Abstract
Study design: Case report
Objective: To examine the resolution of holocord myelopathy based on the hypothesis of altered cerebrospinal fluid (CSF) dynamics.
Setting: Seoul National University Hospital, Seoul, Korea.
Method: We describe a case of thoracic stenosis with holocord myelopathy, which suggests an alternative mechanism for the myelopathy.
Result: Decompression of the thoracic stenosis resulted in the resolution of holocord myelopathy.
Conclusion: Myelopathy may be caused by altered CSF dynamics and this type of myelopathy seems to be interstitial edema. Improvement of altered CSF flow dynamics could resolve this type of myelopathy.
Similar content being viewed by others
Introduction
It is commonly accepted that myelopathy in spinal stenosis is caused by arterial insufficiency. We describe a case suggesting an alternative hypothesis for the pathogenesis of holocord myelopathy in spinal stenosis.
Case report
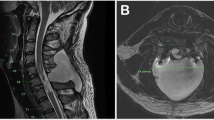
A 64-year-old man was admitted with a chief complaint of difficulty in walking, which developed 4 months previously and thereafter progressed. He could not walk without assistance. On admission, neurological examination showed low extremity weakness (ASIA impairment scale C) and hypoaesthesia to pain and temperature (50/100%, respectively) below the T10 level. Knee and ankle jerks were increased and ankle clonus and Babinski's sign were found bilaterally. Anal tone was decreased and saddle hypoaesthesia was present. Magnetic resonance (MR) images and computed tomography of the thoracic spine showed intramedullary high signal intensity involving whole spinal cord on a T2-weighted image and suspicious stenosis at the T11 level (Figure 1). The midsagittal cardiac-gated phase-contrast cine MR (cine MR) image (1.5 T Genesis Signa Advantage scanner; General Electric, Milwaukee, WI, USA) at the stenotic site showed obstruction of cerebrospinal fluid (CSF) circulation at the T11 level (Figure 1). Posterior decompression of T11 stenosis was performed. Operative findings were of a thickened ligamentum flavum and, after decompression, the thecal sac was expanded. Steroid medication was not given. Postoperatively, lower extremity weakness was improved, resulting in independent walking with a single cane 2 months later (ASIA impairment scale D). Follow-up MR imaging obtained 2 months after the operation showed that the myelopathy of the whole spinal cord was improved and cine MR image (1.5 T Genesis Signa Advantage scanner; General Electric, Milwaukee, WI, USA) revealed good CSF flow around the previous obstruction (Figure 2).
Axial CT scan shows bilateral calcified ligamentum flavum, causing stenosis of the spinal canal at the T11 level (a, arrow). A T2-weighted sagittal image, obtained a day after CT scanning, revealed a high signal intensity lesion in the whole spinal cord and the T2-weighted axial image shows mild stenosis at the T11 level (b, black arrow; c, white arrow). On the mid-sagittal cine MR image, the CSF flow signal is not identified especially anteriorly and compressed along the anterior and posterior SAS, respectively (d, arrow; e, arrow)
After decompressive laminectomy of T11, a T2-weighted sagittal image, obtained 2 months after, reveals decreased extent of the holocord myelopathy (arrow), most conspicuous around the decompressed level and noticeable at the nondecompressed level as well (a, arrow). The compressed dural sac is also relieved with removal of the hypertrophied ligamentum flavum on the axial T2-weighted image (b, arrow). Cine MR image revealed that CSF flow is markedly improved, especially along the anterior SAS (c, arrow; d, arrow)
Discussion
The major factor causing the myelopathy in spinal stenosis has been thought to be the arterial insufficiency due to the mechanical compression imposed by the stenosis.1,2 The commonly accepted pathogenesis is that local ischemia of the cord produced by mechanical compression of the cord causes myelopathy, and that this ischemia is magnified and made irreversible by a disturbance in the blood supply from the systemic circulation.2 Consequently, the myelopathy was found around stenotic level. However, the myelopathy in the present case involved holocord, suggesting that the myelopathy of the patient is different from the usual myelopathy following spinal stenosis.
Myelopathy and CSF flow dynamics
Klekamp et al3 demonstrated that altered dynamics of CSF flow causes interstitial edema in the cervical spine below the stenotic lesion due to the pressure gradient between subarachnoid space (SAS) and the spinal cord.3 This edema is found around the central gray matter and central part of the posterior white matter.3 They also suggest that this interstitial edema was a presyrinx state.3 Therefore, interstitial edema (presyrinx state) may represent a state of altered extracellular fluid dynamics as a consequence of CSF flow alteration.3,4 Cervical CSF flow disturbances tend to produce interstitial edema (presyrinx state) below the level of obstruction, whereas low thoracic lesions tend to produce a presyrinx state above the level of obstruction.3,4 Altered CSF flow dynamics can be evaluated by cine-MR image and we used cine MR image to evaluate the change of CSF flow dynamics. Cine MR images can show either obstruction or excessively turbulent flow within the CSF pathway, and the site of this change can be appreciated by changes or absence of the normal hypointense signal in SAS.5
Lee et al6 suggesed the possibility of the correlation between spinal cord syringomyelia and altered CSF dynamics.6 In his study, patients showed clinical improvement after SAS decompression, resulting in improvement of the altered CSF flow.
In our case, the myelopathy was thought to be interstitial edema (presyrinx state) and the myelopathy seemed to be associated with altered CSF flow dynamics. Decompressive laminectomy improved the altered CSF flow, resulting in the resolution of the interstitial edema.
There is also a possibility that holocord myelopathy in our case was a transient non-tumorous myelopathy, which was incidentally found in the setting of thoracic stenosis. However, centrally located myelopathy, old age, and no cranial involvement suggested that the myelopathy was caused by altered CSF flow dynamics rather than demyelinating disease.7 Moreover, the myelopathy was improved after decompressive surgery and this change is most conspicuous around the decompressed area.
Conclusion
Myelopathy, associated with spinal stenosis, has been thought to be caused by impaired vascular supply. However, myelopathy may also be caused by altered CSF dynamics and this type of myelopathy seems to be interstitial edema. Improvement of altered CSF flow dynamics could resolve this type of myelopathy.
References
Batzdorf U, Flannigan BD . Surgical decompressive procedures for cervical spondylotic myelopathy. A study using magnetic resonance imaging. Spine 1991; 16: 123–127.
Hukuda S, Wilson CB . Experimental cervical myelopathy: effects of compression and ischemia on the canine cervical cord. J Neurosurg 1972; 37: 631–652.
Klekamp J et al. Disturbances of cerebrospinal fluid flow attributable to arachnoid scarring cause interstitial edema of the cat spinal cord. Neurosurgery 2001; 48: 174–185.
Sartoretti-Schefer S, Kollias S, Valavanis A . Transient oedema of the cervical spinal cord. Neuroradiology 2000; 42: 280–284.
Quencer RM, Post MJ, Hinks RS . Cine MR in the evaluation of normal and abnormal CSF flow: intracranial and intraspinal studies. Neuroradiology 1990; 32: 371–391.
Lee JH, Chung CK, Kim HJ . Decompression of the spinal subarachnoid space as a solution for syringomyelia without Chiari malformation. Spinal Cord 2002; 40: 501–506.
Poser CM, Brinar VV . Diagnostic criteria for multiple sclerosis. Clin Neurol Neurosurg 2001; 103: 1–11.
Acknowledgements
This work was supported in part by a grant from the Seoul National University Hospital Research Fund.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Kim, C., Chung, CK., Kwon, B. et al. Holocord myelopathy with thoracic stenosis: case report and hypothesis. Spinal Cord 41, 696–699 (2003). https://doi.org/10.1038/sj.sc.3101522
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101522