Abstract
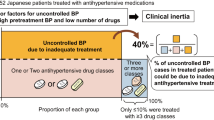
Over half of treated patients with hypertension are not well controlled. However, little is known about physicians’ prescribing behaviour for these patients. Our objective was to clarify whether physicians increase antihypertensive medication in patients with poorly controlled hypertension and what characteristics are predictors of medication increase. This was a retrospective cohort study by surveying medical records in primary care clinics in Tochigi, Japan. Twenty-nine of 79 randomly selected physicians agreed to select 20 consecutive hypertensive patients. This resulted in 547 patients (women 60%; mean (s.d.) age, 68 (12) years) who had blood pressure measurements taken in 1998 and prescription of antihypertensive medication in 1998 and 1999. Mean (s.d.) systolic/diastolic blood pressure was 142 (12)/81 (9) mm Hg and the percentage of patients in good control (<140/90 mm Hg), fair (140–159/90–94) and poor (⩾160/95) were 42%, 47%, and 11%, respectively. Physicians increased medication in 28% of poorly controlled patients (95% confidence interval (CI), 17–41%), which was more than those in fair (12%, 95%CI 8–16%) or good control (7%, 95%CI 4–12%). Multivariate logistic regression analysis showed that systolic and diastolic blood pressures were positively, and the number of kinds of antihypertensive medications and the age of the physician were negatively, associated with an increase in medication. In conclusion, primary care physicians did not increase antihypertensive medication adequately for patients with uncontrolled hypertension. Attempts to understand and to change physicians’ prescription behaviour could reduce the burden of uncontrolled hypertension among treated hypertensive patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
The sixth report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure Arch Intern Med 1997; 157: 2413–2446
Colhoun HM, Dong W, Poulter NR . Blood pressure screening, management and control in England, results from the Health Survey for England 1994 J Hypertens 1998; 16: 747–753
Smith WCS, Lee AJ, Crombie IK, Tunstall-Pedoe H . Control of blood pressure in Scotland: the rule of halves BMJ 1990; 300: 981–983
Baba S et al. Blood pressure levels, related factors, and hypertension control status of Japanese and Americans J Hum Hypertens 1991; 5: 317–332
Psaty BM et al. Temporal patterns of antihypertensive medication use among elderlypatients: The Cardiovascular Health Study JAMA 1993; 270: 1837–1841
Edwards PR et al. Hypertension management of medical aidpatients attending private practice S Afr Med J 1999; 89: 160–164
Swales JD . Current clinical practice in hypertension: The EISBERG (Evaluation and Intervention for Systolic Blood Pressure Elevation-Regional and Global) project Am Heart J 1999; 138: S231–S237
Mashru M, Lant A . Interpractice audit of diagnosis and management of hypertension in primary care: educational intervention and review of medical records BMJ 1997; 314: 942–946
Mancia G et al. Blood-pressure control in the hypertensive population Lancet 1997; 349: 454–457
Berlowitz DR et al. Inadequate management of blood pressure in a hypertensive population N Engl J Med 1998; 339: 1957–1963
Adamson TE, Rodnick JE, Guillion DS . Family physicians and general internists: do they treat hypertensivepatients differently? J Fam Practice 1989; 29: 93–99
Stockwell DH et al. The determinants of hypertension awareness, treatment, and control in an insured population Am J Public Health 1994; 84: 1768–1774
Marques-Vidal P, Tuomilehto J . Hypertension awareness, treatment and control in the community: is the ‘rule of halves’ still valid? J Hum Hypertens 1997; 11: 213–220
Feldman R et al. Adherence to pharmacologic management of hypertension Can J Public Health 1998; 89: 116–118
Guidelines Subcommittee. 1999 World Health Organization-International Society of Hypertension guidelines for the management of hypertension J Hypertens 1999; 17: 151–183
Ramsay LE et al. British Hypertension Society guidelines for hypertension management 1999; summary BMJ 1999; 319: 630–635
Du X et al. Case-control study of stroke and the quality of hypertension control in north west England BMJ 1997; 314: 272–276
Donner A . An empirical study of cluster randomization Int J Epidemiol 1982; 11: 283–286
StataCorp. Stata Statistical Software: Release 5.0 College Station, TX: Stata Corporation 1997
Statistics and Information Department, Minister's Secretariat, Minister of Health and Welfare ed. Report on Survey of Physicians, Dentists and Pharmacists, Health and Welfare Statistics Association 1998
Statistics and Information Department, Minister's Secretariat, Minister of Health and Welfare ed. Patient Survey 1996 Health and Welfare Statistics Association 1996
Tanaka H et al. A brief review of epidemiological studies on ischemic heart disease in Japan J Epidemiol 1996; 6: S49–S59
SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension: final results of the Systolic Hypertension in the Elderly Program (SHEP) JAMA 1991; 265: 3255–3264
Staessen JA et al for the Systolic Hypertension Europe (Syst-Eur) Trial Investigators. Randomised double-blind comparison of placebo and active treatment for olderpatients with isolated systolic hypertension Lancet 1997; 350: 757–764
Reeves RA . Does thispatient have hypertension?: how to measure blood pressure JAMA 1995; 273: 1211–1218
Asai Y, Kawamoto R, Nago N, Kajii E . Blood pressure measurement by primary care physicians: comparison with the standard method Nippon Koshu Eisei Zasshi 2000; 47: 326–336
Acknowledgements
We appreciate the help of all the primary care physicians who participated in this study, Rumiko Shindo for data entry, Catherine D'Este for advice on statistical analysis and John W Sellors for comments on the draft. The participated physicians were: Tsuneyuki Watanabe, Takashi Kobayashi, Kimiya Kobayashi, Koji Saito, Masaru Hirose, Atsushi lino, Takeshi Moroo, Toshio Owada, Masao Umeoka, Yuji Oohashi, Mutsumi Yoshizawa, Hideki Shinohara, Mikio Kobayashi, Shunzo Iwasaki, Tateo Ogura, Yuriko Asahi, Takashi Funada, Naruo Suzuki, Junji Tokoro, Shin Ooneta, Toshihiro Mizunuma, Akihumi Ono, Yasuhiko Kawashima, Tatsuo Kaiga, Teiichi Saito, Kenji Takayasu, Mitsuru Nakamura, Masaki Kawano and Koji Niizaki.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Asai, Y., Heller, R. & Kajii, E. Hypertension control and medication increase in primary care. J Hum Hypertens 16, 313–318 (2002). https://doi.org/10.1038/sj.jhh.1001385
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jhh.1001385
Keywords
This article is cited by
-
Perspectives of patients and physicians regarding hypertensive management from an online survey for excellence: a subanalysis of the PARADOX study by physician categories
Hypertension Research (2020)
-
Racial Disparities in Hypertension Control, but Not Treatment Intensification
American Journal of Hypertension (2010)
-
Why Don’t Diabetes Patients Achieve Recommended Risk Factor Targets? Poor Adherence versus Lack of Treatment Intensification
Journal of General Internal Medicine (2008)
-
Risk factors for uncontrolled hypertension in Italy
Journal of Human Hypertension (2004)