Abstract
Patients with cystic fibrosis are severely affected by an infection with Pseudomonas aeruginosa, a microbe known to synthesize phospholipase C. This study was designed to determine whether that enzyme would affect the function of pulmonary surfactant phospholipids. Mucoid and nonmucoid strains of P. aeruginosa, freshly obtained from patients with cystic fibrosis, were cultured for 12 h on agar plates. The bacteria were suspended in saline solution and then pelleted by centrifugation. The supernatant was used to dilute the surfactant preparation, calf lung surfactant extract, from 35 to 2 mg/mL. Surfactant function, before and after incubation, was examined with a capillary surfactometer, an instrument specifically developed for an evaluation of the ability of surfactant to maintain patency of a narrow glass tube, simulating a terminal conducting airway. Phospholipid hydrolysis was also evaluated biochemically by determining the total content of phospholipids in surfactant before and after incubation. In five experiments, the lipids were separated with thin-layer chromatography, and the phosphorus content was determined in the diacylphosphatidylcholine band before and after incubation for 6, 24, and 48 h. Capillary openness and phospholipid concentration decreased as enzyme concentration and time of incubation increased (p < 0.0001). Linear regression showed a significant correlation between time of capillary openness and phospholipid concentration (r = 0.957;p < 0.0001). Calf lung surfactant extract hydrolysis was catalyzed by extracts of the bacteria, particularly the nonmucoid, analogous to the catalysis observed with phospholipase C. Surfactant hydrolysis catalyzed by enzymes from P. aeruginosa might severely affect surfactant function provided enzyme concentration is high and time of incubation is long.
Similar content being viewed by others
Main
Pulmonary surfactant primarily consists of phospholipid molecules that are amphipathic and thereby maintain alveolar stability. The molecules form a film at the air–liquid interface. When compressed to a smaller area during expiration, the film develops high surface pressure, causing a substantial reduction of the collapsing force exerted by surface tension of the hypophase. The high surface pressure ensures alveolar stability (1), and at end expiration the film will probably be partly extruded from alveoli into terminal conducting airways where it forms a lining layer that has been observed with electron microscopy (2, 3).
Also, at this second location, the surfactant film fulfills a vital function. If the air–liquid interface of cylindrical airways is not lined by a well-functioning surfactant film, moisture is not prevented from moving toward the most narrow sections of conducting airways. When the airway becomes constricted at end expiration, there might be a great risk that the accumulated liquid will bridge across the airway lumen and block airflow. That could lead to air trapping, and if this were to affect many peripheral airways, resistance to average airflow would obviously be augmented. An optimally functioning surfactant film will prevent this blockage from happening and therefore fulfills a most important function. There is evidence that during various pathologic conditions, such as those caused by ozone exposure (4, 5), respiratory syncytial virus infection (6, 7), and asthma challenge (8), an inflammatory reaction develops that is associated with a surfactant dysfunction characterized by a loss of some of the ability of surfactant to secure airway patency.
Patients suffering from cystic fibrosis are probably at particular risk of losing this ability of surfactant to maintain airway patency. The disease is associated with inflammation, causing a leakage of plasma proteins into the airway lumen that is a likely cause of a disturbed function of the pulmonary surfactant (9, 10). However, another, probably more important, reason for surfactant dysfunction is caused by a Pseudomonas aeruginosa infection that so often develops in patients with cystic fibrosis and profoundly aggravates their prognosis (11–13). The infection might disturb the surfactant function by intensifying the inflammatory reaction. However, it might also act through a different mechanism. The P. aeruginosa bacteria can synthesize and release PLC to the environment (14–18). This enzyme can catalyze a hydrolysis of PC, the main and most-active surfactant component. The breakdown products, phosphorylcholine and diacylglycerol, are both completely incapable of forming a film at the air–liquid interface. If a large proportion of the surfactant phospholipid molecules become hydrolyzed, it can be suspected that airway resistance would be seriously augmented, perhaps leading to respiratory failure.
Hydrolysis of surfactant phospholipids, catalyzed by commercially available PLC, has been studied, and it has been shown with the pulsating bubble surfactometer that the hydrolysis results in a deterioration of pulmonary surfactant function (19, 20). However, it is not known what concentration of PLC is required to cause a degree of phospholipid hydrolysis sufficient to jeopardize the ability of surfactant to maintain patency. Furthermore, it is not known whether P. aeruginosa will synthesize and release enough of the enzyme to attain a destructive concentration. To find an answer to these questions, the surfactant preparation CLSE was studied after incubation with various concentrations of PLC and with saline extracts of mucoid and nonmucoid strains of P. aeruginosa. The surface activity of the CLSE was evaluated with a CS, an instrument that is particularly appropriate for an evaluation of the ability of surfactant to maintain airway patency. The degree of phospholipid hydrolysis was evaluated biochemically.
METHODS
Surfactant affected by PLC.
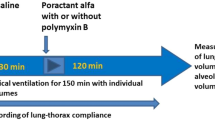
CLSE was kindly donated by ONY Inc. (Amherst, NY) and PLC from Clostridium perfringens was purchased from Sigma Chemical Co. (St. Louis, MO). The surfactant preparation was given a final phospholipid concentration of 1 mg/mL, and the enzyme was diluted in a series in saline solutions whereby its final concentrations ranged from 5 to 0.004875 U/mL. The CLSE was incubated at 37°C with the different PLC concentrations for 6, 24, and 48 h. If hydrolysis of the surface-active phospholipids had taken place after the various periods of incubation, the ability of the surfactant to maintain patency would most likely be disturbed. The possibility of such a disturbance was evaluated with the CS as described below.
The PLC concentrations that, according to studies with the CS, appeared to be high enough to catalyze phospholipid hydrolysis were used for an evaluation of the actual hydrolysis after the various periods of incubation. The lipids were extracted according to Bligh and Dyer (21), and using the colorimetric method of Chen et al. (22), the amount of phosphorus in the extracted lipids was determined, whereby the phospholipid concentration could be calculated. By plotting the CS value of the percentage of time open against the phospholipid concentration, linear regression could be used for an assessment of correlation.
The technique used for a study of how CLSE was hydrolyzed by commercially available PLC, and how surfactant's ability to maintain patency was thereby affected, was also applied to a study of how the enzyme from bacteria caused a breakdown of CLSE.
Surfactant affected by P.
aeruginosa.
Mucoid and nonmucoid strains of the bacteria, recently isolated from sputum samples obtained for routine assay of the clinical status of patients with cystic fibrosis, were applied in a standardized way in triplicate to sucrose agar plates containing 5% sheep blood. After a 12-h incubation period, a study with a McFarland nephelometer suggested that 24 × 108 bacteria were suspended per milliliter. All the bacteria, approximately 0.2 mL, from one plate were scraped off with a cotton-tipped applicator into a test tube. Four milliliters of saline solution was added, and after a few minutes of stirring, the test tube was centrifuged at 10 000 ×g for 5 min. The supernatant contained the extracellular products of the bacteria, but only a small amount of bacterial cells. A volume of 3.6 mL of supernatant was mixed with 0.4 mL of 20 mg/mL CLSE. The surfactant phospholipids were thereby diluted 10 times so that the concentration became 2 mg/mL. For control samples, CLSE was diluted with saline solution to 1 or 2 mg/mL.
The three preparations of CLSE, two diluted with saline extracts of mucoid and nonmucoid bacteria and one diluted with nothing but saline solution, were immediately studied with the CS (n = 9 × 3), and the lipids were extracted from aliquots according to Bligh and Dyer (21) for a phosphorus assay (n = 7 × 3) and for a separation of the lipids with TLC, using the solvent system of Touchstone et al. (23) (n = 5 × 3). In the last five experiments, the 12 samples (two extracts and one control studied on four occasions) were examined with each of the three methods of the study: the CS, the total phospholipids, and the lipids extracted from the PC band of the TLC plates. With the latter method, it was determined what the PC concentration had been at the beginning of the incubation period and after 6, 24, and 48 h. If, on viewing the TLC plate, it was noticed that the PC band had withered because of hydrolysis, it could be expected that the band of neutral lipids would become more noticeable, because one of the hydrolysis products, diacylglycerol, would move with the neutral lipids.
The Capillary Surfactometer.
The CS was developed in this laboratory with the specific aim of making it possible to evaluate the ability of surfactant to maintain patency of a narrow tube (24–26). The instrument uses a glass capillary to simulate a terminal conducting airway. In a short section, the capillary is constricted (inner diameter, 0.3 mm) to a width similar to that of a human respiratory bronchiole (27, 28). Liquid tends to accumulate in this narrow section, and when a small amount (0.5 μL) of the liquid to be evaluated is instilled into the constricted section, it remains there, but will be extruded when pressure, continuously recorded, is slowly raised at one end of the capillary. This will cause the blocking liquid to be pushed away from the narrow section. If it contains well-functioning pulmonary surfactant, a film will quickly form at the air–liquid interface, and, by exerting high surface pressure, it will prevent the liquid from returning to the narrow section of the capillary. Consequently, a steady flow of air through the capillary will meet no resistance, and a pressure of zero is recorded during the entire 120-s period of pressure recording that follows the initial extrusion of the liquid. Thus, the capillary is open 100% of the recording time. If, on the other hand, the surfactant is inadequate in quantity or quality, the liquid will return once or repeatedly. The continuous airflow will meet resistance, and, consequently, pressure will not remain at zero during the entire period of recording (120 s). A minicomputer calculates and prints the percentage of time that pressure remained at zero (Fig. 1) (4–8, 24–26).
Tracings obtained with the CS when a well-functioning surfactant (upper tracing) and a surfactant inhibited by protein (lower tracing) were evaluated. In the photographs that go with the upper tracing, a surfactant preparation, CLSE, 2 mg/mL, is shown being pushed to the right until it is extruded from the narrow section of the capillary. Note how the right meniscus flattens when surface pressure becomes high. The photographs that go with the lower tracing are showing the sample when it is just ready to be extruded (left), when the liquid has been extruded from the narrow section but has started to return (middle), and when the liquid is again blocking the capillary lumen (right). Note that the right meniscus is hemispherical when surface pressure is low.
Statistical evaluation.
Each CS value used for statistical analysis was the mean of three assays. One-way ANOVA was used to assess the duration of incubation on the value of percentage of time open. Unpaired t tests were used for assessments of whether the value of percentage of time open obtained after a certain period of incubation was affected more with one strain of bacteria than with another. If the values were not normally distributed, a Mann-Whitney U test was performed. Linear regression was used for an assessment of correlation between phospholipid concentration and percentage of time open. A p value of <0.05 was considered to show significance.
RESULTS
Surfactant affected by PLC.
The surface activity of the surfactant preparation CLSE (1 mg/mL) declined with increasing PLC concentration. The effect after incubation for 48 h was very pronounced when the enzyme concentration exceeded 0.156 U/mL (Fig. 2). With low enzyme concentrations or when CLSE was incubated with nothing but saline solution, it maintained 100% patency of the narrow tube even after an incubation period of 48 h.
The phospholipid concentration diminished with increasing concentrations of PLC (Fig. 3). It is seen from this figure that if the hydrolysis was sluggish because of a low enzyme concentration, it could still be crucial after a long period of incubation. As the phospholipid concentration diminished, so did the ability of the surfactant to maintain capillary patency, and when the two values were plotted against each other, a significant correlation was obtained (Fig. 4). It is also seen from the figure that the phospholipid concentration could be as low as 0.5 mg/mL, yet the value of percentage of time open would still be close to 100.
As the PLC concentration increased, the phospholipid concentration in the extracted lipids decreased. The phospholipid hydrolysis increased not only with increasing PLC concentration but also with time of incubation. The phospholipid concentration of CLSE samples used for this part of the study was 1 mg/mL, and the 20 values shown are the results of single assays.
When the phospholipid concentration after 6, 24, and 48 h of incubation with PLC was plotted against percentage of time open, a significant correlation was noted, indicating that the principal reason CLSE lost its capacity to maintain patency was the reduced concentration of surface-active phospholipids.
Surfactant affected by a P.
aeruginosa extract.
The CLSE suspension incubated with a saline extract of the bacteria suffered a loss of the ability to keep the capillary open that became more pronounced the longer the incubation lasted (p < 0.0001) (Fig. 5). The extract from the nonmucoid bacteria showed a tendency to cause a greater reduction in percentage of time open than did the extract from the mucoid bacteria, but it was only after an incubation period of 48 h that the difference became significant (p = 0.0273). The CLSE (1 mg/mL) incubated with nothing but saline solution showed that openness was maintained at 100% even after 48 h. This can be explained by the observation that the phospholipid concentration did not diminish when nothing but saline solution had been added to the CLSE. On the other hand, Figure 5 also shows how the phospholipids decreased successively when extracts from P. aeruginosa bacteria were added (p < 0.0001). It appeared as though the phospholipid concentration was reduced more with the nonmucoid than with the mucoid strain of bacteria, but the difference was not statistically significant.
Extracts from the P. aeruginosa caused a loss of ability of CLSE to maintain patency that was significant (p < 0.0001) and more pronounced the longer the incubation lasted (filled symbols). Groups are CLSE + saline only (circles), CLSE + extract from mucoid bacteria (triangles), and CLSE + extract from nonmucoid bacteria (squares) (n = 9 in each group). The extract from the nonmucoid strain appeared to have a more devastating effect, but the difference in effect between the two strains did not reach significance until after incubation for 48 h (p < 0.0273). The open symbols refer to the means of phospholipid concentrations after the various periods of incubation (n = 7 in each group). Note that the phospholipid concentration of CLSE to which nothing but saline solution had been added was not affected by the incubation.
TLC gave an image of how the enzymes from the bacteria catalyzed a hydrolysis of the surfactant phospholipids (Fig. 6). In particular, the PC withered with time of incubation, whereas the band of neutral lipids became more conspicuous. The PC band was scraped off so that the phosphorus content could be analyzed and the PC concentration in the surfactant suspension could be calculated; this is shown by a numerical value on the PC band (Fig. 6). It is particularly the disaturated PC molecules that generate a high surface pressure when a surfactant film is compressed to a reduced area. Surfactant PC has a very high proportion of disaturated molecules. Consequently, it is not surprising that linear regression analysis showed a significant correlation between PC concentration and percentage of time open (p < 0.0001, Fig. 7).
TLC plates from one of the five experiments that show PC hydrolysis when extracts of P. aeruginosa were added to CLSE. Particularly when the extract was from nonmucoid bacteria, there was a very clear withering of the PC band. At the same time, the band of neutral lipids (NL) became more prominent. Numbers on the PC bands indicate the PC concentration in milligrams per milliliter. Numbers at the bottom of the plates indicate the incubation duration in hours. PI, phosphatidyl inositol.
Concentrations of PC in the CLSE suspensions were determined by scraping off the PC bands from TLC plates. Concentrations, obtained after incubation periods of 0, 6, 24, and 48 h, were plotted against the value of percentage of time open. A significant correlation was obtained, similar to the one observed after commercially available PLC catalyzed hydrolysis of CLSE (see Fig. 4).
DISCUSSION
CLSE, a bovine surfactant preparation that has been used successfully for prevention and treatment of the respiratory distress syndrome (29, 30), was used in this study because its composition so closely resembles that of human surfactant and its function is very stable. When PLC, either the commercially available enzyme or the one extracted from P. aeruginosa bacteria, was incubated with CLSE, the surfactant phospholipids were hydrolyzed. This is the most likely cause for the surfactant to lose its surface activity. With TLC (Fig. 6), the PC band, easily identified in the samples that had not yet been incubated, became increasingly vague with time of incubation. The breakdown products of the hydrolysis catalyzed by PLC, phosphorylcholine and diacylglycerol, are not amphipathic. For that reason, they will not participate in the formation of a film exerting high surface pressure. This explains why the values for percentage of time open were lower as the phospholipid concentrations diminished (Fig. 4). One hydrolysis product, diacylglycerol, migrated with the neutral lipids and contributed to a more conspicuous band of those lipids, and did so as the PC band withered (Fig. 6). Our data are in accordance with what has previously been suspected to occur with pulmonary surfactant during an infection with P. aeruginosa (14).
It was shown by Berka et al. (16) and Berka and Vasil (17) that the nonmucoid P. aeruginosa, which causes the initial infection, produces more PLC than does the mucoid strain. They suggested that the bacteria might be able to scavenge inorganic phosphate from cell membranes of the pulmonary epithelium. This would provide the energy for the bacteria to launch the pulmonary infection and colonize their habitat. It can be assumed that if the enzyme has the capacity to catalyze hydrolysis of phospholipids in the membranes of epithelial cells, they are likely also to catalyze hydrolysis of pulmonary surfactant phospholipids, resulting in the harmful effect of the microbes. Our data are consistent with the observations of Berka et al. (16) and Berka and Vasil (17) that the nonmucoid bacteria produce greater amounts of PLC. It might be that the mucus synthesized by the mucoid microbe is a hindrance for its release of PLC.
As Hohlfeld et al. (31) describe in their article on obstructive airway disease, surfactant inhibition is an important link in a cycle that causes airway obstruction. One characteristic of this cycle is that there is always an irritant, an allergic reaction, or an infection that initiates the vicious cycle. In addition to the problems that per se are likely to be caused by a PLC-catalyzed hydrolysis of epithelial cells in the airway wall, the hydrolysis probably initiates a detrimental cycle. The breakdown of epithelial cells will induce an inflammation that will allow a leakage of plasma proteins into the airway lumen. Those proteins are known to inhibit the function of surfactant (32–35) and are likely to reduce its ability to maintain airway patency (4–8, 24–26).
When cystic fibrosis is complicated by an infection with P. aeruginosa, the condition becomes even more arduous to treat effectively. The bacterium is difficult to attack because it evades the body's immune system and grows in microcolonies, thereby decreasing the effectiveness of many antibiotics (11–14). Pulmonary dysfunction resulting from bronchitis is a leading cause of death, and an increased mortality has been associated with the appearance of a P. aeruginosa infection (13). However, in the future, it might be possible to develop treatments that will combat the onset of infection, or at least decrease its severity. The Clara cell 10-kD protein might offer such a possibility. The protein protects phospholipids from phospholipase A2-catalyzed hydrolysis, and has been shown to also prevent PLC-catalyzed hydrolysis of phosphatidylinositol (36, 37).
This study was conducted to examine the possible damage that might be inflicted on pulmonary surfactant by an infection with P. aeruginosa. It was hypothesized that a release of PLC by the microbe might catalyze hydrolysis of the surfactant phospholipids. That could cause surfactant to lose its ability of maintaining patency of conducting airways. They might then become blocked during part of the respiratory cycle, and, in turn, air trapping and hyperinflation of the lungs might occur and most likely cause an increased airway resistance. Those clinical features are typical for patients with cystic fibrosis (38) and are also commonly seen in patients with asthma (39). Our data offer strong evidence that the hypothesis was correct. TLC showed that the enzyme extracted from the microbe catalyzed hydrolysis of the surfactant PC. When the bacteria were of the nonmucoid strain, the PC band practically disappeared after incubation for 48 h, which is the likely explanation for the extremely poor surfactant function observed with the CS. We believe strongly that we were able to show that hydrolysis of the surfactant PC did occur. However, there might have been other factors contributing to the harmful effect we noticed on the ability of surfactant to maintain patency. In the bacterial supernatant, there might have been proteolytic enzymes, catalyzing hydrolysis of surfactant apoproteins B and C. Those proteins are present in CLSE and play a vital role because they promote a fast adsorption of the amphipathic molecules.
The surfactant damage is an interesting observation and might be of great practical importance, but admittedly there are several points of uncertainty. It is not known, for instance, what the enzyme concentration is likely to be in the hypophase of the terminal conducting airway. Nor is it known whether the duration of contact between a surfactant film and PLC released from bacteria will be long enough to be harmful. Furthermore, it is not known whether the surfactant will be recycled and synthesized at a higher rate as a result of the increased catabolism. These considerations might explain why the microbe does not cause an immediate and rapidly progressing pulmonary insufficiency. In the future, it will be of great interest to examine bronchoalveolar lavage fluid from patients with cystic fibrosis with and without an infection with P. aeruginosa. It might show that once the patient has been infected, the surfactant of the bronchoalveolar lavage fluid contains less PC and has a reduced ability to maintain patency.
In our study, the CLSE suspension had a phospholipid concentration of 1 or 2 mg/mL. In the lung, it is difficult to estimate what the phospholipid concentration will be. We do know, however, that a phospholipid monolayer is at the air–liquid interface (2, 3) and will be in touch with the bacteria. The enzyme they release can therefore be suspected to catalyze a hydrolysis of the surfactant phospholipids.
Abbreviations
- CLSE:
-
calf lung surfactant extract
- CS:
-
capillary surfactometer
- PC:
-
diacylphosphatidylcholine
- PLC:
-
phospholipase C
- TLC:
-
thin-layer chromatography
References
Clements JA 1962 Surface phenomena in relation to pulmonary function. Physiologist 5: 11–28.
Gil J, Weibel ER 1971 Extracellular lining of bronchioles after perfusion-fixation of rat lungs for electron microscopy. Anat Rec 169: 185–200.
Gehr P, Schürch S, Berthiaume Y 1990 Particle retention in airways by surfactant. J Aerosol 3: 27–43.
Currie WD, van Schaik SM, Vargas I, Enhorning G 1998 Ozone affects breathing and pulmonary surfactant function in mice. Toxicology 125: 21–30.
Currie WD, Van Schaik SM, Vargas I, Enhorning G 1998 Breathing and pulmonary surfactant function in mice 24 h after ozone exposure. Eur Respir J 12: 288–293.
Van Schaik SM, Vargas I, Welliver RC, Enhorning G 1997 Surfactant dysfunction develops in BALB/c mice infected with respiratory syncytial virus. Pediatr Res 42: 169–173.
Van Schaik SM, Enhorning G, Vargas I, Welliver RC 1998 Respiratory syncytial virus (RSV) causes changes in respiratory function in BALB/c mice. J Infect Dis 177: 269–276.
Hohlfeld JM, Ahlf K, Enhorning G, Balke K, Erpenbeck VJ, Petschallies J, Hoymann HG, Fabel H, Krug N 1999 Dysfunction of pulmonary surfactant in asthmatics after segmental allergen challenge. Am J Respir Crit Care Med 159: 1803–1809.
Griese M, Duroux A, Schams A, Lenz AG, Kleinsasser N 1997 Tracheobronchial surface active material in cystic fibrosis. Eur J Med Res 2: 114–120.
Griese M, Birrer P, Demirsoy A 1997 Pulmonary surfactant in cystic fibrosis. Eur Respir J 10: 1983–1988.
Henry RL, Mellis CM, Petrovic L 1992 Pseudomonas aeruginosa infection is a marker of poor survival in cystic fibrosis. Pediatr Pulmonol 12: 158–161.
Hudson VL, Wielinski CL, Regelmann WE 1993 Prognostic implications of initial oropharyngeal bacterial flora in patients with cystic fibrosis diagnosed before the age of two years. J Pediatr 122: 854–860.
Suter S 1994 New perspectives in understanding and management of the respiratory disease in cystic fibrosis. Eur J Pediatr 153: 144–150.
Liu PV 1974 Extracellular toxins of Pseudomonas aeruginosa. J Infect Dis 130: S94–S99.
Stinson MV, Hayden C 1979 Secretion of phospholipase C by Pseudomonas aeruginosa. Infect Immun 25: 558–564.
Berka RM, Gray GL, Vasil ML 1981 Studies of phospholipase C (heat-labile hemolysin) in Pseudomonas aeruginosa. Infect Immun 34: 1071–1074.
Berka RM, Vasil ML 1982 Phospholipase C (heat-labile hemolysin) of Pseudomonas aeruginosa : purification and preliminary characterization. J Bacteriol 152: 239–245.
Lucchesi GI, Domenech CE 1994 A simple and reliable method for purification of Pseudomonas aeruginosa phospholipase C produced in high phosphate medium containing choline. J Biochem 16: 155–162.
Holm BA, Keicher L, Sokolowski J, Enhorning G 1991 Inhibition of pulmonary surfactant function by phospholipases. J Appl Physiol 71: 317–321.
Enhorning G, Shumel B, Keicher L, Holm BA 1992 Phospholipases introduced into the hypophase affect the surfactant film outlining a bubble. J Appl Physiol 73: 941–945.
Bligh EG, Dyer WL 1959 A rapid method of total lipid extraction and purification. Can J Biochem Physiol 37: 911–917.
Chen PS, Toribara TY, Huber W 1956 Microdetermination of phosphorus. Anal Chem 28: 1756–1768.
Touchstone JC, Chen JC, Beaver KM 1980 Improved separation of phospholipids in thin layer chromatography. Lipids 15: 61–62.
Liu M, Wang L, Li E, Enhorning G 1991 Pulmonary surfactant will secure free airflow through a narrow tube. J Appl Physiol 71: 742–748.
Enhorning G, Holm BA 1993 Disruption of pulmonary surfactant's ability to maintain openness of a narrow tube. J Appl Physiol 74: 2922–2927.
Enhorning G 1996 Pulmonary surfactant function in alveoli and conducting airways. Can Respir J 3: 21–27.
Weibel ER 1963 Morphometry of the Human Lung. Academic Press, New York, 124
Horsfield K, Cumming G 1968 Morphology of the bronchial tree in man. J Appl Physiol 24: 373–383.
Enhorning G, Shennan A, Possmayer F, Dunn M, Chen CP, Milligan J 1985 Prevention of neonatal respiratory distress syndrome by tracheal instillation of surfactant: a randomized trial. Pediatrics 76: 145–153.
Kwong MS, Egan EA, Notter RH, Shapiro DL 1985 Double-blind clinical trial of calf lung surfactant extract for the prevention of hyaline membrane disease in extremely premature infants. Pediatrics 76: 585–592.
Hohlfeld J, Fabel H, Hamm H 1997 The role of pulmonary surfactant in obstructive airway disease. Eur Respir J 10: 482–491.
Ikegami M, Jobe A, Jacobs H, Lam R 1984 A protein from airways of premature lambs that inhibits surfactant function. J Appl Physiol 57: 1134–1142.
Seeger WG, Stohr G, Wolf HRD, Neuhof H 1985 Alteration of surfactant function due to protein leakage: special interaction with fibrin monomer. J Appl Physiol 58: 326–338.
Holm BA, Notter RH, Finkelstein JN 1985 Surface property changes from interactions of albumin with natural surfactant and extracted lung lipids. Chem Phys Lipids 38: 287–298.
Fuchimukai T, Fujiwara T, Takahashi T, Enhorning G 1987 Artificial pulmonary surfactant inhibited by proteins. J Appl Physiol 62: 429–437.
Singh G, Katyal SL, Brown WE, Kennedy AL, Singh U, Wong-Chong M 1990 Clara cell 10 kDa protein (CC10): Comparison of structure and function to uteroglobin. Biochim Biophys Acta 1039: 348–355.
Mantile G, Miele L, Cordella-Miele E, Singh G, Katyal SL, Mukherjee AB 1993 Human Clara cell 10-kDa protein is the counterpart of rabbit uteroglobin. J Biol Chem 268: 2034–2035.
Tepper RS, Hiatt PW, Eigen H, Smith J 1987 Total respiratory system compliance in asymptomatic infants with cystic fibrosis. Am Rev Respir Dis 135: 1075–1079.
Kemp DW 1992 Physiologic evaluation of asthma. Chest 101: 396S–400S.
Acknowledgements
The authors thank Dr. Murray Stinson for providing a critical and valuable review of the manuscript.
Author information
Authors and Affiliations
Additional information
Supported by National Institutes of Health (grant 49971) and The Kettering Family Foundation.
Rights and permissions
About this article
Cite this article
Lema, G., Dryja, D., Vargas, I. et al. Pseudomonas aeruginosa from Patients with Cystic Fibrosis Affects Function of Pulmonary Surfactant. Pediatr Res 47, 121 (2000). https://doi.org/10.1203/00006450-200001000-00021
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200001000-00021
This article is cited by
-
Pilot trial of late booster doses of surfactant for ventilated premature infants
Journal of Perinatology (2011)
-
Ethanolamine utilization in bacterial pathogens: roles and regulation
Nature Reviews Microbiology (2010)