Summary:
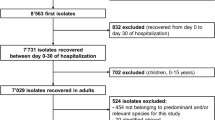
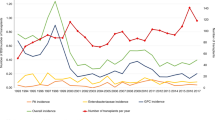
Following the closure of the National Blood and Bone Marrow Transplant Unit in Dublin, because of an outbreak of vancomycin-resistant enterococcal infection, a survey was carried out by the EBMT to investigate the occurrence of outbreaks of infection in SCT units and the impact on patient morbidity, mortality and the administration of the transplant programme over a 10-year period from 1991 to 2001. A total of 13 centres reported 23 outbreaks of infection involving 231 patients: 10 bacterial, eight viral and five fungal outbreaks were reported and 56 deaths were attributed to infection. All fungal and bacterial deaths and the majority of viral deaths occurred in allograft recipients. In all outbreaks, the infection was reported to be hospital acquired and in all the viral, and half the bacterial infections, cross-infection was a major factor. All viral, four of 10 bacterial and three of five fungal outbreaks occurred in HEPA filtered rooms. A total of 12 SCT units reported a partial or total closure. The introduction of mandatory quality management systems such as JACIE should result in a change in attitude to ‘incident reporting’ and together with future surveys should reduce the incidence of infectious outbreaks in SCT units.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Donnelly JP . Bacterial complications of transplantation: diagnosis and treatment. J Antimicrob Chemother 1995; 36: 59–72.
Jantunen E, Ruutu P, Niskanen L et al. Incidence and risk factors for invasive fungal infection in allogeneic BMT recipients. Bone Marrow Transplant 1997; 19: 801–808.
Bostrom L, Ringden O . Viral infections. Clinical bone marrow and blood stem cell transplantation. In: Atkinson K (ed.). Major Transplant Related Problems, Part VIII. Cambridge University Press: Cambridge, 2000, pp 758–782.
Offner F, Cordonnier C, Ljungman P, et al., on behalf of the EBMT-EORTC Joint Project on Aspergillosis prior to BMT. Impact of previous aspergillosis on the outcome of bone marrow transplantation. Clin Infect Dis 1998; 26: 1098–1103.
Gerson SL, Talbot GH, Hurwitz S et al. Prolonged granulocytopenia: the major risk factor for invasive pulmonary aspergillosis in patients with acute leukaemia. Ann Intern Med 1984; 100: 345.
Sayer HG, Longton G, Bowden R et al. Increased risk of infection in marrow transplant patients receiving methylprednisolone for graft-vs-host disease prevention. Blood 1994; 84: 1328.
Giralt S . Complications of non-myeloablative stem cell transplantation. In: Giralt S, Slavin S (eds.). Non-myeloablative stem cell transplantation (NST). Darwin Scientific Publishing Limited: Oxfordshire, UK, 2000, pp 139–148.
Birchard K . Irish bone marrow transplant unit closes. Lancet 2000; 356: 1012.
Gratwohl A, McCann S, Byrne JL et al. Outbreaks of infectious disease in stem cell transplant units: a silent cause of death for patients and transplant programmes. Bone Marrow Transplant 2002; 29 (Suppl. 2): 303.
Cornet M, Levy V, Lortholary J et al. Efficacy of prevention by high-efficiency particulate air filtration or laminar airflow against Aspergillus airborne contamination during hospital renovation. Infect Control Hosp Epidemiol 1999; 20: 508–513.
Sherertz RJ, Belani A, Kramer BS, Elfenbein GJ . Impact of air filtration on nosocomial aspergillus infections unique risk of bone marrow transplant recipients. Am J Med 1987; 83: 709.
Dykewicz CA . Hospital infection control of hematopoietic stem cell transplant recipients. Centres for Disease Control and Prevention, Atlanta, GA, USA 2001; 7: 2.
Withington S, Chambers ST, Beard ME et al. Invasive aspergillosis in severely neutropenic patients over 18 years; impact of intranasal amphotericin B and HEPA filtration. J Hosp Infect 1998; 38: 11.
Wald A, Leisenring W, von Burik JA, Bowden RA . Epidemiology of Aspergillus infections in a large cohort of patients undergoing bone marrow transplantation. J Infect Dis 1997; 175: 1459.
Streifel AJ, Marshall JW . Parameters for ventilation controlled environments in hospitals. In: Moschandreas DJ (ed.). Design, Construction and Operation of Healthy Buildings. Solutions to Global and Regional Concerns. American Society of Heating, Refrigeration and Air-Conditioning Engineers Press: Atlanta, 1998, pp 305–309.
Opal SM, Asp AA, Cannady PB et al. Efficacy of infection control measures during a nosocomial outbreak of disseminated aspergillosis associated with hospital construction. J Infect Dis 1986; 153: 634–637.
Anaissie EJ, Costa SF . Nosocomial aspergillosis is waterborne. Clin Infect Dis 2001; 33: 1546–1548.
Weems JJ, Davis Jr BJ, Tablan OC et al. Construction activity: an independent risk factor for invasive aspergillosis and zygomycosis in patients with hematologic malignancy. Infect Control 1987; 8: 71–75.
Wingard JR, Beals SU, Santos GW et al. Aspergillus infections in bone marrow transplant recipients. Bone Marrow Transplant 1987; 2: 175.
Chazalet V, Debeaupuis JP, Sarfati J et al. Molecular typing of environmental and patient isolates of Aspergillus fumigatus from various hospital settings. J Clin Miocrobiol 1998; 36: 1494–1500.
Hospenthal DR, Kwon-Chung KJ, Bennet JE . Concentrations of airborne Aspergillus compared to the incidence of invasive aspergillosis: lack of correlation. Med Mycol 1998; 36: 165–168.
Vesley D, Streifel AJ . Environmental services. In: Mayhall CB (ed.). Hospital Epidemiology and Infection Control, 2nd edn. Lippincott, Williams & Wilkins: Philadelphia, 1999, pp 1047–1053.
Garner JS . The Hospital Infection Control Practices Advisory Committee Guideline for isolation precautions in hospitals. Infect Control Hosp Epidemiol 1996; 17: 1–80.
CDC. Recommendations for preventing opportunistic infections in stem cell transplant recipients; recommendations of the Infectious Disease Society of America and the American Society of Blood and Bone Marrow. Morb Mortal Wkly Rep 2000; 49: 1–128.
Passweg JR, Rowlings PA, Atkinson KA et al. Influence of protective isolation on outcome of allogeneic bone marrow transplantation for leukaemia. Bone Marrow Transplant 1998; 21: 1231.
Barbaric D, Shaw PJ . Scedosporium infection in immunocompromised patients: successful use of liposomal amphotericin B and intraconazole. Med Pediatr Oncol 2000; 37: 122–125.
Alvarez M, Ponga BL, Rayon C et al. Nosocomial outbreak caused by Scedosporium prolificans (inflatum): four fatal cases in leukaemia patients. J Clin Microbiol 1995; 33: 3290–3295.
Orth B, Frei R, Itin PH et al. Outbreak of invasive mycoses caused by Paecilomyces lilancinus from a contaminated skin lotion. Ann Intern Med 1996; 125: 799–806.
Zambon M, Bull T, Sadler CJ et al. Molecular epidemiology of two consecutive outbreaks of parainfluenza 3 in a bone marrow transplant unit. J Clin Microbiol 1998; 36: 2289–2293.
Lewis VA, Champlin R, Englund J et al. Respiratory disease due to parainfluenza virus in adult bone marrow transplant recipients. Clin Infect Dis 1996; 23: 1033–1037.
Wendt CH, Weisdorf DJ, Jordan MC et al. Parainfluenza virus respiratory infection after bone marrow transplantation. N Engl J Med 1992; 326: 921–926.
Whimpey E, Vartivarian SE, Champlin RE et al. Parainfluenza virus infection in adult bone marrow transplant recipients. Eur J Clin Microbiol 1993; 19: 699–701.
Garcia R, Raad I, Abi-Said D et al. Nosocomial respiratory syncytial virus infections. Infect Control Hosp Epidemiol 1997; 18: 412–416.
Champlin E, Whimbey E . Community respiratory virus infections in bone marrow transplant recipients: The M.D. Anderson Cancer Center Experience. Biol Blood Marrow Transplant 2001; 7: 8S–10S.
Harrington R, Hooton TM, Hackman RC et al. An outbreak of respiratory syncytial virus in a bone marrow transplant center. J Infect Dis 1992; 165: 987–993.
Cubitt WD, Mitchell DK, Carter MJ et al. Application of electronmicroscopy, enzyme immunoassay, and RT-PCR to monitor an outbreak of astrovirus type 1 in a paediatric bone marrow transplant unit. J Med Virol 1999; 57: 313–321.
Hall C . Respiratory syncytial virus and parainfluenza virus. N Engl J Med 2001; 344: 1917–1928.
Whimbey E, Ghosh S . Respiratory syncytial virus infections in immuno-compromised adults. Curr Clin Top Infect Dis 2000; 20: 232–255.
Wendt CH, Hertz MI . Respiratory syncytial virus and parainfluenza virus infections in the immunocompromised host. Semin Respir Infect 1995; 10: 224–231.
Knowles S, Herra C, Devitt E et al. An outbreak of multiply resistant Serratia marcescens: the importance of persistent carriage. Bone Marrow Transplant 2000; 25: 873–877.
Klausner JD, Zukerman C, Limaye AP, Corey L . Outbreak of Stenrophomonas maltophilia bacteremia among patients undergoing bone marrow transplantation: association with faulty replacement of handwashing soap. Infect Control Hosp Epidemiol 1999; 20: 756–758.
Murray BE . Vancomycin-resistant enterococci. Am J Med 1997; 102: 284–293.
Uttley AHC, Collins CH, Naidoo J, George RC . Vancomycin-resistant enterococci. Lancet 1988; 1: 57–58.
McAlister T, George N, Faoagali J, Bell J . Isolation of β-lactamase positive vancomycin resistant Enterococcus faecalis; first case in Australia. Commun Dis Intell 1999; 23: 237–239.
Kirpatrick BD, Harrington SM, Smith D et al. An outbreak of vancomycin-dependent Enterococcus faecium in a bone marrow transplant unit. Clin Infect Dis 1999; 29: 1268–1273.
CDC. Recommendations for preventing the spread of vancomycin resistance; recommendations of the hospital infection control practices advisory committee. Morb Mortal Wkly Rep 1995; 44: 1–13.
Acknowledgements
We thank the following for completing the questionnaire and for providing data: P Browne, St James's Hospital, Dublin, Ireland; JL Byrne, Nottingham City Hospital, Nottingham, UK; C Cordonnier, Hopital Henri Mondor, Paris, France; A Gratwohl, Kantonsspital, Basel, Switzerland; P Ljungman, Huddinge University Hospital, Huddinge, Sweden; S Mackinnon, University College Hospital, London, UK; E Olavarria, Imperial College School of Medicine, London, UK; P Ribaud, Hopital Saint-Louis, Paris, France; M Rovira, Hospital Clinic, Barcelona, Spain; P Shaw, The New Children's Hospital, Sydney, Australia; S Sica, Universita Cattolica, S Cuore, Rome, Italy; P Trabasso, Cicade Universitaria Zeferino Vaz, Sao Paolo, Brazil; MT Van Lint, Ospedale San Martino, Genoa, Italy; L Volin, Helsinki University Central PO, Helsinki, Finland; and K Ward, Windeyer Building, London, UK. We also thank the Department of Microbiology and Infection Control in St James's Hospital, Dublin for the detailed information on the VRE outbreak in Dublin. We also thank the PHLS, Central Public Health Laboratories, Colindale, for carrying out the molecular typing of enterococci.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
McCann, S., Byrne, J., Rovira, M. et al. Outbreaks of infectious diseases in stem cell transplant units: a silent cause of death for patients and transplant programmes. Bone Marrow Transplant 33, 519–529 (2004). https://doi.org/10.1038/sj.bmt.1704380
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1704380
Keywords
This article is cited by
-
Characteristics of viral pneumonia in non-HIV immunocompromised and immunocompetent patients: a retrospective cohort study
BMC Infectious Diseases (2021)
-
Taxonomy
Bone Marrow Transplantation (2020)
-
The good, the bad and the ugly
Bone Marrow Transplantation (2018)
-
Infectious diseases in allogeneic haematopoietic stem cell transplantation: prevention and prophylaxis strategy guidelines 2016
Annals of Hematology (2016)
-
Fungal and viral infections after allogeneic hematopoietic transplantation from unrelated donors in adults: improving outcomes over time
Bone Marrow Transplantation (2015)