Abstract
Objective: Documentation of three-dimensional (3D) images of a giant sacral schwannoma with intrapelvic expansion.
Setting: Nagoya University, Nagoya, Japan.
Results: 3D computed tomography (3D CT) showed a destructed bony region clearly. 3D CT angiography clarified the positional relationship between tumor and iliac arteries. Resection procedure was safely completed based on these 3D evaluations.
Conclusion: 3D images were helpful to make a surgical plan and to complete this complicated resection combined with sacroiliac reconstruction.
Similar content being viewed by others
Introduction
Sacral tumors including schwannoma are relatively uncommon. They often become very large due to vague symptoms and are then difficult to completely resect. We report the following case of giant sacral schwannoma with intrapelvic expansion and discuss the radiological evaluation for surgical plan.
Case report
A 52-year-old woman had edema of the right lower leg for several months. Palpation revealed a mass, approximately 10 × 10 cm2 in size, in the lower portion of the abdomen. The patient had hypesthesia on the right lateral thigh and leg. There was no motor weakness. Bladder and bowel function were normal.
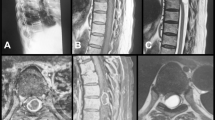
Magnetic resonance imaging (MRI) showed a giant mass in the right lumbosacral region with break through into the pelvic cavity anteriorly (Figure 1). The mass was enhanced with gadolinium and included some cysts. A needle biopsy via a postsacral approach revealed that the tumor was a schwannoma or a nonmalignant me-ningioma. After transfer to our institute, three-dimensional (3D) radiographic evaluations were performed.
Reconstructed 3D computed tomography (3D CT) showed destructive changes involving the right L4/5 and L5/S1 foramen and one-fourth of the L5 vertebra body. More than half of the upper right sacrum was also destroyed (Figure 2a). The tumor seemed to originate from the right L5 root. 3D CT angiography showed that the tumor had pushed the right common iliac artery aside, the right external iliac artery anteriorly, and the right internal iliac artery inferiorly (Figure 2b). Hypervascularity of the tumor was not seen even in conventional digital subtraction angiography (DSA).
A surgical plan was made based on these evaluations. As the anterior segment of the tumor expanded into the intrapelvic space and iliac arteries were stuck to it, an anterior approach should be better for tumor resection. However, postoperative pelvic instability was estimated based on the severely destructive image of the sacrum. At first, bone graft with posterior instrumentation was recommended to secure initial sacroiliac fixation.
Instrumentation should be expanded from L3 and to the ilium because of the destruction of the L4/5 facet, L5 and S1 pedicles in the right side. Autologous bone should be harvested from the left illium to preserve the right bone stock. For left side fixation, we chose an intrasacral rod.
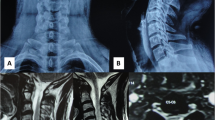
This surgical resection was performed using the following procedures. At first, laminectomy of L4 and L5 was performed through a posterior midline incision and the right L4/5 and L5/S1 facets were excised. Since the tumor originated from the right L5 root, the L5 root was resected. The posterior segment of the tumor was removed by piecemeal dissection. Then, spinal instrumentation was performed according to the surgical plan (Figure 3a and b). After 3 weeks, an anterior resection was performed through a midline abdominal approach. A giant tumor, approximately 20 × 20 cm2 in size was identified in the rectoperitoneal space. The right external iliac artery was stuck to the tumor as shown in 3D CT angiography (Figure 4). This artery was released from the anterior surface of the tumor. The right common iliac vein was ligated. The abdominal neural plexus was freed from the tumor and the capsule was exposed. After partially enucleating the tumor, its capsule was freed from the surrounding tissues. The intraforamen parts of the tumor were removed easily. An iliac strut bone was grafted to the anterior side of the L4–S1 vertebra.
Exposed tumor through an anterior approach. The right external iliac artery is stuck to the tumor as shown in Figure 2b
Histological examination proved the tumor to be an Antoni A-type schwannoma without malignancy. The postoperative course was uneventful and the patient started to walk 1 week after the operation and was discharged 2 months later. The patient did not complain of any symptoms in the 12 months postoperatively.
Discussion
Giant sacral schwannoma is rare. Due to the large capacity for regional expansion into the intrasacral space, and the slow growth rate of the tumor, symptoms develop late in the course of the disease when the tumor has become very large.1,2,3 Such tumors always destroy the spinal column or sacroiliac joint, and reconstruction may be required.4 Complete resection is recommended to prevent recurrence.4,5,6 However, it may require the sacrifice of many nerve roots.1 Detailed radiographic evaluations are required for a surgical plan of accurate resection.
Diagnosis and surgical plan of abnormalities within complex anatomy such as the skull, wrist, and pelvis are limited using standard radiography. Computer programs were created in the early 1970s and 1980s to manipulate cross-sectional CT data to produce 3D rendered images of anatomic structures. In this case, 3D CT demonstrated that the tumor originated from the L5 root in the foramen and extended anteriorly into the intrapelvic space. Although the patient had no symptoms of pelvic instability, 3D CT showed severely destructive changes in the right sacrum and helped us in making a plan for anterior bone graft simultaneous with tumor resection.
CT angiography can be reconstructed to a 3D image. It has become more popular for the evaluation of intracranial aneurysm or pulmonary carcinoma. It demonstrates a good vascular image with a less invasive procedure than conventional DSA.7,8 There is no report of 3D CT angiography for a surgical plan of giant sacral schwannoma. In this case, 3D CT angiography provided us with accurate information about the iliac arteries. It clarified the 3D relationships of the bones, arteries, and tumor. Conventional DSA could not show the depth of the arteries. Actually, iliac arteries and veins were hard to distinguish from surrounding fibrous tussue during the procedure because they were so tense and thin due to the tumor pressure. Based on preoperative 3D image, we could predict vessel positions and possibly prevent unexpected laceration or bleeding from occurring.
Besides conventional 2D evaluation, 3D images were more helpful in making a surgical plan and to complete this complicated resection combined with sacroiliac reconstruction.
References
Kagaya H et al. Giant cauda equina schwannoma. A case report. Spine 2000; 25: 268–272.
Rengachary SS, O'Boynick P, Batnitzky S, Kepes JJ . Giant intrasacral schwannoma: case report. Neurosurgery 1981; 9: 573–577.
Turk PS, Peters N, Libbey NP, Wanebo HJ . Diagnosis and management of giant intrasacral schwannoma. Cancer 1992; 70: 2650–2657.
Santi MD, Mitsunaga MM, Lockett JL . Total sacrectomy for a giant sacral schwannoma. A case report. Clin Orthop 1993; 294: 285–289.
Abernathey CD et al. Surgical management of giant sacral schwannomas. J Neurosurg 1986; 65: 286–295.
Iwasaki M et al. Surgical management of giant schwannoma in the lumbosacral region. J Spinal Disord 1998; 11: 444–447.
Rankin SC . CT antiography. Eur Radiol 1999; 9: 297–310.
Richter CS, Biamino G, Ragg C, Felix R . CT angiography of the pelvic arteries. Eur J Radiol 1994; 19: 25–31.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Satake, K., Matsuyama, Y., Yoshihara, H. et al. Three-dimensional images for surgical plan of giant sacral schwannoma. Spinal Cord 42, 368–370 (2004). https://doi.org/10.1038/sj.sc.3101520
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101520