Abstract
It has been suggested that brain inflammation is important in aggravation of brain damage and/or that inflammation causes neurodegenerative diseases including Parkinson's disease (PD). Recently, systemic inflammation has also emerged as a risk factor for PD. In the present study, we evaluated how systemic inflammation induced by intravenous (iv) lipopolysaccharides (LPS) injection affected brain inflammation and neuronal damage in the rat. Interestingly, almost all brain inflammatory responses, including morphological activation of microglia, neutrophil infiltration, and mRNA/protein expression of inflammatory mediators, appeared within 4-8 h, and subsided within 1-3 days, in the substantia nigra (SN), where dopaminergic neurons are located. More importantly, however, dopaminergic neuronal loss was not detectable for up to 8 d after iv LPS injection. Together, these results indicate that acute induction of systemic inflammation causes brain inflammation, but this is not sufficiently toxic to induce neuronal injury.
Similar content being viewed by others
Introduction
Parkinson's disease (PD) is the second most common neurodegenerative disorder and is characterized by degeneration of dopaminergic neurons in the substantia nigra pars compacta (SNpc), resulting in movement disorder (Gelb et al., 1999). However, as most (90-95%) cases of PD are sporadic in nature, it remains unclear how PD occurs and progresses. Mutations in genes such as those encoding α-synuclein, parkin, PINK1, DJ-1, LRRK2, and Htra2 are found in familial PD patients (Klein et al., 2005; Klein and Schlossmacher, 2006; Thomas and Beal, 2007). However, animals carrying mutations in or knock-outs of these PD-related genes rarely show PD-like symptoms or dopaminergic neuronal loss (Rockenstein et al., 2002; Goldberg et al., 2003; Itier et al., 2003; Von Coelln et al., 2004; Chen et al., 2005b; Zhu et al., 2007). These findings indicate that abnormal functioning of PD-related genes is not enough to cause PD. Thus, certain microenvironmental factors such as brain inflammation have been suggested as important in causation and/or aggravation of neurodegenerative diseases includeing PD (Herrera et al., 2000; Gao et al., 2002). In PD brains, the expression levels of proinflammatory cytokines are higher than in control brains (Mogi et al., 1994; Blum-Degen et al., 1995; Muller et al., 1998; Knott et al., 2000; Nagatsu and Sawada, 2005; Whitton, 2007). Microglia (brain macrophages) are activated in post-mortem PD brains (McGeer et al., 1988; Croisier et al., 2005) and many experimental models of PD (Liberatore et al., 1999; Dehmer et al., 2000; Cicchetti et al., 2002; Wu et al., 2002; Sriram et al., 2006; Vijitruth et al., 2006). It has been suggested that nonsteroidal anti-inflammatory drug (NSAID) use reduces the incidence of PD (Chen et al., 2003; Esposito et al., 2007; Samii et al., 2009), although this contention remains controversial (Chen et al., 2005a; Etminan et al., 2008).
Brain damage induces brain inflammation. Microglia, known to be the principal inflammatory cells in the brain, continuously survey the environment of the normal brain and rapidly respond to damage, producing inflammatory mediators (Kreutzberg, 1996; Raivich et al., 1999; Min et al., 2004; Davalos et al., 2005; Hanisch and Kettenmann, 2007). Systemic inflammation may also induce brain inflammation. Systemically administered LPS may act on endothelial cells in the brain, in turn affecting adjacent microglia (Cao et al., 1999; Inoue et al., 2002; Rummel et al., 2008; Saper, 2010). In addition, inflammatory cells of the bloodstream, activated by systemically administered LPS, may enter the brain and participate in inflammation (Bohatschek et al., 2001; Cunningham et al., 2005; Qin et al., 2007). However, it is not clear whether systemic inflammation induces a level of brain inflammation sufficiently intense to cause neuronal damage. Cultured microglia challenged with LPS and interferon-γ produce neurotoxic inflammatory mediators including inducible nitric oxide synthase (iNOS) (Liu et al., 2000; Possel et al., 2000; Min et al., 2006), whereas microglia activated in vivo by brain injury and/or LPS injection synthesize very little iNOS and are not neurotoxic (Ji et al., 2007; Matsumoto et al., 2007). In the present study, we investigated how systemic inflammation affected brain inflammation, and whether such inflammation caused neuronal toxicity.
Results
Behavior of microglia and astrocytes in response to systemic administration of LPS
To investigate how systemic inflammation (SI) influenced the brain, we first examined the behavior of microglia and astrocytes after systemic administration of LPS. We focused on the SN region because inflammation in this area has been suggested as a risk factor for degeneration of dopaminergic neurons, resulting in PD. When 100 and 500 µg amounts of LPS in 250 µl PBS were intravenously (iv) injected into rats weighing 230-250 g, the TNF-α level in plasma increased sharply within 1 h, but decreased rapidly to the basal level by 3 h, as previously described (Liaudet et al., 2002; Chow et al., 2005; Qin et al., 2007). There was no significant difference in tumor necrosis factor-alpha (TNF-α) levels after injection of 100 and 500 µg LPS (Supplemental Data Figure S1), and we thus used 250 or 500 µg LPS in various experiments. In PBS-treated control animals, ionized calcium binding adaptor molecule 1-immunopositive (Iba-1+) microglia showed a ramified morphology (Figure 1A). Microglial cell density in the substantia nigra reticulate (SNr), where dopaminergic neuronal processes are located, was higher than that in the SNpc, as previously reported (Ji et al., 2007). The processes of Iba-1+ microglia became slightly shorter and thicker 8 h after iv LPS injection, and these features were more prominent in the SNpc than in the SNr. By 24 h post-injection, morphology had returned to normal (Figure 1A).
Behavior of microglia and astrocytes in response to iv LPS administration. Rats were injected iv with LPS (250 µg) dissolved in 250 µl PBS, or with PBS alone. At the indicated times after injection, brains were removed and prepared for immunohistochemistry as described in Methods. Midbrain sections (30 µm in thickness) were stained with anti-Iba-1 (A) or anti-GFAP antibody (B), and expression of Iba-1 or GFAP was visualized using peroxidase-conjugated secondary antibodies. Scale bars: 200 µm in the two left columns; 20 µm in the two right columns.
Astrocyte behavior was also examined in rat brains after induction of SI. Astrocyte density in the SNpc was much lower than in the SNr (Figure 1B). In contrast to what was noted when microglia were studied, there was no dramatic change in either morphology or astrocyte number in either region after iv LPS injection (Figure 1B). These results indicate that systemic LPS administration rapidly (within 8 h) induces brain inflammation, particularly microglial responses.
Neutrophils infiltrate the brain in response to systemic administration of LPS
Neutrophils are recruited to LPS-injected, traumatic, and ischemic brains, and the inflammatory responses are neurotoxic (Ji et al., 2007; Matsumoto et al., 2007). Thus, we examined the neutrophil infiltration pattern of the brain in response to iv LPS injection. To this end, brain sections were stained for a marker of neutrophils, myeloperoxidase (MPO). In the SN, MPO+ cells (arrows) were barely detectable within 4 h of LPS injection, increased in number at 8 h, and decreased in level at 16-24 h (Figure 2A). However, fewer neutrophils infiltrated the brain after iv LPS injection compared with the numbers seen after direct intranigral infusion of LPS (Figure 2A). We also investigated whether the SN was more permeable to neutrophils than were other brain regions, and found that neutrophils appeared to infiltrate the SN and the cortex to similar extents (Figure 2B). These results indicate that the SN is not particularly prone to infiltration of neutrophils during systemic inflammation.
Neutrophils infiltrate the brain in response to iv LPS administration. (A) Sections were obtained from the midbrain at the indicated times after LPS injection (LPS iv), or 24 h after direct LPS injection into the SN (LPS SNpc), and stained with an anti-MPO antibody. PBS-injected brain sections were used as positive controls. (B) Brain sections were obtained from the midbrain and the cortex 8 h after iv LPS injection, stained with an anti-MPO antibody, and MPOexpression was visualized using a peroxidase-conjugated secondary antibody. Scale bars: 200 µm (left panels in B); 50 µm (A and right panel of each region in B); and 10 µm (inset in A).
Expression of proinflammatory mediators in response to systemic administration of LPS
Next, in the SN, we examined expression of mRNAs encoding proinflammatory mediators such as interleukin-1 beta (IL-1β, TNF-α, and interleukin-6 (IL-6), in response to systemic administration of LPS, using real-time quantitative polymerase chain reaction (Q-PCR). All tested mRNA levels increased within 4 h after iv LPS injection, peaked at 8 h, and then to close to (or slightly greater than) basal levels (Figure 3A).
Expression of proinflammatory mediators in the brain in response to iv LPS injection. (A) mRNA was isolated from the midbrain regions of rats at the indicated times after iv LPS injection, and the levels of mRNAs encoding IL-1β, TNF-α, and IL-6 were analyzed by Q-PCR. Values are means ± SEMs of data from 3-5 animals. *P < 0.05; **P < 0.01, compared to intact brain. (B, C) Sections were obtained from the midbrain at the indicated times after LPS or PBS injection, and stained with antibodies detecting IL-1β, CD68, or iNOS; peroxidase-conjugated secondary antibodies (B) or double-labeled antibody combinations (C) were used to visualize binding. Midbrain sections of brains from animals injected iv with LPS were obtained at the indicated times and stained with the combinations of antibodies shown. Scale bars: 50 µm (upper panels in B); 20 µm (inset in the upper panel, and the lower panels in B); and 10 µm (C).
Upon immunohistochemical analysis, IL-1β expression was barely detectable 4 h after LPS administration, increased at 8-16 h, decreased at 24 h, and completely disappeared by 3 d (Figure 3B). We also investigated the expression of iNOS catalyzing nitric oxide production (Bogdan, 2001; Aktan, 2004), and cluster of differentiation 68 (CD68) representing phagocytic status (da Silva and Gordon, 1999; Nerlich et al., 2002; Rezaie et al., 2005). In contrast to what was seen when IL-1β expression was studied, only a limited number of cells expressed iNOS and CD68 (Figure 3B). Interestingly, IL-1β was detected in Iba-1+ but not in MPO+ cells, whereas iNOS and CD68 were detected in MPO+ but not in Iba-1+ cells (Figure 3C). Together, these results indicate that systemic inflammation induced transient expression of proinflammatory mediators, and that microglia and neutrophils synthesized different subsets of such mediators.
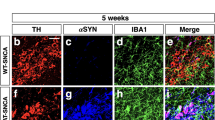
Effect of systemic administration of LPS on dopaminergic neuronal viability
Although iv LPS injection induced brain inflammation, such inflammation was transient and relatively mild compared with that seen after direct injection of LPS into the brain (Ji et al., 2007). Thus, we examined whether systemic inflammation induced dopaminergic neuronal injury. In PBS-injected rats, dopaminergic neurons was unaffected (Figure 4A). In LPS-injected rats, dopaminergic neuronal loss was not detectable for up to 8 d after LPS administration (Figure 4A). Upon stereological counting, the numbers of dopaminergic neurons did not differ significantly after injection of PBS (15,100 ± 1,754 cells, mean ± SEM) or LPS (15,900 ± 2,587 cells, mean ± SEM) (Figure 4B, P > 0.05). Together, these results indicate that, although acute systemic inflammation indeed induces brain inflammation, the effect is mild and does not cause neuronal injury.
LPS administration iv does not influence dopaminergic neuronal viability. (A) Midbrain sections of animals receiving LPS or PBS iv were obtained at 8 d, and stained with an anti-TH antibody. Scale bars: 200 µm (left panels) and 50 µm (right panels). (B) By stereology, the total numbers of TH+ neurons were estimated in the SNpc of LPS- or PBS-injected rats, as described in Methods. Values are means ± SEMs of data from three animals.
Discussion
It has been suggested that systemic inflammation may affect both the onset and progression of chronic brain diseases including PD and Alzheimer's disease, by induction of brain inflammation (Breitner, 1996; in 't Veld et al., 2002; Chen et al., 2003; Klegeris and McGeer, 2005; Esposito et al., 2007; Perry et al., 2007; Samii et al., 2009). The results of the present study show that iv LPS injection indeed induced brain inflammation. Microglia became morphologically activated; neutrophils infiltrated the brain; and inflammatory mediators, including IL-1β, TNF-α, IL-6, iNOS, and CD68, were synthesized (Figure 1-3). However, no neuronal death was evident (Figure 4). These results indicate that systemic inflammation indeed causes brain inflammation, but to only a mild extent and does not result in neuronal death.
The extent of neutrophil infiltration may significantly influence the level of neuronal death in an injured brain. Neutrophils are a major source of proinflammatory mediators including iNOS, Cyclooxygenase-2, Monocyte chemotactic protein-1, which play important roles in neuronal death within LPS-injected and/or ischemic brains (Ji et al., 2007; Matsumoto et al., 2007). Previously, we found that direct injection of LPS recruited more neutrophils to the SN than to the cortex or hippocampus, which suggests that susceptibility to LPS neurotoxicity may differ among these regions (Figure 2B LPS SN; Ji et al., 2008). LPS iv injection recruited fewer neutrophils than did direct LPS injection (Figure 2B), and induced only transient expression of inflammatory mediators, lasting for up to 1-3 d (Figure 1-3). Previously, it was reported that a single intraperitoneal LPS injection increased TNF-α mRNA and protein expression levels in the brain for more than 10 months (Qin et al., 2007). Although we did not analyze the expression levels of inflammatory mediators at such late timepoints, it may be difficult to re-stimulate inflammatory responses after they subside, in the absence of a challenge, for several reasons. First, cerebrospinal fluid is renewed about 11 times daily in adult rats and maintains homeostasis of the brain environment (Johanson et al., 2008). Second, neutrophils of the brain, the major source of proinflammatory mediators, die 1-5 days after LPS intranigral injection, reflecting an early response to damage (Ji et al., 2007). Third, The suppressor of cytokine signaling family proteins and antioxidant enzymes that resolve inflammation processes are activated to prevent long-lasting inflammation (Camhi et al., 1995; Ji et al., 2004). Therefore, acute brain inflammation may not last for months in the absence of a fresh trigger.
Intriguingly, microglia studied in vivo expressed very low levels (if any) of neurotoxic inflammatory mediators including iNOS (Ji et al., 2007; Matsumoto et al., 2007), although microglia in pure culture synthesized high amounts of iNOS and TNF-α (Chao et al., 1992; Meda et al., 1995). This difference in inflammatory response in vitro and in vivo may reflect an influence of astrocytes, which inhibit microglial activities (Vincent et al., 1997; Pyo et al., 2003; Min et al., 2006). Dehydroepiandrosterone (DHEA) and prostaglandins are candidate anti-inflammatory factors secreted by astrocytes (Zwain and Yen, 1999; Molina-Holgado et al., 2000; Taniura et al., 2002). DHEA inhibits the activation of nuclear factor-kappaB (NF-κB) induced by TNF-α (Altman et al., 2008) whereas prostaglandin E2 decreases Akt activation and the nuclear translocation of NF-κB (Shi et al., 2010). Astrocytes remained healthy in the brains of animals injected iv with LPS (Figure 1B), and possibly secreted anti-inflammatory factors suppressing microglial expression of inflammatory mediators. In addition, activated microglia produce neurotrophic factors such as transforming growth factor-β1, neurotrophin-3, and brain-derived neurotrophic factor (Elkabes et al., 1996; Lehrmann et al., 1998; Batchelor et al., 1999; Streit, 2002; Streit, 2005). Furthermore, not all inflammatory mediators produced in the brain are neurotoxic. For example, the effect of IL-1β on neuronal viability is controversial; the material has been suggested to be neurotoxic (Patel et al., 2003; Viviani et al., 2003; Thornton et al., 2006) or neurotrophic/neuroprotective (Strijbos and Rothwell, 1995).
Although systemic inflammation alone does not induce dopaminergic neuronal injury in the SNpc, we cannot exclude the possibility that systemic inflammation may yet be a risk factor for development of neurodegenerative disease. Systemic inflammation may convert a subtoxic insult to toxicity, and/or mild toxicity to potent toxicity. Although parkin-deficient mice do not display degeneration of dopaminergic neurons in the SNpc (Goldberg et al., 2003; Itier et al., 2003; Von Coelln et al., 2004; Zhu et al., 2007), long-term systemic treatment with low-dose LPS triggered persistent neuroinflammation and selective loss of dopaminergic neurons (Frank-Cannon et al., 2008). In a murine prion disease model, systemic LPS administration aggravated the extent of neuronal death (Cunningham et al., 2005). In support of this possibility, it has been reported that long-term use of NSAIDs (that penetrate lipid membranes only poorly) reduces the risk of neurodegenerative disease development (Chen et al., 2003; Esposito et al., 2007).
In summary, systemic inflammation alone may not be sufficiently toxic to induce neuronal death, even in the SN. However, we cannot exclude the possibility that such inflammation may interact with other insults to enhance neuronal damage Therefore, inhibition of systemic inflammation may reduce the likelihood of brain inflammation, thus helping to protect against neuronal damage and development of neurodegenerative disease.
Methods
Systemic administration of LPS
All experiments were performed in accordance with approved animal protocols and guidelines established by the Ajou University School of Medicine Ethics Review Committee for animal experiments. Male Sprague-Dawley (SD) rats (230-250 g in weight, 7 weeks of age) were anesthetized by intraperitoneal injection of ketamine (40-80 mg/kg) and xylazine (5-10 mg/kg). LPS (100-500 µg in 250 µl aliquots of sterile PBS; Sigma, St. Louis, MO) was administered iv through the tail vein. PBS-injected animals were used as controls.
Tissue preparation
Rats were anesthetized and transcardially perfused with saline solution containing 0.5% (w/v) sodium nitrate and heparin (10 U/ml), followed by 4% (v/v) paraformaldehyde in 0.1 M phosphate buffer, pH 7.2, to achieve tissue fixation. Brains were obtained and post-fixed overnight at 4℃ in 4% (v/v) paraformaldehyde. Fixed brains were added, at 4℃, to 30% (w/v) sucrose solution until the brain segments sank. Six separate series of coronal brain slices, with each slice being 30 µm in thickness, were obtained using a sliding microtome (Microm, Walldorf, Germany). For RNA preparation, rats were anesthetized and transcardially perfused with saline solution without paraformaldehyde. Brains were sliced using a Rat Brain Slicer Matrix (1.0 mm slice intervals; RBM-4000C; ASI Instruments, Warren, MI) and a razor blade. The slice including the needle injection spot was selected, and tissue blocks (2 × 2 × 2 mm3) just below the needle tip were prepared and stored at -70℃ until use.
Immunohistochemistry
Prior to 3, 3'-diaminobenzidine (DAB) staining, serial sections were rinsed three times with PBS, treated with 3% (v/v) H2O2 for 5 min, and rinsed with PBS containing 0.2% (v/v) Triton X-100 (PBST). Non-specific binding was blocked by addition of 1% (w/v) BSA in PBST. Sections were incubated for 2 h at room temperature with primary antibodies directed against Iba-1 (1:1,000; Wako Pure Chemical Industries, Osaka, Japan), GFAP (1:300; Sigma, St. Louis, MO), MPO (1:1,000; Dako, Glostrup, Denmark), IL-1β (1:200; R&D Systems, Minneapolis, MN), iNOS (1:200; Abcam, Cambridge, UK), CD68 (1:200; AbD Serotec, Oxford, UK), or tyrosine hydroxylase (TH; 1:2,000; Pelfreeze Biologicals, Rogers, AR). Following rinsing with PBST, sections were incubated with biotinylated secondary antibodies (Vector Laboratories, Burlingame, CA) and the avidin/biotin system (Vector Laboratories), and bands were visualized using 0.05% (w/v) DAB and 0.003% (v/v) hydrogen peroxide in 0.1 M PB. Next, sections were mounted on gelatin-coated slides and examined under a bright-field microscope (Olympus Optical BX51, Tokyo, Japan). Bright-field images were stored using Picture-Frame Application 2.3 software. For immunofluorescence staining, sections were washed twice in PBS, treated with 1% (w/v) BSA, and incubated with combinations of antibodies against Iba-1, MPO, iNOS, interleukin-1β, and CD68. Visualization was achieved using Alexa Fluor488- or Alexa Fluor555-conjugated secondary antibodies (1:600 dilution; Invitrogen, Eugene, OR). DAPI (Vector Laboratories) was employed to detect nuclei. Sections were analyzed by confocal microscopy (Carl Zeiss, Jena, Germany) using 40 × water and 63 × oil immersion objectives at 20℃, and images were captured using Zeiss LSM510 confocal software (Carl Zeiss, Jena, Germany).
Real-time quantitative polymerase chain reaction (Q-PCR)
Total RNA was isolated using an Easy-BLUE RNA Extraction Kit (iNtRON, Sungnam, Korea), and cDNA was prepared using Reverse Transcription Master Premix (ELPisbio, Taejeon, Korea), according to the manufacturers' instructions. For Q-PCR, approximately 50 ng cDNA was analyzed using a KAPA SYBR FAST qPCR Kit (KAPA Biosystems, Boston, MA) and a Corbett Rotor-Gene 6000 real-time rotary analyzer (Corbett Research, Mortlake, NSW, Australia). Specific primers amplifying mRNAs encoding IL-1β, TNF-α, IL-6, and glyceraldehyde-3-phosphate dehydrogenase (GAPDH), and used in Q-PCR, are shown in Supplemental Data Table S1. Q-PCR conditions were as follows: 95℃ for 30 s; followed by 40 cycles of 95℃ for 3 s (melting), 55℃ for 20 s (annealing), and 72℃ for 3 s (elongation). For TNF-α, the annealing conditions were modified to include a 63-59℃ touch-down protocol, thus decreasing the temperature by 0.5℃ per cycle over the first eight cycles. To confirm that single products were amplified under the conditions used, a melting curve analysis was performed for each primer pair, using a melt ramp of 72-95℃ and raising the temperature by 1℃ at each step (5 s/step). Amplified products were also viewed after electrophoresis on 1.5% (w/v) agarose gels, using ethidium bromide staining. The results were normalized to GAPDH levels.
Stereological analysis of dopaminergic neurons
The number of TH+ neurons in every sixth section of the entire SNpc was counted under a bright-field microscope (Olympus Optical BX51, Tokyo, Japan), using Stereo Investigator software (MBF Bioscience, Williston, VT). Counting frames (100 × 100 µm) were randomly placed over SNpc sections, and TH+ neurons were counted using a 40 × objective.
Statistical analysis
Statistical data are expressed as means ± SEMs. The significance of between-group differences was analyzed using the one-way ANOVA tool in the Statistical Package for Social Sciences, version 12 (SPSS, Chicago, IL).
Abbreviations
- CD68:
-
cluster of differentiation 68
- DHEA:
-
dehydroepiandrosterone
- GFAP:
-
glial fibrillary acidic protein
- Iba-1:
-
ionized calcium binding adaptor molecule 1
- MPO:
-
myeloperoxidase
- NSAID:
-
nonsteroidal anti-inflammatory drug
- PD:
-
Parkinson's disease
- Q-PCR:
-
quantitative polymerase chain reaction
- SI:
-
systemic inflammation
- SN:
-
substantia nigra
- TH:
-
tyrosine hydroxylase
References
Aktan F . iNOS-mediated nitric oxide production and its regulation . Life Sci 2004 ; 75 : 639 - 653
Altman R, Motton DD, Kota RS, Rutledge JC . Inhibition of vascular inflammation by dehydroepiandrosterone sulfate in human aortic endothelial cells: roles of PPARalpha and NF-kappaB . Vascul Pharmacol 2008 ; 48 : 76 - 84
Batchelor PE, Liberatore GT, Wong JY, Porritt MJ, Frerichs F, Donnan GA, Howells DW . Activated macrophages and microglia induce dopaminergic sprouting in the injured striatum and express brain-derived neurotrophic factor and glial cell line-derived neurotrophic factor . J Neurosci 1999 ; 19 : 1708 - 1716
Blum-Degen D, Muller T, Kuhn W, Gerlach M, Przuntek H, Riederer P . Interleukin-1 beta and interleukin-6 are elevated in the cerebrospinal fluid of Alzheimer's and de novo Parkinson's disease patients . Neurosci Lett 1995 ; 202 : 17 - 20
Bogdan C . Nitric oxide and the immune response . Nat Immunol 2001 ; 2 : 907 - 916
Bohatschek M, Werner A, Raivich G . Systemic LPS injection leads to granulocyte influx into normal and injured brain: effects of ICAM-1 deficiency . Exp Neurol 2001 ; 172 : 137 - 152
Breitner JC . The role of anti-inflammatory drugs in the prevention and treatment of Alzheimer's disease . Annu Rev Med 1996 ; 47 : 401 - 411
Camhi SL, Alam J, Otterbein L, Sylvester SL, Choi AM . Induction of heme oxygenase-1 gene expression by lipopolysaccharide is mediated by AP-1 activation . Am J Respir Cell Mol Biol 1995 ; 13 : 387 - 398
Cao C, Matsumura K, Ozaki M, Watanabe Y . Lipopolysaccharide injected into the cerebral ventricle evokes fever through induction of cyclooxygenase-2 in brain endothelial cells . J Neurosci 1999 ; 19 : 716 - 725
Chao CC, Hu S, Molitor TW, Shaskan EG, Peterson PK . Activated microglia mediate neuronal cell injury via a nitric oxide mechanism . J Immunol 1992 ; 149 : 2736 - 2741
Chen H, Zhang SM, Hernan MA, Schwarzschild MA, Willett WC, Colditz GA, Speizer FE, Ascherio A . Nonsteroidal anti-inflammatory drugs and the risk of Parkinson disease . Arch Neurol 2003 ; 60 : 1059 - 1064
Chen H, Jacobs E, Schwarzschild MA, McCullough ML, Calle EE, Thun MJ, Ascherio A . Nonsteroidal antiinflammatory drug use and the risk for Parkinson's disease . Ann Neurol 2005a ; 58 : 963 - 967
Chen L, Cagniard B, Mathews T, Jones S, Koh HC, Ding Y, Carvey PM, Ling Z, Kang UJ, Zhuang X . Age-dependent motor deficits and dopaminergic dysfunction in DJ-1 null mice . J Biol Chem 2005b ; 280 : 21418 - 21426
Chow CC, Clermont G, Kumar R, Lagoa C, Tawadrous Z, Gallo D, Betten B, Bartels J, Constantine G, Fink MP, Billiar TR, Vodovotz Y . The acute inflammatory response in diverse shock states . Shock 2005 ; 24 : 74 - 84
Cicchetti F, Brownell AL, Williams K, Chen YI, Livni E, Isacson O . Neuroinflammation of the nigrostriatal pathway during progressive 6-OHDA dopamine degeneration in rats monitored by immunohistochemistry and PET imaging . Eur J Neurosci 2002 ; 15 : 991 - 998
Croisier E, Moran LB, Dexter DT, Pearce RK, Graeber MB . Microglial inflammation in the parkinsonian substantia nigra: relationship to alpha-synuclein deposition . J Neuroinflammation 2005 ; 2 : 14 -
Cunningham C, Wilcockson DC, Campion S, Lunnon K, Perry VH . Central and systemic endotoxin challenges exacerbate the local inflammatory response and increase neuronal death during chronic neurodegeneration . J Neurosci 2005 ; 25 : 9275 - 9284
da Silva RP, Gordon S . Phagocytosis stimulates alternative glycosylation of macrosialin (mouse CD68), a macrophage-specific endosomal protein . Biochem J 1999 ; 338 : 687 - 694
Davalos D, Grutzendler J, Yang G, Kim JV, Zuo Y, Jung S, Littman DR, Dustin ML, Gan WB . ATP mediates rapid microglial response to local brain injury in vivo . Nat Neurosci 2005 ; 8 : 752 - 758
Dehmer T, Lindenau J, Haid S, Dichgans J, Schulz JB . Deficiency of inducible nitric oxide synthase protects against MPTP toxicity in vivo . J Neurochem 2000 ; 74 : 2213 - 2216
Elkabes S, DiCicco-Bloom EM, Black IB . Brain microglia/macrophages express neurotrophins that selectively regulate microglial proliferation and function . J Neurosci 1996 ; 16 : 2508 - 2521
Esposito E, Di Matteo V, Benigno A, Pierucci M, Crescimanno G, Di Giovanni G . Non-steroidal anti-inflammatory drugs in Parkinson's disease . Exp Neurol 2007 ; 205 : 295 - 312
Etminan M, Carleton BC, Samii A . Non-steroidal anti-inflammatory drug use and the risk of Parkinson disease: a retrospective cohort study . J Clin Neurosci 2008 ; 15 : 576 - 577
Frank-Cannon TC, Tran T, Ruhn KA, Martinez TN, Hong J, Marvin M, Hartley M, Trevino I, O'Brien DE, Casey B, Goldberg MS, Tansey MG . Parkin deficiency increases vulnerability to inflammation-related nigral degeneration . J Neurosci 2008 ; 28 : 10825 - 10834
Gao HM, Jiang J, Wilson B, Zhang W, Hong JS, Liu B . Microglial activation-mediated delayed and progressive degeneration of rat nigral dopaminergic neurons: relevance to Parkinson's disease . J Neurochem 2002 ; 81 : 1285 - 1297
Gelb DJ, Oliver E, Gilman S . Diagnostic criteria for Parkinson disease . Arch Neurol 1999 ; 56 : 33 - 39
Goldberg MS, Fleming SM, Palacino JJ, Cepeda C, Lam HA, Bhatnagar A, Meloni EG, Wu N, Ackerson LC, Klapstein GJ, Gajendiran M, Roth BL, Chesselet MF, Maidment NT, Levine MS, Shen J . Parkin-deficient mice exhibit nigrostriatal deficits but not loss of dopaminergic neurons . J Biol Chem 2003 ; 278 : 43628 - 43635
Hanisch UK, Kettenmann H . Microglia: active sensor and versatile effector cells in the normal and pathologic brain . Nat Neurosci 2007 ; 10 : 1387 - 1394
Herrera AJ, Castano A, Venero JL, Cano J, Machado A . The single intranigral injection of LPS as a new model for studying the selective effects of inflammatory reactions on dopaminergic system . Neurobiol Dis 2000 ; 7 : 429 - 447
in 't Veld BA, Launer LJ, Breteler MM, Hofman A, Stricker BH . Pharmacologic agents associated with a preventive effect on Alzheimer's disease: a review of the epidemiologic evidence . Epidemiol Rev 2002 ; 24 : 248 - 268
Inoue W, Matsumura K, Yamagata K, Takemiya T, Shiraki T, Kobayashi S . Brain-specific endothelial induction of prostaglandin E(2) synthesis enzymes and its temporal relation to fever . Neurosci Res 2002 ; 44 : 51 - 61
Itier JM, Ibanez P, Mena MA, Abbas N, Cohen-Salmon C, Bohme GA, Laville M, Pratt J, Corti O, Pradier L, Ret G, Joubert C, Periquet M, Araujo F, Negroni J, Casarejos MJ, Canals S, Solano R, Serrano A, Gallego E, Sanchez M, Denefle P, Benavides J, Tremp G, Rooney TA, Brice A, Garcia de Yebenes J . Parkin gene inactivation alters behaviour and dopamine neurotransmission in the mouse . Hum Mol Genet 2003 ; 12 : 2277 - 2291
Ji KA, Yang MS, Jou I, Shong MH, Joe EH . Thrombin induces expression of cytokine-induced SH2 protein (CIS) in rat brain astrocytes: involvement of phospholipase A2, cyclooxygenase, and lipoxygenase . Glia 2004 ; 48 : 102 - 111
Ji KA, Yang MS, Jeong HK, Min KJ, Kang SH, Jou I, Joe EH . Resident microglia die and infiltrated neutrophils andmonocytes become major inflammatory cells in lipopolysaccharide-injected brain . Glia 2007 ; 55 : 1577 - 1588
Ji KA, Eu MY, Kang SH, Gwag BJ, Jou I, Joe EH . Differential neutrophil infiltration contributes to regional differences in brain inflammation in the substantia nigra pars compacta and cortex . Glia 2008 ; 56 : 1039 - 1047
Johanson CE, Duncan JA, Klinge PM, Brinker T, Stopa EG, Silverberg GD . Multiplicity of cerebrospinal fluid functions: New challenges in health and disease . Cerebrospinal Fluid Res 2008 ; 5 : 10 -
Klegeris A, McGeer PL . Non-steroidal anti-inflammatory drugs (NSAIDs) and other anti-inflammatory agents in the treatment of neurodegenerative disease . Curr Alzheimer Res 2005 ; 2 : 355 - 365
Klein C, Djarmati A, Hedrich K, Schafer N, Scaglione C, Marchese R, Kock N, Schule B, Hiller A, Lohnau T, Winkler S, Wiegers K, Hering R, Bauer P, Riess O, Abbruzzese G, Martinelli P, Pramstaller PP . PINK1, Parkin, and DJ-1 mutations in Italian patients with early-onset parkinsonism . Eur J Hum Genet 2005 ; 13 : 1086 - 1093
Klein C, Schlossmacher MG . The genetics of Parkinson disease: Implications for neurological care . Nat Clin Pract Neurol 2006 ; 2 : 136 - 146
Knott C, Stern G, Wilkin GP . Inflammatory regulators in Parkinson's disease: iNOS, lipocortin-1, and cyclooxygenases-1 and -2 . Mol Cell Neurosci 2000 ; 16 : 724 - 739
Kreutzberg GW . Microglia: a sensor for pathological events in the CNS . Trends Neurosci 1996 ; 19 : 312 - 318
Lehrmann E, Kiefer R, Christensen T, Toyka KV, Zimmer J, Diemer NH, Hartung HP, Finsen B . Microglia and macrophages are major sources of locally produced transforming growth factor-beta1 after transient middle cerebral artery occlusion in rats . Glia 1998 ; 24 : 437 - 448
Liaudet L, Murthy KG, Mabley JG, Pacher P, Soriano FG, Salzman AL, Szabo C . Comparison of inflammation, organ damage, and oxidant stress induced by Salmonella enterica serovar Muenchen flagellin and serovar Enteritidis lipopolysaccharide . Infect Immun 2002 ; 70 : 192 - 198
Liberatore GT, Jackson-Lewis V, Vukosavic S, Mandir AS, Vila M, McAuliffe WG, Dawson VL, Dawson TM, Przedborski S . Inducible nitric oxide synthase stimulates dopaminergic neurodegeneration in the MPTP model of Parkinson disease . Nat Med 1999 ; 5 : 1403 - 1409
Liu B, Du L, Hong JS . Naloxone protects rat dopaminergic neurons against inflammatory damage through inhibition of microglia activation and superoxide generation . J Pharmacol Exp Ther 2000 ; 293 : 607 - 617
Matsumoto H, Kumon Y, Watanabe H, Ohnishi T, Shudou M, Ii C, Takahashi H, Imai Y, Tanaka J . Antibodies to CD11b, CD68, and lectin label neutrophils rather than microglia in traumatic and ischemic brain lesions . J Neurosci Res 2007 ; 85 : 994 - 1009
McGeer PL, Itagaki S, Boyes BE, McGeer EG . Reactive microglia are positive for HLA-DR in the substantia nigra of Parkinson's and Alzheimer's disease brains . Neurology 1988 ; 38 : 1285 - 1291
Meda L, Cassatella MA, Szendrei GI, Otvos L, Baron P, Villalba M, Ferrari D, Rossi F . Activation of microglial cells by beta-amyloid protein and interferon-gamma . Nature 1995 ; 374 : 647 - 650
Min KJ, Yang MS, Jou I, Joe EH . Protein kinase A mediates microglial activation induced by plasminogen and gangliosides . Exp Mol Med 2004 ; 36 : 461 - 467
Min KJ, Yang MS, Kim SU, Jou I, Joe EH . Astrocytes induce hemeoxygenase-1 expression in microglia: a feasible mechanism for preventing excessive brain inflammation . J Neurosci 2006 ; 26 : 1880 - 1887
Mogi M, Harada M, Kondo T, Riederer P, Inagaki H, Minami M, Nagatsu T . Interleukin-1 beta, interleukin-6, epidermal growth factor and transforming growth factor-alpha are elevated in the brain from parkinsonian patients . Neurosci Lett 1994 ; 180 : 147 - 150
Molina-Holgado E, Ortiz S, Molina-Holgado F, Guaza C . Induction of COX-2 and PGE(2) biosynthesis by IL-1beta is mediated by PKC and mitogen-activated protein kinases in murine astrocytes . Br J Pharmacol 2000 ; 131 : 152 - 159
Muller T, Blum-Degen D, Przuntek H, Kuhn W . Interleukin-6 levels in cerebrospinal fluid inversely correlate to severity of Parkinson's disease . Acta Neurol Scand 1998 ; 98 : 142 - 144
Nagatsu T, Sawada M . Inflammatory process in Parkinson's disease: role for cytokines . Curr Pharm Des 2005 ; 11 : 999 - 1016
Nerlich AG, Weiler C, Zipperer J, Narozny M, Boos N . Immunolocalization of phagocytic cells in normal and degenerated intervertebral discs . Spine (Phila Pa 1976) 2002 ; 27 : 2484 - 2490
Patel HC, Boutin H, Allan SM . Interleukin-1 in the brain: mechanisms of action in acute neurodegeneration . Ann N Y Acad Sci 2003 ; 992 : 39 - 47
Perry VH, Cunningham C, Holmes C . Systemic infections and inflammation affect chronic neurodegeneration . Nat Rev Immunol 2007 ; 7 : 161 - 167
Possel H, Noack H, Putzke J, Wolf G, Sies H . Selective upregulation of inducible nitric oxide synthase (iNOS) by lipopolysaccharide (LPS) and cytokines in microglia: in vitro and in vivo studies . Glia 2000 ; 32 : 51 - 59
Pyo H, Yang MS, Jou I, Joe EH . Wortmannin enhances lipopolysaccharide-induced inducible nitric oxide synthase expression in microglia in the presence of astrocytes in rats . Neurosci Lett 2003 ; 346 : 141 - 144
Qin L, Wu X, Block ML, Liu Y, Breese GR, Hong JS, Knapp DJ, Crews FT . Systemic LPS causes chronic neuroinflammation and progressive neurodegeneration . Glia 2007 ; 55 : 453 - 462
Raivich G, Bohatschek M, Kloss CU, Werner A, Jones LL, Kreutzberg GW . Neuroglial activation repertoire in the injured brain: graded response, molecular mechanisms and cues to physiological function . Brain Res Brain Res Rev 1999 ; 30 : 77 - 105
Rezaie P, Corbisiero V, Male D . Transient expression of MIDC-8 in the normal mouse brain . Neurosci Lett 2005 ; 377 : 189 - 194
Rockenstein E, Mallory M, Hashimoto M, Song D, Shults CW, Lang I, Masliah E . Differential neuropathological alterations in transgenic mice expressing alpha-synuclein from the platelet-derived growth factor and Thy-1 promoters . J Neurosci Res 2002 ; 68 : 568 - 578
Rummel C, Inoue W, Sachot C, Poole S, Hubschle T, Luheshi GN . Selective contribution of interleukin-6 and leptin to brain inflammatory signals induced by systemic LPS injection in mice . J Comp Neurol 2008 ; 511 : 373 - 395
Samii A, Etminan M, Wiens MO, Jafari S . NSAID use and the risk of Parkinson's disease: systematic review and metaanalysis of observational studies . Drugs Aging 2009 ; 26 : 769 - 779
Saper CB . The dance of the perivascular and endothelial cells: mechanisms of brain response to immune signaling . Neuron 2010 ; 65 : 4 - 6
Shi J, Johansson J, Woodling NS, Wang Q, Montine TJ, Andreasson K . The prostaglandin E2 E-prostanoid 4 receptor exerts anti-inflammatory effects in brain innate immunity . J Immunol 2010 ; 184 : 7207 - 7218
Sriram K, Matheson JM, Benkovic SA, Miller DB, Luster MI, O'Callaghan JP . Deficiency of TNF receptors suppresses microglial activation and alters the susceptibility of brain regions to MPTP-induced neurotoxicity: role of TNF-alpha . FASEB J 2006 ; 20 : 670 - 682
Streit WJ . Microglia as neuroprotective, immunocompetent cells of the CNS . Glia 2002 ; 40 : 133 - 139
Streit WJ . Microglia and neuroprotection: implications for Alzheimer's disease . Brain Res Brain Res Rev 2005 ; 48 : 234 - 239
Strijbos PJ, Rothwell NJ . Interleukin-1 beta attenuates excitatory amino acid-induced neurodegeneration in vitro: involvement of nerve growth factor . J Neurosci 1995 ; 15 : 3468 - 3474
Taniura S, Kamitani H, Watanabe T, Eling TE . Transcriptional regulation of cyclooxygenase-1 by histone deacetylase inhibitors in normal human astrocyte cells . J Biol Chem 2002 ; 277 : 16823 - 16830
Thomas B, Beal MF . Parkinson's disease . Hum Mol Genet 2007 ; 16 : R183 - R194
Thornton P, Pinteaux E, Gibson RM, Allan SM, Rothwell NJ . Interleukin-1-induced neurotoxicity is mediated by glia and requires caspase activation and free radical release . J Neurochem 2006 ; 98 : 258 - 266
Vijitruth R, Liu M, Choi DY, Nguyen XV, Hunter RL, Bing G . Cyclooxygenase-2 mediates microglial activation and secondary dopaminergic cell death in the mouse MPTP model of Parkinson's disease . J Neuroinflammation 2006 ; 3 : 6 -
Vincent VA, Tilders FJ, Van Dam AM . Inhibition of endotoxin-induced nitric oxide synthase production in microglial cells by the presence of astroglial cells: a role for transforming growth factor beta . Glia 1997 ; 19 : 190 - 198
Viviani B, Bartesaghi S, Gardoni F, Vezzani A, Behrens MM, Bartfai T, Binaglia M, Corsini E, Di Luca M, Galli CL, Marinovich M . Interleukin-1beta enhances NMDA receptor-mediated intracellular calcium increase through activation of the Src family of kinases . J Neurosci 2003 ; 23 : 8692 - 8700
Von Coelln R, Thomas B, Savitt JM, Lim KL, Sasaki M, Hess EJ, Dawson VL, Dawson TM . Loss of locus coeruleus neurons and reduced startle in parkin null mice . Proc Natl Acad Sci USA 2004 ; 101 : 10744 - 10749
Whitton PS . Inflammation as a causative factor in the aetiology of Parkinson's disease . Br J Pharmacol 2007 ; 150 : 963 - 976
Wu DC, Jackson-Lewis V, Vila M, Tieu K, Teismann P, Vadseth C, Choi DK, Ischiropoulos H, Przedborski S . Blockade of microglial activation is neuroprotective in the 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine mouse model of Parkinson disease . J Neurosci 2002 ; 22 : 1763 - 1771
Zhu XR, Maskri L, Herold C, Bader V, Stichel CC, Gunturkun O, Lubbert H . Non-motor behavioural impairments in parkin-deficient mice . Eur J Neurosci 2007 ; 26 : 1902 - 1911
Zwain IH, Yen SS . Neurosteroidogenesis in astrocytes, oligodendrocytes, and neurons of cerebral cortex of rat brain . Endocrinology 1999 ; 140 : 3843 - 3852
Acknowledgements
This work was supported by a KOSEF NRL Program grant funded by the Korean government (MEST) (no. 2-2008025-0), a grant (no. M103KV010011-06K2201-01110) from the Brain Research Center of the 21st Century Frontier Research Program of the Ministry of Science and Technology, Republic of Korea, and a grant (no. R13-2003-019) from KOSEF through the Chronic Inflammatory Disease Research Center (CIDRC) at Ajou University; all to E. Joe.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on the Experimental & Molecular Medicine website
Supplementary information
Rights and permissions
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Jeong, HK., Jou, I. & Joe, Eh. Systemic LPS administration induces brain inflammation but not dopaminergic neuronal death in the substantia nigra. Exp Mol Med 42, 823–832 (2010). https://doi.org/10.3858/emm.2010.42.12.085
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.3858/emm.2010.42.12.085
Keywords
This article is cited by
-
The blood-brain barrier in aging and neurodegeneration
Molecular Psychiatry (2022)
-
Brain profiling in murine colitis and human epilepsy reveals neutrophils and TNFα as mediators of neuronal hyperexcitability
Journal of Neuroinflammation (2021)
-
Toll-like receptor 4 agonist and antagonist lipopolysaccharides modify innate immune response in rat brain circumventricular organs
Journal of Neuroinflammation (2020)
-
Neuroinflammation in the NTS is associated with changes in cardiovascular reflexes during systemic inflammation
Journal of Neuroinflammation (2019)
-
Brilliant blue G protects against brain and liver tissue damage during systemic endotoxemia in rats treated with lipopolysaccharide
Comparative Clinical Pathology (2019)