Abstract
Amygdala opioids such as enkephalin appear to play some role in the control of anxiety and the anxiolytic effects of benzodiazepines, although the opioid receptor subtypes mediating such effects are unclear. This study compared the influences of mu-opioid receptor (MOR) activation in the central nucleus of the amygdala (CEA) on unconditioned fear or anxiety-like responses in two models, the elevated plus maze, and the defensive burying test. The role of MORs in the anxiolytic actions of the benzodiazepine agonist diazepam was also examined using both models. Either the MOR agonist [D-Ala2, NMe-Phe4, Gly-ol5]-enkephalin (DAMGO), or the MOR antagonists Cys-Tyr-D-Trp-Arg-Thr-Pen-Thr-NH2 (CTAP) or β-funaltrexamine (FNA) were bilaterally infused into the CEA of rats before testing. The results show that microinjection of DAMGO in the CEA decreased open-arm time in the plus maze, whereas CTAP increased open-arm behaviors. In contrast, DAMGO injections in the CEA reduced burying behaviors and increased rearing following exposure to a predator odor, suggesting a shift in the behavioral response in this context. Amygdala injections of the MOR agonist DAMGO or the MOR antagonist CTAP failed to change the anxiolytic effects of diazepam in either test. Our results demonstrate that MOR activation in the central amygdala exerts distinctive effects in two different models of unconditioned fear or anxiety-like responses, and suggest that opioids may exert context-specific regulation of amygdalar output circuits and behavioral responses during exposure to potential threats (open arms of the maze) vs discrete threats (predator odor).
Similar content being viewed by others
INTRODUCTION
The amygdala plays a key role in mood behaviors and emotional memory processes (Charney et al, 1998; Davis et al, 1994; Davis, 1992; Panksepp, 1990) in addition to being a key structure in mediating the anxiolytic effects of drugs such as benzodiazepines (BZs) (Pesold and Treit, 1995, 1994; Burghardt and Wilson, 2006; Petersen et al, 1985; Scheel-Kruger and Petersen, 1982; Senders and Shekhar, 1995; Menard and Treit, 1999; Kang et al, 2000). The endogenous opioid system also helps to mediate many responses associated with stress or anxiety (Panksepp, 1990; Drolet et al, 2001), and opioid processes in amygdala appear to play some role in the control of anxiety and the anxiolytic effects of BZs, although the opioid peptides and opioid receptor subtypes mediating such effects are unclear. A role for amygdalar enkephalinergic processes in anxiety responses is suggested by several lines of evidence. Large numbers of enkephalin-immunoreactive neurons are observed in the amygdala (Roberts, 1992; Veinante et al, 1997; Fallon and Leslie, 1986; Gray et al, 1984; Harlan et al, 1987), and the central nucleus of the amygdala (CEA) receives enkephalin afferents from the bed nucleus of the stria terminalis (BNST) as well as other amygdalar nuclei (Poulin et al, 2006). The number of enkephalin neurons and enkephalin mRNA expression show differences between high-anxiety and low-anxiety mice, enkephalin mRNA expression in the amygdala is altered by exposure to predator odor, and pre-proenkephalin-knockout mice show increased levels of anxiety-like behaviors (Konig et al, 1996; Hebb et al, 2004; Filliol et al, 2000). Enkephalins interact with both mu-opioid receptors (MORs) and delta-opioid receptors (DORs), both of which are seen in the amygdala (Mansour et al, 1993, 1994a, 1994b, 1987, 1995; Poulin et al, 2006; Wilson et al, 2002; Goodman et al, 1980) and could mediate the effects of amygdalar enkephalin in anxiety or fear responses.
Imaging studies have demonstrated changes in MOR binding states during periods of negative affect in human volunteers (Zubieta et al, 2003), and MOR-knockout mice show reduced anxiety-like behaviors in the elevated plus maze and light–dark box compared with wild-type controls (Sasaki et al, 2002; Filliol et al, 2000). The local infusion of the MOR agonist morphine into the central amygdala has partial anxiolytic effects in the social interaction test (Rogers and File, 1979), whereas administration of an MOR antagonist into the basolateral region decreased time in the lit compartment of a light–dark transition test in mice (Narita et al, 2006). The effects of MOR ligands in central or basolateral amygdala are supported by the distribution of MOR mRNA and immunoreactivity, and MORs are highly expressed in the intercalated nuclei (IC) and basolateral regions of amygdala, with some expression in the CEA (Poulin et al, 2006; Wilson et al, 2002; Jacobsen et al, 2006). Since the IC are clusters of densely packed GABAergic neurons interspersed between CEA and basolateral regions that receive projections from the prefrontal cortex, the dense localization of MORs in the IC also provides a mechanism for opioids to modulate the gating of information flow between the basolateral and central amygdala (Delaney and Sah, 2001; Royer et al, 1999, 2000b; Royer and Pare, 2002), or the prefrontal inputs to CEA that help regulate fear processes (Berretta et al, 2005; Marowsky et al, 2005; Freedman et al, 2000; McDonald et al, 1996; Royer and Pare, 2002; Quirk et al, 2003).
In addition to these influences on basal anxiety state, endogenous opioid processes appear to be involved in the anxiolytic actions of BZs. Several studies support the possibility that anxiolytic effects of BZs in conflict-based procedures, including the plus maze, might be inhibited by opioid antagonists (Soubrie et al, 1980; Billingsley and Kubena, 1978; Agmo et al, 1995; Tsuda et al, 1996; Koob et al, 1980). The situation is less clear for defensive prod burying, although shock-induced freezing is disrupted by naloxone (Fanselow and Bolles, 1979; Treit et al, 1993; Treit, 1985; de Boer and Koolhaas, 2003). BZs can modulate enkephalin release (Harsing et al, 1982) and we have shown that herpes virus-mediated overexpression of enkephalin in the amygdala potentiates the anxiolytic effects of the BZ agonist diazepam in the plus maze test (Kang et al, 2000; Primeaux et al, 2006). The effects of enkephalin overexpression are reversed by systemic administration of the non-selective opioid receptor antagonist naloxone (Kang et al, 2000) and the DOR antagonist naltrindole (Primeaux et al, 2006). We have also shown that localized injections of the non-selective antagonist naltrexone in the CEA, but not the basolateral nucleus, attenuate the anxiolytic influences of diazepam in the elevated plus maze (Burghardt and Wilson, 2006).
The present study compared the influences of MOR activation in the CEA on unconditioned fear and anxiety-related responses in two models, the elevated plus maze and the defensive burying test. The role of MORs in the anxiolytic actions of the BZ agonist diazepam was also examined in these models. It has been suggested that these models assess differing aspects of fear or anxiety responses (Green, 1991). The elevated plus maze takes advantage of the animal's natural tendencies to avoid brightly lit, open, elevated spaces, but relies on a passive avoidance response to detect anxiety behavior (e.g., avoidance of open arms), and can be confounded by changes in activity levels. In contrast, the defensive prod-burying model is less affected by locomotor changes and (more importantly) the index of anxiety involves an active behavioral response, specifically burying of a discrete object. These tests were selected since they appear to be differentially influenced by both amygdalar processes and opioid drugs (Soubrie et al, 1980; Grijalva et al, 1990; Fanselow and Bolles, 1979; Kopchia et al, 1992; Treit et al, 1993; de Boer and Koolhaas, 2003; Treit, 1985; Billingsley and Kubena, 1978; Agmo et al, 1995; Tsuda et al, 1996; Koob et al, 1980).
METHODS
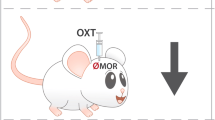
To examine the role of MOR activation in these models, either the MOR agonist [D-Ala2, NMe-Phe4, Gly-ol5]-enkephalin (DAMGO), or the MOR antagonists Cys-Tyr-D-Trp-Arg-Thr-Pen-Thr-NH2 (CTAP) or β-funaltrexamine (FNA) were bilaterally infused into the CEA of rats before testing in the plus maze or defensive burying test. In addition, we examined the role of MOR activation on responses seen with a moderate dose of the BZ agonist diazepam. The diazepam dose was selected based on prior studies (Wilson et al, 2004) to permit detection of potential increases or decreases in diazepam-induced effects in these tests.
Subjects
For all experiments, male Long Evans rats (Harlan, Indianapolis, IN), weighing approximately 175 g upon arrival, were housed singly in an environmentally controlled animal facility on a 12:12 light/dark cycle, with lights on at 0700 hours. Purina rat chow and water were available ad libitum. Animals were housed in an animal facility approved by the Association for Assessment and Accreditation of Laboratory Animal Care (AAALAC), and all procedures were approved by the University of South Carolina Animal Care and Use Committee. Behavioral testing was initiated and completed during the light cycle between 0800 and 1200 hours.
Surgery
One week before testing, bilateral cannula aimed at the CEA were implanted using stereotaxic procedures. Animals were anesthetized with sodium pentobarbital (75 mg/kg, i.p.) and given injections of local anesthetic (1.5% carbocaine, subcutaneous) at pressure points for the earbars and the incision site. The rat was placed in a Kopf stereotaxic unit with the skull flat, the incision site was scrubbed with betadine wash, and a mid-saggital incision was used to expose the skull. The coordinates for CEA were A/P −2.3, M/L+4.0, D/V –6.3 from skull as determined from Bregma based on the atlas of Paxinos and Watson (1997). The tips of the 26-gauge guide cannula (ID, 0.433 inches; Plastics One, Roanoke, VA) were positioned 2 mm above the CEA. Cannulas were anchored to three skull screws (Plastics One) using Ortho-Jet cold-setting dental acrylic (Lang Dental, Wheeling, IL). Nalbuphine (1 mg/kg, subcutaneous) was given postoperatively for pain management and the diet supplemented with bacon softies (Bio-serve, Frenchtown, NJ) was given post-surgically in order to maintain postoperative weight. We allowed a week before testing for post-surgical recovery, and to insure that this single injection of the weak partial agonist nalbuphine would not influence our results with MOR agonists or antagonists. Studies have shown that nalbuphine is a relatively weak partial agonist at MORs (Traynor et al, 2002), and that there is little change in MOR binding even after continuous 7-day exposure to more potent agonists in vivo (Pawar et al, 2007).
Drugs and Microinjections
Rats were habituated to injection procedures on days 4 through 6 after surgery, and dummy cannula were checked and cleaned during these handling sessions. One week after surgery, animals were lightly restrained in a towel in order to remove dummy cannula and insert the injector cannula. Bilateral intra-amygdalar injections were administered by two 2-μl Hamilton microsyringes (Hamilton Co., Reno, NV) controlled by a Harvard Apparatus PHD 2000 microinfusion pump (Harvard, Holliston, MA). Microsyringes were connected to 33-gauge injector cannula (ID, 0.004 inches; Plastics One Inc.) by polyethylene tubing (ID, 0.023 inches). Displacement of an air bubble in the polyethylene tubing was used to confirm injection. Injections were given over a 2-minute period (0.3 μl at the rate of 0.15 μl/min), with 60 s allowed after the injection to permit drug spread. Immediately following the intra-amygdalar injection, dummy cannulas were replaced and animals were given systemic injections of either diazepam (1 mg/kg, i.p.) or vehicle (40% propylene glycol, 10% ethanol).
The MOR agonist DAMGO (0.5 μg/0.3 μl; Ragnauth et al, 2000; Hurley et al, 2003; Gonzalez-Nicolini et al, 2003) and the MOR antagonist CTAP (1 μg/0.3 μl; Gonzalez-Nicolini et al, 2003; Tang et al, 2005; Tershner and Helmstetter, 2000) were obtained from Sigma-Aldrich (St Louis, MO) and prepared in 0.9% sterile saline. The non-competitive MOR antagonist FNA (4 μg/0.3 μl; Ward et al, 1982, 1985; Negus et al, 1993; Primeaux et al, 2006) was prepared in 15% cyclodextran–0.9% saline and was injected at least 24 h (plus maze) or 7 days (burying) before testing. Cyclodextrin is a cyclic sucrose array that increases drug solubility but is inert and secreted rapidly (see Wall and Messier, 2000), and injection of this vehicle had no effect (compared with other control groups) on anxiety or activity measures. Meilandt et al (2004) demonstrated that injections of FNA could depress MOR binding in the hippocampus after such injections by as much as 49% at 24 h, and decreases persisted for up to 11 days (Meilandt et al, 2004). This dose of FNA in the nucleus accumbens can also block the effects of DAMGO-induced feeding at 24 h (Ragnauth et al, 2000). Control rats received similar injections of the appropriate vehicle with each compound. Since no differences were seen between groups of vehicle-treated rats, these were combined for statistical analysis. Doses of agonists and antagonists were selected based on review of the literature, and were doses that had previously demonstrated MOR-selective effects in multiple systems (see references above). Although dose response analysis would be advantageous, repeatedly testing animals in the plus maze and other novelty-based fear models is problematic (Fernandes and File, 1996; File and Zangrossi, 1993), and the use of distinct groups in dose response analysis was deemed an excessive use of rats before the analysis of effective doses in these tests.
Behavioral Testing
Elevated plus maze
One week after cannula implantation, animals were injected bilaterally with vehicle, DAMGO, CTAP, or FNA (24 h earlier) into the amygdala, given a systemic injection of vehicle or diazepam, and tested in the elevated plus maze 30 min later. Each rat was only tested once in the plus maze. The elevated plus maze has been successfully used as a test for anxiolytic agents (Lister, 1987; Pellow et al, 1985), and diazepam (Wilson et al, 2004; Pellow et al, 1985) increases open-arm behavior in the maze. Animals were placed on the elevated plus maze 30 min after the systemic injection of diazepam to allow for the peak anxiolytic effects of each drug without substantial sedation (Wilson et al, 2004). This test was conducted as described in Burghardt and Wilson (2006), as modified from Pellow et al (1985). The black Plexiglas elevated plus maze consisted of two opposing open (56 × 10 × 1 cm), and two closed arms (56 × 10 × 40 cm) elevated 50 cm above the floor, and had a 0.5-cm edge on the open arms. The floor was a gray Plexiglas to accommodate the automated scoring using contrast analysis with Ethovision. Animals were placed in the center square facing an open arm and allowed to explore the maze for 5 min while their behavior was videotaped for later analysis. The animals were tested under high-light conditions (200 lux) with a white noise generator (Sleepmate; Marpac Corp.) to mask extraneous noise. The maze was cleaned with a 5% ammonium hydroxide solution between rats. Behaviors known to be responsive to anxiolytic drugs were scored and included percent open-arm time (open-arm time/(open-arm time+closed-arm time)) and percent open-arm entries (open-arm entries/(open-arm entries+closed-arm entries)). Activity was determined by total distance moved by the rat in the maze (in centimeters) and closed-arm entries. All behaviors were videotaped and scoring was performed with the behavioral tracking system Ethovision (Noldus, the Netherlands). A correlation of ⩾95% between scoring by a trained observer and the Ethovision tracking system was determined before this set of experiments.
Defensive burying test
Since opioid systems in the amygdala modulate nociceptive responses (Kang et al, 1999), this test was modified from that described in Wilson et al (2004) by substituting a noxious (predator) odor rather than a shock probe. Predator odor can induce a similar burying behavior as that seen after shock probe exposure (see Hebb et al, 2004). A Plexiglas chamber (45 × 30 × 44 cm) filled up to a depth of 5 cm with fresh pine bedding, with a piece of ferret-scented towel (5 cm2) placed 2 cm above bedding, was used for this analysis. One week after plus maze testing, animals were randomized with respect to plus maze treatment, injected with pharmacological agents into the amygdala, and received systemic injections of vehicle or diazepam 30 min before testing. Latency to bury, duration of burying (defined as spraying bedding toward the towel), and rears (defined as number of times animal lifted both forelimbs) were measured by an observer blind to the treatment conditions from videotapes for the duration of the 30 min test. In the absence of burying, animals were assigned a latency to bury of 30 min and duration of burying of zero. These animals are included in the analysis, since this is the effect of anxiolytic drugs in this task. Therefore, the number of animals that showed burying behavior is also reported in the results.
Verification of Cannula Placement
After behavioral testing, rats were deeply anesthetized with sodium pentobarbital (100 mg/kg, i.p.) and bilateral injections of 0.1% thionine were administered with the same injection parameters used for drug injection (see above). A total of 10–20 min following the injection, animals were perfused by intracardiac delivery of 0.9% saline, followed by 10% formalin in 0.05 M phosphate-buffered saline. Brains were removed, blocked, and placed in a sucrose solution (3.5% sucrose in 0.1 M sodium phosphate buffer) for at least 48 h. Brains were sectioned using a sliding microtome at 60 μm, mounted on gelatin-coated slides, and stained using an acetylcholinesterase staining protocol modified from Hedreen et al (1985). Briefly, sections were brought to room temperature and placed in a staining solution of 0.2 M Tris maleate, pH 7.5, 0.1 M sodium citrate, 0.03 M cupric sulfate, 5 mM potassium ferricyanide, and 25 mg acetylthiocholine iodide for 75 min. Following incubation, sections were dipped in deionized H2O followed by 70% ethanol, and coverslipped with Permount (Fisher Scientific, St Louis, MO). Placement of the guide cannula and injector tip (dye injection) were determined and transcribed to corresponding (Paxinos and Watson, 1997) brain atlas plates. Rats injected with MOR agonists and antagonists that did not have accurate bilateral cannula placement were excluded from analysis, although there were sufficient rats with DAMGO administration just outside the CEA during plus maze testing, to allow comparison of their results directly with animals receiving a correctly placed DAMGO injection into the nucleus.
Statistics
The effects of MOR agonist and antagonist injections on behavioral endpoints in the plus maze and defensive burying tests were examined using a one-way analysis of variance (ANOVA), with post hoc Newman–Keuls analysis to discern specific differences between groups. The effects of MOR agonists and antagonists in vehicle-injected and diazepam-injected groups were analyzed independently. Significance level was set at P<0.05. After combining some of the vehicle groups, the unequal N values and a significant Levene statistic indicated a violation of the homogeneity of variance assumption for ANOVA for some measures. In these instances, the Welch's correction for ANOVA and the Dunnett T3 post hoc tests were used to assess main treatment effects and specific group differences, respectively. Differences in the number of subjects showing burying behavior in response to ferret-towel exposure was assessed using χ2-analysis.
RESULTS
Elevated Plus Maze
No differences in percent open-arm times between various amygdalar vehicle-treated groups were seen, and these values did not differ from animals receiving vehicle with placements just outside the CEA (F(2,25)=0.4, P=0.7). Therefore, the data from all animals receiving intracerebral vehicle injections have been combined for analysis.
Injections of the MOR agonist DAMGO and the MOR antagonist CTAP altered basal anxiety measures in the elevated plus maze, but not the anxiety-reducing effects of diazepam. As seen in the upper panel of Figure 1, injections of MOR-selective compounds injected into the CEA altered basal percent open-arm time in the elevated plus maze (F(4,62)=6.76, P=0.0002) following systemic vehicle injections. Placements for drug injections in the amygdala are seen in Figure 2. As seen in the top graph of Figure 1, the MOR agonist DAMGO (0.5 μg/0.3 μl) significantly decreased open-arm behavior, whereas the MOR antagonist CTAP (1 μg/0.3 μl) increased percent open-arm time in the elevated plus maze (P<0.05 vs control). The non-competitive antagonist FNA injected 24 h earlier increased open-arm time slightly in the plus maze, but these values did not differ significantly from control levels. This might have been related to the relatively small number of subjects tested with the non-competitive antagonist (N=6), which may have yielded a type II error. Similar results were seen with open-arm entries (percent open entries were as follows: 33.6±2.8 (vehicle), 14.6±5.7 (DAMGO), 39.2±3.2 (CTAP), 36.3±5.2 (FNA), and 32.3±6.8 (DAMGO outside of CEA); F(4,58)=4.07, P=0.006). The selectively of DAMGO's effects in the CEA are further suggested by the lack of changes in open-arm time when placement of the injection site was outside the CEA (see Figure 1, P>0.5 vs control, N=8). These off-target sites of DAMGO are generally medial, anterior, and ventral to the CEA, and include the globus pallidus/caudate, lateral hypothalamus, endopeduncular nucleus, anterior cortical amygdaloid nucleus, and ventral basolateral amygdala. Other drug-injected (CTAP, FNA) groups did not have sufficient numbers placed outside the CEA for analysis (n<3 rats). The injection of MOR agonists and antagonists into the CEA did not alter activity measures during plus maze exposure. There were no differences in distance traveled on the maze between groups (F(4,18.28)=0.71, P=0.59; Figure 1, bottom graph) or in closed-arm entries (F(4,17.46)=1.41, P=0.27). Closed-arm entries (mean±SEM) were as follows: 14.7±0.7 (vehicle), 18.9±3.5 (DAMGO), 12.3±1.0 (CTAP), 18.0±4.4 (FNA), and 14.4±1.53 (DAMGO outside of CEA).
Anxiety (top) and activity (bottom) measures in the elevated plus maze after injection of the MOR agonist DAMGO or MOR antagonists CTAP and FNA into the central amygdala. Animals received a systemic vehicle injection before testing. DAMGO decreased percent open-arm time in the plus maze, whereas DAMGO injections outside the CEA failed to alter open-arm time in the plus maze. The competitive MOR antagonist CTAP had the opposite effect and increased open-arm time in the plus maze (P<0.05). Bars represent mean±SEM for N=26 for amygdalar vehicle-injected control groups and N=6–13 for drug-treated groups.
Panel (a) shows typical dye injection in the central amygdala. Blue staining (thionin) is seen in the CEA, which is lightly stained by acetylcholinesterase (OT represents optic tract). Panel (b) shows placement of injection sites in the central amygdala for animals used in analysis of DAMGO, CTAP, and FNA in the elevated plus maze (with systemic vehicle injections). Plates are adapted from (Paxinos and Watson, 1997) for representing −2.12 to −3.30 from Bregma.
Although DAMGO and CTAP injections modified basal open-arm behaviors in the plus maze, they failed to modulate the anxiolytic actions of diazepam. A moderate dose of diazepam (1 mg/kg, i.p.) was used in these studies to permit observation of either enhancement or attenuation in the anxiety-reducing properties in this test. Systemic injections of diazepam increased open-arm time above levels seen after vehicle injections, consistent with its anxiolytic properties (24.8±3.2% open-arm time in vehicle (in CEA)–vehicle group compared with 42.4±3.1% open-arm time in vehicle (CEA)–diazepam groups). As seen in the top graph of Figure 3, injections of diazepam increased open-arm time to a similar degree following CEA injections of the MOR agonist DAMGO or the MOR antagonist CTAP or FNA (F(3,53)=0.3, P=0.9 for main effect of drug). No differences were seen between amygdalar treatment groups for open-arm entries (data not shown, F=0.3, P=0.8). This suggests that MOR activation in the CEA does not modulate diazepam's actions in the plus maze. There were no differences in distance traveled on the maze between CEA treatment groups after a systemic injection of diazepam (F(4,65)=1.5, P=0.2; Figure 3, bottom graph).
Modulation of MOR in the central amygdala failed to affect the anxiolytic effects of diazepam in the elevated plus maze. Anxiety (top) and activity (bottom) measures in the elevated plus maze after injection of the MOR agonist DAMGO or MOR antagonists CTAP and FNA into the CEA, plus a systemic diazepam (1 mg/kg, i.p.) injection before testing. Bars represent mean±SEM for N=32 for control group receiving intracerebral vehicle, and N=6–8 for DAMGO, CTAP, or FNA-treated groups.
Defensive Burying
Different groups receiving vehicle into the CEA showed similar behaviors in defensive burying, and these values were not different from animals receiving vehicle injections placed outside the CEA (F(2,45)=0.6, P=0.5 for latency; F(2,45)=0.4, P=0.7 for burying). Therefore, the data from all animals receiving intracerebral vehicle injections have been combined for analysis.
Injection of the MOR agonist and antagonists into the CEA also shifted behaviors in the defensive burying task, as seen by significant effects of drug on burying (F(3,30.88)=12.13, P<0.0001), latency to bury (F(3,40.79)=12.67, P<0.0001) and rearing (F(3,35.67)=6.26, P=0.003). The MOR agonist DAMGO injected into the CEA decreased the amount of burying, increased the latency to bury, and enhanced rearing compared with control (vehicle) levels, as well as levels seen following antagonist administration (see Figure 4). The non-competitive antagonist FNA (injected 7 days earlier) and CTAP had the opposite effects on burying and rearing behaviors when compared with the agonist DAMGO, but post hoc analyses revealed that CTAP only significantly modulated rearing in this task, compared with vehicle (P<0.05; Dunnett T3 post hoc test; see Figure 4). The influences of DAMGO in this test are further illustrated by the shift in the number of rats per group showing any burying behavior during the 30-min test period. After intracerebral injections of vehicle, only 3 of the 46 rats failed to bury during the 30-min period of exposure to a predator (ferret)-scented towel. In contrast, 11 of 18 rats injected with DAMGO in the CEA showed no burying behaviors in the test. χ2-Analysis of frequencies of animals showing burying vs no burying behavior revealed a significant difference in expected frequencies with, χ2(2, N=95)=34.46, P<0.0001. For the antagonists, we pooled the frequencies both antagonist groups (CTAP and FNA), since otherwise the expected frequency of no burying was <5, which violates an assumption of the test.
Anxiety measures in the defensive burying task after injection of the MOR agonist DAMGO or MOR antagonists CTAP and FNA into the central amygdala. DAMGO decreased burying (top), increased the latency to bury (middle), and increased rearing (bottom) in this test, compared with control (vehicle injected) levels of behavior. The competitive MOR antagonist CTAP had little effect on burying and latency to bury, although the non-competitive antagonist β-FNA (injected 7 days earlier) increased burying and CTAP decreased rearing in this test. Bars represent mean±SEM for N=46 for the amygdalar vehicle-injected control groups, and N=12–19 for drug-treated groups.
Only the effects of DAMGO and CTAP were tested with systemic diazepam administration in the defensive burying test. The same dose of diazepam (1 mg/kg, i.p.) was used as in the plus maze. Although this dose of diazepam is marginally effective in this test, higher doses (e.g., 2 mg/kg, i.p.) generally eliminate burying in this test, and so we used a lower dose to permit the observation of potential attenuation or augmentation in diazepam effects (see Wilson et al, 2004). Like the plus maze, as seen in Figure 5, neither DAMGO nor CTAP injections into the CEA significantly affected the actions of diazepam in the defensive burying test (F(2,34)=1.0, P=0.4 for burying; F(2,34)=0.8, P=0.45 for latency). The exception was rearing, and DAMGO significantly elevated rearing over levels in vehicle- and CTAP-injected groups (F(2,34)=5.8, P<0.007).
Modulation of MOR in the central amygdala failed to affect the anxiolytic effects of diazepam in the defensive burying task. Injections of the MOR agonist DAMGO or MOR antagonists CTAP into the CEA did not significantly effect the latency to bury or burying duration produced by a systemic diazepam (1 mg/kg, i.p.) injection before testing. DAMGO did increase rearing behaviors over that seen in rats receiving CTAP or vehicle intracerebrally. Bars represent mean±SEM for N=19 for the diazepam-treated group receiving intracerebral vehicle, and N=8 for the DAMGO- and CTAP-treated groups.
DISCUSSION
Overview of Results
These studies examined the role of the amygdalar MORs in two behavioral models of untrained anxiety-like responses, namely the elevated plus maze and defensive burying test. The results show that activation of MORs in the CEA decreased open-arm time in the plus maze. The response was selective for MORs in the CEA region, since DAMGO injections from placements just outside the CEA failed to change plus maze behaviors. Moreover, microinjections of the antagonist CTAP had the opposite effect and produced an increase in open-arm behaviors in the plus maze. Interestingly, DAMGO injections in the CEA also shifted behaviors in the defensive burying test, including a marked reduction in burying behaviors and increases in rearing behaviors in the test. The effects of DAMGO in this model suggest that MOR activation in CEA shifts the behavioral response during exposure to this discrete predator-odor threat. Amygdala injections of the MOR agonist DAMGO or the MOR antagonist CTAP failed to shift the anxiolytic effects of diazepam in either test. These results demonstrate that opioid neurotransmission via MORs in the CEA can modulate unconditioned anxiety or fear responses, and suggest that opioids may regulate amygdalar output circuits to modulate behavioral responses to both potential (open arms of the maze) and discrete threats (predator odor).
Effects of MORs in the Elevated Plus Maze
In the plus maze, DAMGO decreased open-arm time and the antagonist CTAP produced the opposite effects on open-arm behavior. Previous studies have shown that the local infusion of the MOR agonist morphine into the central amygdala has anxiolytic effects (Rogers and File, 1979). These previous studies, however, demonstrated only partial anxiolytic effects in the social interaction test, but not the open-field test. As with other anxiolytics, morphine's effects were dependent on the light level and familiarity of the testing situation during the social interaction task (Rogers and File, 1979). More consistent with our results, MOR-knockout mice show reduced anxiety-like behaviors in the elevated plus maze and light–dark box compared with wild-type controls (Sasaki et al, 2002; Filliol et al, 2000), although this knockout approach did not target changes in gene expression selectively to the CEA.
Effects of MORs in Defensive Burying
There are few studies examining the role of amygdalar opioid peptides in the defensive burying tests, although in the defensive prod (shock probe) test, systemic administration of the MOR antagonist FNA slightly increased the latency to bury (but not burying duration) and a DOR agonist decreased burying (Primeaux et al, 2006; Perrine et al, 2006). Our results demonstrate that DAMGO injections into the CEA reduced burying behavior, increased latency to bury, reduced the number of animals showing burying behavior, and increased rearing during the test. Although DAMGO reduced burying behavior in the defensive burying task in a manner similar to anxiolytics, this interpretation fails to encompass a potential shift in the full behavioral profile elicited during this test, including the increases in rearing observed with DAMGO injections in the CEA. A previous study demonstrated that both the anxiolytic BZ ligand diazepam and the anxiogenic ligand FG7142 produced decreased burying behavior in the defensive prod-burying test (Rohmer et al, 1990). When Rohmer et al (1990) examined the full behavioral profiles with these two ligands, however, distinct patterns emerged and that included more escape movements, rearing, and reduced prod exploration with FG7142 compared with diazepam. Treit et al (1986) also suggested very early that there was a competitive relationship between burying behavior and avoidance behavior in this test (Treit et al, 1986). Thus, one potential explanation of the result in the defensive burying test is direct MOR activation in the CEA, perhaps via interactions with a distinct set of output neurons in the CEA, induced a shift toward more escape-like or avoidance behaviors rather than burying. This would be supported by the increase in rearing seen with DAMGO administration. This might also explain the decrease in open-arm time in the plus maze with DAMGO, since a shift in behavioral response toward avoidance might not only activate escape-type behavior to a predator (discrete) threat, but also avoidance of an unpredictable threatening environment (open arms of the maze). The antagonists FNA and CTAP generally produced the opposite effects on behaviors in the defensive burying task compared with DAMGO, but these differences failed to demonstrate post hoc statistical significance when compared with control groups, with the exception of rearing behaviors. Since the antagonists did not produce significant changes in behavior, this might suggest that direct activation of MORs in the CEA region may induce a shift in the behavioral output during the defensive burying test, but that MOR processes in the CEA are not involved in the normal behavioral responses during the test. Alternatively, perhaps MORs more directly regulate (activate) rearing or escape-type behavioral outputs, rather than burying responses. More refined behavioral analyses will be required to demonstrate whether responses to MOR activation in CEA involve a shift in behavioral outputs that serve to compete with burying behaviors.
An additional caveat to the interpretation of these studies is that we used a modified defensive burying test that involved a predator (ferret) odor rather than a shock probe as the noxious stimulus. This paradigm was selected, however, to avoid the confound that opioid expression in the CEA influences nociceptive processes (Kang et al, 1999). Although this predator-scented stimulus clearly evokes burying behaviors in a manner similar to that seen with a shock (Wilson et al, 2004; Hebb et al, 2004), the behavioral responses and the neural circuits activated by this stimulus might be distinct from that seen with a shock. In fact, studies suggest that predator odors, particularly in a confined environment, activate regions associated with pheromonal responses, including the medial amygdala (Staples et al, 2005), and there are suggestions that inputs from amygdalar nuclei help to regulate the medial hypothalamic defense system activated during predator exposure (Blanchard et al, 2005). Although not seen in all studies, analysis of neuronal activation using cfos has indicated that predator odors can activate the CEA region (Day et al, 2004; Fendt et al, 2005; Dielenberg et al, 2001).
Lack of Evidence for MOR Regulation in the Anxiolytic Actions of Diazepam
These results suggest that MOR activation in the CEA is not involved in the anxiolytic actions of the BZ agonist diazepam in either the plus maze or defensive burying test. Although we have seen that non-selective opioid antagonists injected into the CEA attenuate the anxiolytic actions of diazepam (Burghardt and Wilson, 2006), this may be due to block of DORs or kappa opioid receptors, rather than the MOR, in this area. In fact, the ability of enkephalin overexpression in the CEA to enhance diazepam effects was blocked by systemic administration of the DOR antagonist naltrindole (Primeaux et al, 2006). Although systemic administration of selective MOR antagonists can block the anticonflict effects of diazepam in mice (Tsuda et al, 1996), transgenic MOR-knockout mice also show unaltered anxiolytic effects of diazepam in the elevated plus maze compared with control strains (LaBuda and Fuchs, 2001), and similar anxiety-related effects in response to increases in enkephalin via inhibition of catabolic enzymes (Nieto et al, 2005). Electrophysiological responses to ethanol are also modulated by opioid interactions at the DORs in the CEA (Kang-Park et al, 2007). Several lines of evidence, therefore, suggest that opioids modulate the activity of BZs and perhaps ethanol in the CEA, but these effects appear to involve the DORs, rather than MOR.
Comparison with Enkephalin Overexpression in the Amygdala
Our previous studies using virus-mediated gene transfer to overexpress enkephalin in the amygdalar CEA region did not demonstrate changes in basal anxiety-like behaviors in the plus maze, but rather an enhancement in the anxiolytic actions of diazepam (Primeaux et al, 2006; Kang et al, 2000). Similarly, injections of non-selective antagonists failed to significantly modulate basal anxiety state in this test (Burghardt and Wilson, 2006). Since enkephalin can act on both MORs and DORs, the lack of basal changes in anxiety in the plus maze after pre-proenkephalin overexpression could have been related to offsetting actions on both receptor types in this area. Nieto et al (2005) have demonstrated that MOR-knockout mice respond similarly to increases in endogenous enkephalins as wild-type mice, suggesting a role for DOR in the anxiety-related effects of increases in endogenous enkephalins induced with systemic administration of catabolic inhibitors (Nieto et al, 2005). Similarly, our previous studies have indicated that the effects of enkephalin overexpression on diazepam-induced anxiolysis were blocked by systemic administration of the DOR antagonist naltrindole (Primeaux et al, 2006). Additionally, anatomical studies have demonstrated mismatches between the localization of MOR and enkephalin terminals in the amygdala (Jacobsen et al, 2006), further supporting the likelihood that endogenous enkephalin effects may involve both MOR and DOR interactions in a potentially very complex manner. Such divergent results also highlight the usefulness of combining approaches that directly activate receptors using pharmacological manipulations, with techniques aimed at modifying the endogenous release of neuropeptides during situation-appropriate conditions. It is, however, also likely that approaches that enhance or diminish receptor function for long periods of time (transgenic knockouts or prolonged overexpression) lead to compensatory changes that mask or alter the normal responses to receptor activation.
MOR Activation of Select Neuronal Populations of the Amygdala
Several other studies using microinjection approaches have seen the effects of drug administration on specific behaviors in the plus maze and defensive burying tests (Treit and Menard, 1997; Menard and Treit, 2000; Treit et al, 1993). Lesion studies, including lesions of the amygdala, have similarly suggested dissociations between specific behavioral aspects of these distinct tests of anxiety (Treit and Menard, 1997; Treit et al, 1993). For example, administration of midazolam into the CEA had little effect on open-arm activity in the plus maze, but decreased passive avoidance of the shock probe (Pesold and Treit, 1994, 1995). In the septum, the effects of excitatory amino-acid receptor antagonists suppressed open-arm avoidance in the plus maze and reduced shock-induced burying behavior, without changes in shock-probe avoidance, whereas other ligands shifted both shock-probe avoidance and burying, without altering open-arm avoidance (Menard and Treit, 2000).
The distinct behavioral effects in these two paradigms may be related to the direct effects of MOR agonists on different neuronal populations in the CEA. Electrophysiological studies in amygdalar slices have suggested that the effects of MOR agonists in CEA are dependent upon characterization of the cell type in this area (Finnegan et al, 2005; Zhu and Pan, 2004, 2005; Chieng et al, 2006). In one study, DAMGO evoked an outward current in approximately 60% of CEA neurons that included cells projecting to several different nuclei, including BNST, parabrachial nucleus, and thalamic nuclei (Chieng et al, 2006). In an analogous manner, Zhu and Pan (2004) found that DAMGO evoked outward current in one type of CEA neurons (the so-called A1 cells), but that type B neurons showed no effect of MOR agonists (Zhu and Pan, 2004). Recordings from CEA neurons that selectively project to the ventrolateral periaqueductal gray (vlPAG) demonstrated that DAMGO decreased the frequency of inhibitory post-synaptic currents (IPSCs) in approximately half of these neurons, and also decreased IPSCs evoked by stimulation of the basolateral amygdala (Finnegan et al, 2005). Taken together, these studies demonstrate that distinct sets of neurons appear to respond to MOR agonists (Zhu and Pan, 2004; Chieng et al, 2006); that MOR agonists can reduce the activity of CEA projection neurons to the vlPAG, parabrachial nucleus, BNST, and thalamic reticular nucleus (Finnegan et al, 2005; Chieng et al, 2006); and that MOR agonists can also alter presynaptic release of GABA and glutamate in the amygdala (Finnegan et al, 2005, 2006; Zhu and Pan, 2005). Activation of MOR on these different populations of CEA output neurons seen in electrophysiological analyses may help shift specific aspects of behavioral responses based on the environmental context during the test, which may activate or inhibit distinct neural amygdalar circuits or projections.
It is possible that the sites of injections within the CEA were not identical for both tests and could have contributed to the divergent results. The medial and lateral CEA, for example, show differences in both afferent and efferent projections, as well as divergent electrophysiological and neurochemical profiles, but there were insufficient numbers of subjects to subdivide the injection sites based on sub-regions of the CEA. An additional possibility is that MOR activation in the IC, which is difficult to completely prevent with these microinjection approaches, given their distribution through the amygdala, could serve to modulate the gating of information between the basolateral region and the CEA, and/or the regulatory influences of inputs from the prefrontal cortex (Royer et al, 1999). The IC shows very dense labeling of MOR mRNA and immunoreactivity (Poulin et al, 2006; Wilson et al, 2002; Jacobsen et al, 2006). These IC clusters receive topographic glutamatergic inputs from the basolateral region, and have been shown to generate feed-forward inhibition of CeA neurons (Delaney and Sah, 2001; Royer et al, 1999, 2000b; Royer and Pare, 2002). Moreover, IC neurons show neuronal plasticity in the form of both long-term potentiation and depression (Royer and Pare, 2002), and receive large projections from the prefrontal cortices (McDonald et al, 1996; Freedman et al, 2000). Since stimulation of the prefrontal cortex induces neuronal activation (cfos) in the IC, it has been suggested that the IC may serve as an interface for prefrontal regulation of CEA, which may contribute to learned fear processes and particularly extinction (Berretta et al, 2005; Royer and Pare, 2002; Quirk et al, 2003). In these situations with unconditioned anxiogenic stimuli, perhaps MOR activation regulates the impact of inputs from the prefrontal cortex in a manner similar to dopamine, which is also dense in the IC (Marowsky et al, 2005; Jacobsen et al, 2006). Further, MOR may regulate the context-specific gating of information flow provided by IC neurons between topographic inputs from different regions of the basolateral amygdala into the CEA (Royer and Pare, 2002; Royer et al, 1999, 2000a, 2000b; Pare et al, 2003). Additional studies, however, will be needed to further elucidate how amygdalar MOR activation shifts behavioral responses in other unconditioned and conditioned behavioral paradigms, and the role of other opioid receptor subtypes in these responses.
References
Agmo A, Galvan A, Heredia A, Morales M (1995). Naloxone blocks the antianxiety but not the motor effects of benzodiazepines and pentobarbital: experimental studies and literature review. Psychopharmacology 120: 186–194.
Berretta S, Pantazopoulos H, Caldera M, Pantazopoulos P, Pare D (2005). Infralimbic cortex activation increases c-Fos expression in intercalated neurons of the amygdala. Neuroscience 132: 943–953.
Billingsley ML, Kubena RK (1978). The effects of naloxone and picrotoxin on the sedative and anticonflict effects of benzodiazepines. Life Sci 22: 897–906.
Blanchard DC, Canteras NS, Markham CM, Pentkowski NS, Blanchard RJ (2005). Lesions of structures showing FOS expression to cat presentation: effects on responsivity to a Cat, Cat odor, and nonpredator threat. Neurosci Biobehav Rev 29: 1243–1253.
Burghardt PR, Wilson MA (2006). Microinjection of naltrexone into the central, but not the basolateral, amygdala blocks the anxiolytic effects of diazepam in the plus maze. Neuropsychopharmacology 31: 1227–1240.
Charney DS, Grillon CCG, Bremner JD (1998). The neurobiological basis of anxiety and fear: circuits, mechanisms, and neurochemical interactions (part I). Neuroscientist 4: 35–44.
Chieng BC, Christie MJ, Osborne PB (2006). Characterization of neurons in the rat central nucleus of the amygdala: cellular physiology, morphology, and opioid sensitivity. J Comp Neurol 497: 910–927.
Davis M (1992). The role of the amygdala in fear and anxiety. Annu Rev Neurosci 15: 353–375.
Davis M, Rainnie D, Cassell M (1994). Neurotransmission in the rat amygdala related to fear and anxiety. Trends Neurosci 17: 208–214.
Day HE, Masini CV, Campeau S (2004). The pattern of brain c-fos mRNA induced by a component of fox odor, 2,5-dihydro-2,4,5-Trimethylthiazoline (TMT), in rats, suggests both systemic and processive stress characteristics. Brain Res 1025: 139–151.
de Boer SF, Koolhaas JM (2003). Defensive burying in rodents: ethology, neurobiology and psychopharmacology. Eur J Pharmacol 463: 145–161.
Delaney AJ, Sah P (2001). Pathway-specific targeting of gaba(a) receptor subtypes to somatic and dendritic synapses in the central amygdala. J Neurophysiol 86: 717–723.
Dielenberg RA, Hunt GE, McGregor IS (2001). ‘When a rat smells a cat’: the distribution of Fos immunoreactivity in rat brain following exposure to a predatory odor. Neuroscience 104: 1085–1097.
Drolet G, Dumont EC, Gosselin I, Kinkead R, Laforest S, Trottier JF (2001). Role of endogenous opioid system in the regulation of the stress response. Prog Neuropsychopharmacol Biol Psychiatry 25: 729–741.
Fallon JH, Leslie FM (1986). Distribution of dynorphin and enkephalin peptides in the rat brain. J Comp Neurol 249: 293–336.
Fanselow MS, Bolles RC (1979). Naloxone and shock-elicited freezing in the rat. J Comp Physiol Psychol 93: 736–744.
Fendt M, Endres T, Lowry CA, Apfelbach R, McGregor IS (2005). TMT-induced autonomic and behavioral changes and the neural basis of its processing. Neurosci Biobehav Rev 29: 1145–1156.
Fernandes C, File SE (1996). The influence of open arm ledges and maze experience in the elevated plus-maze. Pharmacol Biochem Behav 54: 31–40.
File SE, Zangrossi Jr H (1993). ‘One-trial tolerance’ to the anxiolytic actions of benzodiazepines in the elevated plus-maze, or the development of a phobic state? Psychopharmacology (Berlin) 110: 240–244.
Filliol D, Ghozland S, Chluba J, Martin M, Matthes HW, Simonin F et al (2000). Mice deficient for delta- and mu-opioid receptors exhibit opposing alterations of emotional responses. Nat Genet 25: 195–200.
Finnegan TF, Chen SR, Pan HL (2005). Effect of the {mu} opioid on excitatory and inhibitory synaptic inputs to periaqueductal gray-projecting neurons in the amygdala. J Pharmacol Exp Ther 312: 441–448.
Finnegan TF, Chen SR, Pan HL (2006). Mu opioid receptor activation inhibits GABAergic inputs to basolateral amygdala neurons through Kv1.1/1.2 channels. J Neurophysiol 95: 2032–2041.
Freedman LJ, Insel TR, Smith Y (2000). Subcortical projections of area 25 (subgenual cortex) of the macaque monkey. J Comp Neurol 421: 172–188.
Gonzalez-Nicolini MV, Berglind W, Cole KS, Keogh CL, McGinty JF (2003). Local mu and delta opioid receptors regulate amphetamine-induced behavior and neuropeptide mRNA in the striatum. Neuroscience 121: 387–398.
Goodman RR, Snyder SH, Kuhar MJ, Young WS (1980). Differential of delta and mu opiate receptor localizations by light microscopic autoradiography. Proc Natl Acad Sci USA 77: 2167–2174.
Gray TS, Cassell MD, Kiss JZ (1984). Distribution of pro-opiomelanocortin-derived peptides and enkephalins in the rat central nucleus of the amygdala. Brain Res 306: 354–358.
Green S (1991). Benzodiazepines, putative anxiolytics and animal models of anxiety. Trends Neurosci 14: 101–104.
Grijalva CV, Levin ED, Morgan M, Roland B, Martin FC (1990). Contrasting effects of centromedial and basolateral amygdaloid lesions on stress-related responses in the rat. Physiol Behav 48: 495–500.
Harlan RE, Shivers BD, Romano GJ, Howells RD, Pfaff DW (1987). Localization of preproenkephalin mRNA in the rat brain and spinal cord by in situ hybridization. J Comp Neurol 258: 159–184.
Harsing LG, Yang HY, Costa E (1982). Evidence for gamma-aminobutyric acid mediation in the benzodiazepine inhibition of the release of met5-enkephalin elicited by depolarization. J Pharmacol Exp Ther 220: 616–620.
Hebb AL, Zacharko RM, Gauthier M, Trudel F, Laforest S, Drolet G (2004). Brief exposure to predator odor and resultant anxiety enhances mesocorticolimbic activity and enkephalin expression in CD-1 mice. Eur J Neurosci 20: 2415–2429.
Hedreen JC, Bacon SJ, Price DL (1985). A modified histochemical technique to visualize acetylcholinesterase-containing axons. J Histochem Cytochem 33: 134–140.
Hurley RW, Banfor P, Hammond DL (2003). Spinal pharmacology of antinociception produced by microinjection of mu or delta opioid receptor agonists in the ventromedial medulla of the rat. Neuroscience 118: 789–796.
Jacobsen KX, Hoistad M, Staines WA, Fuxe K (2006). The distribution of dopamine D1 receptor and mu-opioid receptor 1 receptor immunoreactivities in the amygdala and interstitial nucleus of the posterior limb of the anterior commissure: relationships to tyrosine hydroxylase and opioid peptide terminal systems. Neuroscience 141: 2007–2018.
Kang W, Wilson MA, Wilson SP (2000). Overexpression of proenkephalin in the amygdala potentiates the anxiolytic effects of benzodiazepines. Neuropsychopharmacology 22: 77–88.
Kang W, Wilson SP, Wilson MA (1999). Changes in nociceptive and anxiolytic responses following herpes virus-mediated preproenkephalin overexpression in rat amygdala are naloxone-reversible and transient. Ann N Y Acad Sci 877: 751–755.
Kang-Park MH, Kieffer BL, Roberts AJ, Siggins GR, Moore SD (2007). Presynaptic {delta} opioid receptors regulate ethanol actions in central amygdala. J Pharmacol Exp Ther 320: 917–925.
Konig M, Zimmer AM, Holmes PV, Crawley JN, Brownstein MJ et al (1996). Pain responses, anxiety and aggression in mice deficient in pre-proenkephalin. Nature (London) 383: 535–538.
Koob GF, Strecker RE, Bloom FE (1980). Effects of naloxone on the anticonflict properties of alcohol and chlordiazepoxide. Subst Alcohol Actions Misuse 1: 447–457.
Kopchia KL, Altman HJ, Commissaris RL (1992). Effects of lesions of the central nucleus of the amygdala on anxiety-like behaviors in the rat. Pharmacol Biochem Behav 43: 453–461.
LaBuda CJ, Fuchs PN (2001). The anxiolytic effect of acute ethanol of diazepam exposure is unaltered in mu-opioid receptor knockout mice. Brain Res Bull 55: 755–766.
Lister RG (1987). The use of a plus-maze to measure anxiety in the mouse. Psychopharmacology (Berlin) 92: 180–185.
Mansour A, Fox CA, Akil H, Watson SJ (1995). Opioid-receptor mRNA expression in the rat CNS: anatomical and functional implications. Trends Neurosci 18: 22–29.
Mansour A, Fox CA, Burke S, Meng F, Thompson RC, Akil H et al (1994a). Mu, delta, and kappa opioid receptor mRNA expression in the rat CNS: an in situ hybridization study. J Comp Neurol 350: 412–438.
Mansour A, Fox CA, Meng F, Akil H, Watson SJ (1994b). Kappa 1 receptor mRNA distribution in the rat CNS: comparison to kappa receptor binding and prodynorphin mRNA. Mol Cell Neurosci 5: 124–144.
Mansour A, Khachaturian H, Lewis ME, Akil H, Watson SJ (1987). Autoradiographic differentiation of mu, delta, and kappa opioid receptors in the rat forebrain and midbrain. J Neurosci 7: 2445–2464.
Mansour A, Thompson RC, Akil H, Watson SJ (1993). Delta opioid receptor mRNA distribution in the brain: comparison to delta receptor binding and proenkephalin mRNA. J Chem Neuroanat 6: 351–362.
Marowsky A, Yanagawa Y, Obata K, Vogt KE (2005). A specialized subclass of interneurons mediates dopaminergic facilitation of amygdala function. Neuron 48: 1025–1037.
McDonald AJ, Mascagni F, Guo L (1996). Projections of the medial and lateral prefrontal cortices to the amygdala: a Phaseolus vulgaris leucoagglutinin study in the rat. Neuroscience 71: 55–75.
Meilandt WJ, Barea-Rodriguez E, Harvey SA, Martinez Jr JL (2004). Role of hippocampal CA3 mu-opioid receptors in spatial learning and memory. J Neurosci 24: 2953–2962.
Menard J, Treit D (1999). Effects of centrally administered anxiolytic compounds in animal models of anxiety. Neurosci Biobehav Rev 23: 591–613.
Menard J, Treit D (2000). Intra-septal infusions of excitatory amino acid receptor antagonists have differential effects in two animal models of anxiety. Behav Pharmacol 11: 99–108.
Narita M, Kaneko C, Miyoshi K, Nagumo Y, Kuzumaki N, Nakajima M et al (2006). Chronic pain induces anxiety with concomitant changes in opioidergic function in the amygdala. Neuropsychopharmacology 31: 739–750.
Negus SS, Henriksen SJ, Mattox A, Pasternak GW, Portoghese PS, Takemori AE et al (1993). Effect of antagonists selective for mu, delta and kappa opioid receptors on the reinforcing effects of heroin in rats. J Pharmacol Exp Ther 265: 1245–1252.
Nieto MM, Guen SL, Kieffer BL, Roques BP, Noble F (2005). Physiological control of emotion-related behaviors by endogenous enkephalins involves essentially the delta opioid receptors. Neuroscience 135: 305–313.
Panksepp J (1990). The psychoneurology of fear: evolutionary perspectives and the role of animal models in understanding human anxiety. In: Burrows GD, Roth M, Noyes Jr R (eds). The Neurobiology of Anxiety. Elsevier Science Publishers BV: Amsterdam, pp 3–58.
Pare D, Royer S, Smith Y, Lang EJ (2003). Contextual inhibitory gating of impulse traffic in the intra-amygdaloid network. Ann N Y Acad Sci 985: 78–91.
Pawar M, Kumar P, Sunkaraneni S, Sirohi S, Walker EA, Yoburn BC (2007). Opioid agonist efficacy predicts the magnitude of tolerance and the regulation of mu-opioid receptors and dynamin-2. Eur J Pharmacol 563: 92–101.
Paxinos G, Watson C (1997). The Rat Brain in Stereotaxic Coordinates. Academic Press: San Diego.
Pellow S, Chopin P, File SE, Briley M (1985). Validation of open:closed arm entries in the elevated plus-maze as a measure of anxiety in the rat. J Neurosci Methods 14: 149–167.
Perrine SA, Hoshaw BA, Unterwald EM (2006). Delta opioid receptor ligands modulate anxiety-like behaviors in the rat. Br J Pharmacol 147: 864–872.
Pesold C, Treit D (1994). The septum and amygdala differentially mediate the anxiolytic effects of benzodiazepines. Brain Res 638: 295–301.
Pesold C, Treit D (1995). The central and basolateral amygdala differentially mediate the anxiolytic effects of benzodiazepines. Brain Res 671: 213–221.
Petersen EN, Braestrup C, Scheel-Kruger J (1985). Evidence that the anticonflict effect of midazolam in the amygdala is mediated by the specific benzodiazepine receptors. Neurosci Lett 53: 285–288.
Poulin JF, Chevalier B, Laforest S, Drolet G (2006). Enkephalinergic afferents of the centromedial amygdala in the rat. J Comp Neurol 496: 859–876.
Primeaux SD, Wilson SP, McDonald AJ, Mascagni F, Wilson MA (2006). The role of delta opioid receptors in the anxiolytic actions of benzodiazepines. Pharmacol Biochem Behav 85: 545–554.
Quirk GJ, Likhtik E, Pelletier JG, Pare D (2003). Stimulation of medial prefrontal cortex decreases the responsiveness of central amygdala output neurons. J Neurosci 23: 8800–8807.
Ragnauth A, Moroz M, Bodnar RJ (2000). Multiple opioid receptors mediate feeding elicited by mu and delta opioid receptor subtype agonists in the nucleus accumbens shell in rats. Brain Res 876: 76–87.
Roberts GW (1992). Neuropeptides: cellular morphology, major pathways, and functional considerations. In: Aggleton JP (ed). The Amygdala: Neurobiological Aspects of Emotion, Memory, and Mental Dysfunction. Wiley-Liss Inc.: New York, pp 115–142.
Rogers RJ, File SE (1979). Exploratory behavioral and aversive thresholds following intra-amygdala application of opiates in rats. Pharmacol Biochem Behav 11: 505–511.
Rohmer J-G, Di Scala G, Sandner G (1990). Behavioral analysis of the effects of benzodiazepine receptor ligands in the conditioned burying paradigm. Behav Brain Res 38: 45–54.
Royer S, Martina M, Pare D (1999). An inhibitory interface gates impulse traffic between the input and output stations of the amygdala. J Neurosci 19: 10575–10583.
Royer S, Martina M, Pare D (2000a). Bistable behavior of inhibitory neurons controlling impulse traffic through the amygdala: role of a slowly deinactivating K+ current. J Neurosci 20: 9034–9039.
Royer S, Martina M, Pare D (2000b). Polarized synaptic interactions between intercalated neurons of the amygdala. J Neurophysiol 83: 3509–3518.
Royer S, Pare D (2002). Bidirectional synaptic plasticity in intercalated amygdala neurons and the extinction of conditioned fear responses. Neuroscience 115: 455–462.
Sasaki K, Fan LW, Tien LT, Ma T, Loh HH, Ho IK (2002). The interaction of morphine and gamma-aminobutyric acid (GABA)ergic systems in anxiolytic behavior: using mu-opioid receptor knockout mice. Brain Res Bull 57: 689–694.
Scheel-Kruger J, Petersen EN (1982). Anticonflict effect of the benzodiazpines mediated by a GABAergic mechanism in the amygdala. Eur J Pharmacol 82: 115–116.
Senders S, Shekhar A (1995). Anxiolytic effects of chlordiazepoxide blocked by injection of GABAA and benzodiazepine receptor antagonists in the region of the anterior basolateral amygdala of rats. Biol Psychiatry 37: 437–476.
Soubrie P, Jobert A, Thiebot MH (1980). Differential effects on naloxone against the diazepam-induced release of behavior in rats in three aversive situations. Psychopharmacology 69: 101–105.
Staples LG, Hunt GE, Cornish JL, McGregor IS (2005). Neural activation during cat odor-induced conditioned fear and ‘trial 2’ fear in rats. Neurosci Biobehav Rev 29: 1265–1277.
Tang XC, McFarland K, Cagle S, Kalivas PW (2005). Cocaine-induced reinstatement requires endogenous stimulation of mu-opioid receptors in the ventral pallidum. J Neurosci 25: 4512–4520.
Tershner SA, Helmstetter FJ (2000). Antinociception produced by mu opioid receptor activation in the amygdala is partly dependent on activation of mu opioid and neurotensin receptors in the ventral periaqueductal gray. Brain Res 865: 17–26.
Traynor JR, Clark MJ, Remmers AE (2002). Relationship between rate and extent of G protein activation: comparison between full and partial opioid agonists. J Pharmacol Exp Ther 300: 157–161.
Treit D, Lolordo VM, Armstrong DE (1986). The effects of diazepam on ‘fear’ reactions in rats are modulated by environmental constraints on the rat's defensive repertoire. Pharmacol Biochem Behav 25: 561–565.
Treit D, Menard J (1997). Dissociations among the anxiolytic effects of septal, hippocampal, and amygdaloid lesions. Behav Neurosci 111: 653–658.
Treit D, Pesold C, Rotzinger S (1993). Dissociating the anti-fear effects of septal and amygdaloid lesions using two pharmacologically validated models of rat anxiety. Behav Neurosci 107: 770–779.
Treit D (1985). The inhibitory effect of diazepam on defensive burying: anxiolytic vs analgesic effects. Pharmacol Biochem Behav 22: 47–52.
Tsuda M, Suzuki T, Misawa M, Nagase H (1996). Involvement of the opioid system in the anxiolytic effect of diazepam in mice. Eur J Pharmacol 307: 7–14.
Veinante P, Stoeckel ME, Freund-Mercier MJ (1997). GABA- and peptide-immunoreactivities co-localize in the rat central extended amygdala. Neuroreport 8: 2985–2989.
Wall PM, Messier C (2000). U-69,593 microinjection in the infralimbic cortex reduces anxiety and enhances spontaneous alternation memory in mice. Brain Res 856: 259–280.
Ward SJ, Fries DS, Larson DL, Portoghese PS, Takemori AE (1985). Opioid receptor binding characteristics of the non-equilibrium mu antagonist, beta-funaltrexamine (beta-FNA). Eur J Pharmacol 85: 323–330.
Ward SJ, Portoghese PS, Takemori AE (1982). Pharmacological characterization in vivo of the novel opiate, beta-funaltrexamine. J Pharmacol Exp Ther 82: 494–498.
Wilson MA, Burghardt PR, Ford KA, Wilkinson MB, Primeaux SD (2004). Anxiolytic effects of diazepam and ethanol in two behavioral models: comparison of males and females. Pharmacol Biochem Behav 78: 445–458.
Wilson MA, Mascagni F, McDonald AJ (2002). Sex differences in delta opioid receptor immunoreactivity in rat medial amygdala. Neurosci Lett 328: 160–164.
Zhu W, Pan ZZ (2004). Synaptic properties and postsynaptic opioid effects in rat central amygdala neurons. Neuroscience 127: 871–879.
Zhu W, Pan ZZ (2005). Mu-opioid-mediated inhibition of glutamate synaptic transmission in rat central amygdala neurons. Neuroscience 133: 97–103.
Zubieta JK, Ketter TA, Bueller JA, Xu Y, Kilbourn MR, Young EA et al (2003). Regulation of human affective responses by anterior cingulate and limbic mu-opioid neurotransmission. Arch Gen Psychiatry 60: 1145–1153.
Acknowledgements
This work was supported by RO1 MH063344 to MAW. We thank Drs Jim Fadel and Alexander J McDonald for insightful suggestions on the paper. We also thank Zoie, Valentine, and Pumpkin for donating their ferret-scented towels, and Dr John Hines (Yale University) for enabling their contribution.
Author information
Authors and Affiliations
Corresponding author
Additional information
DISCLOSURE/CONFLICT OF INTEREST
The authors declare that the work was funded by NIH RO1 MH063344, and except for the income received from our primary employer, no financial support of compensation has been received from any individual or corporate entity over the past three years for research or professional service, and there are no personal financial holdings that could be perceived as constituting a potential conflict of interest.
Rights and permissions
About this article
Cite this article
Wilson, M., Junor, L. The Role of Amygdalar Mu-Opioid Receptors in Anxiety-Related Responses in Two Rat Models. Neuropsychopharmacol 33, 2957–2968 (2008). https://doi.org/10.1038/sj.npp.1301675
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1301675
Keywords
This article is cited by
-
Endogenous opioids regulate moment-to-moment neuronal communication and excitability
Nature Communications (2017)
-
Enkephalin Knockdown in the Basolateral Amygdala Reproduces Vulnerable Anxiety-Like Responses to Chronic Unpredictable Stress
Neuropsychopharmacology (2014)
-
Preferential loss of dorsal-hippocampus synapses underlies memory impairments provoked by short, multimodal stress
Molecular Psychiatry (2014)
-
Effects of Antagonists of Mu and Kappa Opioid Receptors on Aggressivity in Male Mice with Repeated Experience of Aggression
Neuroscience and Behavioral Physiology (2014)