Abstract
Using 31P magnetic resonance spectroscopy, we examined changes in the levels of phosphorus metabolites in the temporal lobes of 13 schizophrenic patients before and 12 weeks after initiating haloperidol treatment. Spectra were obtained from a volume of interest positioned in each temporal lobe. Findings were compared with those in 13 age- and gender-matched healthy subjects. Prior to treatment the patients showed higher levels of phosphodiesters (PDE) in both temporal lobes than healthy subjects. Haloperidol administration significantly reduced the excess of PDE in the left temporal lobe, although the PDE concentration remained somewhat higher bilaterally than in controls. Treatment was associated with a decline in the total symptom score according to the Brief Psychiatric Rating Scale and the score for positive symptoms showed a relatively high correlation with reduction in PDE level in the left temporal lobe. These preliminary results suggest that haloperidol may partially normalize disturbed metabolism or abnormalities in components of membrane phospholipids in the left temporal lobe of untreated schizophrenic patients, paralleling symptom alleviation.
Similar content being viewed by others
Main
Functional neuroimaging studies have revealed abnormalities in the brains of schizophrenic patients, especially in the frontal and temporal lobes, basal ganglia, and thalamus (Bertolino et al. 1996; Andreasen et al. 1997; Egan and Weinberger 1997; McClure et al. 1998). Frontal lobe dysfunction generally has been associated with “negative” symptoms and the disorganization syndrome (Liddle et al. 1992; Kaplan et al. 1993; Shioiri et al. 1994; Deicken et al. 1995), whereas temporal lobe dysfunction may be related to “positive” symptoms (Fukuzako et al. 1996; Klemm et al. 1996; Nordahl et al. 1996; Sabri et al. 1997). The effects of neuroleptic treatment on regional cerebral blood flow (rCBF) and metabolism are not yet clear (Miller et al. 1997). Several researchers have found, however, that neuroleptic treatment produced changes in rCBF in the frontal and temporal lobes of schizophrenic patients. Nilsson et al. (1977) demonstrated a widespread reduction in cortical perfusion, especially in frontotemporal regions, after several weeks of treatment with haloperidol. Changes in positive symptom scores correlated well with changes in both frontal and temporal CBF (Berman et al. 1996). Single-dose haloperidol administration in schizophrenic patients ameliorated hypoactivity in the frontal lobes and suppressed hyperactivity in the temporal lobe and adjacent occipital and parietal areas (Matsuda et al. 1991). These CBF changes were not detected when the drug was administered to normal volunteers. These observations suggest that neuroleptics alleviate schizophrenic symptoms by actions in the frontal and temporal lobes.
Phospholipase A2 (PLA2) is a key enzyme in the metabolism of phospholipids that also affects receptor function and signal transduction (Farooqui et al. 1992). In a biochemical study, Gattaz et al. (1995) found platelet PLA2 activity to be greater in schizophrenic patients than in healthy controls; this elevation was reduced by neuroleptic treatment. Neuroleptics may alter brain phospholipid metabolism and composition by regulating PLA2 activity in a manner similar to that seen in platelets and red blood cells. Possible effects of neuroleptics like haloperidol on membrane phospholipid metabolism and composition are under investigation. In one study, haloperidol was found to reduce synthesis of various phospholipids in rat brain (Singh and Shankar 1996).
Disturbed phospholipid metabolism has been proposed as a neurodevelopmental pathogenesis of schizophrenia (Horrobin 1998). In vivo31phosphorus magnetic resonance spectroscopy (31P-MRS) is able to quantitate membrane phospholipids and high-energy phosphate metabolism in the brain (Maier 1995; McClure et al. 1998). Therefore, 31P-MRS may represent a direct test for such a hypothesis. With 31P-MRS, increased levels of phosphodiesters (PDE) and decreased levels of phosphomonoesters (PME) have been observed in the frontal lobes of drug-naive schizophrenic patients compared with levels in healthy subjects (Pettegrew et al. 1991; Stanley et al. 1995). Increased β-phosphates of 5'-adenosine triphosphate (β-ATP) and decreased inorganic orthophosphate (Pi) also have been reported (Pettegrew et al. 1991). Evidence of changes in phosphorus metabolites has been sought after treatment with neuroleptic medication only in the study of Keshavan et al. (1995), with negative results. However, no previous report has investigated metabolite changes in the temporal lobes of drug-naive schizophrenic patients and subsequent alterations in metabolite levels with neuroleptic treatment. In our previous study, the association between membrane phospholipid abnormality in the temporal lobe and positive symptoms was reported in medicated schizophrenic patients (Fukuzako et al. 1996). In the present study, we performed 31P-MRS to investigate metabolite changes in the temporal lobes of schizophrenic patients induced by the administration of haloperidol for 12 weeks and its relations to specific symptoms.
MATERIALS AND METHODS
Twenty-five first-episode, drug-naive Japanese patients (14 men and 11 women aged 16 to 32 years; mean 23.1) who met DSM-III-R diagnostic criteria for schizophrenia or schizophreniform disorder (American Psychiatric Association 1987) and were right-handed according to the Edinburgh Handedness Inventory (Oldfield 1971; Schachter et al. 1987) were recruited from the outpatient clinics of Fujimoto Hospital and Kagoshima University Hospital between 1991 and 1996. All patients gave their written informed consent for participation in the study. None had a recent history of alcohol or drug abuse.
Sixteen patients of the 25 completed adequate MRS studies before and after 12 weeks of treatment with haloperidol. The dose of haloperidol given each patient was determined by the treating psychiatrist. The average total dose of haloperidol administered during the 12-week period was 470 ± 223 mg. All patients were treated in the two institutions, and their diagnoses were reevaluated one year following the first scan. Three patients were excluded from data analysis because their diagnosis remained schizophreniform disorder at this follow-up estimation. As a result, data from the 13 patients (7 men and 6 women aged 16 to 32 years; mean 22.6), who were diagnosed with schizophrenia, were analyzed. They had been ill for 7.4 ± 6.5 months at the time of the first scan. A neuropsychiatrist (T. Fukuzako) evaluated the patients using the Oxford version of the Brief Psychiatric Rating Scale (BPRS, range 0 to 6) (Kolakowska 1976) before and after treatment. The sum of scores for conceptual disorganization, suspiciousness, hallucinatory behavior, mannerisms and posturing, and unusual thought content was taken as the subscale score for positive symptoms. Negative symptom scores were estimated based on emotional withdrawal, motor retardation, uncooperativeness, and blunted affect. This selection criteria was based on the results of Kitamura et al. (1990).
Thirteen age- and gender-matched healthy subjects who served as controls (ages 15 to 31 years; mean 22.2) were relatives of hospital staff members and students at the University. They underwent MRS twice, with the same interval between scans as in the patient group. All subjects were right-handed according to the Edinburgh inventory (Oldfield 1971); a laterality score greater than 80 was considered evidence of right-handedness (Schachter et al. 1987).
The method of MRS data acquisition and processing has been described in our earlier report (Fukuzako et al. 1996). Spectroscopy was performed on a Siemens-Asahi Meditec MR system (Erlangen, Germany) with a magnetic field strength of 2.0 tesla. A circular polarizing head coil was tuned to 84.5 MHz for proton imaging and to 34.2 MHz for in vivo multivoxel 31P-MRS (two-dimensional chemical shift imaging; 2DCSI). T1-weighted spin-echo images with a repetition time of 500 msec and an echo time of 15 msec were acquired for the voxel placement. The field of view was 24 cm with an 8 x 8 data matrix and a 4-cm section thickness. The volume of each voxel was 36 ml. We sought to make the location of the voxels investigated as near to identical as possible between the two MRS scans. On the midsagittal slice, placement of voxels was determined as the posterior limit of the volume of interest (VOI) passing through the superior and inferior colliculus. On the coronal slice, the placement of the voxels was determined as the midline of voxels passing through the interhemispheric fissure and third ventricle. In addition, the inferior limit of the VOIs was placed on a line passing through the inferior aspect of both temporal lobes. The spectra from the two VOIs, each consisting of two voxels, were produced by recalculating the signals already obtained. These VOIs contained mainly the temporal lobes and small part of the frontal and parietal lobes. The time of repetition was 2 sec; the number of sample points was 1024; and the acquisition delay was 1.72 msec. Twelve measurements were obtained for each spectrum. Data were processed with Fourier transformation and exponential multiplication (16 Hz) and then phase-corrected for the constant phase and linear frequency dependent phase.
Spectral peaks were obtained for PME, Pi, PDE, phosphocreatine (PCr), and γ-, α-, and β-ATP. The spectra were quantified by peak area measurements. An automated baseline correction technique removed the sinc-wiggle-like distortion from the baseline of the spectra. The technique minimized the square error between the theoretically derived spectrum and the corrected spectrum. After baseline correction, peak parameters such as height, position, and width were obtained by a Lorentzian curve-fitting procedure. This process was performed automatically after the number of peaks was determined. For each spectrum, the integrated areas for PME, Pi, PDE, and PCr, and for γ-, α-, and β-ATP were measured, and percentages of total phosphorus signal (mole percentages) were calculated. The β-ATP peak was adopted as an ATP reference because γ- and α-ATP peaks contain other phosphate metabolites such as adenosine diphosphate and dinucleotide phosphate. Coefficients of variation (CVs) for controls in this study for each metabolite ranged from 6.5% to 17.6% (PME, lt 12.0%, rt 14.8%; Pi, lt 15.4%, rt 17.6%; PDE, lt 6.5%, rt 6.6%; PCr, lt 15.0%, rt 12.4%; β-ATP, lt 10.5%, rt 10.7%; γ-ATP, lt 11.1%, rt 16.2%; and α-ATP, lt 10.2%, rt 10.1%). These CVs were less than those we had previously calculated based on one voxel (36 ml, range 8.7% to 27.9%) (Fukuzako et al. 1996). We investigated changes between two scans performed one to two weeks apart in five schizophrenic patients who underwent long-term medication and five healthy volunteers. No significant metabolite changes were demonstrated between the two scans by a paired t test, although the sample size was very small. In addition, the CVs in the patients and controls in the previous study of small sample were comparable to those in the present one.
Repeated-measures analysis of variance (ANOVA) was performed separately for patients and controls, with scan (pre- and posttreatment) analyzed and side (left and right) as within-subject factors. Subsequently, two-way ANOVA with a between-subject factor of diagnosis and a within-subject factor of side was performed on data obtained before and after haloperidol treatment, and was followed by Scheffé multiple-comparison method to establish statistically significant differences (p < .05). Pairwise comparisons were made: the second scan to the first scan in each patient or control group; patient to control at the time of the first scan or the second scan; and left to right for the first scan or the second scan in each group. Phosphorus metabolites were analyzed in an exploratory manner without correction for multiple comparison, in spite of the increased risk of a Type I error. Pearson's product moment correlation coefficient (r) was used to test relationships between the two types of values.
RESULTS
No obvious morphologic abnormalities were detected on magnetic resonance images of patients or healthy subjects. Mole percentages of metabolites in controls, in the drug-naive patients, and in patients after 12 weeks of haloperidol treatment are shown in Table 1. In the patient group, ANOVA revealed significant effects of scan (pre- vs. post-treatment) and side for levels of PME (F3, 36 = 3.42; p = .028) and PDE (F3, 36 = 5.21; p = .004). In the control group, no significant effects were observed for any metabolite.
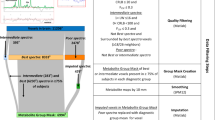
Subsequent repeated-measures ANOVA showed a significant effect of diagnosis for levels of PME (F1, 24 = 4.75; p = .039) and PDE (F1, 24 = 20.0; p < .001) in drug-naive patients compared with healthy subjects. A significant diagnosis-by-side interaction was observed for PCr (F1, 24 = 5.05; p = .034). Post hoc multiple comparison revealed a significant elevation of PDE on both sides in drug-naive patients compared to the control group (left, p < .001; right, p = .004) (Table 1). Haloperidol administration significantly reduced the excess of PDE in the left temporal lobe of schizophrenic patients (p = .028) (Table 1), (Figure 1).
Mole percentages of phosphodiesters (PDE) in the left and right temporal region of schizophrenic patients before (drug-naive) and after (12-week haloperidol) receiving haloperidol for 12 weeks. Mean values (± SD) in healthy controls and long-term medicated patients also are shown (data from our previous study: Fukuzako et al. 1996)
The total BPRS score declined with haloperidol treatment, from an average of 35.3 to 13.4 (paired t-test: t = 9.79, p < .001). After 12 weeks of treatment with haloperidol, only the PDE level showed a remaining trend toward an excess in comparison to levels in healthy subjects (lt, p = .065; rt, p = .073). Relationships between changes in symptom score and metabolite level were tested for PME and PDE on both sides separately because the level of PDE in the left temporal lobe was changed significantly by haloperidol treatment, whereas both levels of PME on the left (p = .061) and of PDE on the right (p = .095) tended to be altered by the medication. Reduction in PDE level in the left temporal lobe correlated well with decline of total BPRS score (r = 0.69, p = .007) and the score for positive symptoms (r = 0.73, p = .003) (Figure 2). The PDE reduction in the right temporal lobe showed a weak correlation with the decline in positive symptom score (r = 0.59, p = .031). The total amount of haloperidol did not correlate significantly with changes in the level of any metabolite. The decline in BPRS score did not correlate with levels of any metabolite prior to haloperidol treatment.
DISCUSSION
In this study, 31P-MRS detected an elevation of PDE in the temporal lobes of drug-naive schizophrenic patients compared with healthy subjects. These results are in part consistent with previous observations reported in the prefrontal cortex of schizophrenic patients (Pettegrew et al. 1991; Stanley et al. 1995). A recent preliminary study of 31P-MRS in the temporal lobes of postmortem brains has shown a nonsignificant decrease in phosphoethanolamine (PE) and increases in glycerophosphoethanolamine (GPE) and glycerophosphocholine (GPC) in schizophrenic subjects, changes smaller but otherwise similar to our own findings (Williamson et al. 1996). Pettegrew et al. (1991) have speculated that increased PDE in the frontal lobes of schizophrenic patients may reflect increased breakdown of membrane phospholipids. The pre-acquisition delay time of 1.72 msec in our study makes interpretation of increased PDE difficult. The PDE resonance obtained from our 31P-MRS method arises from free mobile PDE (GPC, GPE) and mobile PDE moieties (small membrane phospholipid structures such as micelles and vesicles) (Murphy et al. 1989; McNamara et al. 1994; Stanley et al. 1997; McClure et al. 1998). The longer pre-acquisition delay time might yield different results (Stanley et al. 1997). PDE are more concentrated in white matter than in gray (Kilby et al. 1990). However, a decreased gray-to-white matter ratio would be an unlikely cause of increased PDE level, since haloperidol treatment for 10 months does not alter volumes of gray and white matter (Keshavan et al. 1994). Therefore, the increase in PDE may reflect an increase in GPC, GPE, and/or small membrane phospholipid structures (McClure et al. 1998).
Several recent studies have used 1H-decoupled 31P-MRS to try to determine which PDE components contribute to the changes in PDE resonance observed in schizophrenic patients (Potwarka et al. 1996; Bluml et al. 1998). A preliminary study has shown that membrane or mobile phospholipids are increased in the frontal lobes of medicated schizophrenic patients, suggesting abnormal membrane structures (Potwarka et al. 1996). Recent reports suggest that schizophrenia is associated with a deficiency of arachidonic acid and docosahexaenoic acid in cell membranes (Horrobin 1998; Puri and Richardson 1998). On the other hand, Bluml et al. (1998) have demonstrated elevation of GPC and GPE concentrations in the parietal lobes of young medicated schizophrenic patients compared with healthy controls and elderly schizophrenic patients. Although definitive determination of the origins of increased PDE is difficult, disturbed metabolism or abnormalities in components of membrane phospholipids may not be restricted to the frontal lobe in the manner of the gray matter volume reduction observed in first-episode and long-term medicated schizophrenic patients (Lawrie and Abukmeil 1998; Zipursky et al. 1998).
In the present study an elevated level of PDE, especially in the left temporal lobe, was decreased by treatment with haloperidol, in contrast to the report of Keshavan et al. (1995), who reported increased levels of PDE on pretreatment imaging but no significant changes after four weeks of haloperidol treatment. The discrepancy between their results and ours may have resulted from differences in patient characteristics, location of the VOI, or the MRS techniques. Only nine of the 15 patients studied by Keshavan group were diagnosed with schizophrenia, while the remaining six had other psychotic disorders. The VOI was located in the prefrontal cortex in their study; in ours the VOI was placed in the temporal lobe, which has been associated with positive symptoms representing reality distortion that are alleviated substantially by administration of neuroleptics (Fukuzako et al. 1996; Klemm et al. 1996; Nordahl et al. 1996; Sabri et al. 1997). In contrast, the frontal lobe reportedly has been associated with negative symptoms (psychomotor poverty) and disorganization syndromes that often resist neuroleptic treatment (Liddle et al. 1992; Kaplan et al. 1993; Shioiri et al. 1994; Deicken et al. 1995). A relatively high correlation between reductions in PDE level and in scores for positive symptoms lends support to VOI location as the reason for interstudy differences. Also, the depth-resolved surface coil spectroscopy used by the Keshavan group did not eliminate signals originating from the skull and cranial muscles, while our method of 2DCSI was virtually free of such artifacts. Finally, the period of haloperidol administration between the two scans was three times longer in our study than in theirs.
Administration of haloperidol for 12 weeks reduced the level of PDE to that found in patients receiving neuroleptic medication over long periods. However, the resonance representing PDE in the medicated patients still had a trend toward increase, compared with those in healthy subjects. These in vivo results may be consistent with biochemical findings demonstrating that increased PLA2 activity was reduced by administration of neuroleptics (Gattaz et al. 1987, 1995), while remaining higher in treated schizophrenic patients than in healthy subjects (Ross et al. 1997). Our results suggest that neuroleptic medication may partially normalize the disturbed metabolism or abnormalities in components of membrane phospholipids in the temporal lobe of schizophrenic patients, especially on the left side.
Several limitations of this study need to be addressed. First, absolute metabolite quantitation, although preferable to assessment by percentage, was not feasible with our preliminary protocol. Second, alterations in T1 or T2 of phosphorus metabolites in the temporal lobe of schizophrenic patients could have influenced the differences detected between groups. Third, the size of the voxel was large (72 ml) because of the lower sensitivity of the 31P-MRS and reducing the CVs between the scans; the voxels contained small portions of the frontal and parietal lobes besides temporal lobe. Fourth, the voxels contained varing percentages of gray matter, white matter, and CSF, which also may have altered group differences in metabolites. More sophisticated software that collects signals from these tissues separately may be better able to determine how subtle morphologic abnormalities in schizophrenic patients might interact with phosphorus MRS findings in vivo. Fifth, we investigated rest-retest reliability in five medicated schizophrenic patients and five healthy subjects, without any significant metabolite changes between the two scans. However, the sample size may not be sufficient for comparing results with this study. Finally, our MRS method may not be sufficiently sensitive to detect other subtle changes caused by haloperidol treatment.
In conclusion, our preliminary findings suggest that in vivo 31P-MRS shows promise as one way to monitor the effect of the treatment of schizophrenia using neuroleptics and other therapies. Further studies regarding changes in metabolites with treatment using recently developed in vivo 31P- and 1H-MRS techniques (Bertolino et al. 1996; Stanley et al. 1997; Bluml et al. 1998; Deicken et al. 1998) will help to assess such possibilities.
References
American Psychiatric Association. (1987): Diagnostic and Statistical Manual of Mental Disorders, 3rd ed, revised. Washington DC, American Psychiatric Association
Andreasen NC, O'Leary DS, Flaum M, Nopoulos P, Watkins GL, Ponto LLB, Hichwa RD . (1997): Hypofrontality in schizophrenia: Distributed dysfunctional circuits in neuroleptic-naıuml;ve patients. Lancet 349: 1730–1734
Berman I, Merson A, Sison C, Allan E, Schaefer C, Loberboym M, Losonczy MF . (1996): Regional cerebral blood flow changes associated with risperidone treatment in elderly schizophrenia patients: A pilot study. Psychopharmacol Bull 32: 95–100
Bertolino A, Nawroz S, Matty VS, Barnett AS, Duyn JH, Moonen CTW, Frank JA, Tedeschi G, Weinberger DR . (1996): Regionally specific pattern of neurochemical pathology in schizophrenia as assessed by multislice proton magnetic resonance spectroscopic imaging. Am J Psychiatry 153: 1554–1563
Blü S, Tan J, Adatia N, Karme A, Sproull T, Harris K, Ross BD . (1998): Cerebral Glycerophosphorylcholine and Ethanolamine Concentrations Are Elevated in Young Schizophrenics (abstract). Proceedings of the 6th Annual Scientific Meeting (Sydney) SMR, p 736
Deicken RF, Merrin EL, Floyd TC, Weiner MW . (1995): Correlation between left frontal phospholipids and Wisconsin Card Sorting Test performance in schizophrenia. Schizophr Res 14: 177–181
Deicken RF, Zhou L, Schuff N, Fein G, Weiner MW . (1998): Hippocampal neuronal dysfunction in schizophrenia as measured by proton magnetic resonance spectroscopy. Biol Psychiatry 43: 483–488
Egan MF, Weinberger DR . (1997): Neurobiology of schizophrenia. Curr Opin Neurobiol 7: 701–707
Farooqui AA, Hirashima Y, Horrocks LA . (1992): Brain phospholipases and their role in signal transduction. In Bazan N.G. Murphy M.G. Tofano G(eds), Neurobiology of Essential Fatty Acids. New York, Plenum Press, 11–26
Fukuzako H, Fukuzako T, Takeuchi K, Ohbo Y, Ueyama K, Takigawa M, Fujimoto T . (1996): Phosphorus magnetic resonance spectroscopy in schizophrenia: Correlation between membrane phospholipid metabolism in the temporal lobe and positive symptoms. Prog Neuro-Psychopharmacol Biol Psychiatry 20: 629–640
Gattaz WF, Kollisch M, Thurn T, Virtanen JA, Kinnunen PKJ . (1987): Increased plasma phospholipase-A2 activity in schizophrenic patients: Reduction after neuroleptic therapy. Biol Psychiatry 22: 421–426
Gattaz WF, Schmitt A, Maras A . (1995): Increased platelet phospholipase A2 activity in schizophrenia. Schizophr Res 16: 1–6
Horrobin DF . (1998): The membrane phospholipid hypothesis as a biochemical basis for the neurodevelopmental concept of schizophrenia. Schizophr Res 30: 193–208
Kaplan RD, Szechtman H, Franco S, Szechtman B, Nahmias C, Garnett ES, List S, Cleghorn JM . (1993): Three clinical syndromes of schizophreniain untreated subjects: Relation to brain glucose activity measured by positron emission tomography. Schizophr Res 11: 47–54
Keshavan MS, Bagwell WW, Haas GL, Sweeney JA, Schooler NR, Pettegrew JW . (1994): Changes in caudate volume with neuroleptic treatment. Lancet 344: 1434
Keshavan MS, Pettegrew JW, Panchalingam K . (1995): MRS in the study of psychoses: Psychopharmacological studies. In Nasrallah H.A. Pettegrew J.W(eds), NMR Spectroscopy in Psychiatric Brain Disorders. Washington DC, American Psychiatric Press, pp 131–146
Kilby PM, Allis JL, Radda GK . (1990): Spin-spin relaxation of the phosphodiester resonance in the 31P NMR spectrum of human brain: The determination of the concentrations of phosphodiester components. FEBS Lett 272: 163–165
Kitamura T, Yuzuriha T, Morita M, Itoh J, Suga R, Nakagawa Y . (1990): Oxford version of the BPRS: Development and validation of subscales. Psychiatric Diag 1: 101–107
Klemm E, Danos P, Grünwald F, Kasper S, Möller H-J, Biersack H-J . (1996): Temporal lobe dysfunction and correlation of regional cerebral blood flow abnormalities with psychopathology in schizophrenia and major depression—a study with single photon emission computed tomography. Psychiatry Res Neuroimag 68: 1–10
Kolakowska T . (1976): Brief Psychiatric Rating Scale: Glossaries and Rating Instructions. Oxford, Oxford University
Lawrie SM, Abukmeil SS . (1998): Brain abnormality in schizophrenia: A systematic and quantitative review of volumetric magnetic resonance imaging studies. Br J Psychiatry 172: 110–120
Liddle PF, Friston KJ, Frith CD, Hirsch SR, Jones T, Frackowiak RSJ . (1992): Patterns of cerebral blood flow in schizophrenia. Br J Psychiatry 160: 179–186
Maier M . (1995): In vivo magnetic resonance spectroscopy: Applications in psychiatry. Br J Psychiatry 167: 299–306
Matsuda H, Jibiki I, Kinuya S, Shuke N, Sumiya H, Tonami N, Hisada K . (1991): Tc-99m HMPAO SPECT analysis of neuroleptic effects on regional brain function. Clin Nucl Med 16: 660–664
McClure RJ, Keshavan MS, Pettegrew JW . (1998): Chemical and physiologic brain imaging in schizophrenia. Psychiatric Clin North Am 21: 93–122
McNamara R, Arias-Mendoza F, Brown TR . (1994): Investigation of broad resonances in 31P NMR spectra of the human brain in vivo. NMR Biomed 7: 237–242
Miller DD, Rezai K, Alliger R, Andreasen NC . (1997): The effect of antipsychotic medication on relative cerebral blood perfusion in schizophrenia: Assessment with technetium-99m hexamethyl-propyleneamine oxime single photon emission computed tomography. Biol Psychiatry 41: 550–559
Murphy EJ, Rajagopalan B, Brindle KM, Radda GK . (1989): Phospholipid bilayer contribution to 31P NMR spectrum in vivo. Magn Reson Med 12: 282–289
Nilsson A, Risberg J, Johnason M, Gustafson L . (1977): Regional changes of cerebral blood flow during haloperidol therapy in patients with paranoid symptoms. Acta Neurol Scand 64(suppl):478–479
Nordahl TE, Kusubov N, Carter C, Salamat S, Cummings AM, O'Shora-Celaya L, Eberling J, Robertson L, Huesman RH, Jagust W, Budinger TF . (1996): Temporal lobe metabolic differences in medication-free outpatients with schizophrenia via the PET-600. Neuropsychopharmacology 15: 541–554
Oldfield RC . (1971): The assessment and analysis of handedness: The Edinburgh Inventory. Neuropsychologia 9: 97–113
Pettegrew JW, Keshavan MS, Panchalingam K, Strychor S, Kaplan DB, Tretta MG, Allen M . (1991): Alterations in brain high-energy phosphate and membrane phospholipid metabolism in first-episode, drug-naive schizophrenics: A pilot study of the dorsal prefrontal cortex by in vivo phosphorus 31 nuclear magnetic resonance spectroscopy. Arch Gen Psychiatry 48: 563–568
Potwarka J, Drost DJ, Williamson PC . (1996): A study of schizophrenia using 2D 31P chemical shift imaging with 1H decoupling (abstract). Proceedings of the 4th Annual Scientific Meeting (New York) SMR, p 998
Puri BK, Richardson AJ . (1998): Sustained remission of positive and negative symptoms of schizophrenia following treatment with eicosapentanoic acid. Arch Gen Psychiatry 55: 188–189
Ross BM, Hudson C, Erlich J, Warsh JJ, Kish SJ . (1997): Increased phospholipid breakdown in schizophrenia: Evidence for the involvement of a calcium-independent phospholipase A2 . Arch Gen Psychiatry 54: 487–494
Sabri O, Erkwoh R, Schreckenberger M, Owega A, Sass H, Buell U . (1997): Correlation of positive symptoms exclusively to hyperperfusion or hypoperfusion of cerebral cortex in never-treated schizophrenics. Lancet 349: 1735–1739
Schachter SC, Ransil BJ, Geschwind N . (1987): Associations of handedness with hair color and learning disabilities. Neuropsychologia 25: 269–276
Shioiri T, Kato T, Inubushi T, Murashita J, Takahashi S . (1994): Correlations of phosphomonoesters measured by phosphorus-31 magnetic resonance spectroscopy in the frontal lobes and negative symptoms in schizophrenia. Psychiatry Res Neuroimag 55: 223–235
Singh SP, Shankar R . (1996): Effect of haloperidol on phospholipid biosynthesis in rat brain. Ind J Exp Biol 34: 111–114
Stanley JA, Panchalingam K, Miller G, McClure RJ, Pettergrew JW . (1997): A new method to quantify the broad component under the phosphodiester resonance and its application to study first-episode never medicated schizophrenics (abstract). Proceedings of the 5th Annual Scientific Meeting (Vancouver) SMR, p 1408
Stanley JA, Williamson PC, Drost DJ, Carr TJ, Rylett RJ, Malla A, Thompson RT . (1995): An in vivo study of the prefrontal cortex of schizophrenic patients at different stages of illness via phosphorus magnetic resonance spectroscopy. Arch Gen Psychiatry 52: 399–406
Williamson PC, Braner M, Leonard S, Thompson T, Drost D . (1996): 31P magnetic resonance spectroscopy studies in schizophrenia. Prostagland Leukot Essent Fatty Acids 55: 115–118
Zipursky RB, Zhang-Wong J, Lambe EK, Bean G, Beiser M . (1998): MRI correlates of treatment response in first episode psychosis. Schizophr Res 30: 81–90
Acknowledgements
This study was partially supported by grants from the Ministry of Science, Culture, and Education (05770735 and 06770764) and the National Center of Psychiatry and Neurology of the Ministry of Health and Welfare (3A-5) of Japan (Dr. H. Fukuzako).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Fukuzako, H., Fukuzako, T., Kodama, S. et al. Haloperidol Improves Membrane Phospholipid Abnormalities in Temporal Lobes of Schizophrenic Patients. Neuropsychopharmacol 21, 542–549 (1999). https://doi.org/10.1016/S0893-133X(99)00050-0
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1016/S0893-133X(99)00050-0
Keywords
This article is cited by
-
Acid sphingomyelinase/ceramide system in schizophrenia: implications for therapeutic intervention as a potential novel target
Translational Psychiatry (2022)
-
Membrane lipidomics in schizophrenia patients: a correlational study with clinical and cognitive manifestations
Translational Psychiatry (2016)