Abstract
Several lines of evidence indicate that inhibition of the metabotropic glutamate (mGlu) receptor 5 produces anxiolytic-like effects in rodents. Peptide neurotransmitter neuropeptide Y (NPY) produces an anxiolytic effect in rats after intraventricular or intra-amygdalar administration. Many classes of anxiolytic drugs exert their effect through the GABA–benzodiazepine (BZD) receptor complex. Therefore, in the present study we have investigated whether the anxiolytic action of MPEP (2-methyl-6-(phenylethynyl)pyridyne), an mGlu5 receptor antagonist, is mediated by a mechanism involving either the GABA–BZD receptor complex or NPY receptor. In the behavioral studies, the anxiolytic activity of MPEP (10 mg/kg, i.p.) was examined using plus-maze test. The BZD antagonist flumazenil (10 mg/kg, i.p.) was given to one group of rats and Y1 receptor antagonist BIBO 3304 (((R)-N-[[4-(aminocarbonylaminomethyl) phenyl] methyl]-N2-(diphenylacetyl)-argininamide trifluoroacetate)3304) (200 pmol/site, intra-amygdala) to the other. It was found that anxiolytic effects of MPEP were not changed by flumazenil, but were abolished by BIBO 3304. Immunohistochemical studies showed a high density of mGlu5 receptor immunoreactivity (IR) in the amygdala. The effect of MPEP on NPY expression in the amygdala was studied using immunohistochemistry (IH) and radioimmunoassay (RIA). Both methods showed a diminution of NPY IR expression, to about 43% (IH) or 81% (RIA) of the control level after multiple administrations, but we observed an increase up to 148% of the control after single MPEP administration. These effects may suggest a release of NPY from nerve terminals after MPEP administration. Our results indicate that the anxiolytic action of MPEP is conveyed through NPY neurons with the involvement of Y1 receptors in the amygdala and that BZD receptors do not significantly contribute to these effects.
Similar content being viewed by others
INTRODUCTION
Glutamatergic neurotransmission in the central nervous system is mediated by two distinct groups of receptors: ligand-gated ion channels and G-protein-coupled glutamate receptors (Conn and Pin, 1997; Scatton, 1993). It has recently been proposed that glutamatergic system plays an important role in the pathophysiology of anxiety (Chojnacka-Wojcik et al, 2001; Wroblewski and Danysz, 1989). Different functional N-methyl-D-aspartate (NMDA) receptor antagonists exhibit anxiolytic-like activity in animal models (Bennett and Amrick, 1986; Corbett and Dunn, 1993; Plaznik et al, 1994; Przegalinski et al, 1996; Trullas et al, 1989; Winslow et al, 1990). The potential clinical use of NMDA receptor antagonists has been limited due to their undesirable side effects, such as muscle relaxation, ataxia, amnesia, and psychotomimetic effects (Scatton, 1993). The discovery of metabotropic glutamate (mGlu) receptors and identification of selective ligands triggered an intense search for potentially novel and safer pharmacotherapies for the treatment of nervous system disorders. Previous studies showed that diminution of glutamatergic transmission by the antagonists of group I and agonists of groups II and III mGlu receptors had anxiolytic activity (Chojnacka-Wojcik et al, 1997; Helton et al, 1998; Monn et al, 1997; Pilc et al, 2000; Spooren et al, 2000; Tatarczynska et al, 2001b). Additional studies confirmed the anxiolytic effect of the mGluR5 antagonist 2-methyl-6-(phenylethynyl)pyridyne (MPEP) (Brodkin et al, 2002; Klodzinska et al, 1999; Tatarczynska et al, 2001a, 2001b).
The amygdala is a key structure to the regulation of the anxiety and expression of emotional responses to stress (Davis, 1992; Davis et al, 1994). Attention has been focused particularly on the basolateral complex (lateral, basolateral, and basomedial nuclei) and central nucleus of the amygdala (Davis, 1992; Davis et al, 1994). These regions contain many peptidergic neurons. Among different amygdala peptides, neuropeptide Y (NPY) has been shown to play a crucial role in modulating anxiety in animal models, as demonstrated by central administration of the peptide showing anxiolytic effects (Heilig et al, 1989; Kask et al, 2000). The anxiety-related actions of NPY are mediated mainly through three classes of receptors known as the Y1, Y2, and Y5 receptor subtypes (Kask et al, 2000). Two of them are present in the amygdala in high densities, that is, Y1 and Y2 receptors (Dumont et al, 2000; Kask et al, 2000). It was shown that Y1 receptors mediate an anxiolytic-like behavior (Sajdyk et al, 1999), while Y2 receptors are presynaptically located (Colmers and Bleakman, 1994) and play a role in mediating an anxiogenic effect (Redrobe et al, 2003). The amygdala was shown to express a large number of mGlu1 and mGlu5 receptors (Martin et al, 1992; Shigemoto et al, 1993; Smialowska et al, 2002b). A colocalization of group I mGluRs and NPY in the amygdala was also reported. In addition, an interaction between glutamate and NPY (Smialowska et al, 2002b) was evidenced by showing a decrease in NPY immunoreactivity (IR) in the amygdala after the blockade of glutamatergic neurons (Wieronska et al, 2001a). This may suggest that NPY effects are regulated by glutamate in that structure.
In the present work, we decided to find out in the amygdala whether the anxiolytic action of MPEP, a potent, selective, and brain-penetrable mGlu5 receptor antagonist (Gasparini et al, 1999, 2002; Micheli, 2000), is mediated via either a well-known pathway involving GABAergic system and benzodiazepine (BZD) receptors or an interaction with NPY receptor signaling. To solve this problem, we used flumazenil, a BZD receptor antagonist, which abolishes anxiolytic action of diazepam or chlordiazepoxide in animal model used for testing anxiolytic action of drugs (eg plus-maze test) (Pellow and File, 1985), and BIBO 3304 (((R)-N-[[4-(aminocarbonylaminomethyl) phenyl] methyl]-N2-(diphenylacetyl)-argininamide trifluoroacetate)3304), an NPY Y1 receptor blocker, which antagonizes the anxiolytic action of NPY (Sajdyk et al, 1999). The distribution of mGlu5 receptors in the amygdala and the influence of MPEP on NPY IR were also tested.
MATERIALS AND METHODS
Rats
Male Wistar rats weighing 200–230 g were used. The animals were obtained from a local breeding farm. The rats were age-matched, fed ad libitum, and housed six to a cage under a 12 : 12 light–dark cycle. The rats after cannulae implantation were housed singly. During the experiment, all efforts were made to minimize animal suffering and to reduce the number of animals used, in accordance to the National Institutes of Health Guide for the Care and Use of Laboratory Animals and the local ethical Committee. All experiments were performed on the separate groups of rats and in behavioral studies, each animal was used only once in the test.
Drugs
MPEP, an mGlu5 receptor antagonist, was synthesized at Novartis (Basel, Switzerland), BIBO 3304, a Y1 receptor antagonists, was obtained from Dr Mueller, Boehringer-Ingelheim (Biberach, Germany), flumazenil was purchased from Hoffmann-La Roche (Ro 15-1788 Ltd, Basel, Switzerland), and diazepam was obtained from Polfa SA (Cracow, Poland). MPEP was dissolved in 0.9% NaCl, flumazenil and diazepam was suspended in 1% Tween 80, and BIBO 3304 was dissolved in distilled water.
Plus-Maze Procedure
Plus-maze test was performed according to the method described by Pellow et al (1986). Briefly, the plus-maze apparatus was made of wood and consisted of two open arms, 50 × 10 cm and two closed arms 50 × 10 × 40 cm. It was painted in black, but the wooden walls of the closed arms had their natural color, with an open roof. The apparatus was elevated 50 cm above the floor. Two open arms were opposite to each other and were illuminated by a 40 W bulb positioned 20 cm above each open arm.
Each rat was placed individually in a new cage, which was similar to the home cage for 5 min immediately before the test (this procedure resulted in an increase in the total number of arm entries during the test). Each rat was then placed in the center of plus-maze facing one of the open arms. During the 5-min test, the number of entries into open arms and the time spent in the open arms was measured. The maze was cleaned with a paper towel after each trial. Experiments were performed between 09:00 and 12:00.
The drugs were given in the following schedule: in the experiment with flumazenil and MPEP, MPEP (10 mg/kg, i.p.) was injected 60 min before the test and flumazenil (10 mg/kg, i.p.) 30 min after MPEP administration. The plus-maze test was performed 30 min after flumazenil administration, according to Schmidt-Mutter et al (1998). Diazepam (5 mg/kg, i.p.) was injected 2 min prior to flumazenil and 30 min after flumazenil administration, the plus-maze test was performed. The control group received saline i.p.
In the second experiment, BIBO 3304 was administered intra-amygdala, bilaterally in a dose of 200 pmol/0.5 μl/site, 10 min before MPEP i.p. administration according to Sajdyk et al (1999). Then MPEP was injected and 30 min after MPEP administration, the test was carried out. The control group received saline i.p. and destilled H2O intra-amygdala. Rats that received only MPEP were injected intra-amygdala with destilled H2O, and rats that were injected only with BIBO 3304 were injected with saline i.p.
Cannulae Implantation and Histology
The rats, anesthetized with Equitesin, were immobilized in a Kopf stereotaxic instrument. The skin was cut and the skull was cleaned for bilateral implantation of guide cannulae made of 23-gauge stainless-steel tubing, 2 mm above the sites of injection. The guide tubes, secured by the dental cement, were anchored to three stainless-steel screws fixed to the skull. In order to prevent clogging, 30-gauge stainless-steel stylets were placed in the guide cannulae and remained there until the animals were given intracerebral injections 5 days later. The rats were adapted to handling and on the test day, the stylets were withdrawn and replaced by bilateral injection units (30-gauge stainless-steel tubing) terminating 2 mm below the tip of the guides.
The coordinates for injection sites were A −2.56; L ±5; H −8.6, measured from bregma according to Paxinos and Watson (1986) stereotaxic atlas with the aim of administering injections to the basolateral nucleus of the amygdala.
On completion of each experiment, the rats were killed and their brains were removed, fixed in formaline for 24 h, and quickly frozen on dry ice. To check the position of the cannulae tracks, the frozen brains were cut in the coronal plane in a Cryo-cut. Representative drawings of the histological sections, showing the injection sites are shown in Figure 1.
Schematic drawings of coronal sections of the rat brain showing the localization of the cannulae tips in rats injected into the basolateral amygdala. Only data from animals in which the histologically reconstructed sites of microinjections were localized in the indicated area were included in the results of each experiment.
mGlu5 IR
The animals under deep Vetbutal anesthesia were perfused through the ascending aorta with 50 ml of 0.9% NaCl, followed by cold, phosphate-buffered 4% paraformaldehyde as described previously (Smialowska, 1995; Smialowska and Legutko, 1992). The brains were dissected out, postfixed for 3 h, and immersed for a few days in a 5% sucrose solution in phosphate-buffered saline (PBS) at 4°C. The brains were then cut into 30 μm frontal sections, on a freezing microtome, at levels containing the amygdala (coordinates in relation to bregma: −1.8 to −3.8 according to the Paxinos and Watson stereotaxic atlas). Free-floating sections were incubated for 48 h at 4°C in an anti-mGluR5 antiserum (Novartis, Basel, Switzerland) diluted at 1 : 2500. The affinity-purified polyclonal antiserum against mGluR5 was raised in rabbit against a peptide corresponding to the C-terminal amino-acid sequence of rat mGluR5 (PSSPKYDTLIIRDYTQSSSSL) conjugated to ovalbumin (Vidnyászky et al, 1994). After incubation with the mGluR5 antibody, the sections were rinsed in PBS and processed by the avidine–biotine peroxidase complex method using an ABC-peroxidase kit (Vector Lab, Burlingame, USA). The specificity of immunostaining was controlled by omitting the primary antiserum. No mGluR5 IR was detected in these sections.
NPY IR
Immunohistochemistry (IH)—multiple administration
To study the effects of MPEP on NPY IR, rats were divided into two groups, seven rats each. One group received MPEP, which was given at a dose of 10 mg/kg, i.p, three times; the interval between injections was 8 h. The other group received saline, given according to the same schedule as MPEP. The doses and time schedule were chosen on the basis of our previous work (Wieronska et al, 2001a) and other studies (Midgley et al, 1994).
At 30 min after the last injection, the animals under deep Vetbutal anesthesia were perfused through the ascending aorta. The perfusion and procedure of immunostaining were similar to that described earlier (Smialowska et al, 1999). Free-floating sections were incubated for 48 h at 4°C in a rabbit anti-NPY antiserum (Amersham AB, Buckinghamshire, England) diluted at 1 : 2000; then rinsed in PBS and processed by the avidine–biotine peroxidase complex method using an ABC-peroxidase kit (Vector Lab). The specificity of immunostaining was controlled by incubating the tissue section with antiserum preadsorbed with respective synthetic peptides or by omitting the primary antiserum. No NPY IR was detected in these sections.
The intensity of immunostaining and the number of immunoreactive neurons were examined in amygdala sections under a light microscope. Immunoreactive nerve cell bodies were counted on at least five to ten sections, at the following levels: −2.3; −2.8; −3.3; −3.6; −3.8 with respect to bregma, according to the atlas of Paxinos and Watson (1986) (usually two amygdala sections at each level). Then, the mean number of IR neurons per section of amygdala was calculated for each rat.
NPY radioimmunoassay (RIA)—multiple administration
The experimental groups were identical as for the immunochemical method, except that the animals were not perfused but decapitated and the amygdalae were dissected. The assay buffer (pH=7.4) consisted of 19 mM NaH2PO4, 81 mM Na2HPO4, 10 mM Na2 EDTA, 0.1% Triton X-100, 0.01% NaN3, and 0.5% bovine serum albumin. Synthetic porcine NPY (Peninsula Lab. Buckinghamshire, England) was used as a standard in serial dilution ranging between 60 and 1000 pg per tube. The rabbit antiporcine NPY antiserum (RAS 7172, Peninsula Lab.) showed 100% cross-reaction with NPY (human, porcine, rat), NPY 13–36 (porcine), and peptide YY (porcine), and 1.6% with pancreatic polypeptide (human), but it did not show cross-reactivity with VIP (human, porcine, rat), amylin, insulin (human), and somatostatin. 125I-radiolabelled NPY (IM 170, Amersham) was used as a tracer. Assays were carried out in duplicate in polypropylene tubes. Each tube contained a 100 μl aliquot of a diluted sample or the standard and 100 μl of diluted NPY antiserum. After a 48 h preincubation (4°C), 100 μl of 125I-NPY (15 000 cpm/100 μl) was added to each tube, and the tubes were incubated for 24 h (4°C). Free and antibody-bound NPY were separated by adding 500 μl of the charcoal suspension containing 0.8% untreated charcoal powder and 0.08% dextran 70 000. After vortexing for 1 min, the suspension was centrifuged (1500 g, 20 min, 4°C). The supernatant radioactivity was counted in an LKBγ counter. The assay detection limit was 14 pg per tube. The intra- and interassay coefficients of variation were 5 and 11%, respectively. Controls and experimental samples were run in the same assay.
IH—single administration
To compare the behavioral results with NPY IR, we performed one more experiment, in which we studied the changes in NPY IR after the single MPEP administration. The rats were divided into four groups: one control group, which received saline (N=6), and three groups, which received MPEP at a 10 mg/kg (N=5) dose. The first MPEP-treated group was perfused 0.5 h after the injection, the second 6 h, and the third 24 h after the MPEP injection. Then the brains were treated similarly as was described in the Introduction, but we used the anti-NPY antibody from Sigma.
Statistics
The data from the behavioral experiments were analyzed by one-way ANOVA followed by post hoc Neuman–Keuls comparison. Data from immunohistochemical test and RIA were evaluated by the Student's t-test.
RESULTS
Behavioral Studies
Effect of MPEP, diazepam, and flumazenil in the plus-maze test
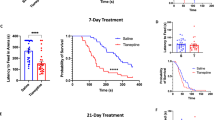
The results from the plus-maze experiment are presented as a percent of the open arm entries and the percent of time spent in the open arms of the maze by an individual animal. MPEP administered at a dose of 10 mg/kg induced an anxiolytic-like effect, significantly increasing the percentage of the time spent in the open arms (from 8.8 up to 48.3%) and the percentage of the entries into the open arms (from 29.4 up to 51.7%). The anxiolytic-like effect of MPEP was not changed by flumazenil administered at a dose of 10 mg/kg (Figure 2a).
(a) Effect of flumazenil (10 mg/kg, i.p.) on the anxiolytic-like activity of MPEP (10 mg/kg, i.p.) in the plus-maze test in rats. MPEP was injected 60 min and flumazenil 30 min before the test. N=6–7 rats per group. F=(2,15)=27.877 (time spent in the open arms) and F(2.15)=9.643 (open arms entries), p<0.001 vs vehicle. (b) Effect of flumazenil (10 mg/kg, i.p.) on the anxiolytic-like activity of diazepam (5 mg/kg) in the plus-maze test in rats. Diazepam was injected 2 min prior to flumazenil and flumazenil 30 min before the test. N=6–7 rats per group. F(2.16)=18.691, p<0.001 vs vehicle (time spent in the open arms) and F(2.16)=9.833, p<01 (open arm entries), A p<0.01 vs diazepam.
Diazepam given at a dose of 5 mg/kg significantly increased the percentage of the time spent in the open arms (from 10.9 up to 70%), as well as the percentage of entries into the open arms (from 38.5 up to 76%). Diazepam at a dose of 5 mg/kg significantly reduced the total number of entries (data not shown). The anxiolytic-like effect of diazepam was abolished by flumazenil given at a dose of 10 mg/kg. Flumazenil given alone had no effect on either the time spent in or the entries into the arms of the plus-maze (Figure 2b).
Effect of MPEP and BIBO 3304 in the plus-maze test
The typical anxiolytic activity of MPEP (10 mg/kg) in the plus-maze procedure, which was evidenced by an increase in time spent in open arms of the maze (up to 45%) as well as more open arms entries (up to 65%) compared to control rats (22.16 and 42%, respectively), was completely abolished by BIBO 3304 (13.4% (time) and 27% (entries)), which given alone had no effect on the behavior of control animals, when given 10 min prior to MPEP administration (Figure 3).
Effect of BIBO 3304 (200 pmol/0.5 μl/site) on the anxiolytic-like activity of MPEP (10 mg/kg, i.p.) in the plus-maze test in rats. MPEP was injected 30 min before the test and BIBO 10 min before the MPEP test. N=6 rats per group. F(4,747)=3.43, p<0.01 (time spent in the open arms) and F(7.045)=3.41, p<0.001 (open arm entries).
IR of mGlu5 and NPY
mGlu5 receptors were seen in the neuropil only, and not in cell bodies. The most intense staining of mGlu5 receptors IR was observed in the lateral, basolateral, central, and cortical nuclei of the amygdala (Figure 4).
Photomicrograph showing mGluR5 IR in the rat brain amygdala. Single immunohistochemical staining with DAB as chromogen. The mGluR5 IR is seen in the neuropil only, and not in cell bodies. Coronal section: BLA-basolateral amygdaloid nucleus, anterior; BLV-basolateral amygdaloid nucleus, ventral; Ce-central amygdaloid nucleus; MeAD-medial amygdaloid nuclei, anterodorsal; MeAV-medial amygdaloid nuclei, anteroventral; BMA-basomedial amygdaloid nuclei; Aco-anterior cortical amygdaloid nuclei. Scale bar=500 μm.
In control rats, a few NPY-IR neurons and terminal fibers were scattered over the whole amygdala region. Subacute treatment with noncompetitive mGlu5 antagonist MPEP induced a decrease in NPY-IR expression. The mean number of NPY-IR neurons per amygdala section decreased significantly from 10.01±1.01 in the control group to 4.3±0.5 in the MPEP-treated rats, which amounts to 42.9% of the control level (Figure 5a and 7). Acute treatment with MPEP did not cause significant changes in NPY IR after 30 min or 24 h, but we observed an increase in NPY IR after 6 h up to 148.65% of control (Figure 6).
(a) Effect of MPEP (10 mg/kg, 3 ×, every 8 h) on NPY IR in the rat brain amygdala. Each column represents the mean number of immunoreactive (IR) nerve cell bodies per amygdala section. The statistical significance was calculated by Student's t-test. N=7, p<0.001 relative to control. (b) Effect of MPEP (10 mg/kg, 3 ×, every 8 h) on NPY IR in the rat brain amygdala. The statistical significance was calculated by Student's t-test. N=7, p<0.001 relative to control.
Photomicrographs showing NPY IR in the rat basolateral amygdaloid nucleus. (a) Control rat; (b) 0.5 h after triple administration of MPEP. NPY-IR nerve cell bodies (empty arrows), processes (triangles), and terminal fibers (arrows) are seen. The number of nerve cell bodies is decreased after multiple MPEP treatment. Scale bar=50 μm.
Effect of MPEP (10 mg/kg) on NPY IR in the rat brain amygdala. Each column represents the mean number of immunoreactive (IR) nerve cell bodies per amygdala section. The rats were killed 0.5 h, 6 h, and 24 h after MPEP administration. The statistical significance was calculated by Student's t-test. N=5–6, p<0.001 relative to control.
Also, in RIA studies we observed a decrease in NPY-like IR in rats that received multiple MPEP administration compared to control animals. The decrease was 81% of control values (Figure 5b).
DISCUSSION
The present findings indicate a key role for Y1 receptor in MPEP-induced anxiolytic effects. Here, as in our previous studies (Tatarczynska et al, 2001b), MPEP caused an increase in the percentage of the open arm entries/time spent in the open arms of the plus-maze. This anxiolytic action of MPEP was similar to diazepam, the compound that exerts well-known anxiolytic action in all animal tests used to screen anxiolytic drugs and that is often used as a positive control.
A question arises as to whether the antianxiety effect at MPEP is connected with a blockade at mGluR5 or NMDA receptors. O’Leary et al (2000) supposed that an inactivation of NMDA receptors by MPEP may be a reason for its anxiolytic effect. MPEP inhibited the NMDA receptor activity only at concentrations higher than 10 μM (O’Leary et al, 2000), which exceeds 1000 times its IC50 for inhibition of mGlu5 receptor activity (Gasparini et al, 2002). Moreover, at a dose of 30 mg/kg, that is, three times higher than the dose used in our experiments, MPEP did not inhibit NMDA-induced convulsions up to a dose of 125 mg/kg, i.p. (Pilc et al, 2002), which is an additional indication that at the doses used in our experiments MPEP is without influence on NMDA receptors. Therefore, all these results have shown that the anxiolytic action of MPEP is due to blockade of mGlu5 receptors.
The antianxiety effect of many classes of anxiolytic drugs, both typical as diazepam and others as serotonergic (Fernandez-Guasti and Lopez-Rubalcava, 1998) and noradrenergic ligands (Soderpalm et al, 1995), competitive NMDA receptor antagonist ACPC (Przegalinski et al, 2000) and mGlu2 receptor agonist LY354740 (Ferris et al, 2001) is blocked by flumazenil, a BZD receptor antagonist. Therefore, in the second part of the experiment, we tried to find out if flumazenil also blocks the anxiolytic action of MPEP. Its effect on the anxiolytic action of diazepam was used as a positive control. As in many earlier studies, flumazenil had no effect when given alone, but it antagonized the effect of diazepam both in the plus-maze and in the conflict drinking test (Wieronska et al, 2001b). Interestingly, the anxiolytic effects of MPEP were not changed by flumazenil administration both in the elevated plus-maze test and in the Vogel's conflict test (data not published). Our results may suggest that BZD receptors are not involved in the anxiolytic action of MPEP.
NPY alone has a clear anxiolytic action after intracerebroventricular or intra-amygdalar administration, which was found in many animal models for anxiety-related disorders (Heilig et al, 1989, 1992). Moreover, it was shown that transgenic rats overexpressing NPY showed a markedly attenuated sensitivity to behavioral consequences of stress, in that they were insensitive to the normal anxiogenic-like effect of restraint stress on the elevated plus-maze and displayed absent fear suppression on behavior in a punished drinking test (Thorsell et al, 2000). In addition, it was shown that the anxiolytic effect of NPY was not mediated through BZDs receptors, since the increase in punished responding produced by NPY is not altered by the administration of flumazenil and is only partially blocked by the picrotoxin receptor ligand isopropylbicyclophosphate (Britton et al, 1997). Both NPY- and MPEP-induced anxiolytic effects are therefore independent of BZD receptors indicating a novel and maybe a common mechanism of action. Earlier studies have revealed that the anxiolytic action of NPY was antagonized by specific antagonist of Y1 receptor, BIBO 3304 injected into the amygdala (Sajdyk et al, 1999). Amygdala is a structure involved in anxiety (Davis, 1992) and rich in NPY neurons (Gustafson et al, 1986; Smialowska and Bajkowska, 1998). BIBO 3304 is a selective NPY1 receptor antagonist with subnanomolar affinity for the rat Y1 receptors. This is one of the best known and specific Y1 antagonists used in different animal models (Capurro and Huidobro-Toro, 1999; Dumont et al, 2000). All these findings indicate that the anxiolytic-like actions of NPY is mediated by the Y1 receptors in the amygdala.
The second part of our results showed that BIBO 3304 administered into the basolateral nucleus of the amygdala did not produce any alteration in the behavior of animals, and this is in agreement with the results of other authors (Capurro and Huidobro-Toro, 1999; Sajdyk et al, 1999). However, BIBO 3304 administered into the amygdala prior to MPEP administration significantly attenuated the anxiolytic effect of MPEP, suggesting that Y1 receptors may be involved in the antianxiety action of MPEP. We suppose that glutamate via mGlu5 receptors regulates NPY neurons in the amygdala, which may affect the behaviors characteristic of anxiety. Such regulation seems to have an anatomical bases as in this study, we also showed, using an immunohistochemical method, that there is a substantial number of mGlu5 receptors in the amygdala, mainly in the lateral, basolateral, and central nuclei. The effect of MPEP on NPY neurons in the amygdala is also supported by our immunohistochemical results in which we showed a decrease in the mean number of NPY-IR neurons in the amygdala after MPEP administration in three doses every 8 h. The treatment schedule (three times, 8 h interval) was chosen on the basis on our previous experiments with receptor antagonists, which showed that visible NPY changes may be observed after a prolonged (16–24 h) strong blockade at receptors (Smialowska, 1995; Smialowska and Legutko, 1992). This decrease in NPY IR observed in the MPEP-treated group seems to be a result of diminution of the peptide content within these neurons, below the level of detection, so that less neurons are visible. In ours and other authors’ earlier immunohistochemical studies, the changes in a number of IR neurons counted in sections after different treatments were used as an index reflecting the changes in the level of immunoreactive material within them (Kerkerian et al, 1986, 1988; Smialowska et al, 1999, 2002a; Smialowska and Legutko, 1991). Therefore, the decrease in a number of NPY-IR neurons observed by us suggests a decrease in the NPY level in amygdala neurons. The immunohistochemical result is additionally confirmed by RIA of NPY in the amygdala, which also showed a diminution of NPY content in this structure after MPEP administration. We suggest that the decrease in the NPY level may result from enhanced release of the peptide and this release produces anxiolytic action; however, further studies are needed to confirm whether MPEP administration induces NPY release.
Single MPEP administration had a much weaker effect on NPY IR, as some increase was found after 6 h, but no changes after both 0.5 and 24 h. We hypothesize that MPEP activates a release of NPY from amygdala neurons, which induce an increase in NPY synthesis. Therefore, no changes in the peptide level were found after 0.5 h; then, after 6 h, synthesis is even higher than release and afterwards (24 h) all move to the central level. When MPEP is given in three doses, the prolonged mGluR5 blockade induces a more abundant NPY release, which is not compensated by the synthesis, therefore NPY-IR level is lowered.
The interaction between glutamate acting via mGlu5 receptors and NPY may represent a novel mechanism of anxiolytic action in the brain, independent of GABA–BZD receptor complex. Our present findings that anxiolytic effect of MPEP are mediated via Y1 receptors may open a new way for the discovery of novel anxiolytic substances free of adverse effects characteristic for BZDs.
References
Bennett DA, Amrick CL (1986). 2-Amino-7-phosphonoheptanoic acid (AP7) produces discriminative stimuli and anticonflict effects similar to diazepam. Life Sci 39: 2455–2461.
Britton KT, Southerland S, Van Uden E, Kirby D, Rivier J, Koob G (1997). Anxiolytic activity of NPY receptor agonists in the conflict test. Psychopharmacology (Berl) 132: 6–13.
Brodkin J, Busse C, Sukoff SJ, Varney MA (2002). Anxiolytic-like activity of the mGluR5 antagonist MPEP. A comparison with diazepam and buspirone. Pharmacol Biochem Behav 73: 359–366.
Capurro D, Huidobro-Toro JP (1999). The involvement of neuropeptide Y Y1 receptors in the blood pressure baroreflex: studies with BIBP 3226 and BIBO 3304. Eur J Pharmacol 376: 251–255.
Chojnacka-Wojcik E, Klodzinska A, Pilc A (2001). Glutamate receptor ligands as anxiolytics. Curr Opin Invest Drugs 2: 1112–1119.
Chojnacka-Wojcik E, Tatarczynska E, Pilc A (1997). The anxiolytic-like effect of metabotropic glutamate receptor antagonists after intrahippocampal injection in rats. Eur J Pharmacol 319: 153–156.
Colmers WF, Bleakman D (1994). Effects of neuropeptide Y on the electrical properties of neurons. Trends Neurosci 17: 373–379.
Conn PJ, Pin JP (1997). Pharmacology and functions of metabotropic glutamate receptors. Annu Rev Pharmacol Toxicol 37: 205–237.
Corbett R, Dunn RW (1993). Effects of 5,7 dichlorokynurenic acid on conflict, social interaction and plus maze behaviors. Neuropharmacology 32: 461–466.
Davis M (1992). The role of the amygdala in fear and anxiety. Annu Rev Neurosci 15: 353–375.
Davis M, Rainnie D, Cassell M (1994). Neurotransmission in the rat amygdala related to fear and anxiety. Trends Neurosci 17: 208–214.
Dumont Y, Cadieux A, Doods H, Fournier A, Quirion R (2000). Potent and selective tools to investigate neuropeptide Y receptors in the central and peripheral nervous systems: BIB03304 (Y1) and CGP71683A (Y5). Can J Physiol Pharmacol 78: 116–125.
Fernandez-Guasti A, Lopez-Rubalcava C (1998). Modification of the anxiolytic action of 5-HT1A compounds by GABA-benzodiazepine agents in rats. Pharmacol Biochem Behav 60: 27–32.
Ferris P, Seward E, Dawson GR (2001). Interactions between LY354740, a group II metabotropic agonist and the GABA(A)-benzodiazepine receptor complex in the rat elevated plus-maze. J Psychopharmacol 15: 76–82.
Gasparini F, Andres H, Flor PJ, Heinrich M, Inderbitzin W, Lingenhohl K et al (2002). [(3)H]-M-MPEP, a potent, subtype-selective radioligand for the metabotropic glutamate receptor subtype 5. Bioorg Med Chem Lett 12: 407–409.
Gasparini F, Lingenhohl K, Stoehr N, Flor PJ, Heinrich M, Vranesic I et al (1999). 2-Methyl-6-(phenylethynyl)-pyridine (MPEP), a potent, selective and systemically active mGlu5 receptor antagonist. Neuropharmacology 38: 1493–1503.
Gustafson EL, Card JP, Moore RY (1986). Neuropeptide Y localization in the rat amygdaloid complex. J Comp Neurol 251: 349–362.
Heilig M, McLeod S, Koob GK, Britton KT (1992). Anxiolytic-like effect of neuropeptide Y (NPY), but not other peptides in an operant conflict test. Regul Pept 41: 61–69.
Heilig M, Soderpalm B, Engel JA, Widerlov E (1989). Centrally administered neuropeptide Y (NPY) produces anxiolytic-like effects in animal anxiety models. Psychopharmacology (Berl) 98: 524–529.
Helton DR, Tizzano JP, Monn JA, Schoepp DD, Kallman MJ (1998). Anxiolytic and side-effect profile of LY354740: a potent, highly selective, orally active agonist for group II metabotropic glutamate receptors. J Pharmacol Exp Ther 284: 654–660.
Kask A, Eller M, Oreland L, Harro J (2000). Neuropeptide Y attenuates the effect of locus coeruleus denervation by DSP-4 treatment on social behaviour in the rat. Neuropeptides 34: 58–61.
Kerkerian L, Bosler O, Pelletier G, Nieoullon A (1986). Striatal neuropeptide Y neurones are under the influence of the nigrostriatal dopaminergic pathway: immunohistochemical evidence. Neurosci Lett 66: 106–112.
Kerkerian L, Salin P, Nieoullon A (1988). Pharmacological characterization of dopaminergic influence on expression of neuropeptide Y immunoreactivity by rat striatal neurons. Neuroscience 26: 809–817.
Klodzinska A, Chojnacka-Wojcik E, Palucha A, Branski P, Popik P, Pilc A (1999). Potential anti-anxiety, anti-addictive effects of LY 354740, a selective group II glutamate metabotropic receptors agonist in animal models. Neuropharmacology 38: 1831–1839.
Martin LJ, Blackstone CD, Huganir RL, Price DL (1992). Cellular localization of a metabotropic glutamate receptor in rat brain. Neuron 9: 259–270.
Micheli F (2000). Methylphenylethynylpyridine (MPEP) Novartis. Curr Opin Invest Drugs 1: 355–359.
Midgley LP, Wagstaff JD, Singh NA, Bush LG, Gibb JW, Hanson GR (1994). Dynamic dopaminergic regulation of neuropeptide Y systems in discrete striatal and accumbens regions. Eur J Pharmacol 251: 191–199.
Monn JA, Valli MJ, Massey SM, Wright RA, Salhoff CR, Johnson BG et al (1997). Design, synthesis, and pharmacological characterization of (+)-2-aminobicyclo[3.1.0]hexane-2,6-dicarboxylic acid (LY354740): a potent, selective, and orally active group 2 metabotropic glutamate receptor agonist possessing anticonvulsant and anxiolytic properties. J Med Chem 40: 528–537.
O'Leary DM, Movsesyan V, Vicini S, Faden AI (2000). Selective mGluR5 antagonists MPEP and SIB-1893 decrease NMDA or glutamate-mediated neuronal toxicity through actions that reflect NMDA receptor antagonism. Br J Pharmacol 131: 1429–1437.
Paxinos G, Watson C (1986). The rat brain in stereotoxic coordinates, 2nd edition. Academic Press inc.: San Diego, California, 92–101.
Pellow S, Chopin P, File SE, Briley M (1985). Validation of open : closed arm entries in an elevated plus-maze as a measure of anxiety in the rat. J Neurosci Methods 14: 149–167.
Pellow S, File SE (1986). Anxiolytic and anxiogenic drug effects on exploratory activity in an elevated plus-maze: a novel test of anxiety in the rat. Pharmacol Biochem Behav 24: 525–529.
Pilc A, Chojnacka-Wojcik E, Tatarczynska E, Borycz J, Kroczka B (2000). Stimulation of group II metabotropic glutamate receptors or inhibition of group I ones exerts anxiolytic-like effects in rats. Amino Acids 19: 81–86.
Pilc A, Kdzinska A, Branski P, Nowak G, Palucha S, Szewczyk B et al (2002). Multiple MPEP administrations evoke anxiolytic- and antidepressant-like effects in rats. Neuropharmacology 43: 181.
Plaznik A, Palejko W, Nazar M, Jessa M (1994). Effects of antagonists at the NMDA receptor complex in two models of anxiety. Eur Neuropsychopharmacol 4: 503–512.
Przegalinski E, Tatarczynska E, Chojnacka-Wojcik E (2000). The influence of the benzodiazepine receptor antagonist flumazenil on the anxiolytic-like effects of CGP 37849 and ACPC in rats. Neuropharmacology 39: 1858–1864.
Przegalinski E, Tatarczynska E, Deren-Wesolek A, Chojnacka-Wojcik E (1996). Anticonflict effects of a competitive NMDA receptor antagonist and a partial agonist at strychnine-insensitive glycine receptors. Pharmacol Biochem Behav 54: 73–77.
Redrobe JP, Dumont Y, Herzog H, Quirion R (2003). Neuropeptide Y (NPY) Y(2) receptors mediate behaviour in two animal models of anxiety: evidence from Y(2) receptor knockout mice. Behav Brain Res 141: 251–255.
Sajdyk TJ, Vandergriff MG, Gehlert DR (1999). Amygdalar neuropeptide Y Y1 receptors mediate the anxiolytic-like actions of neuropeptide Y in the social interaction test. Eur J Pharmacol 368: 143–147.
Scatton B (1993). The NMDA receptor complex. Fundam Clin Pharmacol 7: 389–400.
Schmidt-Mutter C, Pain L, Sandner G, Gobaille S, Maitre M (1998). The anxiolytic effect of gamma-hydroxybutyrate in the elevated plus maze is reversed by the benzodiazepine receptor antagonist, flumazenil. Eur J Pharmacol 342: 21–27.
Shigemoto R, Nomura S, Ohishi H, Sugihara H, Nakanishi S, Mizuno N (1993). Immunohistochemical localization of a metabotropic glutamate receptor, mGluR5, in the rat brain. Neurosci Lett 163: 53–57.
Smialowska M (1995). An inhibitory dopaminergic regulation of the neuropeptide Y immunoreactivity expression in the rat cerebral cortex neurons. Neuroscience 63: 589–595.
Smialowska M, Bajkowska M (1998). Reserpine induces increase in neuropeptide Y immunoreactivity in rat amygdala neurons. Pol J Pharmacol 50: 443–447.
Smialowska M, Bajkowska M, Przewlocka B, Maj M, Turchan J, Przewlocki R (1999). Effect of 6-hydroxydopamine on neuropeptide Y and corticotropin-releasing factor expression in rat amygdala. Neuroscience 94: 1125–1132.
Smialowska M, Legutko B (1991). Influence of imipramine on neuropeptide Y immunoreactivity in the rat brain. Neuroscience 41: 767–771.
Smialowska M, Legutko B (1992). Haloperidol-induced increase in neuropeptide Y immunoreactivity in the locus coeruleus of the rat brain. Neuroscience 47: 351–355.
Smialowska M, Szewczyk B, Branski P, Wieronska JM, Palucha A, Bajkowska M et al (2002a). Effect of chronic imipramine or electroconvulsive shock on the expression of mGluR1a and mGluR5a immunoreactivity in rat brain hippocampus. Neuropharmacology 42: 1016–1023.
Smialowska M, Wieronska JM, Wedzony K (2002b). A search for colocalization of mglula receptors with CRF or NPY in the rat brain amygdala. Folia Histochem Cytobiol 40: 153–154.
Soderpalm A, Blomqvist O, Soderpalm B (1995). The yohimbine-induced anticonflict effect in the rat, Part I. Involvement of noradrenergic, serotonergic and endozepinergic(?) mechanisms. J Neural Transm Gen Sect 100: 175–189.
Spooren WP, Vassout A, Neijt HC, Kuhn R, Gasparini F, Roux S et al (2000). Anxiolytic-like effects of the prototypical metabotropic glutamate receptor 5 antagonist 2-methyl-6-(phenylethynyl)pyridine in rodents. J Pharmacol Exp Ther 295: 1267–1275.
Tatarczynska E, Klodzinska A, Chojnacka-Wojcik E, Palucha A, Gasparini F, Kuhn R et al (2001a). Potential anxiolytic- and antidepressant-like effects of MPEP, a potent, selective and systemically active mGlu5 receptor antagonist. Br J Pharmacol 132: 1423–1430.
Tatarczynska E, Klodzinska A, Kroczka B, Chojnacka-Wojcik E, Pilc A (2001b). The antianxiety-like effects of antagonists of group I and agonists of group II and III metabotropic glutamate receptors after intrahippocampal administration. Psychopharmacology (Berl) 158: 94–99.
Thorsell A, Michalkiewicz M, Dumont Y, Quirion R, Caberlotto L, Rimondini R et al (2000). Behavioral insensitivity to restraint stress, absent fear suppression of behavior and impaired spatial learning in transgenic rats with hippocampal neuropeptide Y overexpression. Proc Natl Acad Sci USA 97: 12852–12857.
Trullas R, Jackson B, Skolnick P (1989). Anxiolytic properties of 1-aminocyclopropanecarboxylic acid, a ligand at strychnine-insensitive glycine receptors. Pharmacol Biochem Behav 34: 313–316.
Vidnyászky Z, Hámori J, Négyessy L, Rüegg D, Knöpfel T, Kuhn R et al (1994). Cellular and subcellular localization of the mGluR5a metabotropic glutamate receptor in rat spinal cord. NeuroReport 6: 209–213.
Wieronska JM, Branski P, Palvcha A, Smialowska M (2001a). The effect of competitive and non-competitive NMDA receptor antagonists, ACPCand MK-801 on NPY and CRF-like immunoreactivity in the rat brain amygdala. Neuropeptides 35: 219–226.
Wieronska JM, Papp M, Pilc A (2001b). Effects of anxiolytic drugs on some behavioral consequences in olfactory bulbectomized rats. Pol J Pharmacol 53: 517–525.
Winslow JT, Insel TR, Trullas R, Skolnick P (1990). Rat pup isolation calls are reduced by functional antagonists of the NMDA receptor complex. Eur J Pharmacol 190: 11–21.
Wroblewski JT, Danysz W (1989). Modulation of glutamate receptors: molecular mechanisms and functional implications. Annu Rev Pharmacol Toxicol 29: 441–474.
Acknowledgements
This study was supported partially by Statutory Founds of the Institute of Pharmacology, Polish Academy of Sciences, Kraków, Poland and partially by the Grant No. 3 P05A 135 22 from the State Committee for Scientific Research, Warszawa, Poland. JM Wieronska, A Palucha, B Szewczyk, and P Branski were supported by a grant from Foundation for Polish Science.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wierońska, J., Śmiałowska, M., Brański, P. et al. In the Amygdala Anxiolytic Action of mGlu5 Receptors Antagonist MPEP Involves Neuropeptide Y but not GABAA Signaling. Neuropsychopharmacol 29, 514–521 (2004). https://doi.org/10.1038/sj.npp.1300322
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1300322
Keywords
This article is cited by
-
Anxiolytic Properties of New Chemical Entity, 5TIO1
Neurochemical Research (2013)
-
Fear-reducing effects of intra-amygdala neuropeptide Y infusion in animal models of conditioned fear: an NPY Y1 receptor independent effect
Psychopharmacology (2009)
-
Wiring and Volume Transmission in Rat Amygdala. Implications for Fear and Anxiety
Neurochemical Research (2008)
-
The Effect of Intrahippocampal Injection of Group II and III Metobotropic Glutamate Receptor Agonists on Anxiety; the Role of Neuropeptide Y
Neuropsychopharmacology (2007)