Abstract
Study design: Epidemiological follow-up study.
Objective: To examine the bladder-emptying methods at least 10 years after a traumatic spinal cord injury (SCI).
Setting: Clinic for Para- and Tetraplegia and Department of Urology, Rigshospitalet, Copenhagen University Hospital, Denmark.
Methods: Retrospective data collection from patient records and data collected with a follow-up questionnaire. The response rate was 84.6% corresponding to 236 SCI individuals, injured in 1956–1990. There were 82/18% male/female patients and 47/53% tetraplegic/paraplegic. Age at the time of follow-up was 50.5 years in mean (range 28–84). Years from time of injury were 24.1 years in mean (range 10–45).
Results: The use of clean intermittent catheterisation (CIC) rose from 11% at the initial discharge to 36% at the time of follow-up. The use of suprapubic tapping fell from 57 to 31% in the same period, while the use of Credé manoeuvre rose from 5 to 19%. During follow-up, 46% changed bladder-emptying method. The results showed the following trends in change of method: a high proportion of discontinuation in normal bladder emptying, suprapubic tapping and abdominal pressure and a high proportion of continuation when using CIC. 28% found their bladder-emptying method to be a problem; of these 58% were tetraplegic. Of the participants using CIC, 92% reported using hydrophilic-coated catheters.
Conclusions: Changing of bladder-emptying method among SCI individuals over time is common. CIC alone or in combination with another bladder-emptying method is the most frequently used method of bladder emptying.
Sponsorship: The study was carried out as part of the primary author's PhD-study, which was financed by Medicon Valley Academy and Coloplast A/S.
Similar content being viewed by others
Introduction
Individuals with a spinal cord injury (SCI) have a disability, which necessitates lifelong follow-up by specialists due to the risk of secondary complications.
The impaired bladder function incurs a risk of developing various urological complications, for example urinary tract infections, urinary stones, urinary incontinence and impaired renal function.
In a 15-year-follow-up study on bladder management,1 the following trends were seen during the period of observation: A large decline in the use of intermittent catheterisation for both genders, an increase in the use of condom-catheter drainage for men and an increased use of urethral indwelling catheter in women.
Another study describing the urological situation 5 years after SCI2 found a trend towards less intermittent catheterisation and more use of abdominal pressure during the follow-up.
The aim of this study was to examine the changes in bladder-emptying methods from 10 to 45 years after a traumatic SCI.
Materials and methods
The study included patients from the Clinic for Para- and Tetraplegia at Rigshospitalet, Denmark (CPT).
The inclusion criteria were a traumatic SCI contracted before 1st of January 1991 and that the participant was still alive at the time of mailing a follow-up questionnaire.
The exclusion criteria were: (1) irregular initial admission at the CPT, (2) follow-up terminated from the CPT, (3) not followed in CPT since 1990 or (4) missing medical record/insufficient data.
In all 279 participants were included in the project. They all received a questionnaire by mail with a prestamped return envelope. Approximately 2 months after the first dispatch of questionnaires a reminder with a new questionnaire was sent to those participants, who had not answered. At the first mailing 204 participants answered and returned their questionnaire. After the second mailing further 32 participants answered and returned their questionnaire.
All together 236 participants answered and returned the questionnaire, 193 men and 43 women injured from 1956 to 1990, corresponding to a response-rate of 84.6%. The age at the time of the study was 50.5 years in mean (SD 11.2, median 50.0, range 28.4–84.5), and follow-up time was 24.1 years in mean (SD 8.7, median 23.7, range 10.7–45.1). Concerning level of injury, 126 participants were paraplegic and 110 tetraplegic, 102 complete and 134 incomplete according to the Frankel classification.3
The nonresponder group consisted of 43 individuals, 35 men and eight women injured from 1960 to 1990.
The study was constructed as an epidemiological follow-up study consisting of data collected retrospectively from patient records and from the follow-up questionnaire concerning urological conditions. This gives the possibility of comparing data from the time of injury with data 10–45 years later and hereby describing the population and in particular changes occurring over years.
Medical record data
The retrospective data collected from the records were bladder-emptying method(s) at discharge from the initial rehabilitation admission at CPT, neurological level of injury (C2–L4) and Frankel classification3 at the time of discharge from the initial rehabilitation at CPT. The neurological level of the SCI is given as the most caudal normal spinal cord segment at the time of discharge from the initial rehabilitation.
The questionnaire
The questionnaire concerned different aspects of late complications in SCI individuals. The questions used in this study are seen in Table 1. As far as possible scales/questions and answer possibilities in the questionnaire were similar or comparable to previously published standards.4 Experience from an earlier study of reproducibility and validity of a questionnaire filled in by spinal cord lesioned individuals before regular follow-up5 has been used to optimise the questions.
Before the questionnaires were mailed to the participants in the main study, a pilot study was carried out including seven men with SCI (four tetraplegic and three paraplegic). The results of the pilot study showed that the questionnaire was comprehensive and easy to answer. Owing to the experience from the pilot study, minor adjustments were made before sending the questionnaire out to all participants in the main study.
To test the validity of the process of typing the answers to the questionnaire into the database, 10% (24 participants (p)) of the questionnaires were checked thoroughly a second time. The results showed that all data entries concerning the included data for the present publication were correct.
To investigate the reproducibility of the questionnaire 38 participants received a second questionnaire 2 years after the first emission. In all, 33 participants returned this second questionnaire (86.8%). The second questionnaire was analysed as to what extent the answers were the same as in the first questionnaire.
The analysis of the answers showed reproducibility of 90–100% concerning questions, where answers are expected to be the same over time, and reproducibility of 70–90% concerning questions, where the answers depend on how the participant feels at the time of answering the questionnaire and therefore are likely to change over time.
Therefore, the reproducibility of the questions used in this article was concluded satisfactory.
Statistical methods
χ2-test was used for tables, df=degrees of freedom. To compare means t-test was used. Five percent was chosen as level of significance.
Results
Representativeness
The comparison between the responder and nonresponder group with regard to gender, neurological level, para-/tetraplegia, Frankel classification,3 age at SCI, age at the time of follow-up, years since SCI and cause of SCI showed no statistical significant differences between the two groups.
Bladder-emptying method
Each participant may use more than one bladder-emptying method. In Tables 2 and 3, the distribution of bladder-emptying method(s) at the initial discharge from CPT and at the time of follow-up, respectively, are seen, further divided by gender, time of SCI and paraplegia or tetraplegia. At the initial discharge, 80% of the participants used only one method of bladder emptying. The remaining 20% used a combination of two bladder-emptying methods, where the most common combination was suprapubic tapping and abdominal pressure. At follow-up 44% of the participants used only one method of bladder emptying and 56% used two or several methods of bladder emptying. The most common combination at follow-up was clean intermittent catheterisation (CIC) and use of condom-catheter or diaper.
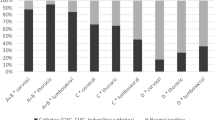
The participants using the five most frequently used bladder-emptying methods at the initial discharge have been analysed concerning how many used the same method at the time of follow-up. These results are shown in Figure 1. Of the participants using either suprapubic tapping or abdominal pressure initially, 36% used intermittent catheterisation at the time of follow-up. Of the participants using urethral indwelling catheter initially, 50% still used permanent catheter and 44% used intermittent catheterisation at follow-up.
Of the 233 participants whose bladder-emptying methods were recordable both initially and at the time of follow-up, 46% (107 p) had completely changed method, 25% (59 p) used the initial method in combination with one or more new methods and 29% (67 p) had not changed method. In the questionnaire the participants were asked if they had changed bladder-emptying method since the initial admission at CPT. Here, 107 participants reported that they had changed method. When comparing with retrospective data, we found that 74% of these (79 p) had completely changed method as reported. In addition 21% (22 p) used the same method at follow-up but in combination with one or more new methods, and only 6% (6 p) were found to have the same method at both times although reporting change of method. In the questionnaire 123 participants reported no change of method. According to the retrospective information 49% (60 p) of these did not change method, 30% (37 p) used the initial method in combination with one or more new methods, while 21% (26 p) actually did change method. This group did not have a significantly longer follow-up compared to the remaining 79% of participants reporting no change of method. The use of condom-catheter or diaper at follow-up has not been interpreted as a change of bladder-emptying method.
Perception of bladder management
One of the questions in the follow-up questionnaire was if the participants found their bladder management to be a problem. In all, 227 participants answered the question. Of the participants, 28% (64 p) did find their bladder management to be a problem. In this group, 80% (51 p) were male and 20% (13 p) were female sunbjets, 58% (37 p) were tetraplegic and 42% (27 p) were paraplegic. There was no significant difference concerning gender, but significantly more tetraplegics than paraplegics (P=0.02) found their bladder emptying method(s) to be a problem. No significant difference was found between the two groups regarding age at follow-up. When analysing bladder emptying methods for the participants who found their bladder management to be a problem and comparing with the remaining participants there were significantly fewer participants with normal bladder emptying in the group who found bladder management to be a problem. Concerning the other methods there were no significant differences but a higher proportion of participants using abdominal pressure, sterile intermittent catheterisation (SIC), suprapubic catheter and condom-catheter or diaper in the group who found bladder management to be a problem.
Use of catheter in CIC
In all, 84 participants used CIC at the time of follow-up. Of these 79 reported which type of catheter they used. A total of 89% (70 p) used hydrophilic-coated catheters. The remaining 11% (9 p) were not specific about which type they used.
Of the participants using CIC, 81 reported the number of catheters they used daily, 30% (24 p) reported that they used five catheters daily, 32% (26 p) used between one and four catheters daily, while 38% (31 p) used from six to 10 catheters daily.
Discussion
The responders to the follow-up questionnaire were found to be representative of the total study population of SCI individuals in a regular follow-up regime at CPT. In addition the data quality were found satisfactory concerning reliability and reproducibility of the questionnaire, validity of data entry and the participants' memory of change of bladder-emptying method over a period of 10–45 years. When comparing the distribution of bladder-emptying methods at the initial discharge with the distribution of bladder-emptying methods at the time of follow-up (Tables 2 and 3) differences are seen. These include that the proportion of participants using suprapubic tapping fell from 57% after the initial rehabilitation to 31% at the time of follow-up; while CIC/SIC procedure increased from 13 to 39% during the same period. CIC is the most common method of bladder emptying at the time of follow-up, when not including use of condom-catheter or diaper, which has to be considered as an incontinence device. This trend was also observed in previous studies2, 6, 7 and is in agreement with recommendations from studies8, 9 that have shown CIC to be a successful long-term option to bladder emptying in SCI individuals. The increased use of CIC was predominant in males. This corresponds to the relatively higher proportion of males compared to females changing from suprapubic tapping since the initial rehabilitation.
The proportion of participants using Credé manoeuvre raised from 5 to 20%, most probably reflecting that it is an easy procedure even though discouraged by the professionals. Fortunately, those injured in recent years use it less.
In the follow-up suprapubic catheters are more frequently used compared to initially. This could be due to a shift away from the trans-urethral indwelling catheter towards the suprapubic catheter over the years as recommended previously10, 11 to reduce complications, but it may also reflect that the suprapubic catheter is more convenient also in relation to sexual function. Both types of permanent catheters are primarily used by women and participants injured in the two later time periods seen in Table 3. Women have less possibility to overcome incontinence compared with men, as they cannot use condom-catheter and no similar collecting device is available for women in whom the permanent catheter may be found to be the best possible solution.
The difference between use of combinations of bladder-emptying methods at the time of the initial discharge (20%) and at the time of follow-up (56%) is notable. One reason could be due to the way the data are obtained. The data obtained from the initial discharge are retrieved from the medical files and are therefore reported by doctors or nurses. The follow-up questionnaire data are from the SCI individuals themselves. The difference also indicates that the optimal bladder-emptying regime in the daily routine sometimes demands combinations of more methods.
Regarding the bladder-emptying method at discharge from the initial rehabilitation period (Table 2) it is noteworthy that suprapubic tapping is used much more among men than women and much less for those injured from 1981–1990 in comparison with those injured prior to 1981. Credé manoeuvre and abdominal pressure are also to be gradually less used over time while intermittent catheterisation is only performed in the last time period. These changes reflect the introduction of intermittent catheterisation in the early 1980s and gradual discouragement of the use of suprapubic tapping, abdominal pressure and Credé manoeuvre. Suprapubic tapping demands a suprasacral bladder dysfunction and is, as expected used more among tetraplegics than paraplegics. Abdominal pressure and CIC demands function of the upper extremities and are as expected more used by paraplegics than tetraplegics.
Concerning the trends in change of bladder-emptying method, it is observed that less than half of the participants, who at the initial rehabilitation used either normal bladder emptying, suprapubic tapping or abdominal pressure continued with the method at the time of follow-up. Only 45% of the participants discharged with normal bladder emptying (Figure 1) reported to use this method only at the time of follow-up. It is important to be aware of this possible outcome for SCI individuals with seemingly normal bladder emptying, that is, the follow-up regime is essential to find these individuals to be able to advise them in their choice of alternative bladder-emptying methods. This finding does, of course, also reflect that the evaluation of the bladder function in the early part of the study period was not so sufficient as it is hopefully today. Concerning the participants using suprapubic tapping and abdominal pressure initially, 36% of the participants in both groups used intermittent catheterisation at the time of follow-up, which as previously mentioned is probably caused by the encouragement by professionals to use CIC.
Of the 26 participants using CIC at discharge, 77% remained on this method. This is not in agreement with earlier studies, which have shown a relatively high percentage of participants discontinuing the use of CIC over time.1, 2, 12 This diversity could be due to the longer timespan in the present follow-up and the time passed since the other studies were carried out. It is encouraging that this trend may have changed.
When analysing the reproducibility of the questionnaire we even found 12% (four of 33) of the participants changing to CIC during the 2 years between the participants answering the same questionnaire, which seems to stress the positive trends found in the main study.
Of the 18 participants, who initially used urethral indwelling catheter, 50% still used permanent catheter at the time of follow-up while 44% used intermittent catheterisation. This is a positive development in accordance with earlier studies recommending avoidance of indwelling catheters because of the risk of chronic urinary tract infections, as well as other urinary complications10 and bladder cancer.13, 14, 15 Although all bladder-emptying methods may not be as professionals might wish, there is a trend towards the more optimal method of intermittent catheterisation and avoidance of the more discouraged methods. Still the risk of incontinence and the desire of a satisfactory social life may tempt some to use a less optimal bladder-emptying method. Complete change in method of bladder emptying during follow-up was seen in 46% of the participants. This result is in agreement with a previous study, which found an even higher percentage (58%) with a follow-up period of only 5 years.2
Those who found their bladder management to be a problem was significantly more often tetraplegic, which could relate to their difficulties in handling the bladder-emptying process alone. When looking at the distribution of bladder-emptying methods at the time of follow-up for this group compared to the rest of the participants, less of the participants who found their bladder management to be a problem had a normal bladder emptying, as expected, and a higher proportion of the participants used abdominal pressure, SIC, suprapubic catheter and condom-catheter or diaper. It is understandable why methods involving assistance from another person or incontinence are more inconvenient.
The high proportion of participants using hydrophilic-coated catheters (92%) is very positive. A recent study16 has shown that use of hydrophilic-coated catheters is associated with less haematuria and a significant decrease in the incidence of urinary tract infections compared to use of conventional plastic catheters.
Conclusion
Changing of bladder-emptying method among SCI individuals over time is common. Some of the changes in bladder-emptying method are due to new knowledge in the area. CIC alone or in combination with another bladder-emptying method is the most frequently used method of bladder emptying at the time of follow-up. The trends seem to favour the recommended methods like CIC, but still convenience and risk of incontinence may influence the choice towards less advisable methods.
References
Cardenas DD, Farrell-Roberts L, Sipski ML, Rubner D . Management of gastrointestinal, genitourinary, and sexual function. In: Stover SL, DeLisa JA, Whiteneck GG (eds) Spinal Cord Injury: Clinical Outcomes from the Model systems. Aspen Publishers: Gaithersburg, MD, 1995 pp 120–144.
Biering-Sorensen F, Nielans HM, Dorflinger T, Sorensen B . Urological situation five years after spinal cord injury. Scand J Urol Nephrol 1999; 33: 157–161.
Frankel HL et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. I. Paraplegia 1969; 7: 179–192.
Levi R, Ertzgaard P . Quality indicators in spinal cord injury care: a Swedish collaborative project. The Swedish Spinal Cord Injury Council 1998. Scand J Rehab Med Suppl 1998; 38: 1–80.
Biering-Sorensen B, Egebart J, Hilden J, Biering-Sorensen F . Reproducibility and validity of a questionnaire filled in by spinal cord lesioned individuals before regular follow-up. Spinal Cord 2001; 39: 161–167.
Anson CA, Shepherd C . Incidence of secondary complications in spinal cord injury. Int J Rehab Res 1996; 19: 55–66.
Gallien P et al. Influence of urinary management on urologic complications in a cohort of spinal cord injury patients. Arch Phys Med Rehab 1998; 79: 1206–1209.
Giannantoni A et al. Clean intermittent catheterization and prevention of renal disease in spinal cord injury patients. Spinal Cord 1998; 36: 29–32.
Perkash I, Giroux J . Clean intermittent catheterization in spinal cord injury patients: a followup study. J Urol 1993; 149: 1068–1071.
Biering-Sorensen F, Bagi P, Hoiby N . Urinary tract infections in patients with spinal cord lesions: treatment and prevention. Drugs 2001; 61: 1275–1287.
Saint S, Chenoweth CE . Biofilms and catheter-associated urinary tract infections. Infect Dis Clin North Am 2003; 17: 411–432.
Yavuzer G et al. Compliance with bladder management in spinal cord injury patients. Spinal Cord 2000; 38: 762–765.
Groah SL et al. Excess risk of bladder cancer in spinal cord injury: evidence for an association between indwelling catheter use and bladder cancer. Arch Phys Med Rehab 2002; 83: 346–351.
Stonehill WH, Dmochowski RR, Patterson AL, Cox CE . Risk factors for bladder tumors in spinal cord injury patients. J Urol 1996; 155: 1248–1250.
West DA et al. Role of chronic catheterization in the development of bladder cancer in patients with spinal cord injury. Urology 1999; 53: 292–297.
Vapnek JM, Maynard FM, Kim J . A prospective randomized trial of the lofric hydrophilic coated catheter versus conventional plastic catheter for clean intermittent catheterization. J Urol 2003; 169: 994–998.
Acknowledgements
We thank secretary Lisbeth Nielsen, Clinic for Para- and Tetraplegia for all her technical and practical assistance during the project. Further, we thank the physiotherapists, occupational therapists and nursing staff at Clinic for Para- and Tetraplegi for inspiration and help with developing the questionnaire. The study was carried out as part of the primary author's PhD-study, which was financed by Medicon Valley Academy and Coloplast A/S.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Hansen, R., Biering-Sørensen, F. & Kristensen, J. Bladder emptying over a period of 10–45 years after a traumatic spinal cord injury. Spinal Cord 42, 631–637 (2004). https://doi.org/10.1038/sj.sc.3101637
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101637
Keywords
This article is cited by
-
Long-term bladder and bowel management after spinal cord injury: a 20-year longitudinal study
Spinal Cord (2018)
-
Surveillance and management of urologic complications after spinal cord injury
World Journal of Urology (2018)
-
The management of neurogenic lower urinary tract dysfunction after spinal cord injury
Nature Reviews Urology (2016)
-
Compliance with clean intermittent catheterization in spinal cord injury patients: a long-term follow-up study
Spinal Cord (2013)