Abstract
The combined effect of obesity and metabolic abnormalities on liver injury is unclear. Aiming to address this knowledge gap, this cross-sectional study was conducted among 16,201 US adults. Multiple linear regression and logistic regression analyses were conducted to assess the associations of obesity profiles, metabolic health status, and weight change with the levels of liver enzymes. The analysis revealed that general obesity and abdominal obesity were positively associated with the levels of liver enzymes and the prevalence of abnormal liver enzymes (P and Ptrend < 0.05). The associations remained significant in both metabolically healthy and metabolically unhealthy subgroups. Additionally, the liver injury index levels of the metabolically unhealthy participants were higher than those of the metabolically healthy individuals within the non-obese, overweight/pre-abdominal obesity, and general/abdominal obesity subgroups (P and Ptrend < 0.05). Furthermore, the subgroup characterized by general/abdominal obesity and metabolic dysfunction exhibited the most robust association with the liver injury index compared to all other subgroups examined. In addition, positive associations were observed between the 1-year and 10-year weight changes and the levels of liver injury indicators (P and Ptrend < 0.05). In conclusion, this study demonstrates that both obesity and metabolic impairment are independently associated with liver injury, and their combined presence have an additional adverse effect on liver health. These findings underscore the importance of addressing both obesity and metabolic dysfunction in order to mitigate the risk of liver injury.
Similar content being viewed by others
Introduction
The liver is one of the main metabolic organs in the human body and participates in a series of important physiological functions, including the decomposition, synthesis, storage, and detoxification of compounds1. With the rapid progression of economic development and changes in lifestyle, liver disease has become a heavy health burden worldwide2. Deaths related to liver disease increased by 11.4% from 2012 to 2017, and accounts for approximately 2 million deaths each year3. Moreover, the number of years lived with disability due to liver disease also increased by 50.7% from 1990 to 2007, and by 34.8% from 2007 to 20174. Consequently, the burden of liver disease has attracted extensive attention. Alongside viral hepatitis and alcohol consumption, nonalcoholic fatty liver disease (NAFLD) has emerged as a rapidly growing contributor to liver mortality and morbidity3. It is the most prevalent liver disorder and major cause for elevated liver enzymes in Asia5.
In addition to viruses, alcohol consumption, nutritional factors, and chemical toxins6,7, the adverse effects of obesity and metabolic dysfunction on the liver have been partially understood. A retrospective study including 767 participants suggested that obesity severity was positively associated with liver disease severity8. Furthermore, a large-population study using Mendelian randomization showed that the two major subtypes of obesity, general and abdominal obesity, which can be measured by body mass index (BMI) and waist circumference (WC), respectively, were causal factors for NAFLD and chronic liver disease in 228,466 women and 195,041men9. When comparing general obesity with abdominal obesity, the latter exhibited a closer association with type 2 diabetes, hypertension, dyslipidemia, cardiovascular disease, cancer, and all-cause mortality10,11. Both general obesity and abdominal obesity have been identified to be associated with liver injury in previous studies12,13, nevertheless, few studies have compared the contributions of these two obesity phenotypes to liver injury.
In addition to obesity, metabolic disorders including insulin resistance, dyslipidemia, and hypertension are also risk factors for liver disease14,15,16. A cross-sectional study involving 236 Mexican children and adolescents found that the prevalence of metabolic syndrome was strongly associated with elevated liver enzyme levels17. Additionally, the causal effects of obesity traits and metabolic diseases, including type 2 diabetes mellitus (T2DM) and hypertension, on the risk of NAFLD has been identified by a Mendelian randomization study18. Interactions exit between obesity and metabolic disorders19. Obesity could induce metabolic dysfunctions, most likely by inflammatory mechanisms20,21. But individuals with obesity may have limited or no features of poor metabolic health, which is referred to as metabolically healthy obesity (MHO)22. Recent research suggests that MHO might be a transient state associated with long-term health complications, including an increased risk of heart failure23. Though both obesity and metabolic dysfunctions have been implicated in liver injury, further studies are needed to explore the combined effects of different obesity phenotype and metabolic health status on liver injury.
In this study, we conducted cross-sectional and retrospective analyses using data of general adults in the United States from the 1999–2016 survey cycles of the National Health and Nutrition Examination Survey (NHANES). Liver injury was assessed based on the levels of liver enzymes, including alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), gamma-glutamyl transferase (GGT), and the AST/ALT ratio. General obesity and abdominal obesity were assessed by BMI and WC, respectively. Metabolic health status was assessed by fasting serum triglyceride (TG), high-density lipoprotein cholesterol (HDL-C), systolic blood pressure (SBP), diastolic blood pressure (DBP), fasting blood glucose (FBG), and a general health questionnaire. The objectives of this study were to assess the associations of different obesity phenotypes and metabolic health status with liver injury, and to evaluate the combined effects of obesity and metabolically unhealthy status.
Materials and methods
Study population
The study participants were sourced from the NHANES, as detailed in existing studies24,25. Briefly, US civilians were recruited using a complex, multistage probability design, conducted by Centers for Disease Control and Prevention (CDC)’s National Center for Health Statistics (NCHS). Comprehensive data collection, including questionnaire interviews, physical examinations, and laboratory tests have been conducted biennially since 1999. The study protocol was approved by the NCHS Research Ethics Review Board, and all participants signed informed consent forms. All methods were performed in accordance with the relevant guidelines and regulations.
For the present analyses, the study focused on adults aged 20–85, utilizing data from NHANES cycles conducted between 1999 and 2016. This time frame was chosen due to inconsistencies observed in questionnaire content, specifically regarding alcohol consumption, which varied since 2017. Additionally, the potential influence of the COVID-19 pandemic starting in 2019 necessitated a focus on pre-pandemic data. After excluding participants without physical examinations or laboratory tests, pregnant individuals, and those infected with hepatitis B or C, a total of 16,201 participants was included in the cross-sectional analyses. Subsequently, after further exclusion of participants lacking retrospective weight data from 10 years ago, 11,677 participants were available for retrospective analyses. The dataset used for this analysis encompasses NHANES data from 1999 to 2016. The details of the program, collection procedures, and data files are publicly available at NHANES website https://www.cdc.gov/nchs/nhanes/.
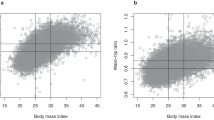
Assessment of obesity and metabolically healthy status
In NHANES, weight, height, and WC were measured by expert anthropometrists to the nearest 0.1 kg and 0.1 cm, respectively, and BMI was calculated by dividing weight (kg) by the squared of height (m2). In this study, non-general obesity was defined as BMI < 25.0 kg/m2, overweight was defined as 25.0 kg/m2 ≤ BMI < 30.0 kg/m2, and general obesity was defined as BMI ≥ 30.0 kg/m2. Non-abdominal obesity was defined as WC < 94.0 cm in men or < 80.0 cm in women, pre-abdominal obesity was defined as 94.0 cm ≤ WC < 102.0 cm in men or 80.0 cm ≤ WC < 88.0 cm in women, and abdominal obesity was defined as WC ≥ 102.0 cm in men or WC ≥ 88.0 cm in women26. In addition, 1-year and 10-year weight changes were calculated by subtracting the self-reported weights 1 and 10 years prior from the current weight.
In this study, metabolically healthy status was defined as: serum TG ≤ 1.7 mmol/L, HDL-C > 1.0 mmol/L in men or > 1.3 mmol/L in women, SBP ≤ 130 mmHg, DBP ≤ 85 mmHg, FBG ≤ 6.1 mmol/L, and no drug treatment for dyslipidemia, diabetes, or hypertension22. Otherwise, individuals were classified as metabolically unhealthy individuals.
Assessment of liver injury
In NHANES, liver enzymes, including ALT, AST, ALP, and GGT were measured during different cycles using specific analyzers. Specifically, the Hitachi Model 704 multichannel analyzer was employed during the 1999–2002 cycles, followed by the Beckman Synchron LX20 during the 2003–2006 cycles, and the Beckman UniCel® DxC800 Synchron during the 2007–2016 cycles, all measured by medical technologists. Rigorous quality control and assurance measures were implemented in compliance with the 1988 Clinical Laboratory Improvement Act. For values of liver enzymes falling below the lower detection limit, an adjustment was made by replacing them with a value equal to the detection limit divided by the square root of the two. In this study, abnormal liver enzymes were defined in line with prior research: ALT > 47.0 IU/L in men or > 30.0 in women, AST > 33.0 IU/L in men and women, ALP > 113.0 IU/L in men and women, GGT > 65.0 IU/L in men and > 36.0 IU/L in women27. In addition, the AST/ALT ratio, calculated by dividing AST by ALT, is also an important indicator of liver injury.
Assessment of covariates
In NHANES, demographic and lifestyle data, including age, gender, race, educational qualification, physical exercise, annual household income, smoking status, and alcohol consumption, were collected using standard questionnaires by trained investigators. In this study, race categories included Mexican Americans, other Hispanics, non-Hispanic whites, non-Hispanic blacks, and other races; educational qualifications were categorized as less than 9th grade, 9–11th grade, high school graduate, associate degree, and college graduate or above; physical exercise was divided into “yes” (defined as vigorous activities that caused heavy sweating or large increases in breathing or heart rate) and “no”; annual household income was divided into high (above the median for each cycle) and low; smoking status was divided into “yes” and “no”; and alcohol consumption was dichotomized as “yes” (drinking at least once a week over the past 12 months) and “no”.
Statistical analysis
In order to address their right-skewed distribution, the levels of liver enzymes and the AST/ALT ratio were subjected to a natural logarithmic transformation. Analysis of Variance, Kruskal–Wallis test, and chi-square test were used to compare the differences in basic characteristics among participants with different general obesity statuses or abdominal obesity statuses for symmetrically distributed variables, right-skewed distributed variables, and categorical variables, respectively. Multiple linear regression and logistic regression analyses were conducted to estimate the associations of general/abdominal obesity with liver enzyme levels as well as the prevalence of abnormal liver enzymes. Potential confounders such as age, gender, race, educational qualification, physical exercise, annual household income, smoking status, alcohol consumption, and batch (survey cycle) were included in the analysis and the results were adjusted for the aforementioned covariates. The percentage of R2 change in the regression analyses was calculated to compare the relative contributions of general obesity and abdominal obesity to adverse effects on liver injury. The participants were further stratified into six subgroups according to general/abdominal obesity status and metabolic health status to assess the combined effects of obesity and metabolic disorders on the liver, with the subgroup of non-general/abdominal obesity and metabolically healthy status as the reference. In retrospective analyses, the associations of 1-year and 10-year weight changes with the levels of liver enzymes and the prevalence of abnormal liver enzymes were evaluated using multiple linear regression and logistic regression analyses.
All P values were two-sided with a statistical significance level of 0.05, and survey-weighted multiple linear and logistical regression analyses were performed with R software (version 4.2.0, R Foundation for Statistical Computing, Austria).
Results
Basic characteristics
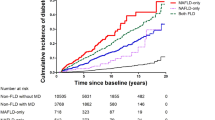
As presented in Table 1, the mean age of 16,201 participants was 49.6 (standard deviation, 17.8) years, with 8119 (50.1%) being male. Participants were categorized into two main groups based on major subtypes of obesity: general obesity and abdominal obesity, which were determined by BMI and WC, respectively. Within the general obesity group, the proportions for non-general obesity, overweight, and general obesity subgroups were 31.1%, 34.5%, and 34.4%, respectively. Within the abdominal obesity group, the proportions for non-abdominal, pre-abdominal, and abdominal obesity subgroups were 25.2%, 20.5%, and 54.2%, respectively. Smoking and drinking rates were 17.1% and 42.2%, respectively. Abnormal ALT, AST, ALP, or GGT were observed in less than 10% of the population, while over 70% of the participants were metabolically unhealthy. Ratios of participants with abnormal liver enzyme levels and unhealthy metabolism increased with the degree of obesity, while AST/ALT decreased (all P < 0.05). These trends were observed in both general obesity and abdominal obesity.
Associations of general obesity and abdominal obesity with liver injury
The associations of general obesity with liver enzyme levels as well as the prevalence of abnormal liver enzymes are presented in Table 2. After adjusting for potential covariates, the levels of ALT, AST, ALP, and GGT significantly increased as degrees of general obesity increased, while the AST/ALT ratio decreased significantly (all P and Ptrend < 0.05). With the non-general obesity subgroup as a reference, the levels of ALT, AST, ALP, and GGT in the general obesity subgroup increased by 26.2% (24.0%, 28.4%), 3.4% (1.8%, 5.0%), 10.0% (8.5%, 11.5%), and 34.7% (32.0%, 37.3%), respectively. A similar trend was also observed for the presence of abnormal liver enzymes. General obesity was positively associated with liver enzyme levels as well as the presence of abnormal liver test (all Ptrend < 0.05).
As shown in Table 3, the levels of ALT, AST, ALP, and GGT as well as the prevalence of abdominal liver enzymes increased significantly from non-abdominal obesity to pre-abdominal obesity and finally to abdominal obesity (all Ptrend < 0.05).
Comparing with abdominal obesity, general obesity had a greater contribution to the effect of ALT (35.7% vs 30.3%), AST (2.4% vs 1.2%), GGT (38.0% vs 30.6%), and AST/ALT (73.9% vs 66.9%) levels, as well as the prevalence of abnormal ALT (147.3% vs 141.0%), abnormal AST (20.8% vs 9.1%), and abnormal GGT (44.1% vs 33.9%). However, it had a lower contribution to the level of ALP (16.8% vs 21.4%) and the prevalence of abnormal ALP (4.3% vs 6.9%).
Combined associations of obesity and metabolically unhealthy status with liver injury
The combined effects of general obesity and metabolically unhealthy status on liver injury are presented in Table 4. With the subgroup characterized by non-general obesity and metabolically healthy status as a reference, the ALT levels of the other five subgroups were significantly increased (all P < 0.05), with the subgroup characterized by general obesity and metabolically unhealthiness having the greatest effect. Similar results were observed in the analyses of other liver enzyme levels and the prevalence of abnormal liver enzymes, whereas the AST/ALT ratio was the lowest in the subgroup characterized by general obesity and metabolically unhealthiness compared to the other subgroups. Additionally, whether in the metabolically healthy subgroup or the metabolically unhealthy subgroup, the levels of ALT, ALP, and GGT, as well as the prevalence of abnormal ALT and GGT were significantly increased from non-general obesity to overweight and finally to general obesity (all Pa < 0.05). On the other hand, regardless of being in the non-general obesity, the overweight, or the general obesity subgroup, the levels of ALT, ALP, and GGT, as well as the prevalence of abnormal ALT and GGT in the metabolically unhealthy subgroup were higher than that in metabolically healthy subgroup (all Pb < 0.05). The combined effect of abdominal obesity and being metabolically unhealthy on the liver injury was consistent with the above results (Table 5).
The effect of weight change on liver injury in retrospective analysis
Table 6 reveals that 1-year and 10-year weight changes were significantly associated with liver enzyme levels as well as the prevalence of abnormal liver enzymes. Each 1-kg increase in 1-year weight change was associated with increased levels of ALT, AST, ALP, and GGT by 0.53% (0.42%, 0.65%), 0.18% (0.09%, 0.27%), 0.14% (0.06%, 0.23%), and 0.39% (0.24%, 0.54%), respectively. Moreover, it was associated with a heightened risk of abnormal ALT and AST by 3.2% (2.2%, 4.2%) and 1.5% (0.5%, 2.5%), respectively. Meanwhile, the estimated changes of ALT, AST, ALP, and GGT levels, along with the risk of abnormal ALT and AST significantly increased with the elevated quartiles of 1-year weight change (Ptrend < 0.05). In contrast, 1-year weight change was negatively associated with the AST/ALT ratio (P and Ptrend < 0.05). Similarly, each 1-kg increase in 10-year weight change was associated with increased levels of ALT, AST, ALP, and GGT by 0.54% (0.46%, 0.62%), 0.11% (0.05%, 0.17%), 0.18% (0.12%, 0.25%), and 0.71% (0.59%, 0.82%), respectively, as well as increased risk of abnormal ALT, AST, and GGT by 3.2% (2.5%, 3.9%), 1.5% (0.7%, 2.3%), and 1.9% (1.3%, 2.6%), respectively. With the increasing quartiles of 10-year weight change, the levels of ALT, AST, ALP, and GGT, as well as the prevalence of abnormal ALT, AST, and GGT gradually increased (Ptrend < 0.05).
Discussion
In the present study, we found that both general obesity and abdominal obesity were positively associated with the indicators of liver injury, with general obesity having a higher contribution. Metabolic abnormalities and obesity had a combined effect on liver injury. Both short-term and long-term weight gain/loss were associated with increased/decreased risk of liver injury.
We used liver enzyme levels as indicators of liver injury. As obtaining liver biopsy is nearly impossible in large-scale general population-based epidemiological studies, blood biomarkers are commonly used. It is noteworthy that liver enzymes, even when released by a small proportion of damaged hepatocytes, can lead to a substantial elevation in serum liver enzyme levels. Consequently, according to the clinical guidelines established by the American College of Gastroenterology (ACG), these enzymes should be considered as indicators of liver injury28,29. Previous studies have commonly employed ALT, AST, ALP, and GGT as markers to evaluate liver injury30,31.
Obesity is a recognized risk factor for liver injury. Liver injuries, including NAFLD, can be caused by excessive fat accumulation, which induces an oversupply of fatty acids in the liver, hepatocyte injury, and chronic low-grade inflammation32,33. BMI is the most widely used crude measure of general obesity. Compared with BMI, waist circumference is strongly associated with abdominal fat distribution and is a better index for abdominal obesity. Dose–response analysis suggested that higher BMI is an independent and dose-dependent risk factor for fatty liver34. Population-based study found that WC to be independently associated with liver disease35. These studies suggest that both general obesity and abdominal obesity pose a risk for liver injury. Although previous studies have suggested that WC may be more strongly associated with an elevated risk of liver cancer compared to BMI11, the contribution of the two obesity types to liver injury has rarely been reported. Our study, on the other hand, found that general obesity had a larger impact on the association with liver enzyme levels and the prevalence of abnormal liver enzymes compared to abdominal obesity. Nonetheless, it is important to note that further validation of these findings is warranted through larger prospective studies.
Metabolic disorders, including insulin resistance, dyslipidemia, and hypertension, are important driving factors on liver injury. Insulin resistance is often associated with chronic low-grade inflammation and abnormal fat metabolism, which leads to the release of numerous molecular mediators from immune cells and adipocytes, and ultimately contributes to liver injury, liver disease progression, and liver repair disorders36,37. Hypertension may induce liver injury and hepatic fibrosis through decreased interleukin-10-mediated or heme oxygenase-1-induced anti-inflammatory mechanisms38. Although obesity is usually associated with metabolic disorders, it is possible for obese individuals to be metabolically healthy. A large cohort study of metabolically healthy population suggested that obesity was strongly and progressively associated with an increased incidence of NAFLD39, indicating that obesity is an independent risk factor for liver injury. In our study, we found that obesity and metabolic health status are independent of each other in the associations with liver enzyme levels and abnormal liver enzyme, furthermore, they had combined effects on liver injury.
Existing evidence indicates that weight gain is an important risk factor for liver injury in general population, and weight loss has shown potential to ameliorate liver injury. A randomized controlled trial showed that weight loss through diet significantly reduced the levels of liver enzymes, including ALT and GGT40. In our study, we investigated the effect of weight change on liver injury parameters and found that both short- and long-term weight change were associated altered risk for liver injury, with weight gain associated with increased risk and weight loss associated with lower risk. Our findings are consistent with previous studies.
The present study utilized data from a large population and analyzed association of different obesity phenotypes as well as and metabolic health status with indicators of liver injury. Our findings provide new insights into the complicated interactions between obesity, metabolism and the risk of liver injury. Nevertheless, there are some limitations in our study. Firstly, it is a cross-sectional association study, and a causal effect of these risk factors still needs to be confirmed in prospective cohort studies. Secondly, even if some covariates were adjusted in our statistical analyses, other variables such as genes that are associated with outcome variables were not available in NHANES datasets. Finally, it should be noted that liver enzymes have a relatively short half-life in the systemic circulation, typically spanning only a few days. Therefore, in order to obtain a more accurate representation of liver injury, it is recommended to perform liver chemical examinations on at least two occasions, with a minimum interval of six months between each assessment41,42.
Conclusion
In the present study, we analyzed a large population dataset and established that both obesity and metabolic health status act as independent risk factors for liver injury. Moreover, these factors exhibit combined effects, further exacerbating the risk. Additionally, our findings revealed a positive association between weight fluctuations and the likelihood of developing liver injury. These results underscore the urgent necessity for increased focus on liver health among adults with metabolically unhealthy obesity and emphasize the significance of weight loss interventions in improving liver injury outcomes.
Data availability
The datasets analysed during the current study are available at NHANES website https://www.cdc.gov/nchs/nhanes/.
References
Trefts, E., Gannon, M. & Wasserman, D. H. The liver. Curr. Biol. 27(21), R1147–R1151 (2017).
Xiao, J. et al. Global liver disease burdens and research trends: Analysis from a Chinese perspective. J. Hepatol. 71(1), 212–221 (2019).
Paik, J. M., Golabi, P., Younossi, Y., Mishra, A. & Younossi, Z. M. Changes in the global burden of chronic liver diseases from 2012 to 2017: The growing impact of NAFLD. Hepatology 72(5), 1605–1616 (2020).
Collaborators GDaIIaP. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 392(10159), 1789–1858 (2018).
Zhou, J. et al. Epidemiological features of NAFLD from 1999 to 2018 in China. Hepatology 71(5), 1851–1864 (2020).
Wang, X. et al. Systemic inflammation mediates the association of heavy metal exposures with liver injury: A study in general Chinese urban adults. J. Hazard Mater. 419, 126497 (2021).
Wang, X. et al. Lipid peroxidation mediates the association between iron overload and liver injury: Cross-sectional and longitudinal analyses in general Chinese urban adults. Environ. Sci. Pollut. Res. Int. 30(1), 60343–60353 (2023).
Seth, A. et al. Severe obesity is associated with liver disease severity in pediatric non-alcoholic fatty liver disease. Pediatr. Obes. 15(2), e12581 (2020).
Censin, J. C. et al. Causal relationships between obesity and the leading causes of death in women and men. PLoS Genet. 15(10), e1008405 (2019).
Xi, B. et al. Secular trends in the prevalence of general and abdominal obesity among Chinese adults, 1993–2009. Obes. Rev. 13(3), 287–296 (2012).
Rahmani, J. et al. Waist circumference and risk of liver cancer: A systematic review and meta-analysis of over 2 million cohort study participants. Liver Cancer 9(1), 6–14 (2020).
Ali, N. et al. Assessment of the relationship of serum liver enzymes activity with general and abdominal obesity in an urban Bangladeshi population. Sci. Rep. 11(1), 6640 (2021).
Johansen, M. J. et al. The effect of overweight and obesity on liver biochemical markers in children and adolescents. J. Clin. Endocrinol. Metab. 105(2), dgz010 (2020).
Katsiki, N., Mikhailidis, D. P. & Mantzoros, C. S. Non-alcoholic fatty liver disease and dyslipidemia: An update. Metabolism 65(8), 1109–1123 (2016).
Heeren, J. & Scheja, L. Metabolic-associated fatty liver disease and lipoprotein metabolism. Mol. Metab. 50, 101238 (2021).
Åberg, F. et al. Association between arterial hypertension and liver outcomes using polygenic risk scores: A population-based study. Sci. Rep. 12(1), 15581 (2022).
Elizondo-Montemayor, L. et al. Association of ALT and the metabolic syndrome among Mexican children. Obes. Res. Clin. Pract. 8(1), e79–e87 (2014).
Xie, J. et al. The associations between modifiable risk factors and nonalcoholic fatty liver disease: A comprehensive Mendelian randomization study. Hepatology 77(3), 949–964 (2023).
Liu, Y. et al. Relationship between obesity severity, metabolic status and cardiovascular disease in obese adults. Eur. J. Clin. Invest. 53(3), e13912 (2023).
Jung, U. J. & Choi, M.-S. Obesity and its metabolic complications: The role of adipokines and the relationship between obesity, inflammation, insulin resistance, dyslipidemia and nonalcoholic fatty liver disease. Int. J. Mol. Sci. 15(4), 6184–6223 (2014).
Saltiel, A. R. & Olefsky, J. M. Inflammatory mechanisms linking obesity and metabolic disease. J. Clin. Invest. 127(1), 1–4 (2017).
Blüher, M. Metabolically healthy obesity. Endocr. Rev. 41(3), bnna004 (2020).
Commodore-Mensah, Y. et al. High burden of subclinical and cardiovascular disease risk in adults with metabolically healthy obesity: The atherosclerosis risk in communities (ARIC) study. Diabetes Care 44(7), 1657–1663 (2021).
Yu, L. et al. Associations between urinary phthalate metabolite concentrations and markers of liver injury in the US adult population. Environ. Int. 155, 106608 (2021).
Chen, C., Ye, Y., Zhang, Y., Pan, X.-F. & Pan, A. Weight change across adulthood in relation to all cause and cause specific mortality: Prospective cohort study. BMJ 367, l5584 (2019).
Larsson, S. C., Wolk, A., Håkansson, N. & Bäck, M. Overall and abdominal obesity and incident aortic valve stenosis: Two prospective cohort studies. Eur. Heart J. 38(28), 2192–2197 (2017).
Xiao, Q., Sinha, R., Graubard, B. I. & Freedman, N. D. Inverse associations of total and decaffeinated coffee with liver enzyme levels in National Health and Nutrition Examination Survey 1999–2010. Hepatology 60(6), 2091–2098 (2014).
Kwo, P. Y., Cohen, S. M. & Lim, J. K. ACG clinical guideline: Evaluation of abnormal liver chemistries. Am. J. Gastroenterol. 112(1), 18–35 (2017).
Kim, W. R., Flamm, S. L., Di Bisceglie, A. M. & Bodenheimer, H. C. Serum activity of alanine aminotransferase (ALT) as an indicator of health and disease. Hepatology 47(4), 1363–1370 (2008).
Carter, A. R. et al. Combined association of body mass index and alcohol consumption with biomarkers for liver injury and incidence of liver disease: A Mendelian randomization study. JAMA Netw. Open. 2(3), e190305 (2019).
Ayonrinde, O. T. et al. Gender-specific differences in adipose distribution and adipocytokines influence adolescent nonalcoholic fatty liver disease. Hepatology 53(3), 800–809 (2011).
Brunt, E. M. et al. Nonalcoholic fatty liver disease. Nat. Rev. Dis. Primers. 1, 15080 (2015).
Milić, S., Lulić, D. & Štimac, D. Non-alcoholic fatty liver disease and obesity: Biochemical, metabolic and clinical presentations. World J. Gastroenterol. 20(28), 9330–9337 (2014).
Fan, R., Wang, J. & Du, J. Association between body mass index and fatty liver risk: A dose-response analysis. Sci. Rep. 8(1), 15273 (2018).
Danielsson, O. et al. Waist and hip circumference are independently associated with the risk of liver disease in population-based studies. Liver Int. 41(12), 2903–2913 (2021).
Manzano-Núñez, F. et al. Insulin resistance disrupts epithelial repair and niche-progenitor Fgf signaling during chronic liver injury. PLoS Biol. 17(1), e2006972 (2019).
Bugianesi, E., Moscatiello, S., Ciaravella, M. F. & Marchesini, G. Insulin resistance in nonalcoholic fatty liver disease. Curr. Pharm. Des. 16(17), 1941–1951 (2010).
Arima, S. et al. Hypertension exacerbates liver injury and hepatic fibrosis induced by a choline-deficient L-amino acid-defined diet in rats. Int. J. Mol. Med. 33(1), 68–76 (2014).
Chang, Y. et al. Metabolically healthy obesity and the development of nonalcoholic fatty liver disease. Am. J. Gastroenterol. 111(8), 1133–1140 (2016).
Straznicky, N. E. et al. The effects of dietary weight loss with or without exercise training on liver enzymes in obese metabolic syndrome subjects. Diabetes Obes. Metab. 14(2), 139–148 (2012).
Lazo, M., Selvin, E. & Clark, J. M. Brief communication: Clinical implications of short-term variability in liver function test results. Ann. Intern. Med. 148(5), 348–352 (2008).
Husain, N. et al. Nonalcoholic fatty liver disease (NAFLD) in the Veterans Administration population: Development and validation of an algorithm for NAFLD using automated data. Aliment Pharmacol. Ther. 40(8), 949–954 (2014).
Acknowledgements
All participants included in this study and all members of CDC’s NCHS are greatly acknowledged.
Funding
This study was supported by the General Project of Key Research and Development Plan of Shaanxi (Grant Number: 2023YBSF424) and the “Phoenix Introduction Plan” Project of Tangdu Hospital, Air Force Military Medical University (Grant Number: 2022YFJH007). Funders had no role in study design, data collection, or data interpretation.
Author information
Authors and Affiliations
Contributions
J.H.: Conceptualization, Methodology, Resources, Validation, Writing—review & editing, Supervision. T.G.: Conceptualization, Methodology, Writing—review & editing. H.Z.: Conceptualization, Methodology, Writing—review & editing. X.W.: Conceptualization, Methodology, Formal analysis, Resources, Validation, Writing—original draft, Writing—review & editing, Supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huang, J., Gao, T., Zhang, H. et al. Association of obesity profiles and metabolic health status with liver injury among US adult population in NHANES 1999–2016. Sci Rep 13, 15958 (2023). https://doi.org/10.1038/s41598-023-43028-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-43028-7
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.