Abstract
Conditioned avoidance response (CAR) behavior and catalepsy (CAT) are the standard preclinical tests used to predict antipsychotic activity and motor side-effect liability, respectively. Recent data in patients show that striatal dopamine D2 occupancy predicts antipsychotic response (at 65% D2 occupancy) and motor side-effects (at greater than 80%). To relate preclinical and clinical findings, this study examined the relationship between striatal D2 occupancy, CAT and CAR in rats receiving typical and atypical antipsychotics. CAT was observed in animals receiving haloperidol, risperidone and olanzapine, but only at doses that produced a D2 receptor occupancy ⩾85%. The D2 occupancy of quetiapine did not cross the 85% threshold (up to 100 mg/kg) and it did not show catalepsy. All drugs were effective in the CAR model at a lower level of D2 occupancy than was required for catalepsy. We suggest that the CAR and CAT models may have displayed high predictive accuracy because they share with the clinical condition a common underlying mechanism: dopamine D2 occupancy. The implications of this finding for understanding antipsychotic action as well as the continued use of these models in drug discovery is discussed.
Similar content being viewed by others
Main
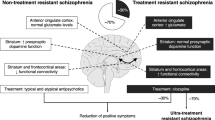
The positron emission tomography (PET) imaging has made it possible to correlate in vivo dopamine (DA) D2 receptor occupancy of antipsychotic drugs with the observed clinical outcome in patients with schizophrenia. Using this technique, Farde et al. (1992) suggested that both antipsychotic response and extrapyramidal side effects (EPS) may be related to D2 receptor occupancy – albeit with different thresholds. With typical antipsychotics, a D2 receptor occupancy in the range of 70% was associated with clinical response while EPS emerged at a D2 receptor occupancy >80% (Farde et al. 1992; Nordstrom et al. 1993). This relationship has been confirmed by subsequent clinical studies. In a double-blind PET study with haloperidol, Kapur et al. found that clinical response was manifest at 65–70% D2 receptor occupancy, but only patients with a D2 receptor occupancy >78% showed signs of EPS (Kapur et al. 2000a).
Newly synthesized potentially antipsychotic drugs are tested in the catalepsy (CAT) test (for EPS liability) and the conditioned avoidance response (CAR) test (for antipsychotic activity) as these tests have high predictive accuracy (Wadenberg 1996; Wadenberg and Hicks 1999). Using a protocol to measure behavior and D2 receptor occupancy in the same animal (rat) in vivo, we recently reported that using the selective DA D2/3 receptor antagonist raclopride, catalepsy was observed only at doses that produced >80% D2 receptor occupancy, while a lower occupancy was sufficient to produce an antipsychotic-like effect in the CAR test (Wadenberg et al. 2000). This finding suggested that the CAR and CAT test may reflect different thresholds of D2 occupancy, and their ability to predict clinical outcomes may be related to this underlying variable. The current study was designed to examine whether this might be true for the clinically relevant typical (haloperidol) and atypical (risperidone, olanzapine and quetiapine) antipsychotics.
The relationship between D2 occupancy and clinical outcome noted for the typical antipsychotic haloperidol also seems to hold for several of the “atypical” antipsychotics, suggesting a continuing role for D2 receptor occupancy. For example, risperidone becomes effective at a dose of 2 mg/day, which is associated with 65% D2 receptor occupancy, while risperidone 6 mg/day leads to a D2 receptor occupancy of >80% and is associated with EPS (Kapur et al. 1999). Olanzapine shows a similar trend—efficacy appears to begin at 10 mg/day, a dose that leads to 70% D2 receptor occupancy while 30–40 mg/day of olanzapine results in D2 receptor occupancy >80% and EPS (Kapur et al. 1999). Quetiapine, on the other hand, produces only modestly high (58–64%) D2 receptor occupancy, and that, too, only transiently (2–3 hours after a single dose), and never exceeds 80%. This might explain why quetiapine does not produce EPS in humans (Kapur et al. 2000b). Thus an examination of the role of D2 occupancy in the context of these newer ‘atypical’ antipsychotics continues to be of great interest.
We were interested in comparing these clinical data with the preclinical situation using the same antipsychotic drugs. Using methods previously standardized (Wadenberg et al. 2000), the present study investigated the relationship between DA D2 receptor occupancy and catalepsy in rats for one typical, haloperidol (Janssen 1967), and three atypical, risperidone (Janssen et al. 1988), olanzapine (Moore et al. 1992), and quetiapine (Migler et al. 1993), antipsychotic compounds. In addition, dose response curves for haloperidol, risperidone, olanzapine, and quetiapine were also established in the conditioned avoidance response test for antipsychotic activity and related to D2 occupancies.
MATERIALS AND METHODS
Animals
Adult male Sprague-Dawley rats, 200–225 g (Charles River, Montréal, Canada) were housed two per cage, in 19 × 10.5 × 8 inches transparent polycarbonate cages (Lab Products Inc., Seaforth, Delaware, USA) under reversed light/dark conditions using a 12-hr on/off schedule (lights off 8 A.M.). Room temperature was maintained at 21±1°C with a relative humidity of 55–60%. Food and water were available ad libitum. The animals were allowed one week of adaptation to laboratory conditions before being used in experiments.
Drugs
Haloperidol, 5 mg/ml ampoules (Sabex Inc., Boucherville, QC, Canada), risperidone (Janssen, Beerse, Belgium), olanzapine (Eli Lilly, Indianapolis, IN, USA), and quetiapine (ICI 204,636) (Zeneca Pharmaceuticals, Macclesfield, Cheshire, England) were used. Haloperidol was diluted with isotone dextrose and given in a volume of 1 mL/kg body weight. Risperidone and quetiapine were dissolved in a minimal amount of glacial acetic acid and made up to volume with physiological saline. Olanzapine was dissolved in propylene glycol. Risperidone, olanzapine and quetiapine were given in a volume of 2 mL/kg body weight. All drugs were administered subcutaneously. [3H] raclopride (NEN Life Sciences, Boston, MA, USA) was used as the radioligand for occupancy studies and given intraveneously in the tail.
Injections and Measurements
The rats were randomized to five different doses of haloperidol (0.025–1.0 mg/kg), six different doses of risperidone (0.05–2.0 mg/kg), five different doses of olanzapine (0.5–10.0 mg/kg), six different doses of quetiapine (5–100 mg/kg), and corresponding vehicle treated control groups. The animals were given an injection of the assigned compound subcutaneously 120 minutes before sacrifice, and received the [3H]-raclopride (7.5 μCi/rat; in a volume of 0.4 mL of 0.9% NaCl solution) injected through a lateral tail vein 30 minutes before sacrifice. The time of 30 minutes before sacrifice was chosen on the basis of previous experiments, where it was observed that the striatal vs. cerebellar uptake ratio for [3H]-raclopride reached a state of equilibrium at this time (Wadenberg et al. 2000).
The rats were tested for catalepsy 110 minutes (haloperidol, risperidone and olanzapine) or 50 minutes (quetiapine) after subcutaneous injection (i.e. 10 minutes before sacrifice and at which time a peak cataleptic effect of the compounds tested was estimated). Animals were sacrificed by decapitation, the brains were immediately removed, and striata and cerebella were rapidly dissected.
After having found a relationship between catalepsy and D2 occupancy, we decided to examine this further by performing a time course using haloperidol. Animals were administered 0.5mg/kg haloperidol subcutaneously and tested for catalepsy at 1 hour post injection (i.e., peak catalepsy) and again, prior to sacrifice at 1, 2, 4, 8 or 24 hours post-injection. Animals were tested two times to avoid artifactual effects of repeated vs. not repeated behavioral testing. The animals received the [3H]-raclopride injected through a lateral tail vein 30 minutes before sacrifice. Animals were sacrificed by decapitation, the brains were immediately removed and striata and cerebella were rapidly dissected.
Measurement of D2 Occupancy
The rats were decapitated and the striata and cerebella were rapidly dissected. The cerebellum was homogenized with a small spatula and approximately one-third (50–100 mg) of this was sampled. The left and right striata were pooled into a single sample (∼ 60 mg). Tissue samples were collected in previously weighed 20 mL glass scintillation vials. The vials were then weighed with tissue and 2 mL of Solvable™ (Canberra Packard, Canada) was added. The vials were kept on an automated shaking-tray, and gently agitated for 24 hours at 23°C. Thereafter, 5 mL of Aquasure™ (formerly Formula 965, Canberra Packard, Canada) scintillation fluid was added, and the mixture was allowed to mix for another 24 hours. Quantitation of [3H] radioactivity was determined by liquid scintillation spectrometry using a Beckman LS5000 CE liquid scintillation counting system at 50% efficiency. Striatal and cerebellar counts were obtained and expressed as disintegrations per min/milligram (DPM/mg) for future calculations.
The D2 receptor binding potential was obtained for each of the animals as Striatum-Cerebellum/Cerebellum. The value for the vehicle-treated control group was pooled, and the occupancy in each rat was then determined using the same formula as used in human studies (Farde et al. 1988; Kapur et al. 1999): % Occupancy = 100 × (D2BPcontrol − D2BPindiv / D2BPcontrol). For further details on the protocol for receptor occupancy assessment, see (Wadenberg et al. 2000).
Catalepsy Measurements
Animals were placed on an inclined (60°) grid and observed by a rater blind to the treatment-assignment status of the animals. To establish a reliable baseline, the first 30 seconds were excluded from the actual rating time. The time the rat remained in the same position was then measured for a maximum of 2.5 min. The catalepsy was scored from 0–5 according to the time (square root transformation) the animal remained immobile (min): 0 = 0–0.08, 1 = 0.09–0.35, 2 = 0.36–0.80, 3 = 0.81–1.42, 4 = 1.43–2.24, 5 = ⩾ 2.25 min. For example, if the rat remained immobile for >2.25 min it was scored as 5, etc. (Ahlenius and Hillegaart 1986). An animal was considered cataleptic with a score greater than or equal to 2.
Conditioned Avoidance Response Behavior
Rats were trained and tested in a computer assisted 2-way active avoidance (shuttlebox) apparatus equipped with a tilting grid floor, with microswitch detection, connected to a high resistance power supply. The boxes were divided into two compartments of equal size by a partition with one opening. Upon presentation of the 80 dB white noise conditioned stimulus (CS), the animals had 10 seconds to move from one compartment of the shuttlebox into the other. If the rat remained in the same compartment for more than 10 seconds, the unconditioned stimulus (UCS), an intermittent electric shock (approx. 0.6 mA of 0.5-sec duration; intershock interval 2.5 sec), was presented in the grid floor until an escape was performed. If the animal did not respond within 50 seconds of the shock period, the trial was terminated (escape failure). Intertrial intervals varied at random between 20 and 40 seconds. The following variables were recorded: avoidance (response to CS within 10 sec), escape (response to CS+UCS), escape failure (failure to respond), and intertrial crosses. The animals were trained for five consecutive days. Experimental manipulations were always preceded by a pretest. All pretest and experimental sessions were run for 10 minutes (Wadenberg et al. 1997a). The same animals were tested repeatedly according to a change-over design serving as their own controls.
Statistics
For catalepsy studies, the statistical analysis was performed by means of the Kruskal-Wallis one-way ANOVA by ranks followed by the Mann-Whitney U-test for comparisons with vehicle treated controls. For CAR studies, the Friedman 2-way ANOVA by ranks, followed by the Wilcoxon matched-pairs signed-ranks test for comparisons with control conditions was used (Siegel and Castellan Jr 1988). Data for dose and time relationships between D2 receptor occupancy and catalepsy were analyzed by correlation analysis (Statistica 5.1, StatSoft, Inc.).
RESULTS
Occupancy and Catalepsy
Haloperidol (0.025–0.1 mg/kg, s.c.) produced a dose dependent increase in striatal D2 receptor occupancy ranging from 56–88%. No catalepsy was observed at these doses. Haloperidol (0.5 or 1.0 mg/kg) produced an average D2 receptor occupancy of 93% and 96%, respectively, and was accompanied by the observation of a maximum (i.e. a median score of 5), and statistically significant (p < .004 compared to vehicle treated controls) cataleptic response (Figure 1, Panel A; Table 1).
Relationship between dose, D2 occupancy and catalepsy for haloperidol (A), risperidone (B) and olanzapine (C). All catalepsy measurements were made at 110 minutes; all occupancy measurements were obtained at 120 minutes. Each non-cataleptic animal is represented by an open circle while each filled circle represents a cataleptic animal. If data from one animal was obscured by a similar point from another, it was staggered to the left or right for visualization on the graph.
Risperidone (0.05–1.0 mg/kg, s.c.) produced a dose dependent increase in striatal D2 receptor occupancy ranging from 29–71%. No catalepsy was observed at these doses. Risperidone (2.0 mg/kg) produced an average D2 receptor occupancy of 85%, and was accompanied by a robust (i.e. a median score of 4), and statistically significant (p < .004 compared to vehicle treated controls) catalepsy (Figure 1, Panel B; Table 1).
Olanzapine (0.5–2.0 mg/kg, s.c.) produced a dose dependent increase in striatal D2 receptor occupancy ranging from 65–83%. No catalepsy was observed at these doses. Olanzapine (5.0 and 10.0 mg/kg) produced an average D2 receptor occupancy of 94% and 95%, respectively, and was accompanied by the observation of maximum (i.e. a median score of 5), and statistically significant (p < .02 compared to vehicle treated controls) catalepsy (Figure 1, Panel C; Table 1).
Quetiapine (5.0–100.0 mg/kg, s.c.) was administered 50 minutes before catalepsy observation. The doses of quetiapine used produced a dose dependent increase in striatal D2 receptor occupancy ranging from 57–81%. No catalepsy was observed at any of these doses (Table 1).
Thus, the general picture is that regardless of the type of antipsychotic used, no catalepsy is observed until D2 receptor occupancy exceeds 80%. However, once D2 receptor occupancy moved into this range, catalepsy started emerging with almost all the animals being cataleptic when the occupancy was in the 90% range. This relationship with occupancy held regardless of whether the animal was treated with a typical or an atypical antipsychotic.
After having established this relationship in a cross-sectional manner, we examined whether or not a similar relationship between D2 occupancy and catalepsy was maintained over time. Haloperidol (0.5 mg/kg, s.c.) produced a maximum catalepsy one hour after administration. The effect lasted up to eight hours at which time a median score of 3 in catalepsy intensity was observed. No catalepsy was present at 24 hours after administration. The corresponding average D2 receptor occupancy was 92% (1hr), 88% (2 hrs), 85% (4hrs), 76% (8 hrs), and 17% (24 hrs), respectively (Figure 2). Again, the overall picture suggests that as long as the occupancy was above 80% catalepsy was robust, but as the occupancy dropped into the low 70% and range and lower, there was a resolution of catalepsy.
Time effect relationship between percent D2 receptor occupancy and catalepsy following a single dose of haloperidol in rats. Haloperidol (0.5 mg/kg, s.c.) was administered. Non-cataleptic animals are presented as open circles and cataleptic animals as filled circles. Each circle represents one animal (total n = 25). Catalepsy scores, expressed as median ± semi-interquartile range, were 5.0 ± 0.5 (1 hr), 5.0 ± 0.0 (2 hrs), 5.0 ± 0.0 (4 hrs), 3.0 ± 1.5 (8 hrs), and 0.0 ± 1.5 (24 hrs), respectively. There was a statistically significant (r = .83; p < .05) positive correlation between catalepsy and percent D2 receptor occupancy.
CAR Behavior
Haloperidol 0.025 or 0.1 mg/kg both produced a statistically significant (p < .05) suppression of CAR behavior 20 minutes after administration. The effect of haloperidol 0.1 mg/kg was still significant (p < .05) 90 minutes after administration. All effects were gone 480 minutes after administration. Haloperidol (0.01 mg/kg) had no effect on CAR (Figure 3, Panel A).
Effects of haloperidol, risperidone, olanzapine or quetiapine on conditioned avoidance response behavior in rats. Haloperidol (0.01–0.1 mg/kg, s.c.) (A), risperidone (0.2–0.8 mg/kg, i.p.) (B), olanzapine (0.5–5 mg/kg, i.p.) (C), or quetiapine (20 or 40 mg/kg, i.p.) (D) was given 20 minutes before the first observation time. Shown are medians ± semi-interquartile range based upon repeated observations in six animals, for each drug, serving as their own controls in a change-over design. * denotes p < .05.
Risperidone 0.4 or 0.8 mg/kg both produced a statistically significant (p < .05) suppression of CAR behavior 20 minutes after administration. The effect was still significant (p < .05) 90 minutes after administration but was completely gone at 240 minutes after administration. Risperidone (0.2 mg/kg) had no effect on CAR (Figure 3, Panel B).
Olanzapine 2.5 or 5.0 mg/kg both produced a statistically significant (p < .05) suppression of CAR behavior 20 minutes after administration. The effect of olanzapine 5.0 mg/kg was still significant (p < .05) 90 minutes after administration. All effects were gone 240 minutes after administration. Olanzapine (0.5 or 1.25 mg/kg) had no effect on CAR (Figure 3, Panel C).
Quetiapine (20 or 40 mg/kg) produced a statistically significant (p < .05) suppression of CAR behavior 20 minutes after administration. The effect of quetiapine 40 mg/kg was statistically significant (p < .05) still 90 minutes after administration. All effects were gone 240 minutes after administration (Figure 3, bottom right). Quetiapine (10 mg/kg; investigated in another set of animals) had no effect on CAR.
No escape failures were observed with any of the compounds used at any dose.
DISCUSSION
The present study showed that regardless of potency or multi-receptor affinity, haloperidol, risperidone and olanzapine all produced catalepsy only at doses producing a striatal D2 receptor occupancy ⩾85%. This may even be true for the atypical antipsychotic quetiapine, however at the highest administered dose of 100 mg/kg it only reached an average D2 receptor occupancy of 81%, and no catalepsy was observed. In each case the dose/occupancy required for action in the CAR model was significantly lower than that required in the CAT model.
Before a further discussion of these findings, certain limitations of the current study need comment. First, while the occupancy/CAT relationship was measured within-animal, the occupancy relationship to CAR is only approximate since it was estimated across groups. As CAR is conventionally done using a repeated-measures within-subject design, we could not measure occupancy in the same animals as it required sacrificing the animal. Second, while we relate both CAT and CAR to striatal D2 occupancy, we do not wish to suggest that they are both mediated by the same brain regions (see below for a discussion). Finally, the experiments were done in batches (i.e. one drug at a time, with raters blind to drug/vehicle and dose status). However, the animals were not randomized to the different drugs, thus limiting the degree to which small differences between drugs should be interpreted.
The above limitations notwithstanding, these findings are consistent with the previous observation (Wadenberg et al. 2000) that the relationship between D2 receptor occupancy and catalepsy in rats is similar to the relationship between human D2 receptor occupancy and EPS. The present study extends theses findings to the more clinically relevant antipsychotics and establishes that for each drug, the CAR effects occurred at a lower dose than the CAT effects. On average, the CAR effects first became evident at a dose that was third to a fourth of the dose required to produce catalepsy (Janssen et al. 1967), except for quetiapine where no catalepsy was observed. To get an estimate of the D2 occupancies required for CAR effect we referred to the animals in the CAT experiments. The data suggest that CAR effects become evident after 50% striatal D2 occupancy. And in general, for the drugs studied, the striatal D2 occupancy for ED50 in the CAR test was between 10–20% lower than that required for catalepsy (Table 1). This is consistent in trend with recent clinical findings where patients treated with haloperidol, risperidone or olanzapine show antipsychotic response at a D2 receptor occupancy of 65–70%, while EPS occurred only at doses that led to >80% D2 occupancy (Kapur et al. 2000a; Kapur et al. 1999). Quetiapine shows a different profile in patients such that antipsychotic response occurs at doses with rather low D2 occupancy (20–30%) at the conventional point of measurement, i.e. 12 hours after the last dose (Kapur et al. 2000b). However, it has been shown that this low occupancy at 12 hours is preceded by an occupancy in the 50–60% range in the period 1–2 hours after drug administration (Gefvert et al. 1998). Since CAR is an acute test, it is interesting that transiently high occupancy required for ED50 in rats in this test was in the range of 60%.
While the numerical coincidence between animal models and human effects are remarkable – catalepsy and EPS in the 80% range, and CAR and clinical response at a lower level of D2 occupancy – the models go only so far. For instance, catalepsy is observed in animals after a single dose that gives rise to 85% D2 occupancy. However, in humans EPS is observed only after repeated dosing that leads to 80% D2 occupancy. Similarly, effects on CAR are observed in animals 20–90 minutes following a single dose of an antipsychotic, while in humans the antipsychotic response gradually accumulates over several days of treatment once 60–70% D2 receptor occupancy is reached. Thus, these animal models are not replicas of the human effect, but only predictive models. Our data suggest that the reason these models may have identified and accurately predicted antipsychotic activity and EPS liability so well is because they share the common mechanism—D2 receptor occupancy—linking the animal models to the human condition.
The data raise several interesting questions about the use of these animal models. Since CAR and CAT occur along the same continuum of occupancy – is activity in CAR just a milder form of catalepsy? There are several reasons why this is unlikely to be the case. First, while we only measured striatal D2 receptor occupancy, we do not wish to suggest that the CAR and CAT reflect behavioral effects of D2 occupancy in the same region. There is evidence to suggest that CAR is mediated primarily via DA mesocorticolimbic pathways involving the ventral striatum (Wadenberg et al. 1990), while catalepsy is considered an effect primarily of D2 receptor blockade in the caudate putamen regions (dorsal striatum) of the DA nigrostriatal pathway (Calderon et al. 1988; Hauber and Munkle 1997). Second, anticholinergic agents, while completely reversing catalepsy, have minimal or no effect on the CAR model (Setler et al. 1976) suggesting a functional dissociation between these two models. Finally, a selective dose of a 5-HT1A agonist facilitates suppression of the CAR, while at the same time it antagonizes the effects on catalepsy, thus providing a double dissociation (Wadenberg and Ahlenius 1991). Thus, CAR is not just a milder form of catalepsy, but instead represents a distinct process, requiring some transfer of motivational drives into motor action, crucially dependent upon the integrity of the dopaminergic systems in the ventral striatum and nucleus accumbens (Salamone et al. 1997).
The other issue that our data raises is that if CAR is premised on D2 blockade, what is the likelihood that this model will correctly identify an antipsychotic that does not work via this mechanism. The problem is that currently all antipsychotics have at least some effect on D2 receptors (Kapur and Seeman 2001) and they are also all effective in CAR (Wadenberg and Hicks 1999). However, the CAR model shows some features that suggest that it may be more than just an assay of D2 occupancy. For example, clozapine, the prototype atypical antipsychotic, is very effective in the CAR model (Wadenberg and Hicks 1999). We have recently observed (unpublished data) that it exerts its effects in this model at a level of D2 occupancy that is substantially lower than that required by a specific D2 blocker like raclopride. This is interesting because in humans, the level of D2 occupancy required for clinical response with raclopride is in the range of 70% (Nordstrom et al. 1993), while clozapine seems to exert its effects with averages in the 40–60% range (Kapur et al. 1999; Nordstrom et al. 1995) thus raising the possibility that CAR may be a behavioral assay that can at least partially be dissociated from D2 blockade. Second, some cholinergic agonists show efficacy in this model (Shannon et al. 1999; Shannon et al. 2000), and preliminary data in patients with dementia and psychosis suggests a possibility of an antipsychotic effect in this population (Bodick et al. 1997)(though no convincing tests of this in schizophrenia are as yet available). Finally, the CAR test has been successful in making negative predictions. For example, L-745,870, a D4-selective agent was ineffective in this model (Bristow et al. 1997a), and was subsequently found to be ineffective in patients (Bristow et al. 1997b; Kramer et al. 1997). Similarly, a selective blockade of the serotonin 5-HT2 receptor is not effective in the CAR model (Wadenberg et al. 1997a, 1998), and clinical trials with 5-HT2 agents in schizophrenia have not shown any convincing antipsychotic efficacy (Announcement 1999; Truffinet et al. 1999). The final answer to whether CAR can be considered something more than an assay for 50–80% D2 receptor occupancy, can only be tested when we have a truly non-D2 receptor antipsychotic and examine its behavior in this model. Until then, prospective use of this model in screening should always be mindful of its close association with quantitative D2 blockade.
Finally, these data raise the question whether a similar relationship (with D2 occupancy) exists in the other models conventionally used to detect antipsychotics (e.g. amphetamine and apomorphine induced hyperlocomotion or disruption of sensorimotor gating (Arnt et al. 1997; Higgins 1998)). We are not aware of any systematic studies relating activity in these models to in vivo measures of D2 occupancy, especially with the currently relevant antipsychotics. However, given that these models are primarily (though not exclusively) dopaminergic challenges, one would expect D2 occupancy to have a causal effect in these models (Higgins 1998). It was precisely to escape this circularity (i.e. dopaminergic challenge blocked by dopamine antagonist) that we chose to focus on the CAR model, which does not rely on a dopaminergic challenge to produce its main effect (Wadenberg and Hicks 1999).
In conclusion, we found that both typical and atypical antipsychotics induced catalepsy at doses producing a striatal D2 receptor occupancy of ⩾85%. In addition, the drugs were effective in the CAR model at occupancies which were lower than those required for catalepsy, and are reminiscent of the occupancies observed in humans for therapeutic effect. These results are consistent with recent findings from clinical-neuroimaging studies and suggest central dopamine D2 receptor occupancy is the underlying variable which leads to the accuracy of these animal behavioral tests in predicting the outcome of clinical treatment.
References
Ahlenius S, Hillegaart V . (1986): Involvement of extrapyramidal motor mechanisms in the suppression of locomotor activity by antipsychotic drugs: a comparison between the effects produced by pre- and post-synaptic inhibition of dopaminergic neurotransmission. Pharmacol Biochem Behav 24: 1409–1415
Announcement (1999): Management Decisions on Priority Pipeline Products—MDL 100907, Vision Extra, Vol 4, pp 2–3
Arnt J, Skarsfeldt T, Hyttel J . (1997): Differentiation of classical and novel antipsychotics using animal models. Int Clin Psychopharmacol 12 Suppl 1: S9–S17
Bodick NC, Offen WW, Levey AI, Cutler NR, Gauthier SG, Satlin A, Shannon HE, Tollefson GD, Rasmussen K, Bymaster FP, Hurley DJ, Potter WZ, Paul SM . (1997): Effects of xanomeline, a selective muscarinic receptor agonist, on cognitive function and behavioral symptoms in Alzheimer disease. Arch Neurol 54: 465–473
Bristow LJ, Collinson N, Cook GP, Curtis N, Freedman SB, Kulagowski JJ, Leeson PD, Patel S, Ragan CI, Ridgill M, Saywell KL, Tricklebank MD . (1997a): L-745,870, a subtype selective dopamine D4 receptor antagonist, does not exhibit a neuroleptic-like profile in rodent behavioral tests. Journal of Pharmacology and Experimental Therapeutics 283: 1256–1263
Bristow LJ, Kramer MS, Kulagowski J, Patel S, Ragan CI, Seabrook GR . (1997b): Schizophrenia and L-745, 870, a novel dopamine D4 receptor antagonist. Trends in Pharmacological Sciences 18: 186–188
Calderon SF, Sanberg PR, Norman AB . (1988): Quinolinic acid lesions of rat striatum abolish D1- and D2-dopamine receptor-mediated catalepsy. Brain Res 450: 403–407
Farde L, Nordstrom AL, Wiesel FA, Pauli S, Halldin C, Sedvall G . (1992): Positron emission tomographic analysis of central D1 and D2 dopamine receptor occupancy in patients treated with classical neuroleptics and clozapine: relation to extrapyramidal side effects. Archives of General Psychiatry 49: 538–544
Farde L, Wiesel FA, Halldin C, Sedvall G . (1988): Central D2-dopamine receptor occupancy in schizophrenic patients treated with antipsychotic drugs. Archives of General Psychiatry 45: 71–76
Gefvert O, Bergstrom M, Langstrom B, Lundberg T, Lindstrom L, Yates R . (1998): Time course of central nervous dopamine-D-2 and 5-HT2 receptor blockade and plasma drug concentrations after discontinuation of quetiapine (Seroquel(R)) in patients with schizophrenia. Psychopharmacology 135: 119–126
Hauber W, Munkle M . (1997): Motor depressant effects mediated by dopamine D2 and adenosine A2A receptors in the nucleus accumbens and the caudate-putamen. Eur J Pharmacol 323: 127–131
Higgins GA . (1998): From rodents to recovery: Development of animal models of schizophrenia. CNS Drugs 9: 59–68
Janssen PA . (1967): The pharmacology of haloperidol. Int J Neuropsychiatry 3 (Suppl 1): 10–18
Janssen PA, Niemegeers CJ, Awouters F, Schellekens KH, Megens AA, Meert TF . (1988): Pharmacology of risperidone (R 64 766), a new antipsychotic with serotonin-S2 and dopamine-D2 antagonistic properties. The Journal of Pharmacology and Experimental Therapeutics 244: 685–693
Janssen PA, Niemegeers CJ, Schellekens KH, Lenaerts FM . (1967): Is it possible to predict the clinical effects of neuroleptic drugs (major tranquilizers) from animal data? IV. An improved experimental design for measuring the inhibitory effects of neuroleptic drugs on amphetamine- or apomorphine-induced “Cheroing” and “agitation” in rats. Arzneimittelforschung 17: 841–854
Kapur S, Seeman P . (2001): Does fast dissociation from the dopamine D2 receptors explain atypical antipsychotic action—a new hypothesis. American Journal of Psychiatry 158: 360–369
Kapur S, Zipursky R, Jones C, Remington G, Houle S . (2000a): Relationship between dopamine D(2) occupancy, clinical response, and side effects: A double-blind PET study of first-episode schizophrenia. Am J Psychiatry 157: 514–520
Kapur S, Zipursky R, Jones C, Shammi CS, Remington G, Seeman P . (2000b): A positron emission tomography study of quetiapine in schizophrenia: a preliminary finding of an antipsychotic effect with only transiently high dopamine D2 receptor occupancy. Arch Gen Psychiatry 57: 553–559
Kapur S, Zipursky RB, Remington G . (1999): Clinical and theoretical implications of 5-HT2 and D2 receptor occupancy of clozapine, risperidone, and olanzapine in schizophrenia. Am J Psychiatry 156: 286–293
Kramer MS, Last B, Getson A, Reines SA . (1997): The effects of a selective D4 dopamine receptor antagonist (L-745,870) in acutely psychotic inpatients with schizophrenia. D4 Dopamine Antagonist Group [published erratum appears in Arch Gen Psychiatry 54:1080]. Arch Gen Psychiatry 54: 567–572
Migler BM, Warawa EJ, Malick JB . (1993): Seroquel: behavioral effects in conventional and novel tests for atypical antipsychotic drug. Psychopharmacology 112: 299–307
Moore NA, Tye NC, Axton MS, Risius FC . (1992): The behavioral pharmacology of olanzapine, a novel “atypical” antipsychotic agent. The Journal of Pharmacology and Experimental Therapeutics 262: 545–551
Nordstrom AL, Farde L, Nyberg S, Karlsson P, Halldin C, Sedvall G . (1995): D1, D2, and 5-HT2 receptor occupancy in relation to clozapine serum concentration: a PET study of schizophrenic patients [see comments]. Am J Psychiatry 152: 1444–1449
Nordstrom AL, Farde L, Wiesel FA, et al. (1993): Central D2-dopamine receptor occupancy in relation to antipsychotic drug effects—a double-blind PET study of schizophrenic patients. Biological Psychiatry 33: 227–235
Salamone JD, Cousins MS, Snyder BJ . (1997): Behavioral functions of nucleus accumbens dopamine: empirical and conceptual problems with the anhedonia hypothesis. Neurosci Biobehav Rev 21: 341–359
Setler P, Sarau H, McKenzie G . (1976): Differential attenuation of some effects of haloperidol in rats given scopolamine. Eur J Pharmacol 39: 117–126
Shannon HE, Hart JC, Bymaster FP, Calligaro DO, DeLapp NW, Mitch CH, Ward JS, Fink-Jensen A, Sauerberg P, Jeppesen L, Sheardown MJ, Swedberg MD . (1999): Muscarinic receptor agonists, like dopamine receptor antagonist antipsychotics, inhibit conditioned avoidance response in rats. J Pharmacol Exp Ther 290: 901–907
Shannon HE, Rasmussen K, Bymaster FP, Hart JC, Peters SC, Swedberg MD, Jeppesen L, Sheardown MJ, Sauerberg P, Fink-Jensen A . (2000): Xanomeline, an M(1)/M(4) preferring muscarinic cholinergic receptor agonist, produces antipsychotic-like activity in rats and mice. Schizophr Res 42: 249–259
Siegel B, Castellan NR, Jr . (1988): Nonparametric Statistics for The Behavioral Sciences. New York, McGraw-Hill
Truffinet P, Tamminga CA, Fabre LF, Meltzer HY, Riviere ME, Papillon-Downey C . (1999): Placebo-controlled study of the D4/5-HT2A antagonist fananserin in the treatment of schizophrenia. Am J Psychiatry 156: 419–425
Wadenberg M-LG . (1996): Serotonergic mechanisms in neuroleptic-induced catalepsy in the rat. Neurosci Biobehav Rev 20: 325–339
Wadenberg M-LG, Ahlenius S . (1991): Antipsychotic-like profile of combined treatment with raclopride and 8-OH-DPAT in the rat: enhancement of antipsychotic-like effects without catalepsy. J Neural Transm Gen Sect 83: 43–53
Wadenberg M-LG, Ericson E, Magnusson O, Ahlenius S . (1990): Suppression of conditioned avoidance behavior by the local application of (-)sulpiride into the ventral, but not the dorsal, striatum of the rat. Biol Psychiatry 28: 297–307
Wadenberg M-LG, Hicks PB . (1999): The conditioned avoidance response test re-evaluated: is it a sensitive test for the detection of potentially atypical antipsychotics? Neurosci Biobehav Rev 23: 851–862
Wadenberg M-LG, Hicks PB, Young KA, Richter JT . (1997a): Further evidence for a role of the 5-HT2 receptor in the mediation of antipsychotic activity. Schizophrenia Research 24: 83
Wadenberg M-LG, Kapur S, Soliman A, Jones C, Vaccarino F . (2000): Dopamine D2 receptor occupancy predicts catalepsy and the suppression of conditioned avoidance response behavior in rats. Psychopharmacology (Berl)) 150: 422–429
Wadenberg M-LG, Young KA, Trompler RA, Zavodny RA, Richter TJ, Hicks PB . (1997b): A novel computer-controlled conditioned avoidance apparatus for rats. J Pharmacol Toxicol Methods 38: 211–215
Wadenberg M-LG, Hicks PB, Richter JT, Young KA . (1998): Enhancement of antipsychoticlike properties of raclopride in rats using the selective serotonin(2A) receptor antagonist MDL 100,907. Biological Psychiatry 44: 508–515
Acknowledgements
We thank Corey Jones, Alex Kecojevic, Doug Hussey, Kevin Cheung, and Judy Sinyard for their expert technical assistance. This study was partially funded by support from the Theodore and Vada Stanley Foundation (USA) and by the Canada Research Chair to SK. Partial financial support from Eli Lilly Canada and AstraZeneca Canada is acknowledged.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wadenberg, ML., Soliman, A., VanderSpek, S. et al. Dopamine D2 Receptor Occupancy Is a Common Mechanism Underlying Animal Models of Antipsychotics and Their Clinical Effects. Neuropsychopharmacol 25, 633–641 (2001). https://doi.org/10.1016/S0893-133X(01)00261-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/S0893-133X(01)00261-5
Keywords
This article is cited by
-
Neonatal phencyclidine as a model of sex-biased schizophrenia symptomatology in adolescent mice
Psychopharmacology (2023)
-
Effect of 5-HT2A receptor antagonism on levels of D2/3 receptor occupancy and adverse behavioral side-effects induced by haloperidol: a SPECT imaging study in the rat
Translational Psychiatry (2021)
-
Dopamine D2 receptors in the expression and extinction of contextual and cued conditioned fear in rats
Experimental Brain Research (2021)
-
Structure-inspired design of β-arrestin-biased ligands for aminergic GPCRs
Nature Chemical Biology (2018)
-
In Vitro and In Vivo Characterization of PCC0104005, a Novel Modulator of Serotonin-Dopamine Activity, as an Atypical Antipsychotic Drug
Scientific Reports (2018)