Abstract
Study design:
Case report.
Objective:
To report a rare complication following a stab injury to the upper cervical spine and cord.
Setting:
National spinal injury unit in a Scottish university teaching hospital.
Case report:
A 19-year-old male sustained a stab injury to his upper cervical spine, with a partial cord transection. After 5 months of rehabilitation, his condition deteriorated. CT scans showed hydrocephalus, which was treated by shunting. After shunting, the patient's condition improved but he remained tetraplegic requiring ventilatory support at night.
Conclusion:
Hydrocephalus as a late complication of a cervical spine injury is rare but should be considered if the condition of the patient with an upper cervical spine injury deteriorates. The likely mechanism of the hydrocephalus development is also discussed.
Similar content being viewed by others
Introduction
Hydrocephalus is a recognized complication of head injury. It has also been described following penetrating injuries to the brain stem.1 However, to our knowledge, hydrocephalus as a result of a spinal injury has not been reported. We report a patient who developed a severe hydrocephalus following a penetrating spinal injury.
Case history
A 19-year-old male was found with multiple stab injuries to face, neck and hand. He had a past medical history of multiple illicit substance abuse. At the time of admission, he was drowsy and could not move any limbs. After resuscitation, he opened his eyes spontaneously and he was able to speak but had difficulty breathing. There was no external evidence of head injury and he had a Glasgow coma score of nine since he did not have a motor response due to limb paralysis.
Clinical examination revealed unequal pupils, smaller on the left side. All other cranial nerves functioned normally. He had an ASIA2 motor score of zero as there was no muscle activity in the upper or lower limbs and he had diaphragmatic type ventilation.
He had an incomplete injury and had an ASIA impairment score of B as he had preservation of light-touch sensation over the L3,4,5 dermatomes of the left side and some sacral sensation and also had preserved ankle reflexes.
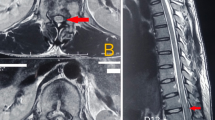
Plain radiographs of the cervical spine were normal, but the chest radiograph showed a raised hemidiaphragm on the right side. A magnetic resonance scan of the brain stem region showed partial transection of the cervical cord just above the craniovertebral junction with a thin line of hemorrhage at the transection and a larger clot just anterior to the transection level causing slight compression of the cord (Figure 1). Magnetic resonance angiography showed that there was no injury to the vertebral arteries.
He required intubation and ventilation shortly after admission. After 5 months on ventilatory support, his condition started to deteriorate with increased muscle spasm and dysreflexic episodes. He had two seizures, which presented as uncontrolled jerking movements of the head and neck during which the patient was unresponsive to any external stimulus. Computerized tomographic scans of the brain showed marked enlargement of all four ventricles.
The hydrocephalus was treated by insertion of a ventriculoperitoneal shunt. There were no further seizures and the general condition of the patient gradually stabilized. Over the next 3 months, his condition improved and he was partially weaned off ventilatory support.
At 6 years following the injury, the patient had recovered complete sensation in all four limbs with grade three power of the left upper limb and an ASIA motor score of 16. He still requires ventilator support at night but has full bladder sensation and control.
A repeat MRI (Figure 2) showed moderate hydrocephalus of the lateral and third ventricles despite shunting. There was no evidence of a syrinx and the residual 25% of the intact spinal cord and dura was clearly seen. Chest X-ray showed good expansion of both lungs and normal function of the right hemidiaphragm.
Discussion
Complete cord injury is seen in only about a fifth3 of the patients with stab injuries. The prognosis in those patients with complete injuries is the same as that for other spinal cord injuries, but in patients with incomplete cord injury the prognosis is good.3,4,5 Over 60% of patients with incomplete injuries will be able to walk independently or with minimal assistance.3
Late presentation6,7,8 of complications following spinal stab injury is rare and may occur due to retained foreign material4 (such as a portion of a weapon) or infection. Other late sequelae include myelomalacia4 or syringomyelia,9 which may lead to progressive neurological deterioration.
Hydrocephalus may be either communicating or noncommunicating. The noncommunicating type is usually the result of obstruction to flow due to congenital causes such as aqueduct stenosis or tumors. Communicating hydrocephalus is usually postinflammatory in origin and complicates acute or chronic meningitis or it may follow hemorrhage or trauma when blood in the cerebrospinal fluid (CSF) may degrade CSF absorption at the arachnoid villi. Hydrocephalus following head injury10 or injury to the brain stem1 is usually the communicating type and presents relatively early.
Hydrocephalus as a result of spinal pathology is rare, and has been reported with spinal tumors where the pathogenesis may be disruption11 of the CSF flow, impaired absorption due to elevated CSF protein, tumor infiltration into the basal cisterns and even compression12 of the spinal venous plexus by tumor.
In our patient, we consider that the pathogenesis may be related to the high level of the penetrating injury leading to blood from the site of injury (Figure 1) entering the basal cisterns and impairing the absorption of the CSF by the arachnoid villi over the hemispheres, hence leading to a communicating hydrocephalus. This is supported by the CT scans that showed a communicating type of hydrocephalus with dilation of the third, fourth and lateral ventricles and also due to the absence of any obvious pathology on CT or MRI scans that could lead to obstruction of CSF flow.
Conclusion
Hydrocephalus as a result of stab injury to the spine is an unusual complication and should be considered especially if there is delayed presentation of neurological symptoms such as an epileptic seizure or if there is spinal neurological deterioration.
References
Nathoo N, Boodhoo H, Nadvi SS, Naidoo SR, Gouws E . Trans-cranial brainstem stab injuries: a retrospective analysis of 17 patients. Neurosurgery 2000; 47: 1117–1122.
Maynard Jr FM et al. International standards for neurological and functional classification of spinal cord injury. Spinal Cord 1997; 35: 266–274.
Peacock WJ, Shrosbree RD, Key AG . A review of 450 stab-wounds of the spinal cord. S Afr Med J 1977; 51: 961–964.
Stab wounds of the spinal cord. In: Yashon D (ed). Spinal Injury, 2nd edn. Appleton-Century-Crofts: East Norwalk, CT 1986 (Chapter 14) pp 307–317.
Walters RL, Sie I, Adkins RH, Yakura JS . Motor recovery following spinal cord injury by stab wounds: a multicenter study. Paraplegia 1995; 33: 98–101.
Heary RF, Vaccaro AR, Mesa JJ, Balderston RA . Thoraco-lumbar infections in penetrating injuries to the spine. Orthop Clin North Am 1996; 27: 69–81.
Silvestro C, Cocito L, Pisani R . Delayed effects of a migrated foreign body (sewing needle) in the cervical spine: a case report. Spine 2001; 26: 578–579.
Velmahos GC, Degiannis E, Hart K, Souter I, Saadia R . Changing profiles in spinal cord injuries and risk factors influencing recovery after penetrating injuries. J Trauma 1995; 38: 334–337.
Williams B . Pathogenesis of posttraumatic syringomyelia. Br J Neurosurg 1992; 6: 517–520.
Garfield J . The cranium. In: Mann CV, Russell RCG (eds). Bailey and Love's Short Practice of Surgery, 21st edn. Chapman & Hall: London 1991 pp 538–595.
Rifkinson-Mann S, Wisoff J, Epstein F . The association of hydrocephalus with intramedullary spinal cord tumor: a series of 25 patients. Neurosurgery 1990; 27: 749–754.
Bland LI, McDonald JV . Hydrocephalus following spinal cord schwannoma resection. Arch Neurol 1992; 49: 882–885.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Joseph, G., Johnston, R., Fraser, M. et al. Delayed hydrocephalus as an unusual complication of a stab injury to the spine. Spinal Cord 43, 56–58 (2005). https://doi.org/10.1038/sj.sc.3101655
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101655
Keywords
This article is cited by
-
2008 ArgoSpine best poster award
ArgoSpine News & Journal (2008)