Abstract
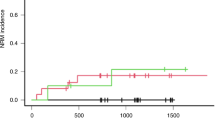
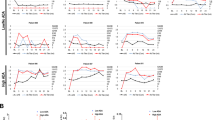
Allogeneic hematopoietic cell transplantation (HCT) is the only treatment for selected inherited metabolic storage diseases (IMSD); a significant shortcoming is failure to achieve donor-derived engraftment. This study was undertaken to determine whether busulfan pharmacokinetics (BU PK) are altered in children with IMSD and whether BU concentrations are important in achieving engraftment. BU samples were obtained from 39 IMSD children, including 20 children with Hurler syndrome, undergoing HCT. Patients received oral BU (40 mg/m2/dose × 8 doses), cyclophosphamide (60 mg/kg/day × 2 doses) and TBI (750 cGy in one fraction) as a preparative regimen. Median (range) oral clearance corrected for bioavailability (Cl/F in ml/min/kg), area under the curve (AUC in ng min/ml) and BU plasma concentration (Cp in ng/ml) with the fourth dose were 5.2 (2.1–11.4), 318 294 (112 893–640 995) and 950 (314–1780), respectively. Children <3 years of age had lower AUC and Cp but higher Cl/F (P ⩽ 0.03). BU Cp (P = 0.06) or marrow cell dose (P = 0.32) was not different in Hurler syndrome compared to other IMSD. A median BU Cp of 959 and 831 ng/ml was achieved in children with full and failed early engraftment, respectively. There was no difference in early and late engraftment between children with Hurler and other IMSD. In conclusion, we found no significant association between engraftment, marrow cell dose and BU exposure when combined with CY and TBI in children with IMSD. Bone Marrow Transplantation (2001) 27, 855–861.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Hobbs JR, Hugh-Jones K, Barrett AJ et al. Reversal of clinical features of Hurler's disease and biochemical improvement after treatment by bone-marrow transplantation Lancet 1981 2: 709–712
Krivit W, Pierpont ME, Ayaz K et al. Bone-marrow transplantation in the Maroteaux–Lamy syndrome (mucopoly-saccharidosis type VI). Biochemical and clinical status 24 months after transplantation New Engl J Med 1984 311: 1606–1611
Wall DA, Grange DK, Goulding P et al. Bone marrow transplantation for the treatment of alpha-mannosidosis J Pediatr 1998 133: 282–285
Aubourg P, Blanche S, Jambaque I et al. Reversal of early neurologic and neuroradiologic manifestations of X-linked adrenoleukodystrophy by bone marrow transplantation New Engl J Med 1990 322: 1860–1866
Krivit W, Shapiro E, Kennedy W et al. Treatment of late infantile metachromatic leukodystrophy by bone marrow transplantation (see comments) New Engl J Med 1990 322: 28–32
Krivit W, Shapiro EG, Peters C et al. Hematopoietic stem-cell transplantation in globoid-cell leukodystrophy New Engl J Med 1998 338: 1119–1126
Peters C, Balthazor M, Shapiro EG et al. Outcome of unrelated donor bone marrow transplantation in 40 children with Hurler syndrome Blood 1996 87: 4894–4902
Peters C, Shapiro EG, Anderson J et al. Hurler syndrome: II. Outcome of HLA-genotypically identical sibling and HLA-haploidentical related donor bone marrow transplantation in fifty-four children. The Storage Disease Collaborative Study Group Blood 1998 91: 2601–2608
Vassal G, Deroussent A, Challine D et al. Is 600 mg/m2 the appropriate dosage of busulfan in children undergoing bone marrow transplantation? Blood 1992 79: 2475–2479
Yeager AM, Wagner JE Jr, Graham ML et al. Optimization of busulfan dosage in children undergoing bone marrow transplantation: a pharmacokinetic study of dose escalation Blood 1992 80: 2425–2428
Regazzi MB, Locatelli F, Buggia I et al. Disposition of high-dose busulfan in pediatric patients undergoing bone marrow transplantation Clin Pharmacol Ther 1993 54: 45–52
Hassan M, Oberg G, Bekassy AN et al. Pharmacokinetics of high-dose busulphan in relation to age and chronopharmacology Cancer Chemother Pharmacol 1991 28: 130–134
Gibbs JP, Liacouras CA, Baldassano RN, Slattery JT . Up-regulation of glutathione S-transferase activity in enterocytes of young children Drug Metab Dispos 1999 27: 1466–1469
Czerwinski M, Gibbs JP, Slattery JT . Busulfan conjugation by glutathione S-transferases alpha, mu, and pi Drug Metab Dispos 1996 24: 1015–1019
Slattery JT, Sanders JE, Buckner CD et al. Graft-rejection and toxicity following bone marrow transplantation in relation to busulfan pharmacokinetics (published erratum appears in Bone Marrow Transplant 1996 Oct;18(4):829) Bone Marrow Transplant 1995 16: 31–42
Byrne JL, Stainer C, Cull G et al. The effect of the serotherapy regimen used and the marrow cell dose received on rejection, graft-versus-host disease and outcome following unrelated donor bone marrow transplantation for leukaemia Bone Marrow Transplant 2000 25: 411–417
Ringden O, Remberger M, Runde V et al. Peripheral blood stem cell transplantation from unrelated donors: a comparison with marrow transplantation Blood 1999 94: 455–464
Gorin NC, Labopin M, Laporte JP et al. Importance of marrow dose on posttransplant outcome in acute leukemia: models derived from patients autografted with mafosfamide-purged marrow at a single institution Exp Hematol 1999 27: 1822–1830
Reisner Y, Martelli MF . Stem cell escalation enables HLA-disparate haematopoietic transplants in leukaemia patients Immunol Today 1999 20: 343–347
Cornetta K, Gharpure V, Mills B et al. Rapid engraftment after allogeneic transplantation using CD34-enriched marrow cells Bone Marrow Transplant 1998 21: 65–71
Clarke E, Potter MN, Hale G et al. Double T cell depletion of bone marrow using sequential positive and negative cell immunoaffinity or CD34+ cell selection followed by Campath-1M; effect on CD34+ cells and progenitor cell recoveries Bone Marrow Transplant 1998 22: 117–124
O'Donnell PV, Jones RJ, Vogelsang GB et al. CD34+ stem cell augmentation of elutriated allogeneic bone marrow grafts: results of a phase II clinical trial of engraftment and graft-versus-host disease prophylaxis in high-risk hematologic malignancies Bone Marrow Transplant 1998 22: 947–955
Wagner JE, Santos GW, Noga SJ et al. Bone marrow graft engineering by counterflow centrifugal elutriation: results of a phase I–II clinical trial Blood 1990 75: 1370–1377
Slattery JT, Risler LJ . Therapeutic monitoring of busulfan in hematopoietic stem cell transplantation Ther Drug Monit 1998 20: 543–549
Snedecor G, Cochran W . Statistical Methods, 8th edn Iowa State University Press: Ames, IA 1989
Kaplan EM, Meier P . Non parametric estimation from incomplete observations J Am Stat Assoc 1958 53: 457
Vassal G, Fischer A, Challine D et al. Busulfan disposition below the age of three: alteration in children with lysosomal storage disease Blood 1993 82: 1030–1034
Grochow LB, Krivit W, Whitley CB, Blazar B . Busulfan disposition in children Blood 1990 75: 1723–1727
Hassan M, Fasth A, Gerritsen B et al. Busulphan kinetics and limited sampling model in children with leukemia and inherited disorders Bone Marrow Transplant 1996 18: 843–850
Bolinger AM, Zangwill AB, Slattery JT et al. An evaluation of engraftment, toxicity and busulfan concentration in children receiving bone marrow transplantation for leukemia or genetic disease Bone Marrow Transplant 2000 25: 925–930
Pawlowska AB, Blazar BR, Angelucci E et al. Relationship of plasma pharmacokinetics of high-dose oral busulfan to the outcome of allogeneic bone marrow transplantation in children with thalassemia Bone Marrow Transplant 1997 20: 915–920.
Gupta P, McCarthy JB, Verfaillie CM . Stromal fibroblast heparan sulfate is required for cytokine-mediated ex vivo maintenance of human long-term culture-initiating cells Blood 1996 87: 3229–3236
Gupta P, Oegema TR Jr, Brazil JJ et al. Structurally specific heparan sulfates support primitive human hematopoiesis by formation of a multimolecular stem cell niche Blood 1998 92: 4641–4651
Ringden O, Remberger M, Ruutu T et al. Increased risk of chronic graft-versus-host disease, obstructive bronchiolitis, and alopecia with busulfan versus total body irradiation: long-term results of a randomized trial in allogeneic marrow recipients with leukemia. Nordic Bone Marrow Transplantation Group (see comments) Blood 1999 93: 2196–2201.
Styler MJ, Crilley P, Biggs J et al. Hepatic dysfunction following busulfan and cyclophosphamide myeloablation: a retrospective, multicenter analysis Bone Marrow Transplant 1996 18: 171–176
Ozkaynak MF, Weinberg K, Kohn D et al. Hepatic veno-occlusive disease post-bone marrow transplantation in children conditioned with busulfan and cyclophosphamide: incidence, risk factors, and clinical outcome Bone Marrow Transplant 1991 7: 467–474
Brodsky R, Topolsky D, Crilley P et al. Frequency of veno-occlusive disease of the liver in bone marrow transplantation with a modified busulfan/cyclophosphamide preparative regimen Am J Clin Oncol 1990 13: 221–225
Hartman AR, Williams SF, Dillon JJ . Survival, disease-free survival and adverse effects of conditioning for allogeneic bone marrow transplantation with busulfan/cyclophosphamide vs total body irradiation: a meta-analysis Bone Marrow Transplant 1998 22: 439–443
Bandini G, Belardinelli A, Rosti G et al. Toxicity of high-dose busulphan and cyclophosphamide as conditioning therapy for allogeneic bone marrow transplantation in adults with haematological malignancies Bone Marrow Transplant 1994 13: 577–581
Acknowledgements
We wish to thank the nursing staff in the Pediatric Blood and Marrow Transplant Unit at Fairview-University Medical Center for the collection of blood samples and to recognize our collaborators at Duke University, All Children's Hospital in St Petersburg, FL, and Children's Hospital of Philadelphia for contributing patient samples for pharmacokinetic analysis. This work was supported in part by a grant from the Children's Cancer Research Fund (CP) and by National Institutes of Health Grant No. NS-29099 (WK).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Jacobson, P., Park, J., DeFor, T. et al. Oral busulfan pharmacokinetics and engraftment in children with Hurler syndrome and other inherited metabolic storage diseases undergoing hematopoietic cell transplantation. Bone Marrow Transplant 27, 855–861 (2001). https://doi.org/10.1038/sj.bmt.1703010
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1703010
Keywords
This article is cited by
-
Busulfan systemic exposure and its relationship with efficacy and safety in hematopoietic stem cell transplantation in children: a meta-analysis
BMC Pediatrics (2020)
-
Combination of enzyme replacement and hematopoietic stem cell transplantation as therapy for Hurler syndrome
Bone Marrow Transplantation (2008)
-
Transplantation of allogeneic CD34-selected stem cells after fludarabine-based conditioning regimen for children with mucopolysaccharidosis 1H (M. Hurler)
Bone Marrow Transplantation (2005)
-
Allogeneic stem cell transplantation for the treatment of lysosomal and peroxisomal metabolic diseases
Springer Seminars in Immunopathology (2004)
-
Hematopoietic cell transplantation for inherited metabolic diseases: an overview of outcomes and practice guidelines
Bone Marrow Transplantation (2003)