Abstract
A new generation of proven or potential antipsychotics, including aripiprazole, bifeprunox, SSR181507 and SLV313, exhibit agonist actions at serotonin 5-HT1A receptors, but little comparative data are available on their pharmacological profiles. Here, we compared in mice the in vivo antipsychotic-like vs cataleptogenic activities of these compounds with those of drugs that exhibit little interaction at 5-HT1A receptors, such as haloperidol, olanzapine and risperidone. All the drugs dose-dependently reduced apomorphine-induced climbing or sniffing and, with the exception of ziprasidone, produced complete suppression of these responses. In the bar catalepsy test, when administered alone, haloperidol, olanzapine and risperidone produced marked catalepsy, whereas, at doses up to 40 mg/kg, aripiprazole, SLV313, SSR181507, and sarizotan produced little or no catalepsy. The latter compounds, therefore, displayed a large separation between doses with ‘antipsychotic-like’ and those with cataleptogenic actions. When 5-HT1A receptors were blocked by pretreatment with WAY100635 (2.5 mg/kg, s.c.), cataleptogenic properties of SSR181507 and sarizotan were unmasked, and the catalepsy induced by bifeprunox was enhanced. In the case of aripiprazole and SLV313, although WAY100635 produced upward shifts in their dose–response, the magnitude of catalepsy appeared to reach an asymptotic plateau, suggesting that other mechanisms may be involved in their low cataleptogenic liability. The present data confirm that 5-HT1A receptor activation reduces or even completely prevents the cataleptogenic potential of novel antipsychotic agents. Further, they indicate that the balance of affinity and/or efficacy between D2 and 5-HT1A receptors profoundly influences their pharmacological activities, and will likely impact their therapeutic profiles.
Similar content being viewed by others
INTRODUCTION
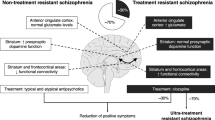
Although conventional neuroleptics control positive symptoms in schizophrenia, they also induce extrapyramidal side effects (EPS) such as dystonia, parkinsonism, akathisia and tardive dyskinesia. These effects are mediated by blockade of dopamine D2 receptors, but their expression can be modulated by other systems, most notably, serotonin (5-HT) (for review, see: Meltzer et al, 2003). Hence, the development of newer generation antipsychotics has been focused on multiple receptorial mechanisms that could lead to improved clinical efficacy and reduced EPS liability. In particular, focus on 5-HT2A and 5-HT2C receptor subtypes led to the development of antipsychotics (eg risperidone and olanzapine) that antagonize these receptors, in addition to D2 receptors. Recently, particular attention has been given to the 5-HT1A receptor as a promising additional target for antipsychotic therapy (for review, see: Millan, 2000; Bantick et al, 2001). In fact, 5-HT1A receptor agonists attenuate antipsychotic-induced EPS in humans (Yoshida et al, 1998), non-human primates (Christoffersen and Meltzer, 1998) and rats (Prinssen et al, 1999, 2002). In addition, 5-HT1A receptor activation increases dopamine release in a regionally-selective manner in the prefrontal cortex (Ichikawa and Meltzer, 2000), suggesting alleviation of the proposed deficiency in dopaminergic neurotransmission in this brain region of schizophrenics (Honey et al, 1999). Indeed, amelioration of this ‘hypofrontality’ is associated with improvement in negative and cognitive symptoms of schizophrenia (Honey et al, 1999). Consistent with this idea, clinical studies have reported that buspirone and tandospirone, two partial agonists at 5-HT1A receptors, substantially ameliorate cognitive performance and reduce the incidence of EPS in schizophrenic patients treated with haloperidol (Sumiyoshi et al, 2001a, 2001b). The atypical antipsychotic clozapine, which displays improved capacity to treat negative symptoms with minimal EPS liability, exhibits agonist properties at 5-HT1A receptors (Newman-Tancredi et al, 1998; Cussac et al, 2002) and both its absence of cataleptogenic properties and its elevation of dopamine release in frontal cortex are partially mediated by 5-HT1A receptors (Millan et al, 1998; Rollema et al, 1997). The ability of clozapine to occupy 5-HT1A receptors in non-human primates at clinically-relevant doses has been demonstrated by PET scans with [3H]WAY100635 (Bantick et al, 2000; Chou et al, 2003). In addition, the more recent antipsychotic, ziprasidone, which also activates 5-HT1A receptors, has a notably low incidence of EPS in humans (Daniel et al, 1999). Lastly, 5-HT1A agonists exert antidepressant- and anxiolytic-like properties (Blier and Ward, 2003), of particular interest to schizophrenic patients of whom an appreciable proportion suffer from comorbid anxiety and/or depression (Buchanan et al, 2002). Thus, combined 5-HT1A agonist and D2 antagonist properties would be expected to have a wider spectrum of activity than currently used antipsychotics, and in particular, exhibit greater efficacy against negative/cognitive symptoms with reduced EPS liability.
In this context, several laboratories have reported the development of a new generation of potential antipsychotic agents with varying levels of agonist/antagonist actions at D2 and 5-HT1A receptors. These compounds, currently in various phases of development, include SLV313 (Glennon et al, 2002), SSR181507 (Claustre et al, 2003), bifeprunox (DU127090; Wolf, 2003) as well as sarizotan (EMD128130; Bartoszyk et al, 2004), that seems, however, to have been lately reoriented towards an antidyskinetic indication. Nonetheless, these compounds display marked diversity in their actions at 5-HT1A receptors in vitro, with varying potencies and efficacies for activation of cellular signal transduction (Newman-Tancredi et al, 2005), likely to profoundly influence their profile of action. Indeed, the extent to which 5-HT1A agonists are able to reverse neuroleptic-induced catalepsy is dependent on their efficacy: high-efficacy activation seems necessary to completely abolish haloperidol-induced catalepsy (Prinssen et al, 1999, 2002). Further, the intrinsic activity of a series of 5-HT1A receptor ligands correlates positively with the magnitude of their antidepressant-like effects in the forced swimming test (Koek et al, 2001). The issue, therefore, arises as to what could be the desirable balance of affinity and efficacy between D2 and 5-HT1A receptors that would exhibit antipsychotic activity with reduced EPS liability.
As no formal comparison between the pharmacological profiles of these new generation ligands is available, we set out to compare the antipsychotic vs cataleptogenic activity of drugs varying in 5-HT1A agonist vs D2 antagonist properties, along with those of more typical and atypical antipsychotics (see Table 1). First, we used the apomorphine-induced climbing and stereotypies tests (considered predictive of antipsychotic potential) and the catalepsy paradigm (thought to predict EPS liability). Second, drug-interaction studies were conducted using the 5-HT1A antagonist, WAY100635 (Forster et al, 1995), with the aim of determining whether activation of 5-HT1A receptors is responsible for ‘masking’ the induction of catalepsy that would be expected following D2 receptor blockade. Such a pattern of pharmacological interaction has been observed in rats for another antipsychotic exhibiting both D2 antagonist properties and, less potently, 5-HT1A agonist properties, nemonapride (Prinssen et al, 1998). This compound induces catalepsy at low doses but, when doses are sufficient to activate 5-HT1A receptors, catalepsy is attenuated, and blockade of 5-HT1A receptors by WAY100635 pretreatment ‘unmasks’ this 5-HT1A receptor influence (Prinssen et al, 1998; Kleven et al, 2005).
METHODS
Animals
Male NMRI mice (Iffa-Credo, Lyon, France) weighing 20–24 g upon arrival were group-housed for a 5-day quarantine period in polycarbonate Type III cages (internal dimensions 375 × 215 × 149 mm3, L × l × H; floor surface 806 cm2) in an environmentally controlled room (ambient temperature, 21±1°C; relative humidity, 55±5%; 12 : 12 light : dark cycle, lights on at 0700). Standard laboratory food (A04; Animal Food and Engineering, Epinay sur Orge, France) and filtered water (0.22 μm pore diameter; in bottles) were freely available. The mice were transferred to the experimental room on the day before experiments and housed individually in polystyrene hanging cages (internal dimensions 220 × 185 × 80 mm3, L × l × H; floor surface 187 cm2), where they were food-restricted but had free access to water. All experiments were performed in a quiet room, between 0900 and 1600, by a single experimenter and in a blind fashion with respect to the treatment administered. Animals were handled and cared for in accordance with the Guide for the Care and Use of Laboratory Animals (National Institutes of Health, USA), the European Directive 86/609, and the internal protocoles (No 194 and 240) were carried out in compliance with local ethical committee guidelines for animal research. Mice were used only once and were killed immediately after the experiment.
Apomorphine-Induced Climbing and Sniffing
Each animal was placed into cylindrical wire-mesh cages (diameter, 14 cm; height, 13 cm; mesh size, 3 mm) and allowed to adapt for 60 min. Thereafter, mice were injected twice, first with test compound or saline (i.p. or s.c.), followed 45 min later by s.c. injection of apomorphine (2.5 mg/kg). The observational method used was an adaptation of the method of Fray et al (1980), combined with a time-sampling procedure (Waddington, 1986). Behavioral observations were made from 55 to 65 min after the first injection: animals were observed for 10 s every minute for the presence or absence of climbing (ie all fours paws on the cage, above the floor). Sniffing was scored when the animal showed uninterrupted sniffing for at least 3 s during this 10 s sampling period. Thus, the score for climbing or sniffing could vary from 0 to 10 for the entire observation period.
Catalepsy
Each animal was injected with the test compound or saline (i.p. or s.c.) and the catalepsy procedure was measured using the bar test 60 min after the injection: the forelimbs were placed on a cylindrical metal bar (diameter, 0.4; 3.5 cm above the table) and the time during which both forelimbs remained on the bar was recorded up to a maximum of 30 s. The test was repeated three times (inter-trial interval: 1 min). Animals were put back in their home cage after each measurement of catalepsy.
In order to investigate the effects of 5-HT1A receptors on catalepsy induced by some antipsychotics, WAY100635 (2.5 mg/kg) or saline were administered s.c., 15 min before test compounds (s.c. or i.p.) that is, 75 min before recording catalepsy.
Analysis of Data
Drug effects on apomorphine-induced behaviors were expressed as the mean±SEM score and the dependent variables used for catalepsy were the mean duration (s) of three trials and the percentage of animals showing a duration of 30 s in one or more trials. Data were analyzed with a one-way ANOVA followed by post hoc comparisons using Dunnett's test. Interactions between WAY100635 and antipsychotics were analyzed with a two-way ANOVA, with pretreatment (WAY100635 or saline) and the doses of antipsychotics as the factors, followed by Dunnett's post hoc tests. A P-value <0.05 was considered statistically significant. To calculate ED50 values, the results were expressed as the percentage of mice showing reduction of apomorphine-induced climbing and sniffing (ie scores <9), and as the percentage of mice presenting at least once a duration of catalepsy of 30 s. The climbing and sniffing criterion for calculation of ED50 were based upon the incidence of each particular behavior observed in control animals treated with apomorphine 2.5 mg/kg (Kleven et al, 1996). ED50 values and their associated confidence limits were calculated with the Litchfield and Wilcoxon probit analysis procedure (Tallarida and Murray, 1987) implemented using a procedure written using the Research Programming Language (RPL) of RS/1 (Bolt, Beranek and Newman, Cambridge, MA), that used all data points between 0 and 100% effects to correct 0 and 100% effects (Litchfield and Wilcoxon, 1949). When less than two intermediate effects were observed, 0 and/or 100% effects were transformed by means of Berkson's adjustment (Hubert, 1984) to permit the use of the Litchfield and Wilcoxon procedure.
Drugs
Ziprasidone HCl, risperidone, olanzapine, aripiprazole, bifeprunox mesylate (DU127090; N-[4-[(3-chloro-4-fluorophenyl)amino]-7-[3-(morpholin-4-yl)propoxy]quinazolin-6-yl]prop-2-enamide mesylate), SSR181507 HCl ((3-exo)-8-benzoyl-N-[[(2S)7-chloro-2,3-dihydro-1,4-benzodioxin-1-yl]methyl]-8-azabicyclo[3.2.1]octane-3-methanamine monohydrochloride), sarizotan HCl (EMD-128130; (-)-3-[[[(R)-2-chromanylmethyl]amino]methyl]-5-(p-fluorophenyl)pyridine monohydrochloride), nemonapride and WAY100635 (N-[2-[4-(2-methoxyphenyl)-1-piperazinyl]ethyl]-N-(2-pyridinyl) cyclohexanecarboxamide dihydrochloride) were synthesized by JL Maurel, Chemistry Department, Centre de Recherche Pierre Fabre (Castres, France). SLV313 (piperazine, 1-(2,3-dihydro-1,4-benzodioxin-5-yl)-4-[[5-(4-fluorophenyl)-3-pyridinyl]methyl) and SLV314 ((2R)-2H-1,4-Benzoxazin-3(4H)-one, 8-[4-[3-(5-fluoro-1H-indol-3-yl)propyl]-1-piperazinyl]-2-methyl) was obtained from Solvay Duphar B.V. (Weesp, The Netherlands). Haloperidol, fluphenazine, eticlopride HCl, raclopride and apomorphine hydrobromide were purchased from Sigma RBI (St Quentin Fallavier, France) and clozapine from Tocris (Illkirch, France).
Raclopride, fluphenazine, eticlopride, WAY100635 and apomorphine were prepared and administered s.c. in distilled water, whereas aripiprazole, bifeprunox, sarizotan, and ziprasidone were prepared as a suspension in aqueous Tween 80 (1% v/v in distilled water) and administered i.p. SSR181507, SLV313, SLV314, nemonapride, haloperidol, clozapine, olanzapine, and risperidone were prepared in distilled water with a drop of lactic acid, after which the pH was adjusted to 5–7 with a 1 N solution of sodium hydroxide and injected s.c. An injection volume of 1 ml/100 g was used throughout and doses refer to the weight of the free base. Taking into consideration that at doses of 40 mg/kg and above several compounds (eg clozapine, olanzapine…) begin to exert major interfering effects (eg ataxia, sedation…) that would greatly complicate interpretation of data, absolute upper limits of 40 mg/kg were retained.
RESULTS
Antagonism of Apomorphine-Induced Climbing and Sniffing
All drugs dose-dependently reduced apomorphine-induced climbing and, with the exception of ziprasidone, produced complete suppression of this response at higher doses (Figure 1, filled circles). Apomorphine-induced sniffing (open circles) was also decreased in a dose-dependent manner over a similar dose-range, except for bifeprunox, SSR181507 and SLV313 that reduced or blocked sniffing only at the higher doses. In contrast, ziprasidone and sarizotan exhibited little effect on apomorphine-induced sniffing, even at the highest dose tested (40 mg/kg).
Effects of antipsychotics on apomorphine-induced climbing (filled circles) and sniffing (open circles) in mice. Values represent the mean±SEM behavioral score of seven animals during observation periods (10 s every min, from 55 to 65 min after drug administration). Apomorphine (2.5 mg/kg, s.c.) was administered 45 min after different doses of antipsychotics. *P<0.05 compared with apomorphine control groups using Dunnett's test, following significant ANOVA. Note the different x-axis scale for nemonapride and bifeprunox. N=7/dose.
Table 2 shows a summary of ED50 estimates, 95% confidence limits and the maximal effects observed. The majority of compounds were somewhat more potent for antagonism of climbing than sniffing behavior. Nevertheless, the confidence limits of their ED50's overlapped. Ziprasidone was the only compound that yielded markedly different ED50's for climbing (2.2 mg/kg) vs sniffing (>40 mg/kg). The ability of the antipsychotics to inhibit apomorphine-induced climbing and sniffing correlated positively (r=0.75 and 0.78, P<0.001, respectively) with their affinity at rat D2 receptors but not with their affinity at rat 5-HT1A receptors (r=−0.17 and −0.28, P>0.05, respectively) (based on affinity values published by Newman-Tancredi et al, 2005).
Catalepsy
Haloperidol and risperidone dose-dependently induced catalepsy at low doses in the bar test (Figure 2). Although bifeprunox, aripiprazole, clozapine, and SLV313 were substantially less effective or potent than haloperidol and risperidone, they too produced dose-dependent increases in catalepsy. Nemonapride induced catalepsy in a biphasic manner: that is, less catalepsy at higher doses. In contrast, SSR181507 and sarizotan did not induce catalepsy when tested at doses up to 40 mg/kg. As shown in Table 2, the ED50 values of drugs that activate 5-HT1A receptors, that is, SSR181507, sarizotan, aripiprazole, clozapine, and SLV313 were greater than 40 mg/kg. In contrast, the ED50 values of haloperidol, eticlopride, fluphenazine, and risperidone, none of which interact with 5-HT1A receptors, were 100-fold lower (0.4, 0.4, 0.29, and 0.65 mg/kg, respectively).
Effects of antipsychotics in the catalepsy bar test in mice. Values represent the duration of catalepsy in s and are expressed as mean±SEM, N=7/dose. The antipsychotics were administered s.c. or i.p. at 60 min before testing. *P<0.05 compared with saline control using Dunnett's test, following significant ANOVA.
The percentage of mice fulfilling the criteria for reduction of apomorphine-induced climbing and presence of catalepsy (for calculations of ED50 values) is illustrated in Figure 3. Bifeprunox, aripiprazole, nemonapride, SLV313, sarizotan, and SSR181507 were characterized by potent reversal of apomorphine-induced climbing with a broad separation with respect to cataleptogenic activity. The catalepsy vs climbing dose ratio was calculated by dividing ED50 values for inhibiting apomorphine-induced climbing with those for eliciting catalepsy: bifeprunox, nemonapride and SLV313 showed wider separation in this dose ratio (173.3–1000) than did haloperidol and risperidone (4.4–5.4: Table 2).
Effects of antipsychotics on apomorphine-induced climbing (filled circles) and in the catalepsy bar test (open squares) in mice. Values represent the percentage of animals showing climbing scores <9 and one or more catalepsy duration of 30s (see Materials and Methods section for details). Drugs on the left-hand side of the graph have little or no interaction at 5-HT1A receptors whereas drugs on the right-hand side of the graph have 5-HT1A agonist properties. This order was retained based on the data of affinity at 5-HT1A receptors for these compounds (Newman-Tancredi et al, 2005). Note the different x-axis scale for nemonapride and bifeprunox. N=7/dose.
Catalepsy in Combination with WAY100635
When administered in combination with saline, WAY100635 (2.5 mg/kg) did not induce catalepsy (data not shown). Pretreatment with WAY100635 produced a shift to the left of the haloperidol and ziprasidone dose–response curve (F(1,48)=5.1 and F(1,36)=5.3, P<0.05, respectively; Figure 4). After pretreatment with WAY100635, significant levels of catalepsy were observed for aripiprazole (F(1,72)=12.4, P<0.001), SLV313 (F(1,60)=25.6, P<0.001), bifeprunox (F(1,96)=33.6, P<0.001) and nemonapride (F(1,60)=14.1, P<0.001). In the case of nemonapride, pretreatment with WAY100635 enhanced significantly the effects of low doses and prevented the decrease in catalepsy at higher doses. For aripiprazole and SLV313, the magnitude of catalepsy appeared to reach an asymptotic plateau (Figure 4). In contrast, pretreatment with WAY100635 produced a marked incidence of catalepsy in SSR181507- and sarizotan- treated rats (F(1,36)=51.2, P<0.001 and F(1,48)=31.8, P<0.001, respectively).
Effects of haloperidol, nemonapride, ziprasidone, aripiprazole, bifeprunox, SSR181507, SLV313 or sarizotan alone or in combination with WAY100635 in the catalepsy bar test. Values are means±SEM of the duration of catalepsy in s, N=7/group. WAY100635 (2.5 mg/kg, s.c.; filled squares) or saline (open squares) was administered 15 min before antipsychotics, which were administered 60 min before testing. *P<0.05 compared with animals treated with saline using Dunnett's test, following significant ANOVA.
DISCUSSION
Several laboratories have reported the development of a new generation of potential antipsychotic agents with varying levels of agonist/antagonist actions at D2 and agonist activity at 5-HT1A receptors. These compounds, currently undergoing various stages of clinical development, include SLV313, SSR181507, and bifeprunox, along with another compound with potent 5-HT1A agonist properties, sarizotan, originally developed as an antipsychotic but more recently redirected towards an antidyskinetic indication. However, these compounds display marked diversity in their actions at 5-HT1A receptors in vitro, with varying potencies and efficacies for activation of cellular signal transduction (Newman-Tancredi et al, 2005). The present data confirm that 5-HT1A receptor activation reduces the cataleptogenic potential of novel antipsychotic agents but show also that their profile of action is highly diverse and is likely to be related to their affinity/efficacy at both D2 and 5-HT1A receptors.
Antipsychotic Activity of the New Generation of Antipsychotics: Influence of 5-HT1A Receptor Agonist Properties
In accordance with previous studies, conventional (haloperidol, fluphenazine), atypical (olanzapine, clozapine, risperidone, and ziprasidone) as well as new generation potential antipsychotic agents (eg SSR181507, bifeprunox, SLV313) dose-dependently antagonized apomorphine-induced climbing in mice. Apomorphine-induced sniffing was also blocked in a dose-dependent manner over a similar dose range by all these drugs, with the exception of ziprasidone and sarizotan, which did not block sniffing at the highest dose tested, 40 mg/kg. Activity in this model is predictive of efficacy against the positive symptoms of psychosis (Protais et al, 1976) and demonstrates in vivo antagonist activity at dopamine D2 receptors of these compounds. A correlation analysis based on affinities at rat striatal D2 sites (Newman-Tancredi et al, 2005) shows that the ability of antipsychotics to inhibit apomorphine-induced climbing and sniffing correlated positively with their affinity at rat D2 receptors. Indeed, reflecting its potent blockade of D2 receptors in limbic/striatal structures, haloperidol was highly active in this model (ED50=0.09 mg/kg) whereas clozapine was active only at higher doses (ED50=8.7 mg/kg), which corresponds to its lower affinity at D2 receptors (Brunello et al, 1995). The activity of haloperidol and clozapine in this preclinical test is consistent with their clinical potency requiring low- and high-dose ranges, respectively, to control the positive symptoms of schizophrenia (Meltzer, 1995). Nemonapride potently blocked apomorphine-induced stereotyped behavior: this compound interacts with both D2 and 5-HT1A receptors but D2 receptor antagonism is seen at doses approximately 16–64 times lower than those having 5-HT1A agonist properties (Assié et al, 1997). In clinical studies, nemonapride was reported to have therapeutic efficacy in schizophrenia and to produce relatively mild EPS (Kudo et al, 1989). SLV313, SSR181507 and bifeprunox, compounds that have balanced affinity at D2 and 5-HT1A receptors, dose-dependently and potently reduced climbing and stereotyped behaviors produced by apomorphine. In contrast, ziprasidone and sarizotan have little effect at the highest doses tested in this model. It might have been the case that antagonist effects could have been observed at higher doses (or alternatively at other postinjection observation times). However, as mentioned in the Methods section, the use of doses above 40 mg/kg was precluded because of interfering side-effects that could be observed with some compounds at this ceiling dose. Ziprasidone has similar affinity at 5-HT1A and D2 receptors but also multiple interactions at numerous other receptor subtypes (Seeger et al, 1995; Newman-Tancredi et al, 2005) whereas sarizotan has high efficacy at 5-HT1A receptors and partial agonist properties at D2 receptors (Kuzhikandathil et al, 2004; Bartoszyk et al, 2004, Newman-Tancredi et al, 2005). The results with sarizotan are in agreement with earlier studies showing its weak antagonism of methylphenidate-induced behaviors in rats, another measure predictive of antipsychotic activity (Kleven et al, 2004). Taken together, these data indicate that 5-HT1A activation does not alter the antipsychotic-like effects of D2 antagonists in this model of positive symptoms of schizophrenia. Accordingly, for active avoidance behavior in mice, another animal model of antipsychotic potential, the coadministration of the 5-HT1A antagonist SL88.0338 did not modify the activity of SSR181507 (Depoortere et al, 2003). In addition, data obtained in rats suggest that the potency of D2 antagonists (such as raclopride) in the same test is even enhanced by addition of a compound with 5-HT1A agonist properties (such as 8-OH-DPAT: Prinssen et al, 1996).
In clinical studies, buspirone and tandospirone, two partial agonists at 5-HT1A receptors, substantially improved negative symptoms scores and reduced the incidence of EPS in schizophrenic patients treated with haloperidol (Sumiyoshi et al, 2001a, 2001b). In a single case study, Pantelis and Barnes (1993) have found that, when given together with neuroleptics, low doses of buspirone had beneficial effects on anxiety and psychosis whereas higher doses exacerbated psychosis. Thus, whereas preclinical studies generally find that 5-HT1A agonists attenuate neuroleptic-induced EPS (see Introduction), the therapeutic effects of combined 5-HT1A agonist/D2-like antagonist compounds remain largely uncharacterized and await further clinical studies. Indeed, sarizotan, which exhibits very high efficacy at 5-HT1A receptors and partial agonist properties at D2 receptors (Bartoszyk et al, 2004; Newman-Tancredi et al, 2005) is now in development as an antidyskinetic agent in L-DOPA-treated Parkinson's disease patients (Bartoszyk et al, 2004) likely because of insufficient antipsychotic activity (present data and Kleven et al, 2004). In contrast, interestingly, an older neuroleptic, tiospirone, with very low efficacy at 5-HT1A receptors (Newman-Tancredi et al, 1998, 2005), exhibited antipsychotic properties in humans comparable with those of haloperidol, but with a lower incidence of EPS (Moore et al, 1987).
Non-Catalepogenic Properties of the New Generation of Antipsychotics: Role of 5-HT1A Receptors
The atypical antipsychotics, clozapine, ziprazidone as well as the new generation of potential antipsychotic agents (eg SSR181507, aripiprazole, SLV313) induced little or no catalepsy compared with the typical antipsychotics, haloperidol, or fluphenazine in the bar test. ED50 values for SSR181507, sarizotan, aripiprazole, clozapine, and SLV313 were greater than 40 mg/kg, which is 100-fold higher than for haloperidol. However, we cannot exclude that pharmacokinetic peculiarities of some of these drugs (such as slow brain penetration or else: see below) may explain the fact that little or no catalepsy was observed under our experimental conditions (ie observation 1 h after drug administration). In fact, it has been reported that the maximum catalepsy response to aripiprazole occurred at 8 h post-administration (Hirose et al, 2004). This is an interesting observation, considering that in both rats and humans, a major metabolite of aripiprazole is a pure dopamine D2 antagonist (Lawler et al, 1999), which may mitigate the D2 receptor partial agonist properties of aripiprazole. Nevertheless, these results are generally consistent with previous literature for these ligands concerning their low cataleptogenic liability in rats (Glennon et al, 2002; Depoortere et al, 2003; Wolf, 2003; Bartoszyk et al, 2004; Kleven et al, 2005). Additionally, pretreatment with the 5-HT1A receptor antagonist, WAY100635, enhanced or reinstated catalepsy induced by antipsychotics, consistent with results reported by Kleven et al (2005). For example, WAY100635 pretreatment induced near maximal catalepsy in the bar test for SSR181507 and sarizotan, which alone, even at doses up to 40 mg/kg, induced no catalepsy. Depoortere et al (2003) have also reported that in coadministration with SL88.0338, another 5-HT1A antagonist, SSR181507 produced catalepsy in rats. Nemonapride induced catalepsy in a biphasic manner: that is, catalepsy at low but not at high doses, and pretreatment with WAY100635 reinstated nemonapride-induced catalepsy at higher doses. These findings extend previous data reported by Prinssen et al (1998), indicating that the 5-HT1A receptor agonist properties of nemonapride at high doses are responsible for its lowered propensity to produce catalepsy in rats. These observations demonstrate that activation of 5-HT1A receptors plays an important role in the relatively low or noncataleptogenic liability seen with compounds reported to have dual D2/5-HT1A actions (for review, see: Millan, 2000; Bantick et al, 2001). Another important finding of the present study was that pretreatment with WAY100635 enhanced catalepsy induced by the dopamine D2-like receptor antagonist haloperidol in mice. This confirms previous data reported by Prinssen et al (1998), showing that cotreatment with WAY100635 slightly, but significantly, enhanced haloperidol-induced catalepsy in rats. While having no effect on catalepsy itself, WAY100635 likely increases neuroleptic-induced catalepsy by blockade of 5-HT1A auto-receptors controlling tonic 5-HT release. Thus depletion of 5-HT by repeated treatment with the 5-HT synthesis inhibitor p-chlorophenylalanine methyl ester, abolished the enhancement by WAY100635 of catalepsy induced by raclopride (Prinssen et al, 2000). In addition, tonic 5-HT1A receptor activity has been demonstrated in animals during periods of active arousal (for review, see Routledge, 1996) and antipsychotic-induced catalepsy is very sensitive to 5-HT1A receptor stimulation (for review, see Wadenberg, 1996).
In the case of aripiprazole and SLV313, although WAY100635 produced upward shifts in their dose–response curves, the magnitude of catalepsy appeared to reach an asymptotic plateau, suggesting that other mechanisms may be involved in their low cataleptogenic liability. Indeed, although a partial agonist at 5-HT1A receptors, aripiprazole exhibits efficacy lower than that of other antipsychotics in assays of G-protein activation and adenylyl cyclase activity in cloned human and native rat hippocampal membranes (Newman-Tancredi et al, 2005). Moreover, as well as activating 5-HT1A receptors, aripiprazole is also a D2 receptor partial agonist (Bartoszyk et al, 2004) and has interactions at numerous other receptor subtypes (Shapiro et al, 2003) including 5-HT2A and 5-HT2C, targets that are known to profoundly influence antipsychotic drug action (Meltzer et al, 2003). In this context, it is likely that aripiprazole's partial D2 agonist properties or multi-receptor profile contribute to both its weak cataleptogenic profile and the limited catalepsy obtained in the presence of WAY100635. It has been recently suggested that aripiprazole is capable of directing D2 receptor signalling to specific intracellular responses (Urban et al, 2004) and it may be speculated that such signalling pathways are specifically involved in motor control, for example in brain regions such as striatum that display high densities of D2 receptor expression. In contrast, SLV313 exhibits balanced 5-HT1A/D2 affinity and intermediate efficacy at 5-HT1A receptors, but little interaction with D1, 5-HT2A or α1/2 adrenergic receptors (Newman-Tancredi et al, 2005; Assié MB, unpublished observations). SLV313 blocks psychostimulant-induced behaviors in rodents in the absence of catalepsy; of the compounds tested here SLV313 had the highest antipsychotic-like vs catalepsy separation (present data; Glennon et al, 2002; Kleven et al, 2005) suggesting that its balance of 5-HT1A/D2 properties produces a favorable antipsychotic profile. In contrast, SLV314, another ‘selectively nonselective’ 5-HT1A agonist/D2 antagonist (Roth et al, 2004), exhibits affinity at 5-HT1A receptors that is two orders of magnitude lower than that of D2 receptors and its cataleptogenic liability is higher than that of SLV313 (ED50=0.5 vs >40 mg/kg). In addition to exerting classical antipsychotic-like effects, SLV314 has also been reported to induce antidepressant and anxiolytic-like effects (McCreary et al, 2002) probably due to its potent serotonin reuptake inhibition properties rather than to its direct 5-HT1A activation (Tuinstra et al, 2002). Taken together, these data suggest that the lack of catalepsy of these novel antipsychotics (eg SSR181507, aripiprazole, SLV313) depend on both the affinity and efficacy of these ligands at 5-HT1A and D2 receptors.
Conclusions
A new generation of potential antipsychotics is being developed, including bifeprunox, SSR181507 and SLV313, which selectively targets 5-HT1A receptors as well as dopamine D2 receptors. The present data confirm that antipsychotics that activate 5-HT1A receptors exhibit low EPS liability and support the concept that combined D2 receptor blockade and 5-HT1A activation is a promising strategy to reduce the EPS liability of antipsychotics, while retaining desired antipsychotic properties (Bantick et al, 2001; Millan 2000). Nevertheless, the present data indicate also that the balance of affinity and efficacy at both D2 and 5-HT1A receptors profoundly influences the pharmacological profile of these new generation antipsychotics, and will likely impact their therapeutic profiles.
References
Assié MB, Cosi C, Koek W (1997). 5-HT1A receptor agonist properties of the antipsychotic nemonapride: comparison with bromerguride and clozapine. Eur J Pharmacol 334: 141–147.
Bantick RA, Deakin JFW, Grasby PM (2001). The 5-HT1A receptor in schizophrenia: a promising target for novel atypical neuroleptics ? J Psychopharmacol. 15: 37–46.
Bantick RA, Montgomery AJ, Malek N, Choudry T, Messa C, Deakin JFW et al (2000). Occupancy/downregulation of the 5-HT1A receptor by clozapine measured using PET scanning. J Psychopharmacol 14: PG20.
Bartoszyk GD, Van Amsterdam C, Greiner HE, Rautenberg W, Russ H, Seyfried CA (2004). Sarizotan, a serotonin 5-HT1A receptor agonist and dopamine receptor ligand. 1. Neurochemical profile. J Neural Transm 111: 113–126.
Blier P, Ward NM (2003). Is there a role for 5-HT1A agonists in the treatment of depression? Biol Psychiatry 53: 193–203.
Brunello N, Masotto C, Steardo L, Markstein R, Racagni G (1995). New insights into the biology of schizophrenia through the mechanism of action of clozapine. Neuropsychopharmacology 13: 177–213.
Buchanan RW, Kreyenbuhl J, Zito JM, Lehman A (2002). Relationship of the use of adjunctive pharmacological agents to symptoms and level of function in schizophrenia. Am J Psychiatry 159: 1035–1043.
Chou YH, Halldin C, Farde L (2003). Occupancy of 5-HT1A receptors by clozapine in the primate brain: a PET study. Psychopharmacology 166: 234–240.
Christoffersen CL, Meltzer LT (1998). Reversal of haloperidol-induced extrapyramidal side effects in cebus monkeys by 8-hydroxy-2-(di-n-propylamino) tetralin and its enantiomers. Neuropsychopharmacology 18: 399–402.
Claustre Y, Peretti DD, Brun P, Gueudet C, Allouard N, Alonso R et al (2003). SSR181507, a dopamine D2 receptor antagonist and 5-HT1A receptor agonist. I: Neurochemical and electrophysiological profile. Neuropsychopharmacology 28: 2064–2076.
Cussac D, Duqueyroix D, Newman-Tancredi A, Millan MJ (2002). Stimulation by antipsychotic agents of mitogen-activated protein kinase (MAPK) coupled to cloned, human (h) serotonin 5-HT1A receptors. Psychopharmacology 162: 168–177.
Daniel DG, Zimbroff DL, Potkin SG, Reeves KR, Harrigan EP, Lakshminarayanan M (1999). Ziprasidone 80 mg/day and 160 mg/day in the acute exacerbation of schizophrenia and schizoaffective disorder: a 6-week placebo-controlled trial. Ziprasidone Study Group. Neuropsychopharmacology 20: 491–505.
Depoortere R, Boulay D, Perrault G, Bergis O, Decobert M, Francon D et al (2003). SSR181507, a dopamine D2 receptor antagonist and 5-HT1A receptor agonist. II: Behavioral profile predictive of an atypical antipsychotic activity. Neuropsychopharmacology 28: 1889–1902.
Forster EA, Cliffe IA, Bill DJ, Dover GM, Jones D, Reilly Y et al (1995). A pharmacological profile of the selective silent 5-HT1A receptor antagonist, WAY-100635. Eur J Pharmacol 281: 81–88.
Fray PJ, Sahakian BJ, Robbins TW, Koob GF, Iversen SD (1980). An observational method for quantifying the behavioural effects of dopamine agonists: contrasting effects of d-amphetamine and apomorphine. Psychopharmacology 69: 253–259.
Glennon J, McCreary AC, Ronken E, Siarey R, Hesselink MB, Feenstra R et al (2002). SLV313 is a dopamine D2 receptor antagonist and serotonin 5-HT1A receptor agonist: In vitro and in vivo neuropharmacology. Eur Neuropsychopharmacol 12: S277.
Hirose T, Uwahodo Y, Yamada S, Miwa T, Kikuchi T, Kitagawa H et al (2004). Mechanism of action of aripiprazole predicts clinical efficacy and a favourable side-effect profile. J Psychopharmacol 18: 375–383.
Honey GD, Bullmore ET, Soni W, Varatheesan M, Williams SCR, Sharma T (1999). Differences in frontal cortical activation by a working memory task after substitution of risperidone for typical antipsychotic drugs in patients with schizophrenia. Proc Nat Acad Sci USA 96: 13432–13437.
Hubert JJ (1984). Bioassay. Kendall/Hunt: Dubuque, IA.
Ichikawa J, Meltzer HY (2000). The effect of serotonin1A receptor agonism on antipsychotic drug-induced dopamine release in rat striatum and nucleus accumbens. Brain Res 858: 252–263.
Kleven M, Prinssen EPM, Koek W (1996). Role of 5-HT1A receptors in the ability of mixed 5-HT1A receptor agonist/dopamine D2 receptor antagonists to inhibit methylphenidate-induced behaviors in rats. Eur J Pharmacol 313: 25–34.
Kleven MS, Barret-Grévoz C, Bruins-Slot L, Newman-Tancredi A (2005). Novel antipsychotics agents with 5-HT1A agonist properties: role of 5-HT1A receptor activation in attenuation of catalepsy induction in rats. Neuropharmacology 49: 135–143.
Kleven MS, Barret-Grévoz C, Newman-Tancredi A (2004). In vivo pharmacology of novel antipsychotics with diverse dopamine D2 and serotonin 5-HT1A properties: evidence for lowered EPS liability. Coll Inter NeuroPsychopharmacol Abs 02: 503.
Koek W, Vacher B, Cosi C, Assié MB, Patoiseau JF, Pauwels PJ et al (2001). 5-HT1A receptor activation and antidepressant-like effects: F13714 has high efficacy and marked antidepressant potential. Eur J Pharmacol 420: 103–112.
Kudo Y, Ikawa G, Kawakita Y, Saito M, Sakai T, Nakajima T et al (1989). A double-blind comparative study of a new benzamide compound YM-09151 with sulpiride in schizophrenia. J Clin Ther Med 5: 2149–2175.
Kuzhikandathil EV, Sayed N, Pasuit JB, Bartoszyk GD (2004). Differential effects of sarizotan on dopamine receptor function. Soc Neurosci Abs 163: 6.
Lawler CP, Prioleau C, Lewis MM, Mak C, Jiang D, Schetz JA et al (1999). Interactions of the novel antipsychotic aripiprazole (OPC-14597) with dopamine and serotonin receptor subtypes. Neuropsychopharmacology 20: 612–627.
Litchfield JT, Wilcoxon F (1949). A simplified method of evaluating dose-effect experiments. J Pharmacol Exp Ther 96: 99–113.
McCreary AC, Glennon J, Tuinstra T, Herremans AHJ, Van der Heyden JAM, Feenstra R et al (2002). SLV313: A novel antipsychotic with additional antidepressant and anxiolytic-like actions. Eur Neuropsychopharmacology 12: S274.
Meltzer HY (1995). Atypical antipsychotic drugs. In: Bloom FE, Kupfer DJ (eds). Psychopharmacology: The Fourth Generation of Progress. Raven Press Ltd: New York. pp 1277–1288.
Meltzer HY, Li Z, Kaneda Y, Ichikawa J (2003). Serotonin receptors: their key role in drugs to treat schizophrenia. Prog Neuro-psychopharmacol Biol Psychiatr 27: 1159–1172.
Millan MJ (2000). Improving the treatment of schizophrenia: Focus on serotonin 5- HT1A receptors. J Pharmacol Exp Ther 295: 853–861.
Millan MJ, Schreiber R, Dekeyne A, Rivet JM, Bervoets K, Mavridis M et al (1998). S 16924 ((R)-2-[1-[2-(2,3-dihydro-benzo[1,4] dioxin-5-yloxy)-ethyl]-pyrrolidin-3yl]-1-(4-fluoro-phenyl)-ethanone), a novel, potential antipsychotic with marked serotonin (5-HT)1A agonist properties: II. Functional profile in comparison to clozapine and haloperidol. J Pharmacol Exp Ther 286: 1356–1373.
Moore NC, Meyendorff E, Yeragani V, LeWitt PA, Gershon S (1987). Tiaspirone in schizophrenia. J Clinical Psychopharmacology 7: 98–101.
Newman-Tancredi A, Assié MB, Leduc N, Ormière AM, Danty N, Cosi C (2005). Novel antipsychotics activate recombinant human and native rat serotonin 5-HT1A receptors: affinity, efficacy and potential implications for treatment of schizophrenia. Int J Neuropsychopharmacol 8: 1–16.
Newman-Tancredi A, Gavaudan S, Conte C, Chaput C, Touzard M, Verrièle L et al (1998). Agonist and antagonist actions of antipsychotic agents at serotonin 5-HT1A receptors: a [35S]GTPγS binding study. Eur J Pharmacol 355: 245–256.
Pantelis C, Barnes TRE (1993). Acute exacerbation of psychosis with buspirone ? J Psychopharmacol 7: 295–300.
Prinssen EP, Colpaert FC, Koek W (2002). 5-HT1A receptor activation and anti-cataleptic effects: high-efficacy agonists maximally inhibit haloperidol-induced catalepsy. Eur J Pharmacol 453: 217–221.
Prinssen EPM, Kleven MS, Koek W (1996). Effects of dopamine antagonists in a two-way active avoidance procedure in rats: interactions with 8-OH-DPAT, ritanserin, and prazosin. Psychopharmacology 128: 191–197.
Prinssen EPM, Kleven MS, Koek W (1998). The cataleptogenic effects of the neuroleptic nemonapride are attenuated by its 5-HT1A receptor agonist properties. Eur J Pharmacol 356: 189–192.
Prinssen EPM, Kleven MS, Koek W (1999). Interactions between neuroleptics and 5-HT1A ligands in preclinical behavioral models for antipsychotic and extrapyramidal effects. Psychopharmacology 144: 20–29.
Prinssen EPM, Koek W, Kleven MS (2000). Effects of WAY 100635 on antipsychotic-induced catalepsy in 5-HT depleted animals: a role for tonic activation of 5-HT1A receptors. Eur J Pharmacol 395: 143–147.
Protais P, Costentin J, Schwartz JC (1976). Climbing behaviour induced by apomorphine in mice: a simple test for the study of dopamine receptors in striatum. Psychopharmacology 50: 1–6.
Rollema H, Lu Y, Schmidt AW, Zorn SH (1997). Clozapine increases dopamine release in prefrontal cortex by 5-HT1A receptor activation. Eur J Pharmacol 338: 3–5.
Roth BL, Sheffler DJ, Kroeze WK (2004). Magic shotguns versus magic bullets: selectively non-selective drugs for mood disorders and schizophrenia. Nat Rev Drug Discovery 3: 353–359.
Routledge C (1996). Development of 5-HT1A receptor antagonists. Behav Brain Res 73: 153–156.
Seeger TF, Seymour PA, Schmidt AW, Zorn SH, Schulz DW, Lebel LA et al (1995). Ziprasidone (CP-88,059): A new antipsychotic with combined dopamine and serotonin receptor antagonist activity. J Pharmacol Exp Ther 275: 101–113.
Shapiro DA, Renock S, Arrington E, Chiodo LA, Liu LX, Sibley DR et al (2003). Aripiprazole, a novel atypical antipsychotic drug with a unique and robust pharmacology. Neuropsychopharmacology 28: 1400–1411.
Sumiyoshi T, Matsui M, Nohara S, Yamashita I, Kurachi M, Sumiyoshi C et al (2001a). Enhancement of cognitive performance in schizophrenia by addition of tandospirone to neuroleptic treatment. Am Journal of Psychiatry 158: 1722–1725.
Sumiyoshi T, Matsui M, Yamashita I, Nohara S, Kurachi M, Uehara T et al (2001b). The effect of tandospirone, a serotonin1A agonist, on memory function in schizophrenia. Biol Psychiatry 49: 861–868.
Tallarida RJ, Murray RG (1987). Manual of Pharmacological Calculations with Computer Programs. Springer Verlag: New York.
Tuinstra T, Herremans AHJ, McCreary AC, Van der Heyden JAM, Long SK, Van Hess R et al (2002). SLV314: Behavioral profile of a molecule combining dopamine D2 receptor antagonism with serotonin reuptake inhibition. Soc Neurosci Abs 894: 19.
Urban JD, Gay EA, Mailman RB (2004). Functional selectivity as a mechanism of action of newer atypical antipsychotic drugs. Soc Neurosci Abs 163: 4.
Waddington JL (1986). Psychopharmacological studies in rodents: stereotaxic intracerebral injections and behavioral assessment. In: Joseph MH, Waddington JL (eds). Working Methods in Neuropsychopharmacology. Manchester University Press: Manchester. pp 1.
Wadenberg ML (1996). Serotonergic mechanisms in neuroleptic-induced catalepsy in the rat. Neurosci Biobehav Rev 20: 325–339.
Wolf W (2003). DU127090. Current Opin Invest Drugs 4: 72–76.
Yoshida K, Sugita T, Higuchi H, Hishikawa Y (1998). Effect of tandospirone on tardive dyskinesia and parkinsonian symptoms. Eur Psychiatry 13: 421–422.
Acknowledgements
The present study was funded by Pierre Fabre Médicament. All authors are employees of the Pierre Fabre Research Centre. The authors thanks, N Consul-Denjean, E Senaux and L Hejoaka for technical expertise and J Besnard for assistance with data management and analysis. We thank Solvay-Duphar, for the kind donation of SLV313 and SLV314.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bardin, L., Kleven, M., Barret-Grévoz, C. et al. Antipsychotic-Like vs Cataleptogenic Actions in Mice of Novel Antipsychotics Having D2 Antagonist and 5-HT1A Agonist Properties. Neuropsychopharmacol 31, 1869–1879 (2006). https://doi.org/10.1038/sj.npp.1300940
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1300940
Keywords
This article is cited by
-
Structure-based design of a novel third-generation antipsychotic drug lead with potential antidepressant properties
Nature Neuroscience (2022)
-
Quinoline analogs of 2-aminoindane as potential central dopaminergic agents
Medicinal Chemistry Research (2019)
-
Effects of Derivatives of 3-Hydroxypyridine and Succinic Acid on Stereotypical Behavior and Catalepsy in Mice
Neuroscience and Behavioral Physiology (2018)
-
Comparative pharmacology of antipsychotics possessing combined dopamine D2 and serotonin 5-HT1A receptor properties
Psychopharmacology (2011)
-
Pharmacological blockade of dopamine D2 receptors by aripiprazole is not associated with striatal sensitization
Naunyn-Schmiedeberg's Archives of Pharmacology (2011)