leg muscles are commonly due to volume conduction. Exp Neurol 1988; 100: 265–273.
Myklebust BM, Gottlieb GL . Development of the stretch reflex in the newborn: reciprocal excitation and reflex irradiation. Child Dev 1993; 64: 1036–1045.
Loeb GE, Gans C . Electromyography for Experimentalists. The University of Chicago Press: Chicago USA 198 pp 88–94.
Crone C, Nielsen J . Central control of disynaptic reciprocal inhibition in humans. Acta Physiol Scand 1994; 152: 351–363.
Hultborn H, Illert M, Santini M . Convergence on interneurons mediating the reciprocal Ia inhibition of motoneurons. Acta Physiol Scand 1976; 96: 193–201, 351–367, 368–391.
Crone C, Hultborn H, Jespersen B, Nielsen J . Reciprocal Ia inhibition between ankle flexors and extensors in man. J Physiol 1987; 389: 163–185.
Schieppati M . The Hoffmann reflex: a means of assessing spinal reflex excitability and its descending control in man. Prog Neurobiol 1987; 28: 345–376.
Edds MV . Collateral nerve regeneration. Q Rev Biol 1953; 28: 260–276.
Murray JG, Thompson JW . The occurrence and function of collateral sprouting in the sympathetic nervous system of the cat. J Physiol 1957; 135: 133–162.
Liu CN, Chambers WW . Intraspinal sprouting of dorsal root axons. Arch Neurol Psychiatry 1958; 79: 46–61.
McCouch GP, Austin GM, Liu CN, Liu CY . Sprouting as a cause of spasticity. J Neurophysiol 1958; 21: 205–216.
Illis LS . Changes in spinal cord synapses and a possible explanation for spinal shock. Exp Neurol 1963; 8: 328–335.
Illis LS . Spinal cord synapses in the cat: the normal appearances by the light microscope. Brain 1964; 87: 543–554.
Illis LS . Spinal cord synapses in the cat: the reaction of the boutons termineaux at the motoneurone surface to experimental denervation. Brain 1964; 87: 555–572.
Illis LS . The motor neuron surface and spinal shock. In: Williams D (ed) Modern Trends in Neurology, vol 4. Butterworths: London 1967 pp 53–68.
Illis LS . Experimental model of regeneration in the central nervous system. I. Synaptic changes. Brain 1973; 96: 47–60.
Illis LS . Experimental model of regeneration in the central nervous system. II. The reaction of glia in the synaptic zone. Brain 1973; 96: 61–68.
Cameron AA, Cliffer KD, Dougherty PM, Garrison CJ, Willis WD, Carlton SM . Time course of degenerative and regenerative changes in the dorsal horn in a rat model of peripheral neuropathy. J Comp Neurol 1997; 379: 428–442.
Goldstein B, Little JW, Harris RM . Axonal sprouting following incomplete spinal cord injury: an experimental model. J Spinal Cord Med 1997; 20: 200–206.
Merrill EG, Wall PD . Plasticity of connection in the adult nervous system. In: Cotman CW (ed) Neuronal Plasticity. Raven Press: New York 1978 pp 97–111.
Illis LS . Rehabilitation following brain damage: some neurophysiological mechanisms. Determinants of recovery. Int Rehabil Med 1982; 4: 166–172.
Illis LS . Rehabilitation following brain damage: some neurophysiological mechanisms. The effects of repetitive stimulation in recovery from damage to the central nervous system. Int Rehabil Med 1982; 4: 178–184.
Rymer WZ, Katz RT . Mechanisms of spastic hypertonia. Phys Med Rehabil: State Art Rev 1994; 8: 441–454.
Steward O . Reorganization of neuronal connections following CNS trauma: principles and experimental paradigms. J Neurotrauma 1989; 6: 99–152.
Calancie B . Interlimb reflexes following cervical spinal cord injury in man. Exp Brain Res 1991; 85: 458–469.
Calancie B, Lutton S, Broton JG . Central nervous system plasticity after spinal cord injury in man: interlimb reflexes and the influence of cutaneous stimulation. Electroencephalogr Clin Neurophysiol 1996; 101: 304–315.
Calancie B, Broton JG . Evidence for CNS caudal to cervical spinal cord injury in man. Soc Neurosci Abstr 1992; 589: 14.
Jankowska E, Johannisson T, Lipski J . Common interneurones in reflex pathways from group Ia and Ib afferents of ankle extensors in the cat. J Physiol 1981; 310: 381–402.
Jankowska E, McCrea DA . Shared reflex pathways from Ib tendon organ afferents and Ia muscle spindle afferents in the cat. J Physiol 1983; 338: 99–111.
Lundberg A, Malmgren K, Schomburg ED . Cutaneous facilitation of transmission in reflex pathways from Ib afferents to motoneurones. J Physiol 1977; 265: 763–780.
Raineteau O, Schwab ME . Plasticity of motor systems after incomplete spinal cord injury. Nat Rev Neurosci 2001; 2: 263–273.
Little JW, Micklesen P, Umlauf R, Britell C . Lower extremity manifestations of spasticity in chronic spinal cord injury. Am J Phys Med Rehabil 1989; 68: 32–36.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Xia, R., Rymer, W. Reflex reciprocal facilitation of antagonist muscles in spinal cord injury. Spinal Cord 43, 14–21 (2005). https://doi.org/10.1038/sj.sc.3101656
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101656
Keywords
This article is cited by
-
Co-contraction of ankle muscle activity during quiet standing in individuals with incomplete spinal cord injury is associated with postural instability
Scientific Reports (2021)
-
Effect of tendon vibration during wide-pulse neuromuscular electrical stimulation (NMES) on muscle force production in people with spinal cord injury (SCI)
BMC Neurology (2018)
-
Effects of acute spinalization on neurons of postural networks
Scientific Reports (2016)
-
Co-contraction modifies the stretch reflex elicited in muscles shortened by a joint perturbation
Experimental Brain Research (2010)
-
Increases in muscle activity produced by vibration of the thigh muscles during locomotion in chronic human spinal cord injury
Experimental Brain Research (2009)