Abstract
Study design: Post intervention, repeated measures design, comparing two interventions.
Setting: Orthopedic pediatric hospital specializing in spinal cord injury.
Methods: Nine subjects, ages 7–20 years, received an eight-channel implanted lower extremity functional electrical stimulation (FES) system for standing and walking. Electrodes were placed to stimulate hip and knee extension, and hip abduction and adduction. Standing and walking were achieved through constant stimulation to the implanted muscles, allowing a swing through gait pattern with an assistive device. After training with FES and long leg braces (LLB), subjects were tested in eight upright mobility activities, which were scored based upon completion time and level of independence.
Results: Seven subjects completed data collection. These subjects completed four activities faster (P<0.02) and five activities more independently (P<0.025) with FES as compared to LLB. Transitions between sitting and standing, which were scored in isolation for two mobility activities, were achieved faster and with more independence with FES. In addition, subjects reported preferring FES for the majority of activities. No activity required more time or more assistance to complete with FES as compared to LLB.
Conclusion: The implanted FES system provided these subjects with enhanced functional abilities over traditional LLB and decreased the need for physical assistance by a caregiver, suggesting that it is a realistic alternative for upright mobility in a pediatric population with spinal cord injury.
Sponsorship: This study was funded by Shriners Hospitals for Children, Grant #8530.
Similar content being viewed by others
Introduction
Standing is often desired by people with spinal cord injuries in order to perform standing activities near the wheelchair and has the potential for both physiological and psychological benefits.1,2,3 Typically, people with paraplegia who desire standing are prescribed long leg braces (LLB). User abandonment has been reported to be high (30% to 71%) due to issues including poor fit into a wheelchair, bulkiness beneath clothing, skin irritation, and difficulty in donning.2,4 A completely implanted functional electrical stimulation (FES) system may provide an alternative method of upright mobility while alleviating some of these abandonment issues. It may also provide potential benefits of enhanced functional upright abilities by allowing a quicker transition from sitting to standing with greater independence, therefore acting as a complement to the wheelchair.1
The majority of research on FES for upright mobility has provided stimulation to muscles using electrodes placed on the skin surface5,6,7 or through percutaneous intramuscular electrodes.1,8,9,10,11,12 implanted directly into the muscle, exiting at the skin surface. Collectively, this research has shown that upright mobility with FES is feasible.1,5,6,8,9,10,11,12 More recently, completely implanted systems have been employed in adults.13,14,15,16 There is no work published on these systems in a pediatric population.
Kobetic et al13,14 implanted a 16-channel lower extremity FES system in a 41-year-old adult with T10 paraplegia. Follow-up reports14 indicated that the subject was able to stand with a walker for 8 min and walk for 20 m with stand-by assistance. Despite some issues of undesired recruitment of the hip flexors with stimulation, the subject reported perceived health benefits of increased energy and decreased spasticity in his lower extremities and a psychological benefit of looking other people in the eye while standing.14 Davis et al17 implanted an 8-channel FES system in seven adults with low cervical and thoracic SCI. With this system, subjects were able to perform standing pivot transfers with an assistive device. Davis et al15 implanted a 22-channel FES system in one adult subject with T10 complete paraplegia. Their results showed that the subject was able to stand for one hour using a closed-loop system with electrogoniometers on the knee to detect joint position. With this system, stimulation to the quadriceps muscles was required for 10% of the total standing time.15
Previous work in our laboratory1,9,10 has shown that children with paraplegia could perform functional activities in at least an equal amount of time and with at least equal independence using a percutaneous FES system as compared to LLB. Children were tested on common activities including a sit to stand transition, reaching items on a shelf, short distance ambulation (6 m), ascending and descending stairs, and maneuvering in an inaccessible bathroom. The children preferred using the FES system for 62% of the activities, LLB for 27% of activities, and showed no preference for 11% of activities. Muscle fatigue was not noted to be an issue as the tested activities could be completed in a short time period.
Due to the positive outcomes with a percutaneous FES system, our study's aim was to implement and evaluate a permanent implanted FES system for children and adolescents with thoracic level spinal cord injuries. Our study hypothesis was that children and adolescents would be able to don the external FES system and perform seven functional upright mobility activities with a completely implanted FES system in at least comparable time and with at least comparable independence as compared to LLB.
Methods
Subjects
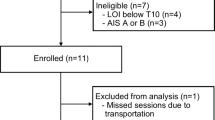
Nine subjects (Table 1), aged 7–20 years, met the selection criteria (Table 2) and received the lower extremity implanted FES system. All subjects had diagnoses of paraplegia, except subject 5 with a diagnosis of C7 tetraplegia. Prior to gait training with LLB, subject 5 underwent bilateral upper extremity tendon transfers to provide grasp and pinch to allow her to maintain hold of a walker. All subjects had prior experience with ambulation with LLB prior to participating in the study. LLB used by the subjects included reciprocating gait orthoses (RGO), hip knee ankle foot orthoses (HKAFO), and knee ankle foot orthoses (KAFO), which had been prescribed by physicians and physical therapists as part of each subject's regular physical therapy intervention post SCI (Table 1).
Parents of all subjects less than 18 years of age signed an informed consent form. Subjects 13 years of age and older also signed the consent form. This study was approved by the governing institutional review board.
Components of FES system
The internal components consisted of an 8-channel internal stimulator (NeuroControl Corporation, Cleveland, OH, USA) and eight electrodes. Power and FES patterns were provided to the internal stimulator by a research grade external control unit18 which communicated with the internal stimulator though the use of a radio frequency antenna secured to the skin directly over the implant site. Subjects selected and activated the FES patterns via a thumb switch worn like a ring or attached to the assistive device.
The internal stimulator delivered a balanced asymmetrical biphasic waveform with pulse duration up to 200 μsec, a frequency to 20 Hz, and a current to 20 mA. The pulse duration was the primary parameter adjusted to modulate the force of the muscle contraction. The frequency remained fixed at 20 Hz and the current at 20 mA for most subjects. The current was lowered to 8 and 14 mA to the femoral nerve electrodes in one of the younger and smaller subjects to obtain a more gradual force recruitment of the quadriceps muscles appropriate for the sit to stand transition.
Bilateral ankle foot orthoses (AFO) set in zero degrees of dorsiflexion were worn when ambulating with the FES system to protect the ankle complex and to provide a biomechanical advantage of maintaining knee extension. The AFO also served to decrease muscle fatigue and the number of joints needing control.19
Surgical procedure
The internal stimulator and eight electrodes were surgically implanted in each subject. The internal stimulator was placed into the subcutaneous fascia of the right lower quadrant of the abdomen and secured with sutures. Electrodes were placed bilaterally into the gluteus medius and maximus for hip abduction and extension, the posterior fibers of the adductor magnus for hip extension and adduction, and near the femoral nerve just distal to the branch to the sartorius for knee extension. Following electrode implantation, all electrode leads were tunneled subcutaneously and attached to the internal stimulator. To prevent unwanted hip flexion with stimulation to the femoral nerve, a 1 cm section of the proximal rectus femoris tendon was incised just distal to the separation of the main head and the reflected heads of its attachment to the pelvis. The sartorius was also released in subjects 3, 7 and 8 due to strong hip flexion and external rotation with stimulation to the femoral nerve. The most recent subject, subject 9, underwent an alternative method for stimulated knee extension, implanting the vastus lateralis instead of the femoral nerve. This avoided the need to release the rectus femoris, while still providing adequate knee extension strength.
Either an epimysial or intramuscular electrode20 was implanted into each targeted muscle in the first three subjects. The subsequent six subjects received all intramuscular electrodes. Epimysial electrodes are sutured directly to the muscle therefore requiring an incision, while intramuscular electrodes are placed directly into the muscle tissure using a percutaneous approach and are held in place by a barb. The incision required to place an intramuscular electrode is minimal (0.5 cm). Initially it was felt that an epimysial electrode would be optimial for stimulating the femoral nerve, as it could be secured to the tissue immediately beneath the nerve. It was later determined that an intramuscular electrode could be placed to stimulate the femoral nerve and still provide sufficient quadriceps force. Epimysial electrodes were also initially placed onto the gluteus medius muscle, which was accessible by expanding the incision required to release the proximal rectus femoris tendon. The change was made to using all intramuscular electrodes, as there was a desire to decrease the size and number of incisions necessary to implant the system.
As five of the subjects were skeletally immature, it was necessary to accommodate for growth. Extra lead wire (mean of 5 cm per subject) was placed for each electrode in an S-shape along the path to the stimulator to accommodate growth of the pelvis and the proximal femur.21 Growth was estimated via growth charts and by bone age using the Greulich-Pyle method.22 Two growing subjects also received bilateral tibial derotational osteotomies due to excessive tibial external rotation (<50°), one during the initial implant and one after training. Table 3 provides a summary of the surgical procedures for each subject, including the type of electrode implanted for each muscle.
Post-operative period
Following implantation, each subject's hips were immobilized for 2–4 weeks in an orthoses or hip abduction pillow to maintain the hips in 20° abduction and limit hip flexion to no greater than 20°. Subjects were able to self-propel a reclining wheelchair for mobility during this time after receiving assistance to transfer into the wheelchair. The goal of this immobilization phase was to minimize excessive joint motion due to spasticity in order to maintain electrode placement while tissue encapsulation of the implanted components occurred. Any increased spasticity post-operatively was treated with antispasticity medication. The first seven subjects were each immobilized for 4 weeks following implantation. The next two subjects were immobilized for only 2 weeks based on the thought that sufficient encapsulation of the electrodes had occurred by this time.
FES patterns
Prior to the development of the FES patterns, stimulation levels for each muscle were determined individually for each subject to provide optimal exercise and walking programs. The optimal amount of stimulation was defined as the lowest pulse duration that provided the maximum force, as measured by manual muscle testing (MMT).23
Following immobilization, each subject participated in 2–4 weeks of FES strengthening. Three exercise patterns were performed in supine. The first was a kicking exercise for strengthening the quadriceps muscles performed with the knee supported in approximately 30° of flexion. Five sets of 10 maximal contractions, held for 5 s, were performed twice daily, 6 days per week. Weights in 1 lb increments were added when the subjects's leg could extend fully against gravity through all five sets. Weights lifted ranged from 2 to 10 lbs depending on the size of the subject and the stimulated muscle strength. The second exercise was a bridging exercise performed under the same conditions, except weights were not added. In this pattern, the adductor magnus and gluteal muscles were stimulated. The third exercise was an endurance exercise where submaximal stimulation (75% of maximum) was provided to all implanted muscles in a cyclical pattern over a 90 min time period. This exercise was performed twice daily, 6 days per week.
An additional exercise in standing was performed after approximately 1 week of supine exercises. Subjects were positioned in a supportive stander and used a program that activated all muscles continuously at 80% of maximum stimulation. This allowed the subjects to accommodate to the standing position in combination with the stimulation. When this standing exercise was tolerated for an entire therapy session (up to 45 min, the bridging, kicking, and endurance patterns were decreased to once daily.
Standing and walking were initiated after 2 weeks of exercise for the younger, smaller subjects and up to 4 weeks for the older, larger subjects. This was related to safety, as the smaller subjects could more easily be stabilized by the physical therapist if their muscles fatigued while standing. This enabled earlier incorporation of play activities in standing, which provided motivation for the younger subjects.
To perform sit-to-stand, stimulation to all muscles was ramped up to the maximum level over 2–3 s. The pulse duration was ramped down over 1–2 s to perform stand-to-sit. These time periods allowed the subjects time to stabilize the upper body with the upper extremities during the transitions. The standing and walking patterns provided continuous stimulation to all implanted muscles (Figure 1), allowing ambulation using a swing through gait pattern with forearm crutches or a walker. Three subjects preferred a reciprocal walking pattern using the upper body and trunk to advance one lower extremity at a time. For reciprocal walking, one subject required the hip extensor stimulation to be decreased. The other two did not and were able to alternate between the two methods of walking spontaneously.
Upright mobility training
Following the 2–4 week strengthening period, each subject received training in seven mobility activities and system donning (Table 4) using both FES and LLB. The specific activities were chosen due to their relevance and appropriateness for the age group studied. Training time ranged from 3 to 8 weeks and continued until each subject demonstrated consistent completion times and levels of independence for each activity with FES and LLB. The goal for each training session was to maximize functional independence and timeliness with both FES and LLB.
In addition to the training in the seven activities, subjects were trained in other age appropriate upright activities of their interest as they learned how to use the FES system safely. This included activities such as playing video games or pool, cooking, grooming at a sink, writing on a chalkboard, throwing a ball, and transferring into and out of a car (Figure 2). Many of these self-selected activities included components of the activities chosen for data collection.
Data collection
After completing training, subjects were tested in the seven upright functional mobility activities and system donning with FES and LLB. Five repeated measures were collected for each activity and condition. Activities were scored based on completion time and on level of independence, using a 7-point scale based on the functional independence measure (FIM). Immediately after testing, subjects were asked to identify if FES or LLB were preferred for each activity.
Data analysis
A generalized linear model analysis of variance (ANOVA) with repeated measures was used to compare the completion times and FIM scores between FES and LLB for the seven upright activities and system donning. A normalized rank transformation was performed to the data prior to the analysis. A P-value ⩽0.05 was accepted to determine significance.
Results
Subjects completed four activities more quickly when using FES as compared to LLB (Table 5), including system donning, stand and reach, the high transfer, and the inaccessible bathroom transfer. They also required less assistance, as shown by an increase in FIM scores, for these same four activities plus the floor to stand activity (Table 6). No activity required more time or more assistance to complete with FES as compared to LLB. Two of the activities, stand and reach and the high transfer, were also scored based on their component activities, which included the sit to stand and stand to sit transitions. Analysis of these components showed that the subjects were able to stand up faster with FES during the stand and reach and the high transfer (Table 5). They also required less assistance to stand up and return to sitting in the wheelchair during the stand and reach and to perform the stand to sit component of the high transfer (Table 6). In addition, subjects reported preferring FES for 87.5% of the activities, LLB for 3.6% of the activities, and showed no preference for 8.9% of the activities.
Of the 72 initial electrodes implanted, 60 (83%) have continued to function without difficulty. Twelve electrodes (17%) required revision, 11 of these in subjects 2 and 3. Two revised electrodes required an additional revision. The primary reason for revisions was inadequate force production (less than 4 out of 5 for knee extension and less than 2 out of 5 for all other motions) of an electrode post-operatively. Following these revisions, all electrodes functioned without further incident. Table 7 indicates the MMT grades for all stimulated muscles for each subject following the training period.
Subjects 3 and 4 demonstrated the ability to stand with FES. However, they were unable to complete training and data collection. Following bilateral derotational tibial osteotomies, subject 3 developed a pressure sore and increased spasticity, which interfered with his completion of training and a necessary revision to one electrode to the femoral nerve. Family issues prevented him from returning to continue with training. Subject 4, a college student, had some personal difficulties that prevented him from returning during his break from school to complete the training, which was the original plan. He did return for training at a later date during another school break but was having significantly increased spasticity at that time, causing one lower extremity to move into flexion while standing with FES.
Discussion
The subjects in this study made important functional gains using the FES system. Four of the eight tested activities were performed faster with FES. Donning was faster with FES thus providing the ability to prepare for standing in a more timely manner. The stand and reach and high transfer activities were faster, thus providing a quicker transition to being upright, allowing performance of important activities involving reaching items inaccessible from the wheelchair and transferring to a higher surface, such as a sport utility vehicle. In addition, subjects gained greater independence in five activities, therefore demanding less physical assistance from a caregiver. Four of the younger subjects who required assistance to stand from the wheelchair with LLB were able to perform this with FES without any physical assistance. The sit to stand activity was potentially made easier as standing up from the wheelchair in a flexed knee position with FES is less demanding on the upper extremities than standing up with the knees locked in extension with LLB.
In this study, FES was able to address several of the issues reported to be related to abandonment of LLB. Donning of the system became less difficult as indicated by increased independence. By eliminating the need for LLB that crossed the hip and/or knee, the bulkiness was decreased, allowing subjects to wear the FES components beneath the clothing. Subjects could also utilize their regular wheelchairs without modifications that increase the width, therefore providing a wheelchair that best met their functional needs for activities in the wheelchair and in standing. Longer-term follow-up will ascertain if these benefits do lead to a decrease in abandonment of FES as compared to LLB.
In comparing this study to our earlier work with percutaneous FES,1 the functional results are similar for the majority of activities tested. Two trends in the current study that differed were the increase in level of independence for the activities involving sit to stand transitions when using FES and the ability to don the FES system with greater independence than with LLB. This was likely due to the inclusion of younger children and subjects with higher level injuries (C7 to T1).
Historically, it has been shown that the achievement of knee and hip extension for this population is critical in order to obtain good standing posture with FES. Therefore, the techniques to create these movements are important to the success of an FES system. Different approaches have been taken to achieve these.
In our study, we chose to first implant an electrode near the femoral nerve for stimulated knee extension, releasing the proximal rectus femoris muscle in order to avoid hip flexion with stimulation. This technique did allow us to use one electrode to effectively stimulate the quadriceps group. Therefore, we were able to avoid stimulated hip flexion in standing when stimulating the rectus femoris as reported in the study by Kobetic et al,14 which limited standing time and increased the demand on the upper extremities. Our recent change to implanting the vastus lateralis in subject 9 also avoided the problem of hip flexion in standing and demonstrated that sufficient knee extension force for standing could be obtained by implanting this muscle, which concurs the work reported by Davis et al17 and Uhlir et al.16 Davis et al17 demonstrated that standing could be achieved by implanting the vastus lateralis for knee extension in seven subjects. In the study by Uhlir et al, three out of four subjects obtained sufficient force for standing when using the vastus lateralis. The fourth subject was within 10% of the force needed using both the vastus lateralis and medialis. They reported that a minimum of 40 Nm of quadriceps force was needed for standing.16 In our study, it appeared that an MMT grade of 4+/5 to 5/5 was necessary to achieve sufficient quadriceps force for standing.
One problem we encountered with the electrode implanted near the femoral nerve was a decrease in quadriceps force production when the hip was positioned in flexion, the functional position required to begin standing from the wheelchair. Subjects 2 and 3 underwent electrode revisions due to this. Subject 2 experienced the most difficulty, so two electrodes were placed to stimulate the left quadriceps muscles, sacrificing the gluteus medius channel. This phenomenon was observed to a lesser degree with four additional electrodes in other subjects, however, revisions were not required as sufficient knee extension force for standing was retained. Once this problem became apparent, the surgical technique was revised to detect this problem intra-operatively. Prior to identifying the final electrode placement, the response was tested in hip flexion. If the force decreased significantly, a new position that eliminated or minimized the problem was sought for the electrode. In an attempt to alleviate this problem for future subjects, subject 9 received an electrode to the vastus lateralis. One of his vastus lateralis electrodes did require a revision due to a decrease in knee extension force with the hip in flexion or extension 6 weeks postoperatively.
The achievement of hip extension is another critical component for standing in this population to maintain an upright posture. Kobetic et al14 reported that a minimum manual muscle test grade of 3/5 was needed for the hip extensors to provide an upright posture in standing. In our study, the manual muscle test grades for the gluteus maximus and the posterior fibers of the adductor magnus ranged from 2/5 to 3−/5. However, we did implant two muscles for hip extension as compared to one muscle in the study by Kobetic et al,14 which likely increased the total hip extension force. Implanting two hip extensors combined with the release of the recturs femoris (and most recently implanting the vastus lateralis) appeared to provide good upright posture with little arm fatigue. Kobetic et al14 reported arm fatigue which was felt to be related to insufficient hip extension force and recruitment of the hip flexors.
As more knowledge was gained regarding electrode placement and the functional effects, several important considerations emerged regarding balanced muscle responses around a joint. For example, balancing the external rotation obtained from the gluteus maximus with the internal rotation of the gluteus medius enabled the subject to stand and walk with the foot progression angle in neutral or a small amount of external rotation. Functionally, excessive external rotation caused the subject to hit the walker with the feet when advancing the lower extremities. Therefore, an electrode was implanted in the anterior fibers of the gluteus medius in order to obtain hip abduction and internal rotation. If excessive external rotation in standing were still problematic, it could be partially compensated for by increasing the stimulation to the adductor magnus to bring the lower extremities closer together or by using a wider walker. No revisions to electrodes were performed due to excessive external rotation. However, the subjects who displayed this problem did express that less external rotation would be helpful. Subject 3 did undergo bilateral derotational tibial osteotomies after receiving the implant, due to excessive external tibial torsion which caused his lower extremities to contact the walker when standing and walking. In all subsequent subjects, the need for this procedure was assessed pre-operatively. As a result, subject 7 received bilateral derotational tibial osteotomies during the surgery to implant the FES system.
Another balance found to be important was hip abduction and adduction. One earlier subject obtained minimal adduction from the posterior fibers of adductor magnus. This caused her lower extremities to abduct over time as she continued walking, limiting her walking distance. As this was the subject with tetraplegia, she did not have the upper body strength to compensate for this problem. This issue did not affect her ability to stand from the wheelchair. A revision to the electrode was offered to this subject but she declined, not wanting to go through another operative procedure. Longer distance ambulation was not one of her goals, so the revision was not necessary in order for her to use the system as she desired.
While not formally measured, subjects demonstrated the ability to stand with FES for longer periods of time than were tested in this study. Across all subjects, standing time ranged from approximately 5 to 45 min. Using this open loop system, three of the younger children were able to stand and walk for up to 45 min, which involved walking to different activities in close proximity and then performing the activities while standing. Most of this involved play activities, activities around a classroom or kitchen, and activities with other children or a parent. Davis et al15 demonstrated that an adult could stand with FES with a closed loop system for up to 1 h. One 20-year-old subject in our study, who desired longer distance walking, consistently demonstrated the ability to ambulate 87 m using a swing through gait pattern with loftstrand crutches without physical assistance, demonstrating the feasibility of walking longer distances than were tested in this study.
Conclusion
The subjects in this study made important functional gains with the implanted FES system as compared to LLB and preferred FES for the majority of the activities. Electrode positioning was refined and the changes in methods evolved throughout the study. Results of this study suggest that an implanted FES system is a realistic alternative for upright mobility for children and adolescents with paraplegia.
References
Bonaroti DM et al. Comparison of functional electrical stimulation to long leg braces for upright mobility for children with complete thoracic spinal cord injuries. Arch Phys Med Rehabil 1999; 80: 1047–1053.
O'Daniel WE & Hahn HR . Follow-up usage of the Scott-Craig Orthosis in paraplegia. Paraplegia 1981; 19: 373–378.
Heinnemann AW, Mageira-Planey R, Schiro-Geist C & Gimines G . Mobility for persons with spinal cord injury: an evaluation of two systems. Arch Phys Med Rehabil 1987; 68: 90–93.
Sykes L, Edwards J, Powell ES & Ross RS . The reciprocating gait orthosis: long-term usage patterns. Arch Phys Med Rehabil 1995; 76: 779–783.
Brissot R et al. Clinical experience with functional electrical stimulation-assisted gait with Parastep® in spinal cord-injured patients. Spine 2000; 25: 501–508.
Klose KJ et al. Evaluation of a training program for persons with SCI paraplegia using the Parastep® ambulation system: part 1: ambulation performance and anthropometric measures. Arch Phys Med Rehabil 1997; 78: 780–793.
Kralj A et al. Gait restoration in paraplegic subjects: a feasibility demonstration using multichannel surface electrode FES. J Rehabil RD 1983; 20: 3–20.
Shimada Y et al. Clinical use of percutaneous intramuscular electrodes for functional electrical stimulation. Arch Phys Med Rehabil 1996; 77: 1014–1018.
Mulcahey MJ & Betz RR . Upper and lower extremity applications of functional electrical stimulation: a decade of research with children and adolescents with spinal injuries. Pediatr Phys Ther 1997; 9: 113–122.
Bonaroti D et al. A comparison of FES with KAFO for providing ambulation and upright mobility in a child with a complete thoracic spinal cord injury. J of Spinal Cord Med 1999; 22: 159–166.
Kobetic R & Marsolais EB . Synthesis of paraplegic gait with multichannel functional neuromuscular stimulation. IEEE Trans Rehab Eng 1994; 2: 66–79.
Moynahan M et al. Home use of a functional electrical stimulation system for standing and mobility in adolescents with spinal cord injury. Arch Phys Med Rehabil 1996; 77: 1005–1013.
Kobetic R, Triolo R & Marsolais EB . Muscle selection and walking performance of multichannel FES system for ambulation in paraplegia. IEEE Trans Rehab Eng 1997; 5: 23–29.
Kobetic R et al. Implanted functional electrical stimulation system for mobility in paraplegia: a follow-up case report. IEEE Trans Rehab Eng 1999; 7: 390–398.
Davis R, Houdayer T, Andrews B & Barriskill A . Paraplegia: prolonged standing using closed loop functional electrical stimulation and Andrews ankle-foot orthosis. Artificial Organs 1999; 23: 418–420.
Uhlir JP, Triolo RJ & Kobetic R . The use of selective electrical stimulation of the quadriceps to improve standing function in paraplegia. IEEE Trans Rehab Eng 2000; 8: 514–522.
Davis JA et al. Surgical technique for installing an eight-channel neuroprosthesis for standing. Clin Orthop 2001; 385: 237–252.
Smith BT et al. A portable 24 channel functional electrical stimulation system for upper and lower extremity applications. The Proceedings of the RESNA Conference 1996; 276–278.
Miyamoto S et al. Hybrid functional electrical stimulation for energy-efficient restoration of standing-up motion. Arch Phys Med Rehabil 1999; 80: 40–47.
Memberg W, Peckham PH & Keith MW . A surgically implanted intramuscular electrode for an implantable neuromuscular stimulation system. IEEE Trans Rehab Eng 1994; 2: 80–91.
Akers JM, Smith BT & Betz RR . Implantable electrode lead in a growing limb. IEEE Trans Rehab Eng 1999; 7: 35–45.
Malina RM & Bouchard C . Biological maturation: concept and assessment.. In:Growth, Maturation, and Physical Activity. 1st edn. Champaign, IL: Human Kinetics Books, 1993; pp 231–249.
Kendall FP, McCreary EK & Provance PG . Muscles: Testing and Functio, (4th edn). Baltimore, MD: Williams and Wilkins, 1993.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Johnston, T., Betz, R., Smith, B. et al. Implanted functional electrical stimulation: an alternative for standing and walking in pediatric spinal cord injury. Spinal Cord 41, 144–152 (2003). https://doi.org/10.1038/sj.sc.3101392
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101392
Keywords
This article is cited by
-
Boosting brain–computer interfaces with functional electrical stimulation: potential applications in people with locked-in syndrome
Journal of NeuroEngineering and Rehabilitation (2023)
-
The role of electrical stimulation for rehabilitation and regeneration after spinal cord injury
Journal of Orthopaedics and Traumatology (2022)
-
“Long-term stability of stimulating spiral nerve cuff electrodes on human peripheral nerves”
Journal of NeuroEngineering and Rehabilitation (2017)
-
In vivo 31P NMR spectroscopy assessment of skeletal muscle bioenergetics after spinal cord contusion in rats
European Journal of Applied Physiology (2014)
-
Pediatric Spinal Cord Injury
Current Physical Medicine and Rehabilitation Reports (2014)