Abstract
The COVID-19 pandemic had a profound global impact, characterized by a high fatality rate and the emergence of enduring consequences known as Long COVID. Our study sought to determine the prevalence of Long COVID syndrome within a population of Northeastern Mexico, correlating it with patients' comorbidities, number of COVID-19 reinfection, and vaccination status. Employing an observational cross-sectional approach, we administered a comprehensive questionnaire covering medical history, demographics, vaccination status, COVID-related symptoms, and treatment. Our participant cohort included 807 patients, with an average age of 41.5 (SD 13.6) years, and women accounting 59.3% of the cohort. The follow-up was 488 (IQR 456) days. One hundred sixty-eight subjects (20.9%) met Long COVID criteria. Long COVID-19 was more prevalent when subjects had reinfections (p = 0.02) and less frequent when they had a complete vaccination scheme (p = 0.05). Through logistic regression, we found that male gender (OR 0.5, p ≤ 0.001), blood types of AB− (OR 0.48, p = 0.003) and O− (OR 0.27, p ≤ 0.001) in comparison with A+ and two doses of vaccines (OR 0.5, p = 006) to be protective factors against Long COVID; while higher BMI (OR 1.04, p = 0.005) was a risk factor. We saw that the prevalence of Long COVID was different within vaccinated patients and specific blood types, while being female and a higher BMI were associated with an increased risk of having long-COVID.
Similar content being viewed by others
Introduction
The COVID-19 global pandemic caused by the severe acute respiratory syndrome Coronavirus-2 started in 2019, and has been responsible for more than 700 million cases and nearly 7 million deaths1. The established pathogenetic mechanism by which the virus infiltrates its host involves the binding of its spike protein to angiotensin-converting enzyme 2 (ACE2). This, in turn, triggers an inflammatory cascade orchestrated by both cellular and humoral immune responses, culminating in a spectrum of acute symptoms that can range from a mild flu-like illness to severe acute respiratory distress syndrome (ARDS) accompanied by multiorgan failure2. Recent studies have shown that subjects that recovered from acute infection could develop a reinfection3. Since the introduction of vaccines against SARS-CoV-2, the incidence and severity of the disease have decreased globally. The main vaccines used in the Mexican population were Pfizer-BioNTech BNT162b2, Moderna Spikevax, Oxford/AstraZeneca ChAdOx1-S, Janssen Ad26.COV2.S, Sinovac-CoronaVac, CanSino Biologics Ad5-nCoV-S, and Sputnik V. The accessibility was different depending on the region and age. Their efficacy for prevention of acute or severe diseases varies from > 90% (mainly those of messenger RNA) to as low as 50%4. Nowadays, the community knows the possible vaccine combinations that enhance their response against the acute infection5.
Long COVID syndrome, or post-acute COVID-19 syndrome, is defined, according to the Center for disease control and prevention (CDC), as a clinical condition in which the symptoms associated with acute infection of COVID-19 persist for a duration of 4 weeks or more following the initial diagnosis. Several signs and symptoms are associated with this disease, affecting different organic systems, and they vary from persistent coughing to cardiovascular complications6,7,8. This syndrome has been associated with multiple factors, mainly from the host and the severity of the acute disease. The main risk factors associated are female sex, hypertension, obesity, and immunocompromised patients7,8. The pathophysiological mechanisms are not well established yet, but it is believed that it is linked to chronic inflammation caused by the persistence of viral load, lymphopenia, and autoimmune factors, which result in long-term tissue damage. The theory by which these autoimmune factors are present is believed to be associated to persistence of spike proteins in the blood stream9. Additionally, there has been an observed association with the presence of inflammatory cytokines: IL-6, tumor necrosis factor alpha, nitric oxide, and calcium channel modulating activity10.
Numerous cohort and observational studies have confirmed a relationship between vaccination status within a group experiencing Long COVID and a control group without symptoms; most of them evaluated the relation with BNT16b2 vaccine or ChAdOx1-S. One such investigation, involving 28,356 adults aged 18–69 in England, examined those who had tested positive for COVID-19 and subsequently received vaccination. Within this cohort, 23.7% reported symptoms indicative of Long COVID syndrome. A parallel study in France followed up with 155 adults who had experienced COVID-19 symptoms. Over a 120-day span, 16.6% of the vaccinated individuals experienced a complete resolution of symptoms, in contrast to 7.5% of those who remained unvaccinated11,12. An additional study, also conducted in the United Kingdom, explored the connection between post-vaccine antibody titers and post-COVID syndrome. Within this context, 61% reported no alteration in symptoms, 21% noted worsening, and 16% experienced improvement 2 weeks following vaccination13. A systematic review by the UK Health Security Agency, encompassing 16 observational studies conducted in 2022, concluded that vaccines were effective in preventing Long COVID, particularly with earlier virus variants, largely by averting acute infections14. In a meta-analysis encompassing 12 global studies and a collective patient pool of 614,392 individuals, variations in the reduction of odds ratios (OR) were observed across different vaccination doses. However, the significance of this information was deemed inconclusive due to substantial heterogeneity among the studies15. In Italy, a different study determined a Long COVID syndrome prevalence rate of 31%, which exhibited a decline across the initial three pandemic waves and in conjunction with the BNT162b2 vaccine16. There is scare information that has evaluated different vaccination schemes with/without booster and the prevalence of Long COVID.
In Mexico, a case–control study was undertaken involving 219 patients across three different cities. This study aimed to compare the risk of developing persistent COVID-19 symptoms between individuals who had contracted symptomatic infection and those who remained symptom-free. The findings revealed an elevated risk of Long COVID when the infection was symptomatic, with a relative risk (RR) of 2.43 (90% CI 1.78, 3.33). Among the symptoms reported, those associated with a heightened risk of persisting after a COVID-19 infection included chills, dyspnea, new anosmia or dysgeusia, nausea or vomiting, cough, and red eyes17. In another study focusing on symptom clusters within a central Mexican hospital, a prevalence of COVID-19 symptoms was observed at 23.8% within 30 days following hospital discharge. After 90 days of follow-up, many symptoms displayed a tendency to decrease, except for specific symptoms such as alopecia, rhinorrhea, lacrimation, lack of concentration, paresthesia, arthralgias, and memory loss18. The comprehensive investigation conceded no existing findings about the relationship between vaccines in Mexico and the prevalence of Long COVID. Given the considerable diversity in vaccine administration within the Mexican population, it becomes crucial to explore whether these findings diverge from studies conducted in regions where vaccine distribution was more selective. Also, there is scare information of the relation with Long COVID, reinfection in Mexico.
This study aimed to determine the prevalence of Long COVID syndrome in a population living in Northeastern Mexico. Additionally, it aimed to explore potential differences in the occurrence of Long COVID based on vaccination status and the frequency of COVID-19 reinfections. Lastly, the study aimed to uncover any potential associations between clinical risk factors and the emergence of Long COVID within our specific region.
Results
There was a total of 818 surveys applied; however, a total of 804 were analyzed after duplicates were removed and exclusion criteria applied. The median (IQR) follow-up of the patients from the first COVID-19 infection until survey application was 488.5 (456). They were a total of 477 (59.3%) women and 327 (40.6%) men with a mean (SD) age of 41.5 (13.6) years. There were 535 (66.5%) patients that had no history of any medical condition.
The most prevalent diseases were the presence of hypertension with 127 (15.8%) patients, type 2 diabetes with 122 (15.2%), and autoimmune disease with 54 (6.7%), which had not significant differences between subjects that developed Long COVID vs. the control group. Subjects that developed Long COVID had a statistically significant higher frequency of a history of allergies [n = 37 (31.4%) vs n = 81 (13.1%)], p = 0.022. The rest of the variables regarding the medical history by presence of Long COVID are addressed in Table 1.
Among the different vaccination schemes the surveyed had, the most common were the complete scheme with the Pfizer-BioNTech BNT162b2 plus a booster with 273 (34%) patients, of which the type of booster vaccine varied. After that, the second most common scheme was the Sinovac-CoronaVac regime plus booster with a total of 123 (14.1%) patients, followed the Oxford/AstraZeneca ChAdOx1-S complete regime plus booster with 110 (13.7%) patients. The least common vaccines that people received were the CanSino Biologics Ad5-nCoV-S (n = 22, 2.7%), Janssen Ad26.COV2-S (n = 8, 1.0%) and Sputnik V Gam-COVID-Vac regime had the least amount (n = 4, 0.5%). The rest of the variables regarding the most common vaccination schemes are addressed in Table 2.
Of the surveyed patients, a total of 804 individuals experienced acute COVID-19 at least once since March 2020. Most of these patients were treated ambulatory, reflecting a mild disease (n = 674, 83%). Within this group, 168 (20.9%) patients met the criteria for Long COVID during their initial COVID-19 infection. The most prevalent symptom associated with Long COVID in this cohort was fatigue/tiredness, which was present in 50 (29.8%) patients. Other prevalent symptoms included alopecia in 35 (20.8%) patients, dysgeusia in 30 (17.9%) patients, and cough in 29 (17.3%) patients.
A significant difference was observed in the prevalence of Long COVID syndrome among distinct vaccination categories. Among the unvaccinated group, 73 (25.1%) individuals experienced Long COVID, the group with incomplete vaccination regimen included 16 (18.4%) individuals experienced Long COVID. Notably, the prevalence of Long COVID was lowest in the group with a complete vaccination regimen, with 43 (16%) individuals. The group that received a booster shot consisted of 36 (22.8%) individuals with Long COVID. This difference of overall Long COVID prevalence between vaccination status groups reached statistical significance, p = 0.05. Among patients experiencing anosmia as a symptom of Long COVID syndrome, a statistically significant difference in vaccination status was observed on patients with complete vaccination regime, p = 0.049. There was no other statistical difference between the vaccination groups and the isolated symptoms. The rest of the variables regarding diagnosis and symptoms of Long COVID within the first COVID-19 infection, along with the corresponding comparison to vaccination are addressed in Table 3.
A total of 188 patients experienced a second COVID-19 infection, of which 163 (86%) received ambulatory treatment and 28 (14.8%) individuals met the criteria for Long COVID syndrome. The prevailing symptoms within this group were fatigue/tiredness, affecting 8 (28.5%) patients, followed by persistent cough, which impacted 7 (25%) patients. Among the individuals who contracted the virus for a third time (24 in total, 91% received ambulatory treatment), only 4 (16.7%) of them fulfilled the criteria for Long COVID. The symptoms observed in this subset included fatigue/tiredness in 1 case (25%), migraine in 1 case (25%), alopecia in 1 case (25%), and anosmia in 1 case (25%). Notably, no significant distinction was observed between the vaccination status and the presence of Long COVID in either of these groups. Some of the same individuals that had Long COVID during the first infection also developed it after the second infection and during the third infection. But from the 28 cases in the second infection 17 were new cases and no new Long COVID cases were found during the third infection. The rest of the variables regarding diagnosis and symptoms of Long COVID within the second and third COVID-19 infection, along with the corresponding comparison to vaccination are addressed in Tables 4 and 5. When comparing the number of reinfection and the presence of Long COVID through chi-square text there was a higher prevalence in the group with more reinfections, p = 0.02.
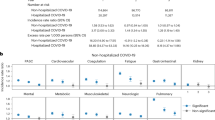
Additionally, a logistic regression model was executed to pinpoint predictors of the Long COVID syndrome. The dependent variable was the presence of Long COVID, and the independent variables were age, gender, Body Mass index (BMI), blood type, number of reinfections and the number of vaccine schemes in the first infection. The findings showed a reduction in the risk to present Long COVID in male gender (OR 0.520, p = 0.001), AB− (OR 0.481, p = 0.003), and blood type O− (OR 0.276, p ≤ 0.001) in comparison with A+ and the presence of two vaccines (OR 0.551, p = 0.006); while a higher BMI (OR 1.043, p = 0.005) was the main risk factors. Reinfection had a marginal effect (p = 0.097) and there was no effect on age or the presence of allergies. Further details regarding the remaining variables in this model can be found in Table 6.
Discussion
This cross-sectional observational study showed a prevalence of Long COVID of 20.9% during the first infection, 14.8% during second reinfection and 16.7% after third reinfection. There was a reduced prevalence of Long COVID when patients had a complete vaccination scheme that could include one or two boost of any of the studied vaccines. Additional risk factors for Long COVID were being female, BMI, and the number of reinfections. The protective factors were blood type AB− and O− in comparison with A+.
The overall prevalence of Long COVID of 20.9%, aligns with the range of prevalence documented in studies from various countries6,12,15,16,18. The most prevalent symptoms overall were fatigue, hair loss, cough, sore throat, rhinorrhea, dyspnea, insomnia, and migraine. These results are consistent compared with other studies, although some place memory loss and concentration issues among the common symptoms associated with Long COVID and we did not find these issues8.
In relation to patient comorbidities associated with the presence of Long COVID, our investigation revealed a higher prevalence of history of allergies in the Long COVID group; however, in the regression model it did not show to be a risk factor. Nonetheless, when contrasting the outcomes between the non-Long COVID group and the Long COVID group, similar proportions were found including Hypertension, Type 2 Diabetes, Autoimmune Diseases, and Dyslipidemia. Additionally, through our regression model we found other risk factors such as being female, overweight or obese and A+ blood type in comparison with O− or AB-. In the literature there are heterogeneity of results, some studies confirm our findings, while other studies do not, this could be in relation to the different design of the studies and in relation that studies are conducted in different populations and that Long COVID distributes differently according to several sociodemographic status9,19
Concerning the vaccine's effectiveness in averting Long COVID symptoms, statistically significant findings emerged for patients who received a two-dose scheme before COVID-19 infection showing a lowered prevalence of Long COVID; also patients with a booster dose had a lower prevalence of anosmia. However, no distinction was observed between the vaccinated and unvaccinated groups during second and third reinfections. Nevertheless, an important decrease in the prevalence of Long COVID syndrome was evident among patients with multiple infections, compared to the prevalence of the first infection. This phenomenon might be linked to a favorable correlation with their vaccination status, the existence of less aggressive viral variants, or the plausible influence of acquired natural immunity from prior infections. The Cohort studied by Richard et al., showed that vaccination after COVID-19 infection was associated to a reduction in symptoms of Long COVID at 6 months20. Furthermore, in a longitudinal study conducted by Azzolini et al., the prevalence of Long COVID showed a decline within the BNT162b2 vaccinated group when contrasted with the unvaccinated cohort16. The limitation of these studies is that the population was vaccinated with ChAdOx1nCoV-19 Oxford-AstraZeneca, Ad26.COV2.S Janssen COVID-19, BNT162b2 Pfizer-BioNTech and mRNA-1273 Moderna. Our study adds an analysis of a population with more diverse scheme of vaccination showing that all combinations are related to a lower prevalence of Long COVID in the first infection.
In regards of the COVID-19 reinfection, we saw a notable decrease in the prevalence of Long COVID compared to the total of patients that tested positive. During the first infection the prevalence was 20.9%, in the second infection was 14.9%, and in the third 16.7%. Our Chi-square model showed a higher proportion of Long COVID in subjects with multiple reinfections; however, our regression modeled showed marginal effects. In the literature there are contradictory results. The study of Bowe et al. reported that after two or more reinfection and a follow-up of 6 months, there was an increase in pulmonary, cardiovascular, hematological, musculoskeletal, gastrointestinal, kidney and neurological sequalae regardless of vaccination status. The limitation of the study was that the subjects were predominantly Caucasian males21. A study conducted in the Amazonas that included 1371 patients that were infected with SARS-COV-2 showed that reinfection was associated with higher number of symptoms of Long COVID22. In a separate prospective study carried out in Italy by Peghin et al., an observation spanning 2 years was conducted on patients who had experienced a COVID-19 infection, there was discernible influence of reinfection on the dynamics of Long COVID syndrome23.
Within our predictive model, the male sex, as well as blood types AB− and O−, and two vaccination schemes before first COVID-19 infection emerged as protective factors against the development of Long COVID syndrome. Conversely, female sex and higher BMI were associated with an elevated likelihood of experiencing Long COVID following a COVID-19 infection. Finally, we did not find any correlation with age. In the study conducted in Amazonas, BMI and female gender were also related to be risk factors22. Female risk was also confirmed by Bechmann et al.24 and other researchers9,18. In relation to blood type. Other studies have reported that A+ is a risk factor for Long COVID; we found this association but only when compared with AB− and O− blood types. Caution must be taken when interpreting the significance of blood types A− and B− in relation to Long COVID in our model, as the limited number of patients with these blood types in our subjects makes it challenging to draw definitive conclusions about their potential risk or protective effects against the condition. Finally, in a review conducted by Abul et al., it was observed that the prevalence of Long COVID rises among older adults. Approximately 1 in 4 older adults may experience this syndrome, contrasting with 1 in 5 among the younger population25; in our study we could not confirm this finding.
The value of this research study is that it analyzes the risk factors for Long COVID in a Northern population of Mexico that is exposed to different brands and types of vaccines that are not frequently reported in the literature. These subjects could suffer of multiple reinfections confirmed by SARS-COV 2 PCR and analyzes other risk factors such as gender, age, BMI, blood type and comorbidities.
The primary limitation encountered during this investigation revolves around the absence of a population with moderate to severe disease; nearly all subjects included in the study exhibited mild symptoms. Research indicates that individuals with more severe illnesses, necessitating invasive treatments like ECMO, often grapple with emotional and physical consequences in contrast to those who experience milder disease and treatment18,26.
Another limitation stemmed from the lack of information pertaining to the specific viral variant responsible for the acute infection. This data gap hinders our ability to explore potential associations with the development of Long COVID syndrome. This shortfall is primarily attributed to the limited molecular testing that most patients underwent. Filling this gap could have provided valuable insights and facilitated additional correlations with disease prevalence. While it's possible to infer the variant based on the infection date, considering the prevailing prevalence during the specific wave of infection, this method remains inherently imprecise. An additional challenge encountered in this study pertained to the analysis of Long COVID symptoms following the second and third COVID-19 infections. This challenge stemmed from the limited number of subjects within each group, which resulted in potentially unreliable p values from the chi-square analysis.
A significant bias observed in our study relates to memory recall, as patients often struggled to recollect precise details. To address this, patients consulted family members and documents saved in their personal items to aid their recollection. We mitigated this issue by conducting individualized interviews through a questionnaire and requesting patients to present their vaccination certificates as validation.
In conclusion, our findings reveal a reduction in the prevalence of Long COVID infection among the vaccinated groups when compared to the unvaccinated cohort. This prevalence aligns with the average reported in diverse meta-analyses. Furthermore, a decrease in the overall prevalence within reinfections was observed. Certain risk factors are linked to a heightened likelihood of developing Long COVID following a COVID-19 infection such as female gender and BMI, while other factors indicate a lower risk. Notably, a protective association was identified with blood types O− and AB− and two vaccine schemes of any vaccine.
This intricate and nonspecific syndrome presents numerous aspects that remain to be fully comprehended. To establish a comprehensive understanding, standardized multi-centric trials should be undertaken, aimed at discerning the true prevalence, severity, and associations inherent to this syndrome. This effort is essential to equip medical practitioners with the insights required to offer optimal treatment strategies to patients grappling with Long COVID.
Methodology
We executed an observational cross-sectional study within a hospital situated in Northeastern Mexico called Hospital Clinica Nova, this clinic attends a population of 50,000 steel workers and their families offering from vaccination and preventive healthcare to hospitalization and management of severe diseases. This study focused on patients with a prior occurrence of acute COVID-19 infection. The methodology adhered to the STROBE guidelines27. Approval for the study was obtained from the local Institutional Review Board (reference 170102022-CNa-MIa-CI), and all procedures were conducted in accordance with the ethical principles outlined in the World Medical Association's Code of Ethics (Declaration of Helsinki) pertaining to human experimentation.
The eligibility criteria encompassed adults aged 18 or older who were associated with the medical services at our hospital. To be included, participants needed to have a documented history of a COVID-19 infection confirmed through a positive diagnostic test. Acceptable tests included reverse transcriptase polymerase chain reaction (RT-PCR) or SARS-COV2 antigen test. Conversely, individuals were excluded if they exhibited suspected COVID-19 symptoms but lacked a positive diagnostic test. Also excluded were those who had experienced an acute infection within the last 4 weeks and failed to provide the comprehensive information requested during the interview.
Data collection occurred within the timeframe spanning April to May 2023. Following the signing of the informed consent, every participant underwent a comprehensive survey encompassing inquiries related to demographics (age, gender), anthropometric information [height (cm), weight (kg), body Mass Index], blood type, and patient comorbidities (Type 1 or 2 diabetes, hypertension, obstructive pulmonary disease, dyslipidemia, active cancer, previous cancer, heart failure, coronary disease, atrial fibrillation, cerebral vascular event, end stage renal disease, autoimmune disease, rheumatology disease, use of immunosuppressive medicine, organ transplantation, allergies, any medications, etc.). The number of reinfections was documented, and it was defined as a SARS-COV2 positive test, followed by a negative test that indicated patient recovery after 8–12 days of initial symptoms, and then a new infection confirmed by a positive test, followed by a negative test that indicated recovery3. We documented the number and type of vaccines vs. SARS-COV 2. It is important to notice that vaccination and booster in Mexico were applied by age group and not by individualized risk factors. A detailed roster of symptoms (for example: fatigue, muscle pain, alopecia, concentration problems, cough, dyspnea, loss of taste, loss of smell, thoracic pain, abdominal pain, fever, arthritis, constipation, diarrhea, loss of weight, coagulation problems, numbness, skin problems, heart failure, heart attack, etc.) experienced during the COVID-19 infection period, including their duration, was documented. If the duration of a symptom lasted more than 4 weeks in any of the infections, it was considered that the subject had Long COVID. Additionally, participants provided information about the severity of their acute symptoms and clarified if they were treated ambulatorily or if they required inpatient hospitalization or admission to an ICU unit. Every patient had an individualized interview by a trained physician. The data was anonymized and uploaded to an electronic database for analysis.
Statistical methods
The researchers reviewed the quality control and the anonymization of the database. Normality assumption was evaluated with the Shapiro–Wilk test. Descriptive statistics such as mean, standard deviation, median, interquartile range, frequencies, and percentages were computed. We used the Chi-square test to compare the medical history of the patients and their relationship with developing Long COVID syndrome. Also, a Fisher’s exact test with a Monte Carlo approximation was used to see if there is any relation between the Long COVID syndrome presence and its symptoms with the patient’s vaccination status. A multivariable logistic regression model was used to assess the relationship between Long COVID and characteristics, including age, sex, history of allergies, BMI, blood type, number of reinfections and number of SARS-COV2 vaccines. A sample size of 750 patients was calculated, according to the primary aim, by using a logistic regression model through the G Power 3.1 The statistical analysis was performed con SPSS vs. 25. A p value < 0.05 was considered statistically significant. Missing values that occurred completely at random were handled using a complete case analysis approach.
Ethical approval
Ethics committee/local Institutional Review Board from Hospital Clinica Nova gave ethical approval. Reference 170102022-CNa-MIa-CI.
Data availability
Data are available upon reasonable request to the authors.
References
Vandenberg, O., Martiny, D., Rochas, O., Van Belkum, A. & Kozlakidis, Z. Considerations for diagnostic COVID-19 tests. Nat. Rev. Microbiol. 19, 171–183 (2021).
Ochani, R. et al. COVID-19 pandemic: From origins to outcomes. A comprehensive review of viral pathogenesis, clinical manifestations, diagnostic evaluation, and management. Infez. Med. 29, 20–36 (2021).
Sotoodeh Ghorbani, S. et al. Epidemiologic characteristics of cases with reinfection, recurrence, and hospital readmission due to COVID-19: A systematic review and meta-analysis. J. Med. Virol. 94, 44–53 (2022).
Fiolet, T., Kherabi, Y., MacDonald, C.-J., Ghosn, J. & Peiffer-Smadja, N. Comparing COVID-19 vaccines for their characteristics, efficacy and effectiveness against SARS-CoV-2 and variants of concern: A narrative review. Clin. Microbiol. Infect. 28, 202–221 (2022).
Rashedi, R., Samieefar, N., Masoumi, N., Mohseni, S. & Rezaei, N. COVID-19 vaccines mix-and-match: The concept, the efficacy and the doubts. J. Med. Virol. 94, 1294–1299 (2022).
Aiyegbusi, O. L. et al. Symptoms, complications and management of long COVID: A review. J. R. Soc. Med. 114, 428–442 (2021).
Crook, H., Raza, S., Nowell, J., Young, M. & Edison, P. Long covid—mechanisms, risk factors, and management. BMJ https://doi.org/10.1136/bmj.n1648 (2021).
Chen, C. et al. Global prevalence of post-coronavirus disease 2019 (COVID-19) condition or long COVID: A meta-analysis and systematic review. J. Infect. Dis. 226, 1593–1607 (2022).
Yong, S. J. Long COVID or post-COVID-19 syndrome: Putative pathophysiology, risk factors, and treatments. Infect. Dis. 53, 737–754 (2021).
Theoharides, T. C. Could SARS-CoV-2 spike protein be responsible for long-COVID syndrome?. Mol. Neurobiol. 59, 1850–1861 (2022).
Silva Andrade, B. et al. Long-COVID and post-COVID health complications: An up-to-date review on clinical conditions and their possible molecular mechanisms. Viruses 13, 700 (2021).
Ayoubkhani, D. et al. Trajectory of long covid symptoms after covid-19 vaccination: Community based cohort study. BMJ https://doi.org/10.1136/bmj-2021-069676 (2022).
Sivan, M., Greenhalgh, T., Milne, R. & Delaney, B. Are vaccines a potential treatment for long covid?. BMJ https://doi.org/10.1136/bmj.o988 (2022).
Harrison, S., Walters, B., Simmons, Z., Cook, M. & Clark, R. The effectiveness of vaccination against long COVID. 1–24 (2022).
Byambasuren, O., Stehlik, P., Clark, J., Alcorn, K. & Glasziou, P. Effect of covid-19 vaccination on long covid: Systematic review. BMJ Med. 2, e000385 (2023).
Azzolini, E. et al. Association between BNT162b2 vaccination and long COVID after infections not requiring hospitalization in health care workers. JAMA 328, 676–678 (2022).
Lopez-Leon, S. et al. More than 50 long-term effects of COVID-19: A systematic review and meta-analysis. Sci. Rep. 11, 16144 (2021).
Wong-Chew, R. M. et al. Symptom cluster analysis of long COVID-19 in patients discharged from the temporary COVID-19 hospital in Mexico City. Ther. Adv. Infect. Dis. 9, 204993612110692 (2022).
Abumayyaleh, M. et al. Post-COVID-19 syndrome and diabetes mellitus: A propensity-matched analysis of the International HOPE-II COVID-19 Registry. Front. Endocrinol. 14, 25 (2023).
Richard, S. A. et al. Persistent COVID-19 symptoms at 6 months after onset and the role of vaccination before or after SARS-CoV-2 infection. JAMA Netw. Open 6, e2251360 (2023).
Bowe, B., Xie, Y. & Al-Aly, Z. Acute and postacute sequelae associated with SARS-CoV-2 reinfection. Nat. Med. 28, 2398–2405 (2022).
Silva, K. M. et al. Prevalence and predictors of COVID-19 long-term symptoms: A cohort study from the Amazon Basin. Am. J. Trop. Med. Hyg. 109, 466–470 (2023).
Peghin, M. et al. Post-COVID-19 syndrome 2 years after the first wave: The role of humoral response, vaccination and reinfection. Open Forum Infect. Dis. 10, 364 (2023).
Bechmann, N. et al. Sexual dimorphism in COVID-19: Potential clinical and public health implications. Lancet Diabetes Endocrinol. 10, 221–230 (2022).
Abul, Y., Leeder, C. & Gravenstein, S. Epidemiology and clinical presentation of COVID-19 in older adults. Infect. Dis. Clin. North Am. 37, 1–26 (2023).
Fernando, S. M. et al. Association of extracorporeal membrane oxygenation with new mental health diagnoses in adult survivors of critical illness. JAMA 328, 1827 (2022).
von Elm, E. et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Ann. Intern. Med. 147, 573–577 (2007).
Acknowledgements
This project has been supported by the Techint Group of Companies.
Funding
This research was conducted using private funding from Techint Group of Companies. The funders had no role in study design, data collection, analysis, and decision to publish.
Author information
Authors and Affiliations
Contributions
Conceptualization: M.E.R.-I., E.A., M.A.S.S., and M.R. Formal analysis: J.F.R.T., M.E.R.I., A.G.-S., and A.R.C. Investigation: J.F.R.T., M.E.R.I., and A.G.S. Resources: M.E.R.I. Data acquisition: J.F.R.T., A.G.S., A.R.C., M.H.C., R.K.A., D.L.V.P., A.L.E., J.J.G.A., Y.G.M.P., D.A.O.S., D.P.M.R. Writing—original draft: J.F.R.T., M.E.R.I., and A.G.S. Writing—review and editing: M.E.R.I., E.A., A.G.C., and M.R. Project administration: J.F.R.T., M.E.R.I., M.A.S.S. Supervision: M.E.R.I. Funding acquisition: M.E.R.I., and M.R. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Romero-Ibarguengoitia, M.E., Rodríguez-Torres, J.F., Garza-Silva, A. et al. Association of vaccine status, reinfections, and risk factors with Long COVID syndrome. Sci Rep 14, 2817 (2024). https://doi.org/10.1038/s41598-024-52925-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-52925-4
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.