Abstract
We have previously reported the isolation of a gene from Xq13, coding for a putative regulator of transcription (XNP). It is a member of the helicase family, and has now been shown to be the gene involved in the X-linked α-thalassemia/mental retardation (ATR-X) syndrome. ATR-X mutations were only found in the 3′-part of the coding sequence, which includes the helicase domains. However, no ATR-X mutation has yet been found in one of the seven conserved helicase domains. In this paper, we report a mutation in XNP, segregating in a family presenting an ‘ATR-X’ phenotype without α-thalassemia, that causes a proline to serine transition in the helicase II domain.
Similar content being viewed by others
Introduction
We have previously reported physical and transcriptional mapping in the Xq13.3 region [1, 2] and described several genes which had been postulated as candidates for genes involved in X-linked mental retardation (XLMR). One, which we named XNP, is particularly interesting as the transcript is abundant both in human and mouse brain. In the developing mouse brain, the gene is highly expressed in territories where neural proliferation is occurring. Its expression is reduced once the neurones are fully differentiated, making XNP a good candidate for a gene responsible for an MR phenotype [3]. Database comparisons with XNP putative protein show that it is a member of the helicase family, as it contains the seven conserved protein domains shared by all the members of the DNA helicase family [4, 5]. It has recently been shown to be mutated in 13 patients with α-thalassemia/mental retardation (ATR-X) syndrome [6, 7]. Missense and nonsense mutations were found and one patient showed a 2kb deletion in the 3′-region of the gene. All these mutations involve the 3′-half of the coding region of the gene. However, no mutations have so far been found in one of the seven conserved helicase domains. Based on the large spectrum of expression of this gene in various tissues [3], we have postulated that different mutations in this gene could lead to variations in clinical presentation.
In a recent report, we have described a mutation in the conserved helicase V domain, segregating with the Juberg-Marsidi syndrome in a large family [8]. In this paper, we report a family in which a mutation in this gene segregates with an ‘ATR-X-like’ phenotype, but without associated α-thalassemia. This mutation is located in the conserved helicase II domain. This is, thus, the second case of a mutation in a conserved helicase domain of the XNP gene, segregating with an X-linked mental retardation syndrome, without α-thalassemia.
Methods
Lymphocytes were prepared as follows: 10 ml of fresh blood (obtained after informed consent) was diluted to 1/2 (v/v) in PBS and loaded onto 15 ml of Lymphoprep™. The tube was then centrifuged for 40 min at 1,200 rpm in order to recover the lymphocytes at the interphase. Cells were washed twice in PBS. PolyA+ RNA was then prepared using the QuickPrep mRNA purification kit according to the manufacturer’s instructions (Pharmacia). 500 ng of mRNA were reverse transcribed in 50 µl of 1X Superscript reaction buffer (Gibco BRL) containing 3 ng/µl (dN)6, 40 units of RNasin (Promega), 1 mM dNTP and 200 units Superscript II reverse transcriptase (Gibco BRL). PCR reactions were conducted using standard conditions in 100 µl reaction volume and 1/10th of the 1st-strand reaction. The primers used to amplify the whole coding region of the XNP cDNA were: XNP21/XNP2 CTGAGAAGTCAACAGGGAAAGG and CTTGAACCTTAATACGTCGCC 1,100-bp amplicon; XNP3/XNP23 GTGAATCCGAAGATGAACAGC and GAGGACGTTTCACAGTTGC 811-bp amplicon; XNP5/XNP6 GACAAACTGGATTTCAGCACG and TCTAGCTGCAAACACCAAGG 836-bp amplicon; XNP7/XNP8 GCTCTATGCAGGTGCAAAGC and TCCAGAGATATGAGGGACTGG 549-bp amplicon; XNP9/XNP10 AATGGCAGAGGAAATTGGG and GAAACGCATGGTCAGTACC 788-bp amplicon; XNP11/XNP22 GAAGAAGGTACTGACCATGC and GCCACTGGCTGATACATTCC 547-bp amplicon. Additional primers: XNP25/XNP26 TTCTATACGATCAAGGAGGAGG and ATATTCGTGTTTTGGAGGC. PCR primers used to amplify genomic sequences of XNP in the critical region were as follows: XNP 73: 5′ GTGCTGTATTAACCAAATACGGG, XNP 31: 5′ AAATAATCCTCCTCCTTGATCG. All primers were used at 60°C annealing temperature. Amplification products were directly sequenced.
Results
We have studied a family in which an X-linked mental retardation phenotype segregates over at least two generations. The pedigree is presented in figure 1a. Patient III.1 has severe mental retardation with hypotonia; speech was absent at age 4. Typical facial features (fig. 1b) include epicathic folds, telecantus, midface hypoplasia, flat nasal bridge, small triangular nose with anteverted nostrils and with columella not extending below the nasal alae, carp-shaped mouth, hypoplastic lower central incisors, apparently low-set and posteriorly angulated ears, and protrusion of the tongue. There were short tagering fingers and overlapping toes. External genitalia were normal. He had no anemia. Hematological examinations was performed at 2 years of age and the results were in the normal range for a young child (MCV: 76.6 fl and MCH: 25.1 pg/cell). HbH screening, after incubation of fresh red cells with 1% brilliant cresyl blue at room temperature (3–24 h), was negative on three separate occasions. This was confirmed by starch gel electrophoresis, performed in neutral and alkaline buffers, which failed to show the presence of HbH. Chromosome analysis, fragile-X screening, brain CT scan, and metabolic screening were negative.
Patient II.3 was the maternal uncle of the propositus. He was severely mentally retarded, could not speak and died at 7 years of age. Photographs showed the same facial dysmorphism as his nephew.
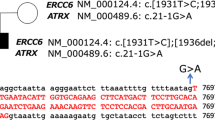
As the clinical examination clearly indicated an ‘ATR-X-like’ phenotype, even though no thalassemia is present in the family, we searched for a mutation in the XNP gene in the affected proband (patient III.1). As XNP is expressed in lymphocytes, RNA was exctracted from the fresh blood of patient III.1, in order to perform RT-PCR. We found no abnormal PCR products and thus sequenced the whole coding region (5 kb), using a set of primers we have designed (see Methods). The sequence was compared to the reference sequence (Genbank access number: L34363), and one point mutation was found, at codon 852 (fig. 2). This mutation causes the replacement of a proline by a serine, a change which is not conservative. It should be noted that this mutation lies in a domain that is conserved between different members of the helicase family (domain II) [5].
Position of the mutation in the mutant XNP transcript (III.1). HaeIII restriction sites in the cDNA fragment amplified using primers XNP31/XNP73 are indicated by small vertical lines, both in III.1 and in a normal control. The mutation disrupts a HaeIII site in the patient. The respective length of individual HaeIII restriction fragments is indicated. The partial normal and mutated XNP cDNA (III.1) and protein sequences are indicated and numbered according to the previously published data (GenBank access number: L34363).
This mutation destroys a HaeIII restriction site, and we used this difference to look for this mutation in the family and in the general population. This mutation was not found in 150 unrelated chromosomes (data not shown), ruling out the possibility of a polymorphism. We also analyzed the inheritance of the mutation in the family (fig. 3). The mutation is transmitted by females, who are obligate unaffected carriers. This mode of transmission is clearly X-linked, and is consistent with the hypothesis of a pathological role of this mutation.
Segregation of the mutation in the family. After PCR amplification with XNP primers, the resulting product was digested with HaeIII and electrophoresed. Normal individuals share three fragments of 175, 75 and 27 bp. Because the mutation abolishes a HaeIII site, affected patients share only two fragments of 202 and 75 bp. Lane 1: individual III.1; lane 2: individual III.2; lane 3: individual II.2; lane 4: individual 1.2, lane 5 = a control male; lane 6 = a control female. The marker (100 bp ladder) is at the extreme right.
Schematic representation of the position of XNP mutations. ‘Full ATR-X’ mutations [7, 12] are indicated below. This includes a splicing mutation [12] and two nonsense mutations [7], indicated by asterisks. Other mutations are missense mutations (position and amino acid changes are indicated). The position of the two missense XNP mutations without thalassemic clinical presentation, the Juberg-Marsidi mutation [8] in helicase V domain and the presently reported mutation in helicase II domain, are indicated above and underlined. The position of the seven conserved helicase domains in the putative protein is indicated by dark bars (and numbered, from IA to VI). The position of the polyglutamic acid stretch, (E)n, is also indicated.
Discussion
The archetype of the manifestation of the ATR-X syndrome includes severe and global mental retardation without speech, characteristic facial appearance, urogenital abnormalities, a mild type of α-thalassemia, and miscellaneous abnormalities (growth retardation, cardiac defects, cleft palate, mild skeletal abnormalities, renal malformations …) [9]. Genital abnormalities can lead to sex reversal [10], but are not always present [11]. Facial dysmorphic features and severe mental retardations appear to be the only constant features. The mild α-thalassemia includes a perturbation in the α-globin chain synthesis, leading to a lower level of Hb, hypochromic and microcytic red blood cells. The most classical finding is the presence of HbH inclusions in fresh blood cells. We may note that these features were not found in the propositus (globin chain synthesis was performed, but was unfortunately inconclusive; data not shown).
We have already reported a family, in which a splicing mutation in the XNP gene segregated with an ATR-X phenotype with neither α-thalassemia nor HbH disease [12]. We correlated the absence of α-thalassemia to the expression of significant amount (about 30%) of the correctly spliced transcript, a situation comparable to that found in Menkes/occipital horn syndrome [13]. In the present case, a point mutation introduces a nonconservative change in the aminoacids of the putative XNP protein. This mutation is located in the 3′-part of the gene, in the region in which the classical ATR-X mutations were found [7]. However, in contrast to mutations inducing a full ATR-X phenotype, this mutation lies in a putative ‘helicase domain’, defined by homologies with yeast and drosophila genes. We have recently explored a large pedigree, in which a Juberg-Marsidi syndrome segregates, and demonstrated that the genetic basis of the disease, in this family, was the presence of a point mutation, changing a well-conserved amino acid in the helicase V domain [8]. An outline of the XNP mutations reported to date and their associated phenotype is displayed in figure 4. We cannot speculate further on the relationship between nonthalassemic phenotypes and mutations in the conserved domains, as this hypothesis is based only on 2 cases. Moreover, as we know that the expression of the gene is widespread, it is highly probable that, apart from constant clinical signs, such as severe mental regardation and facial dysmorphism, other clinical signs, as genital disorders and thalassemia, will be variable. As the syndrome was first reported as α-thalassemia with mental retardation, only patients exhibiting an association of these two traits have been considered as ATRX so far. It is thus very important to search for XNP mutations in additional XLMR patients presenting characteristic facial dysmorphism, but without α-thalassemia.
References
Gecz J, Villard L, Lossi AM, Millasseau P, Djabali M, Fontés M: Physical and transcriptional mapping of DXS56-PGK1 1 Mb region: Identification of three new transcripts. Hum Mol Genet 1993;2:1389–1396
Villard L, Gecz J, Colleaux L, Lossi AM, Chelly J, Ishikawa-Brush Y, Monaco AP, Fontés M: Construction of a YAC contig spanning the Xq13.3 subband. Genomics 1995,26:115–122.
Gecz J, Pollard H, Consalez GG, Villard L, Stayton C, Millasseau P, Khrestchatisky M, Fontés M: Cloning and expression of the murine homologue of a putative human X-linked nuclear protein gene closely linked to PGK1 in Xq13.3. Hum Mol Genet 1994;3:39–44
Stayton CL, Dabovic B, Gulisano M, Gecz J, Broccoli V, Giovanazzi S, Bossolasco M, Monaco L, Rastan S, Boncinelli E, Bianchi ME, Consalez G: Cloning and characterization of a new human Xq13 gene, encoding a putative helicase. Hum Mol Genet 1994;3:1957–1964
Carlson M, Laurent BC: The SNF/SWI family of global transcriptional activators. Curr Opin Cell Biol 1994;6:396–402
Gibbons RJ, Suthers GK, Wolkie AOM, Buckle VJ, Higgs DR: X-linked alpha-thalassemia/mental retardation (ATR-X) syndrome: Localization to Xq12-21.3 by X inactivation and linkage analysis. Am J Hum Genet 1992;51:1138–1149
Gibbons RJ, Picketts DJ, Villard L, Higgs DR: Mutations in a putative global transcriptional regulator cause X-linked mental retardation with α-thalassemia (ATR-X syndrome). Cell 1995;80:837–845
Villard L, Saugier-Veber P, Gecz J, Mattei JF, Munnich A, Lyonnet S, Fontés M: XNP mutation in a large family with Juberg-Marsidi syndrome. Nature Genet 1996;12:359–360
Gibbons RJ, Bruton L, Buckle VJ, Burn J, Clayton-Smith J, Davison BCC, Gardner RJM, Homfray T, Kearney L, Kingston HM, Newbury-Ecob R, Porteous MEP, Wilkie AOM, Higgs DR: Clinical and hematologic aspects of the X-linked α-thalassemia/mental retardation syndrome (ATR-X). Am J Med Genet 1995;55:288–299
Lacombe D, Pedespan JM, Taib J, Micheau M, Guerin V: Syndrome α-thalassémie/retard mental lié à l’X. Arch Fr Pédiatr 1993;50:723–724
McPherson EW, Clemens MM, Gibbons RJ, Higgs DR: X-linked α-thalassemia/mental retardation (ATR-X) syndrome: A new kindred with severe genital anomalies and mild hematologic expression. Am J Med Genet 1995;55:302–306
Villard L, Toutain A, Lossi AM, Gecz J, Houdayer C, Moraine C, Fontés M: Splicing mutation in the ATR-X gene can lead to a dysmorphic mental regardation phenotype without α-thalassemia. Am J Hum Genet 1996,58:499–505.
Das S, Levinson B, Vulpe C, Whitney S, Gitschier J, Packman S: Similar splicing mutations of the Menkes/Mottled copper-transporting ATPase gene in occipital horn syndrome and the blotchy mouse. Am J Hum Genet 1995:56:570–576.
Acknowledgements
We thank the family members for their cooperation. We would like to thank D. Lena for discussing hematological examinations and M. Mitchell for critical reading of the manuscript. This work was financially supported by the Groupement d’Etudes et de Recherches sur les Génomes (GREG).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Villard, L., Lacombe, D. & Fontés, M. A Point Mutation in the XNP Gene, Associated with an ATR-X Phenotype without α-Thalassemia. Eur J Hum Genet 4, 316–320 (1996). https://doi.org/10.1159/000472225
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1159/000472225
Key Words
This article is cited by
-
Alpha thalassaemia-mental retardation, X linked
Orphanet Journal of Rare Diseases (2006)
-
Mutation in the 5′ alternatively spliced region of the XNP/ATR-X gene causes Chudley–Lowry syndrome
European Journal of Human Genetics (2005)