Abstract
Study design: Prospective, open label, cross-over-designed clinical study.
Objective: To evaluate the effectiveness of an instillation of lidocaine into the bladder with versus without electromotive drug administration (EMDA) to anesthetize the bladder before botulinum-A toxin injections.
Setting: Neurourology, Swiss Paraplegic Center, Balgrist University Hospital, Zurich, Switzerland.
Methods: In all, 28 patients with severe neurogenic detrusor overactivity but preserved bladder sensibility were treated with botulinum-A toxin injections into the detrusor muscle. A measure of 300 u of botulinum-A toxin (Botox®) was injected at 30 sites sparing the trigone. Prior to the injection, the bladder was anesthesized with conventional lidocaine instillation in a group of 10 patients and with lidocaine instillation enhanced by EMDA in 28 patients. The patients scored the injection pain on a 10-point rating scale. Pain rating scores with versus without EMDA enhancement of the lidocaine instillation were analyzed and the costs of the EMDA procedure were compared to general/spinal anesthesia.
Results: The mean pain score of the 10 patients who underwent the injections of Botox® after conventional lidocaine instillation was 4.0 (SD 1.6). Following EMDA enhanced lidocaine instillation slight even or no pain occurred during the injections of Botox®, and the mean pain score was 0.5 (SD 0.2). Compared to spinal or general anesthesia, the local anesthesia saved around 15% of the costs.
Conclusions: EMDA enhanced instillation of lidocaine enables a sufficient anesthesia of the bladder wall that ensures a painless application of the botulinum-A toxin injections into the detrusor muscle. This method may avoid general or spinal anesthesia in patients with preserved bladder sensibility. It ensures considerable cost reduction, avoids anesthesia-related risks and complications and enables the procedure on an outpatient basis.
Similar content being viewed by others
Introduction
The first reports of botulinum-A toxin injections to treat neurogenic detrusor overactivity in spinal cord injured patients were published in 2000,1,2 and the interest in using botulinum-A toxin for treating neurogenic incontinence is increasing.3,4 Animal experiments revealed that injections of botulinum-A toxin into the detrusor muscle effectively block the release of acetylcholine at the presynaptic neuromuscular junction and suppress detrusor contraction.3 Improved continence following treatment with botulinum-A toxin into the detrusor in spinal cord-injured patients can be obtained in up to 90% of the patients and the beneficial effect lasted for a mean of 9 months (6–14 months).1,2
The injection of the toxin into the bladder wall is usually performed as an outpatient procedure. Although the intervention is generally well tolerated in patients with complete loss of bladder sensation, pain and discomfort occur in patients with preserved sensibility. The intravesical instillation of 2% lidocaine prior to the injection may reduce pain and discomfort but it remains often insufficient to ensure a painless intervention. Therefore, in most of the patients with preserved sensibility a general or spinal anesthesia is required, which prolongs the procedure and increases the cost.
The technique of electromotive drug administration (EMDA) is known to increase drug delivery into the bladder wall after intravesical instillation of lidocaine. A direct pulse current across the bladder mucosa moves a high concentration of ionized lidocaine into the bladder wall by several electrokinetic forces.5 Drug penetration is enhanced by iontophoresis (active transport of ionized drug down an electrical gradient of appropriate polarity), electroosmosis (ionized or nonionized drug transport accelerated by convective flow of water due to current-induced movement of other ions) and electroporation (increased permeability due to direct electrical effects on a biological membrane that permits increased transport along concentration gradients).6,7,8 Iontophoresis is the predominant electrokinetic force involved in the transport of local anesthetic drug.9
Canine studies using methylene blue have shown a greater penetration of the dye into the bladder wall with EMDA compared to controls without EMDA, indicating that more profound local anesthesia under EMDA with lidocaine, which has a molecular weight similar to methylene blue, is due to deeper penetration of the drug into the bladder tissues.9 The scientific basis and the rationale for using salt-free lidocaine 2% to anesthetize the bladder have been explained in detail by Fontanella et al.10 The presence of sodium chloride in the solution virtually ensures ineffectual local anesthesia since these ions are highly mobile, and there is charge competition between them and the lidocaine ions. EMDA has been used to deliver local anesthetic agents for transurethral surgery. Examples include transurethral microwave thermotherapy of benign prostate hyperplasia, hydrostatic distension of the bladder for interstitial cystitis and transurethral bladder surgery.5,10,11,12
In this study, we hypothesized that the EMDA enhanced instillation of lidocaine might be a sufficient local anesthesia in patients with preserved bladder sensibility, which could allow painless injection of botulinum-A toxin into the detrusor muscle. The effectiveness of an instillation of lidocaine into the bladder with versus without EMDA to anesthetize the bladder was evaluated in a prospective study in 28 patients. The intervention time and costs of the local EMDA procedure were compared to costs of spinal or general anesthesia.
Patients and methods
This prospective open study included 28 patients (17 males, 11 females, mean age: 35 years), who signed an informed consent before entering the study. The underlying disease was in 24 cases a spinal cord injury, in two cases a multiple sclerosis and in two cases a myelomeningocele. All patients presented with an incomplete spinal cord lesion and had a severe neurogenic bladder dysfunction of the upper motoneurone type with some preservation of the bladder sensibility. Indication for injecting the botulinum-A toxin into the detrusor was detrusor overactivity incontinence in 20 cases who failed to respond to high doses of oral anticholinergicss, severe side effects of anticholinergic drugs in two cases and both these indications in six cases. The local anesthesia was performed by a nurse in our outpatient department.
Local anesthesia procedures
In the group with conventional lidocaine instillation, 10 patients received intravesical instillation of 40 ml of lidocaine 2% and the drug was drained 20 min later. For instillation and draining, a normal 16F Foley-catheter was used. Then the injections were performed using a conventional rigid 22 F cystoscope and each patient scored injections' pain on a scale of 0 (no pain at all) to 10 (worst pain imaginable).13 The patients were instructed to come back to the clinic for reinjection after recurrence of the incontinence. Prior to subsequent reinjections, these 10 patients converted to the EMDA group.
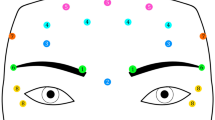
In the group with EMDA enhanced lidocaine instillation, 28 patients received EMDA enhanced lidocaine instillation prior to the injection. The drug solution for EMDA was prepared in a sterile dish by mixing 75 ml lidocaine hydrochloride 4% (sodium chloride-free) with 75 ml sterile water and 1.5 ml 1/100 000 epinephrine giving a final solution of 150 ml lidocaine 2% with epinephrine 1/100 000. The urethra was lubricated with 20 ml lidocaine 2% gel and the bladder was catheterised using a 16F balloon catheter with 3 sides holes near the tip and containing the positive electrode. The catheter used for males provided, via five additional holes distal to the ballon, an anesthetic effect in the prostatic urethra. The bladder was first drained and irrigated with 100 ml sterile water to check for hematuria. Thereafter, 100 ml of the drug solution was instillated. The dispersive cathode electrodes were placed on abdominal skin that had been degreased with alcohol wipes, and a 2–5 mm layer of conductive gel was applied. Air bubbles were eliminated by pressing and sliding the saline-impregnated dispersive electrodes gently side to side to avoid skin injury. The generator consisted of a battery-powered, current-controlled, programmable Physionizer 30® (Physion Srl, Mirandola, Italy) with a range of 0–30 mA and options of constant or pulse direct current (2 pulse current, 5 kHz), the latter being more efficient.9,10 The pulse current was activated and increased progressively (40–60 μA/s to a maximum of 25 mA, for 20–25 min, total charge 600 mA). Every 5 min, the catheter was rotated 90° to expose fresh areas of the prostatic urethra (for consistency it was also done in women). About 50 ml was withdrawn in the first-quarter run and reinfused to circulate the instillate and check for hematuria. About 50–60 ml instillates were removed at the second turn to minimize dilution by new urine and replaced with 50 ml fresh drug solution. At the end of the procedure, the bladder was drained and flushed. Immediately thereafter, the injection of Botox® was performed as described below. The patients scored injections' pain on the 10-point scale described previously.
Injection procedure
The bladder was prefilled with 100 ml normal saline and 300 u of botulinum-A toxin (Botox® Allergan Inc., Irvine, CA, 100 u diluted in 10 ml normal saline 0.9% without preservative, 10 u/ml/site) were injected at 30 sites of the detrusor muscle using a rigid cystoscope and a flexible 6F-injection needle with a 5 mm needle tip (Dantec®, Denmark).
Cost calculations
We compared the costs of the EMDA enhanced lidocaine instillation to the costs of spinal and general anesthesia in our institution, both on an outpatient basis. The costs of the local anesthesia include one current generator, one catheter electrode, three vials containing 30 ml lidocaine 4%, two vials epinephrine, 20 ml anesthetic gel for urethral lubrication, two skin reference electrodes, 125 ml conduction gel for these electrodes and costs for nursing and costs for the room at the outpatient department. With respect to the generator it was assumed that the device can be used for at least 100 treatments considering approximately 1/100 of the initial purchase expense per treatment. The costs for the spinal or general anesthesia include costs for the anesthesiologist, for the time in the operating room, for the drugs used for anesthesia and costs for postanesthetic monitoring.
Results
Injection of Botox® following conventional instillation of lidocaine (10 cases)
The intravesical instillation of lidocaine was well tolerated and the injections of the toxin were uneventful. Instillation and injection required around half an hour. All patients mentioned a certain degree of pain and discomfort during the injection. The mean pain score indicated by the 10 patients after the procedure was 4 (SD 1.6). There was no difference in the pain scores between males and females. None of the patients had macroscopic hematuria and all could return home after cystoscopy. The mean duration of botulinum-A toxin effect was 36 weeks and then reinjection under EMDA was performed.
Injection of Botox® following EMDA enhanced instillation of lidocaine (28 cases)
The EMDA procedure including preparation of the solution required around 1 h. The EMDA enhanced instillation of lidocaine and the toxin injections were well tolerated in all patients and no side effects were observed. During cystoscopy, we paid special attention to potential mucosa lesions caused by the catheter electrodes or the applied current. However, in none of our patients these lesions were observed.
The injections of Botox® caused a slight pain in 12 patients and 16 patients reported no pain at all. The mean pain score calculated in all 28 cases of the EMDA group was 0.5 (SD 0.2). Patients who had already undergone botulinum-A toxin injection after conventional instillation of lidocaine reported a remarkable reduction or even the absence of the pain and discomfort caused by the injections and would prefer the EMDA-enhanced instillation of lidocaine in the future. The mean pain score in this group was 0.7 (SD 0.5).
Cost comparison
The costs for the anesthesia using EMDA enhanced instillation of lidocaine approximates 491.00. CHF compared to 582.00 CHF for spinal or general anesthesia performed in the operating room (for details see Table 1). In our institution, the local anesthesia using instillation of lidocaine enhanced by EMDA is 90.00 CHF cheaper to perform.
Discussion
Promising reports on the effect of botulinum-A toxin injections into the detrusor muscle to treat detrusor overactivity incontinence have been published in 20001,2 and the interest in this new treatment option is still increasing.4 The currently administrated toxin dose of 300 units Botox® has been established in a previously performed dose titration study.2 The results of this study confirmed the efficacy of this new approach for the treatment of neurogenic detrusor overactivity and consecutive incontinence. However, in patients with preserved bladder sensibility the injection may cause pain or discomfort. Although the instillation of lidocaine 2% before injection of the toxin may prevent severe pain, it did not provide adequate local anesthesia in all patients. The two established options to overcome this situation are general or spinal anesthesia. Both solutions increase the severity and the costs of the basically simple procedure and require a skilled specialist's assistance.
This study assessed the efficacy of an alternative technique to anesthetize the bladder with instillation of lidocaine enhanced by EMDA. This simple and safe technique does not require specialized training. The neurophysiological function of various afferent fibers within the bladder wall is not fully understood but some studies suggest why lidocaine is effective. Chandiramani et al14 suggested that the applied lidocaine partially interrupted afferent nociceptive arcs of an abnormal spinal detrusor reflex in patients with neurological disease. All local anesthetic drugs reversibly inhibit all types of fibers, although those of small diameter, such as C fibres are more susceptible. Thus it is reasonable to postulate that afferent C fibers within the submucosal plexus of the bladder wall transmit nociceptive impulses and passively administrated lidocaine partially inhibits these superficially sited fibers. When EMDA is applied more lidocaine is administrated and tissue penetration is deeper,11 anesthesia is more profound and this also appears to cause some inhibition of motor fibers with relaxation of the detrusor muscle. EMDA with lidocaine 2% (13 mmol in 150 ml) is not toxic as indicated by the absence of toxic symptoms and serum lidocaine level (mean: 0.3 mg/ml) safe.10,11,15 Successful anesthesia of the bladder and the urethra using instillations of lidocaine with EMDA before invasive lower urinary tract procedures, such as biopsies or intravesical administration of capsaicin, has previously been reported.5,10,16 EMDA with lidocaine can be conveniently administrated by a trained nurse and is largely automated. Patients are able to leave the hospital immediately after completion of the botulinum-A toxin injections, and recovery facilities normally required after general anesthesia or heavy sedation are not required; the savings in immediate and long-term morbidity and costs are considerable. Moreover, the indications of application of botulinum-A toxin into the detrusor might be increased to other pathologies such as neurogenic detrusor overactivity due to multiple sclerosis (most of these patients have preserved sensations) or idiopathic detrusor overactivity without the inconvenience of a general or spinal anesthesia.
Conclusion
Instillation of lidocaine enhanced by EMDA provides a noninvasive, safe and effective local anesthesia of the bladder wall that ensures a painless application of botulinum-A toxin injections into the detrusor muscle. This method may avoid general or spinal anesthesia in patients with preserved bladder sensibility. It ensures a considerable cost reduction, avoids anesthesia-related risks and complications and enables the procedure on an outpatient basis.
References
Schurch B, Schmid DM, Stohrer M . Treatment of neurogenic incontinence with botulinum toxin A. N Engl J Med 2000; 342: 665.
Schurch B, Stohrer M, Kramer G, Schmid DM, Gaul G, Hauri D . Botulinum-A toxin for treating detrusor hyperreflexia in spinal cord injured patients: a new alternative to anticholinergic drugs? Preliminary results. J Urol 2000; 164: 692–697.
Franks ME et al. Botulinum toxin injection into the bladder wall decreases acetylcholine (ACH) and nor-epinephrine (NE) release; potential treatment for the overactive bladder. J Urol (Suppl.) 2000; 163, Abstract 181.
Schulte-Baukloh H, Michael T, Schobert J, Stolze T, Knispel HH . Efficacy of botulinum – a toxin in children with detrusor hyperreflexia due to myelomeningocele: preliminary results. Urology 2002; 59: 325–327; discussion 327–328.
Jewett MA, Valiquette L, Sampson HA, Katz J, Fradet Y, Redelmeier DA . Electromotive drug administration of lidocaine as an alternative anesthesia for transurethral surgery. J Urol 1999; 161: 482–485.
Gangarosa LP, Park NH, Wiggins CA, Hill JM . Increased penetration of nonelectrolytes into mouse skin during iontophoretic water transport (iontohydrokinesis). J Pharmacol Exp Ter 1980; 212: 377–381.
Stephen RL, Miotti D, Bettaglio R, Rossi C, Bonezzi C . Electromotive administration of a new morphine formulation: morphine citrate. Artif Organs 1994; 18: 461–465.
Prausnitz MR, Bose VG, Langer R, Weaver JC . Electroporation of mammalian skin: a mechanism to enhance transdermal drug delivery. Proc Natl Acad sci USA 1993; 90: 10504–10508.
Gurpinar T, Truong LD, Wong HY, Griffith DP . Electromotive drug administration to the urinary bladder: an animal model and preliminary results. J Urol 1996; 156: 1496–1501.
Fontanella UA, Rossi CA, Stephen RL . Bladder and urethral anaesthesia with electromotive drug administration (EMDA): a technique for invasive endoscopic procedures. Br J Urol 1997; 79: 414–420.
Gurpinar T Wong HY, Griffith DP . Electromotive administration of intravesical lidocaine in patients with interstitial cystitis. J Endourol 1996; 10: 443–447.
Riedl CR, Knoll M, Plas E, Pfluger H . Intravesical electromotive drug administration technique: preliminary results and side effects. J Urol 1998; 159: 1851–1856.
Huskisson EC . Measurement of pain. Lancet 1974; 2: 1127–1131.
Chandiramani VA, Peterson T, Duthie GS, Fowler CJ . Urodynamic changes during therapeutic intravesical instillations of capsacin. Br J Urol 1996; 77: 792–797.
Lugnani F, Mazza G, Cerulli N, Rossi C, Stephen R . Ionotophoresis of drugs in the bladder wall: equipment and preliminary studies. Artif Organs 1993; 17: 8–17.
Dasgupta P, Fowler CJ, Stephen RL . Electromotive drug administration of lidocaine to anesthetize the bladder before intravesical capsaicin. J Urol 1998; 159: 1857–1861.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Schurch, B., Reitz, A. & Tenti, G. Electromotive drug administration of lidocaine to anesthetize the bladder before botulinum-A toxin injections into the detrusor. Spinal Cord 42, 338–341 (2004). https://doi.org/10.1038/sj.sc.3101593
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101593
Keywords
This article is cited by
-
A morphological evaluation of botulinum neurotoxin A injections into the detrusor muscle using magnetic resonance imaging
World Journal of Urology (2009)
-
7 Jahre Botulinum-A-Toxin in der Behandlung der neurogenen Detrusorhyperaktivität
Der Urologe (2007)
-
Intravesikale Therapie der überaktiven Blase
Der Urologe (2006)
-
Botulinumtoxin in der Urologie
Der Urologe, Ausgabe A (2004)