Abstract
Recent studies suggest that secreted phospholipases A2 (sPLA2s) represent attractive potential tumour biomarkers and therapeutic targets for various cancers. As a first step to address this issue in human colorectal cancer, we examined the expression of the full set of sPLA2s in sporadic adenocarcinomas and normal matched mucosa from 21 patients by quantitative PCR and immunohistochemistry. In normal colon, PLA2G2A and PLA2G12A were expressed at high levels, PLA2G2D, PLA2G5, PLA2G10 and PLA2G12B at moderate levels, and PLA2G1B, PLA2G2F and PLA2G3 at low levels. In adenocarcinomas from left and right colon, the expression of PLA2G3 was increased by up to 40-fold, while that of PLA2G2D and PLA2G5 was decreased by up to 23- and 14-fold. The variations of expression for sPLA2-IID, sPLA2-III and sPLA2-V were confirmed at the protein level. The expression pattern of these sPLA2s appeared to be linked respectively to the overexpression of interleukin-8, defensin α6, survivin and matrilysin, and downregulation of SFRP-1 and RLPA-1, all these genes being associated to colon cancer. This original sPLA2 profile observed in adenocarcinomas highlights the potential role of certain sPLA2s in colon cancer and suggests that sPLA2-III might be a good candidate as a novel biomarker for both left and right colon cancers.
Similar content being viewed by others
Main
Sporadic colorectal cancer is a major human health concern in industrialised countries and is the third leading cause of mortality by cancer. The accumulation of genetic alterations in several key genes (APC, K-ras, DCC and p53) has been associated with tumour development (Fearon and Vogelstein, 1990). In particular, the activation of the Wnt/β-catenin/Tcf-4 pathway is known to play a key role in colon tumorigenesis, leading to overexpression of a large number of target genes, including c-myc, cyclin D1, MMP-7, ITF-2, Il-8, gastrin, uPAR, cryptdin/defensin and EPR-1 genes (Kolligs et al, 2002; Levy et al, 2002). Moreover, the participation of tumour modifier genes may also contribute to pathogenesis, providing a basis to individual genetic predispositions, in addition to environmental and diet influences (Wiesner et al, 2003; Yan et al, 2004; Rakoff-Nahoum and Medzhitov, 2007). A comprehensive characterisation of such tumour modifier genes must take into account the stage of cancer and the location of the tumour within the large intestine, that is, ‘right’ or ‘left’ colon. This information may lead to a better understanding of the molecular events involved in colorectal cancer, and may provide new therapeutic targets to improve patient treatment outcomes (Williams et al, 2003; Barrier et al, 2005). It is also of interest to investigate the expression of such genes to identify new biomarkers of human colorectal cancers for early diagnosis and prognosis (Williams et al, 2003; Barrier et al, 2005).
In humans, 10 secreted phospholipases A2 (sPLA2s) have been described in the last decade, and the analysis of their functions in physiological and pathophysiological conditions is under intense investigation. Human sPLA2s have been classified into groups IB, IIA, IID, IIE, IIF, III, V, X, XIIA and XIIB according to their structural properties (Laye and Gill, 2003; Rouault et al, 2003; Murakami et al, 2005; Cummings, 2007). Several of these proteins have recently been proposed either as biomarkers of pathologies (Smith et al, 2003; Mallat et al, 2005; Wootton et al, 2007) or as therapeutic targets (Laye and Gill, 2003; Cummings, 2007; Henderson et al, 2007). These enzymes have the capacity to generate biologically active lipid mediators such as lysophosphatidic acid (LPA) and arachidonic acid (AA), which can be further converted into prostaglandin E2 (PGE2). These lipid mediators are known to be involved in cell proliferation, cell migration, angiogenesis, and are likely to play a role in the initiation and/or progression of colorectal cancer (Morioka et al, 2000; Krause and DuBois, 2001; Laye and Gill, 2003; Mills and Moolenaar, 2003; Murakami et al, 2005). AA can also participate in apoptosis by activating sphingomyelinases and ceramide production (Dong et al, 2005; Ilsley et al, 2005).
Secreted phospholipases A2 have been recently proposed as targets for anticancer drugs (Laye and Gill, 2003; Cummings, 2007), and there is increasing evidence for their involvement in various human cancers. Indeed, the expression levels of sPLA2-V and sPLA2-X are modified in human lung cancer (Masuda et al, 2005b), and those of sPLA2-V and sPLA2-XIIA in human ovarian cancer (Gorovetz et al, 2006). In particular, the overexpression of human sPLA2-IIA in gastric adenocarcinoma was proposed to be related to prolonged survival and less frequent metastasis (Leung et al, 2002; Aggarwal et al, 2006). By contrast, sPLA2-IIA overexpression has been associated to oncogenic effects in prostate cancer (Sved et al, 2004) and is related to poor prognosis (Graff et al, 2001). The polymorphism of the sPLA2-IIA gene, PLA2G2A, is also associated to some phenotypic features of patients with familial adenomatous polyposis (Yanaru-Fujisawa et al, 2007). More recently, human sPLA2-XIIB was shown to be upregulated in 50% of patients with hepatitis C virus-associated hepatocellular carcinoma (Smith et al, 2003). Finally, a protective role for sPLA2-IIA against ApcMin-induced intestinal tumours has been established in mice (MacPhee et al, 1995; Cormier et al, 1997). However, data on sPLA2 and human cancers are still sparse, and often rely on only one or a few sPLA2s.
In this study, we have analysed the expression pattern of the full set of sPLA2s in tumour vs normal matched mucosa from patients with adenocarcinomas located in the left and right colon. Variation in the expression of a number of other genes associated with colon tumorigenesis and/or inflammation was also examined to establish possible gene coregulations. Our data provide the first comprehensive analysis of the expression pattern of all sPLA2s in normal human colon mucosa as well as adenocarcinomas. These data further support the fact that several sPLA2s may contribute to the initiation, progression or modulation of colon tumorigenesis, and may provide new potential tumour markers for this disease.
Materials and methods
Human tissues and RNA isolation
Fourteen colon adenocarcinoma specimens from the left colon (descending part of the colon) and seven colon adenocarcinoma specimens from the right colon (ascending part of the colon) were obtained from surgical resections according to the French and American institutional guidelines. No specimen was from rectum. The patients did not receive chemotherapy or radiotherapy prior to surgery. The specimens were from 42- to 85-year-old patients (median age: 71 years), 14 men and 7 women. Samples were well (3 out of 21), moderately (14 out of 21) or poorly (4 out of 21) differentiated sporadic adenocarcinomas, with pTNM classification ranging pT2–4 N0–2 M0–1. Neither adenoma nor Duke'D adenocarcinoma was examined in this study. All samples had an expression of hMLH1 and hMSH2 unchanged as evaluated by immunohistochemistry and quantitative PCR (qPCR) (data not shown). Tissues from the non-necrotic part of the tumour and from distant normal mucosa were snap frozen in liquid nitrogen and stored at −80°C. Each tissue sample (20–100 mg) was mixed with 700 μl of lysis buffer plus β-mercaptoethanol (nucleospin RNA II kit; Macherey-Nagel, Hoerdt, France) in a green-cap tube containing Lysing Matrix D (Q-BIOgene, Illkrich, France), and tissue disruption was achieved with the fast prep instrument (FP220A; Q-BIOgene). Total RNA was then isolated using the nucleospin RNA II kit, including DNase treatment. RNA concentration was determined by OD260 and RNA quality was evaluated by analysis on an Agilent Bioanalyzer (Agilent Technologies, Les Ulis, France).
Quantitative PCR
First-strand cDNA was synthesised from 5 μg of total RNA using 100 U of MMLV reverse transcriptase (#M170A; Promega, Charbonnières-les bains, France) in a final volume of 50 μl with 500 ng of random primers (#C118A; Promega). Quantitative PCR was carried out in 96-well ABgene plates using the GENEAMP 5700 sequence Detection System apparatus (Applied Biosystems, Courtaboeuf, France) with the qPCR Master Mix Plus for SYBR® Green I (Eurogentec, Angers, France). All reactions were performed in a total volume of 16 μl and contained 50 ng of reverse transcribed RNA (based on the initial RNA concentration) and 250 nM of each primer set. The primer sets were designed using the Primer Express program from Applied Biosystems for the following human genes: PLA2G2A (NM_000300), sPLA2-IID gene (PLA2G2D) (NM_012400), sPLA2-IIE gene (PLA2G2E) (NM_0145891), sPLA2-IIF gene (PLA2G2F) (NM_022819), sPLA2-III gene (PLA2G3) (NM_015715), sPLA2-V gene (PLA2G5) (NM_000929), sPLA2-X gene (PLA2G10) (NM_003561), sPLA2-XIIA gene (PLA2G12A) (BC_017218), sPLA2-XIIB gene (PLA2G12B) (NM_032562), iPLA2-VIB gene (PLA2G6) (NM_003560), ptgs1 (BC_029840), COX-2 gene (ptgs2) (NM_000963), ptges1 (NM_004878), ptges2 (NM_198797), Il-1α (NM_000575), Il-6 (NM_000600), Il-10 (NM_57627), PPARγ (NM_138712), PPARδ (NM_006238), u-PA (NM_002658), u-PAR (NM_002659), IL-8 (NM_000584), EPR-1 (NM_002219), MMP-7 (NM_002423), SFRP-1 (NM_003012), PLA2R1 (NM_007366), TNF-α (NM_000594), MMP-9 (NM_004994), MSH2 (NM_000251), MLH1 (NM_000249). Most primer sets were designed to span an intron in order to avoid amplification from potential traces of genomic DNA in the total RNA preparations. Only the primer sets for MLH1, uPAR, EPR-1, MMP-7 and bcl-2 genes were not spanning an intron. For primer sets spanning an intron, we checked that no amplification signal was obtained using human genomic DNA as template in the qPCR (data not shown). The sequences of the designed primer sets are available on request. We used Qiagen commercial primer sets for cPLA2-IVA gene (PLA2G4A) (ref. QT00085813) and sPLA2-IB gene (PLA2G1B) (ref. QT00000637). We used published primer sets for RLPA-1 and RLPA-2 genes (Shida et al, 2004) and HD-6 gene (Andreu et al, 2005). The efficiency and specificity of each primer sets were validated using either serial dilutions of cloned human sPLA2 cDNAs or mixed human tissue cDNA for the other genes. Moreover, when enough total RNA was collected, negative controls without added reverse transcriptase were performed. Thermal cycling was performed at 95°C for 10 min, followed by 40 cycles comprising each a denaturation step at 95°C for 15 s, and an annealing/extension step at 60°C for 1 min. Amplification of the appropriate product was verified by analysing the dissociation curve that was obtained after PCR with the following steps: 15 s at 95°C, 20 s at 60°C, and then a slow ramp of 20 min from 60 to 95°C. The abundance of the mRNA target was calculated relative to the expression of the reference gene TOP1 and is expressed as , where ΔCt=Ct (gene of interest)−Ct (TOP1). The choice of TOP1 as a reference gene was determined using a Human GeNorm kit (PrimerDesign Ltd, Southampton, UK), allowing the determination of the best reference gene among 12 widely used reference genes. The data were also validated using GAPDH as a reference gene (data not shown). When the relative level of expression was plotted for normal mucosa (n) (Figure 1), we used the formula , with ΔCt=Ct(n)gene−Ct(n)TOP1. The Ct(n) values for TOP1 were typically around 20. When the expression of each gene in normal mucosa vs tumours (Figure 2 , 3 and 4) was plotted, the comparative Ct method (detailed in the ABI Prism 7700 Sequence Detection System User Bulletin no. 2) was used to determine the relative quantities of mRNA, and we changed the sign in order to get the lowest level of expression at the bottom and the highest level of expression at the top of the y axis, that is, −ΔCt=−(Ct gene of interest−Ct TOP1). When the expression of each gene was compared between the tumour (t) and the matched normal mucosa (n), the decrease or increase factor φ in the tumour vs the normal mucosa (Figure 5A and B) was calculated with the formula , with ΔCt(n)=Ct(n)gene−Ct(n)TOP1, ΔCt(t)=Ct(t)gene−Ct(t)TOP1, and I the absolute value of the term ΔCt(n)−ΔCt(t).
Expression level of sPLA2 genes in human colon normal mucosa. The relative averaged expression level of all sPLA2 genes and the two reference genes used in this study (TOP1 and GAPDH) is shown for the 14 samples from left colon and the 7 samples from right colon. Arbitrary units are used (see Materials and Methods).
Expression level of sPLA2 genes in human adenocarcinomas and normal matched mucosa. The expression level of sPLA2 genes and of the M-type sPLA2 receptor (PLA2R1) was measured in adenocarcinomas and normal matched mucosa for the 14 left-sided samples. The data were obtained after normalisation with TOP1 used as reference gene and using the formula −ΔCt=Ct gene of interest−Ct TOP1. N, normal tissues; T, tumour tissues.
Expression level of sPLA2, tumour-related and inflammation-related genes in human left colon adenocarcinomas. After normalisation with the TOP1 reference gene, the expression level for each gene in the tumour was compared to that in the normal matched mucosa. The zero value indicates no variation, a positive value indicates an increased expression level in tumour vs normal tissue and a negative value indicates a decreased expression level in tumour vs normal tissue (see Materials and Methods). The incidence of variation in the different samples is indicated.
Expression level of sPLA2, tumour-related and inflammation-related genes in human right colon adenocarcinomas. Same legend as Figure 3.
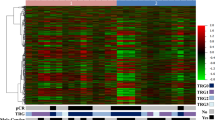
Hierarchical clustering of genes. Heatmaps comparing the log 2 ratio between the expression level in adenocarcinomas and normal epithelium for the 14 patients with left-sided adenocarcinomas (A) and for the 7 patients with right-sided adenocarcinomas (B) are shown. The distance corresponds to an Euclidean distance calculated using the Mev3.1 software.
Immunohistochemistry
All experiments were performed using paraffin-embedded tissues from the same patients as those used for the qPCR experiments. The expression of sPLA2-IID, sPLA2-III, sPLA2-V and COX-2 proteins was analysed in tumours and normal matched tissues from three to four patients. Consecutive 4-μm tissue sections were deparaffinised in xylene and rehydrated in graded alcohol dilutions. Immunolabelling was performed using avidin–biotin–peroxidase technique (Vectastain ABC kit; Vector, Burlingame, CA, USA). Before immunostaining, endogenous peroxidase activity was inhibited with 0.1% hydrogen peroxide in methanol for 30 min. Colour development was achieved with 3-amino-9-ethyl-carbazole, and sections were finally counterstained with haematoxylin. Specific rabbit polyclonal antibodies against recombinant human sPLA2-IID, sPLA2-III and sPLA2-V were produced as described (Haas et al, 2005), and used at working dilutions of 1/300, 1/250 and 1/100, respectively. All anti-sPLA2 antibodies were tested for specificity towards the various sPLA2s and were shown to be highly specific for each human sPLA2 (Haas et al, 2005). Negative controls were performed by omission of the primary antibody. To further check for the specificity of labelling with sPLA2-IID-, sPLA2-III- and sPLA2-V-specific antibodies, competition experiments were performed in which the antibody was preincubated with the corresponding purified recombinant sPLA2 used for immunisation, prior to covering the tissue slides. The competition was performed by preincubating the relevant antibody solution with 200 nM of human recombinant sPLA2-III or 100 nM of human recombinant sPLA2-IID and sPLA2-V for 1 h at room temperature. Purified recombinant proteins were obtained as described (Rouault et al, 2007). Human COX-2 antibodies were from Cayman (Montigny-le Bretonneux, France) (ref. 160112, working dilution 1/500), human MLH1 antibodies were from BD Pharmingen (Le Pont-de-Claix, France) (clone G168-178, working dilution 1/100), and human MSH2 antibodies were from Calbiochem (Darmstadt, Germany) (clone FE-11, working dilution 1/125).
Statistics
We determined that the sample data from left and right colons followed a Gaussian distribution using the D'agostino–Pearson normality test. Normal mucosa and tumour paired data for each gene were analysed using the Bonferroni test, and statistical significances were represented by *P<0.05, **P<0.01 and ***P<0.001. We looked for correlation between all genes examined in this study by using the Mev3.1 software and hierarchical clustering to analyse different linkages to cluster genes and samples. Euclidean distance was used to calculate the distance between two genes.
Results
Expression levels of sPLA2 genes in normal human colon mucosa
We first looked at the mRNA levels for the different sPLA2 genes in normal mucosa and compared their relative expression levels. Our data show dramatic differences in the relative expression of sPLA2. The lowest gene expression level was found for PLA2G3, and the highest gene expression level was found for PLA2G2A (Figure 1). The level of PLA2G2A expression was particularly high. It is above that of TOP1 and almost reaches that of GAPDH, which are both used as reference genes and are known to be highly expressed in many tissues, including colon. By contrast, the expression of PLA2G3 was generally very low, in fact below the limit of detection in many samples (Figure 1). The expression levels of PLA2G2F and PLA2G1B were also low, while that of other sPLA2 genes were moderate. The expression of PLA2G2E was not detectable (data not shown). We also compared the expression levels in normal mucosa of left and right colon. A significant difference in gene expression levels was seen for PLA2G2F, PLA2G1B, PLA2G12B and PLA2G10 (respectively 30-, 13-, 24- and 40-fold lower expression in right-sided normal mucosa than in left-sided normal mucosa). No or minor differences were observed in gene expression for PLA2G2A, PLA2G2D, PLA2G3, PLA2G5 and PLA2G12A between right- and left-sided normal mucosa (Figure 1).
Expression levels of sPLA2 genes in left and right colon adenocarcinomas vs normal human colon mucosa
We next compared sPLA2 gene expression in adenocarcinomas vs normal mucosa. The raw data for samples from the left colon are shown in Figure 2. The fold-increase or fold-decrease in the expression of each gene in adenocarcinomas vs normal mucosa is represented in Figure 3. Interestingly, we observed a 40-fold increase in PLA2G3 expression in the adenocarcinomas. In contrast, we found 23- and 14-fold decreases for PLA2G2D and PLA2G5, respectively. Similar data were obtained for samples from the right colon, with a 22-fold increased expression in tumour vs normal mucosa for PLA2G3, and 10- and 44-fold reduced expression for PLA2G2D and PLA2G5, respectively (Figure 4). No variation in expression between the tumours and normal mucosa was observed for PLA2G1B, PLA2G2A, PLA2G2F, PLA2G10, PLA2G12A and PLA2G12B and for the M-type sPLA2 receptor (PLA2R1) (Figure 3 and 4). The expression of PLA2G2E was not detectable in any of the samples analysed (data not shown).
Expression levels of genes involved in inflammation and tumorigenesis in left and right colon adenocarcinomas vs normal human colon mucosa
Since sPLA2s may exert a coordinate action with other genes in tumorigenesis and associated inflammation, we also examined the expression of a panel of genes known to be involved in inflammation and colorectal tumorigenesis (Figure 3 and 4). In left colon samples, we did not observe any differences in expression levels between adenocarcinomas and normal mucosa for most of the inflammation-related genes examined in this study, that is, ptgs2, ptges1, ptges2, TNF-α, Il-1α, Il-6, Il-10, PPARγ, PPARδ, MMP-9 and PLA2G6. Only a slight decrease in the expression of ptgs1 and PLA2G4A was observed. With the exception of ptges2 and Il-1α, we found that the inflammation-related genes were already expressed at high levels in the normal mucosa.
We also looked at the expression of urokinase plasminogen activator (u-PA) and its receptor (u-PAR) that play a role in cell adhesion and cell migration, and are involved in late stages of tumour development, contributing to tumour cell invasion and metastatic spread (Terada et al, 2005). No changes were observed in u-PA and u-PAR gene expression levels.
RLPA-1 and RLPA-2 genes code for two distinct LPA receptors (Mills and Moolenaar, 2003). While the expression of RLPA-2 did not change, that of RLPA-1 was decreased by 20-fold in tumour vs normal matched mucosa.
IL-8, EPR-1, HD-6 and MMP-7 are target genes of the Wnt/β-cat/tcf-4 pathway (Kolligs et al, 2002; Levy et al, 2002; Wheatley and McNeish, 2005). Interestingly, a marked increase in expression was found for Il-8, HD-6 and MMP-7 expression in the tumours (8-, 22- and 70-fold, respectively). The level of EPR-1 was not changed. SFRP-1 codes for an antagonist of the Wnt pathway, which binds to the frizzled receptor and blocks frizzled–Wnt interaction (Suzuki et al, 2004). Our results show a dramatic 130-fold decrease in the expression of SFRP-1 in the tumour.
Similar data were obtained for most genes in the right-sided samples (Figure 4). Indeed, no variation in expression was observed for most inflammatory-related genes, while a dramatic increase (280-fold) and a strong decrease (125-fold) were found for MMP-7 and SFRP-1, respectively. However, in contrast to left-sided samples, we observed no variation in HD-6 and Il-8 expression levels and a strong increase (45-fold) in EPR-1 expression.
Incidence and coregulation of studied genes
We first looked at the incidence of the above variations, that is, the number of samples showing an increase or decrease in the expression level of a particular gene within the 21 patients used in this study (Figure 3, 4 and 5). The increase in PLA2G3 expression showed a high incidence (12 out of 14 for left-sided samples and 5 out of 7 for right-sided samples), which was similar to that of MMP-7 gene overexpression (10 out of 14 for left-sided samples and 6 out of 7 for right-sided samples). The incidence for the overexpression of HD-6 and Il-8 was lower, since these two genes were not significantly upregulated in right-sided samples. The decrease in PLA2G2D and PLA2G5 expression also showed a high incidence (12 out of 14 and 5 out of 7; and 11 out of 14 and 5 out of 7, respectively), which was similar to that of RLPA-1 and SFRP-1 gene expression (13 out of 14 and 6 out of 7; and 14 out of 14 and 7 out of 7, respectively). We did not observe any difference between female and male patients used in our study for the variations of expression of PLA2G3, PLA2G2D and PLA2G5 (data not shown).
Euclidean distance is commonly used to evaluate linkages in the expression of different genes. We used this method to point out linkages between the variations in expression level of the most relevant genes. In left-sided adenocarcinomas (Figure 5A), a first cluster (cluster I) of upregulated genes was observed containing PLA2G3 and several genes related to colon cancer such as HD-6, MMP-7 and Il-8. A second cluster (cluster II) of several downregulated genes, including SFRP-1, PLA2G2D, RLPA-1, PLA2G5, PLA2G4A and ptgs1, was observed. These two clusters appeared most likely to discriminate adenocarcinomas from normal tissues. Remarkably, there are 3 sPLA2 genes out of 11 genes in these two clusters. The other genes did not show any linkage with colon tumorigenesis, since their expression levels were up- or downregulated or not changed among the different patients. When looking at right-sided samples (Figure 5B), similar patterns were observed even though the number of patients was lower.
Protein expression levels of sPLA2-IID, sPLA2-III and sPLA2-V in colon adenocarcinomas and normal matched mucosa
To confirm that the variation of expression for PLA2G2D, PLA2G3 and PLA2G5 is also observed at the protein level, immunohistochemical analyses were performed on tissue sections from the same patients as those used for qPCR. For each sPLA2 protein analysed, tissue sections from three or four patients showing a significant increase or decrease of sPLA2 expression were selected and immunostained (Figure 6). The labelling for sPLA2-IID and sPLA2-V was markedly decreased in tumour cells compared to the normal matched epithelium, in accordance with the qPCR data. By contrast, the labelling for sPLA2-III was absent or very low in the normal epithelium, with a significant increase in tumour tissue. The absence of labelling in competition experiments (data not shown) or when the primary antibody was omitted (Figure 6) demonstrated that the signals observed for the three sPLA2 proteins were specific. In addition, immunohistochemical analysis of COX-2 showed a more intense protein expression in tumours than in normal mucosa in a subset of patients (data not shown).
Secreted phospholipase A2 immunolabelling in representative colon adenocarcinomas and normal matched mucosa. For sPLA2-IID and sPLA2-V expression, a strong staining in the surface epithelium of the normal mucosa was observed, contrasting with the weak or absent staining observed in tumour cells. For sPLA2-III expression, a very faint staining was observed in normal epithelial cells, contrasting with the moderate to strong staining observed in tumour cells. For each sPLA2, a representative immunolabelling from 1 patient out of 3–4 patients analysed is shown. As shown in the bottom picture, no staining is observed when the primary antibody is omitted. Scale bar is 100 μm.
Discussion
Several lines of evidence have been accumulated during the past decade to support the role of sPLA2s in cancer pathogenesis. Their role in human cancer, however, has not been clarified. As a first step towards addressing this issue, we have analysed the expression patterns of the full set of human sPLA2s in colorectal cancer tissue samples and normal matched mucosa. Our results indicate that (i) several sPLA2s, including sPLA2-IIA, sPLA2-X and sPLA2-XIIA, are highly expressed in both normal and tumour colon tissues; (ii) the expression levels of sPLA2-III, sPLA2-IID and sPLA2-V are dramatically altered in adenocarcinomas at both mRNA and protein levels; and (iii) their mRNA profiles are part of gene expression clusters with other genes associated with inflammation and cancer. Together, our data are further suggestive of a role of these sPLA2s in colorectal cancer and open the possibility that sPLA2s, in particular sPLA2-III, may provide novel cancer biomarkers.
sPLA2 gene expression levels in colon adenocarcinomas and normal human colon
Colon adenocarcinomas analysed in this study are likely cancers without high microsatellite instability. Indeed, we used immunohistochemical analysis as a reliable method for screening DNA mismatch repair defects (Lindor et al, 2002), and found that the expression of hMLH1 and hMSH2 was unchanged. Furthermore, we analysed the normal mucosa and the tumour tissues from the right and left colon separately because of their distinct gene expression patterns (Glebov et al, 2003; Birkenkamp-Demtroder et al, 2005). We observed similar levels of expression for most sPLA2s in left and right normal mucosa, with PLA2G2A having a high expression level, PLA2G3 being not detectable in most samples and the other sPLA2 genes showing intermediate levels of expression (Figure 1). Interestingly, we observed marked alterations in the expression levels of PLA2G2D, PLA2G5 and PLA2G3 in colon adenocarcinomas. In contrast, there was no difference in the expression levels of the other sPLA2 genes (Figure 2, 3 and 4). The absence of tumour-related alterations in the gene expression of PLA2G2A and PLA2G10 in human sporadic colon cancer tissues is consistent with earlier studies (Dimberg et al, 1998; Osterstrom et al, 2002; Murakami et al, 2005). These data obtained in humans differ from those obtained in mice, which showed an increased expression of PLA2G2A and no variation in PLA2G5 expression in tumours from azoxymethane-treated mice (Ilsley et al, 2005).
Expression level of genes involved in inflammation and tumorigenesis in colon adenocarcinomas and normal human colon
No significant changes between adenocarcinomas and normal colon were observed for most inflammation-related genes. It should be noted that many of these genes were expressed at high levels within the normal mucosa, in particular, MMP-9, PLA2G6 and ptgs2. A recent study by Chen et al (2004) has also shown high mRNA expression levels of several inflammation-related genes in normal-appearing colon mucosa of patients with colon cancer. Therefore, our data would suggest a possible pre-existing inflammatory condition within the normal mucosa distant from the tumours, and likely explain the absence of increased expression in adenocarcinomas vs normal mucosa for several inflammation-related genes. The slight decrease in ptgs1 (the COX-1 gene) appeared in agreement with that observed in colon adenocarcinomas of stage III (Duke's C) patients (Church et al, 2004). The COX-1 protein is considered to exert dual opposing effects in cancer, acting as either a tumour suppressor or a tumour initiator (Chulada et al, 2000). The slight decrease in PLA2G4A expression that we observed may be related to the dual opposing effects of cPLA2-IVA in cancer, that is, proliferative effects via metabolism of AA into eicosanoids, such as PGE2, and antiproliferative effects via AA-dependent ceramide production leading to apoptosis (Ilsley et al, 2005). The absence of increase in ptgs2 (the COX-2 gene) levels in our set of patients is in accordance with two recent qPCR studies also performed on patients with colon cancer (Church et al, 2004; Gustafsson et al, 2007), and may be related to the inflammatory status of the normal mucosa discussed above. The fact that we did not observe an increase of COX-2 at the mRNA level, while we detected an overexpression at the protein level by immunohistochemistry as previously reported (Wendum et al, 2003), is in line with the post-transcriptional regulation of COX-2 expression (Dixon et al, 2003). Therefore, mRNA and protein levels of COX-2 may not be closely linked, as recently proposed in colon cancer tissues (Gustafsson et al, 2007) and colon cancer cells (Dixon et al, 2003).
Downregulation of sPLA2-IID and sPLA2-V expression in human colon adenocarcinomas
A marked decrease in the expression level of PLA2G2D and PLA2G5 was observed in both left- and right-sided adenocarcinomas (Figure 2, 3 and 4). These variations were also observed at the protein level by immunohistochemical analyses. Indeed, sPLA2-IID and sPLA2-V were found to be present in epithelial cells of normal mucosa, and their expression was markedly reduced in tumours (Figure 6). The decreased expression of sPLA2-IID and sPLA2-V in tumours may suggest a protective role of these sPLA2s, as it has been proposed for sPLA2-IIA in mice (MacPhee et al, 1995; Cormier et al, 1997). A similar decrease in expression of sPLA2-IID and sPLA2-V was also described in gastric tissues with signet-ring cell carcinoma (Masuda et al, 2005a). Interestingly, the PLA2G2A, PLA2G2C, PLA2G2D, PLA2G2E, PLA2G2F and PLA2G5 genes reside within the same region of human chromosome 1 at p35–36.1 (Valentin et al, 2000), a region frequently altered in colorectal cancer (Spirio et al, 1996). The decreased expression for PLA2G2D and PLA2G5 appears to be linked (cluster II, Figure 5) to that observed for PLA2G4A, ptgs1, SFRP-1 and RLPA-1, which have been proposed as tumour suppressor genes in colon cancer (Chulada et al, 2000; Shida et al, 2004; Suzuki et al, 2004; Dong et al, 2005).
Upregulation of PLA2G3 and Wnt target genes in human colon adenocarcinomas
A marked increase in sPLA2-III expression level was observed in both left- and right-sided adenocarcinomas, a finding that was confirmed by immunohistochemical analysis. No or very weak sPLA2-III expression was observed in normal epithelial cells, but a robust expression was observed in tumours (Figure 6). Our findings are consistent with the recent observation that sPLA2-III can trigger the proliferation of human colon cancer cells in vitro (Murakami et al, 2005). Parallel to the increase in PLA2G3 gene expression level, we observed an increase in the expression level of four target genes of the Wnt/β-cat/Tcf-4 pathway: Il-8 (Levy et al, 2002), HD-6 (also called defensin α6) (Kolligs et al, 2002), MMP-7 (also called matrilysin) (Nelson et al, 2000) and EPR-1 (also called survivin) (Kolligs et al, 2002), as well as a concomitant dramatic decrease in SFRP-1 gene expression level. Therefore, our data are consistent with the activation of the Wnt/β-cat/Tcf-4 pathway in the development of colon adenocarcinomas. It will be of interest to determine whether the expression of PLA2G3 is related to the activation of the Wnt/β-cat/Tcf-4 pathway, as already suggested for PLA2G2A in gastric cancer (Aggarwal et al, 2006).
Our data further support the role of LPA in the pathogenesis of colon cancer. LPA exerts its effects through at least three different receptors: RLPA-1, RLPA-2 and RLPA-3 (Mills and Moolenaar, 2003). It has been demonstrated that the Wnt/β-cat/Tcf-4 pathway is involved in the proliferative effects of LPA through binding to RLPA-2 (Yang et al, 2005). We observed a decreased expression of RLPA-1 and a sustained expression of RLPA-2, which is in agreement with the predominant expression of RLPA-2 in adenocarcinomas (Shida et al, 2004). Whether sPLA2-III plays a role in the production of LPA, which in turn activates RLPA-2, remains to be established.
The sPLA2-III as a novel potential biomarker of human colon cancer
Because of their upregulation during colorectal carcinogenesis, Wnt target genes and their associated products have been examined for their potential use as biomarkers. The level of Il-8 protein was found to be increased in colorectal cancer patients (Terada et al, 2005). A significant increase in the level of defensin α6 has also been found in patients with colon cancer (Nam et al, 2005). Although Il-8 and defensin α6 levels have been recently proposed as markers of human colorectal cancer (Nam et al, 2005; Terada et al, 2005), our data show that they would detect only left-sided adenocarcinomas (Figure 3, 4 and 5). In contrast, the increased expression of sPLA2-III was observed in both left and right colon adenocarcinomas, indicating that the analysis of sPLA2-III levels would detect cancers located in both left and right colon. MMP-7 is a matrix metalloprotease that has been associated with tumour invasion and metastasis (Nelson et al, 2000). We found that the expression pattern of PLA2G3 was more similar to that of MMP-7, which was also increased in both left and right colon adenocarcinomas (Figure 3, 4 and 5).
In conclusion, this work is the first comprehensive analysis of the expression pattern of the full set of sPLA2s in human colon cancer. The distinct expression pattern observed for sPLA2 genes suggests that mRNA profiling of the full set of human sPLA2s may be useful to detect colon tumours either by analysing their expression pattern in tumours (Barrier et al, 2005), in circulating blood cells (Burczynski et al, 2005) or directly in serum on circulating mRNA, as recently proposed for other genes (Li et al, 2006). Moreover, we have observed a dramatic increase in sPLA2-III expression in both left- and right-sided adenocarcinomas, suggesting that sPLA2-III may represent a novel broad molecular biomarker of colon cancer. It will be of interest to determine whether the expression level of sPLA2-III also increases at earlier stages of tumorigenesis, including adenomas. It will also be useful to detect the sPLA2-III protein in human colon biopsies, stools or serum using the recently time-resolved fluoroimmunoassays developed for the different human sPLA2s (Nevalainen et al, 2005).
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Aggarwal A, Guo DL, Hoshida Y, Yuen ST, Chu KM, So S, Boussioutas A, Chen X, Bowtell D, Aburatani H, Leung SY, Tan P (2006) Topological and functional discovery in a gene coexpression meta-network of gastric cancer. Cancer Res 66: 232–241
Andreu P, Colnot S, Godard C, Gad S, Chafey P, Niwa-Kawakita M, Laurent-Puig P, Kahn A, Robine S, Perret C, Romagnolo B (2005) Crypt-restricted proliferation and commitment to the Paneth cell lineage following Apc loss in the mouse intestine. Development 132: 1443–1451
Barrier A, Lemoine A, Boelle PY, Tse C, Brault D, Chiappini F, Breittschneider J, Lacaine F, Houry S, Huguier M, Van der Laan MJ, Speed T, Debuire B, Flahault A, Dudoit S (2005) Colon cancer prognosis prediction by gene expression profiling. Oncogene 24: 6155–6164
Birkenkamp-Demtroder K, Olesen SH, Sorensen FB, Laurberg S, Laiho P, Aaltonen LA, Orntoft TF (2005) Differential gene expression in colon cancer of the caecum versus the sigmoid and rectosigmoid. Gut 54: 374–384
Burczynski ME, Twine NC, Dukart G, Marshall B, Hidalgo M, Stadler WM, Logan T, Dutcher J, Hudes G, Trepicchio WL, Strahs A, Immermann F, Slonim DK, Dorner AJ (2005) Transcriptional profiles in peripheral blood mononuclear cells prognostic of clinical outcomes in patients with advanced renal cell carcinoma. Clin Cancer Res 11: 1181–1189
Chen LC, Hao CY, Chiu YS, Wong P, Melnick JS, Brotman M, Moretto J, Mendes F, Smith AP, Bennington JL, Moore D, Lee NM (2004) Alteration of gene expression in normal-appearing colon mucosa of APC(min) mice and human cancer patients. Cancer Res 64: 3694–3700
Chulada PC, Thompson MB, Mahler JF, Doyle CM, Gaul BW, Lee C, Tiano HF, Morham SG, Smithies O, Langenbach R (2000) Genetic disruption of Ptgs-1, as well as Ptgs-2, reduces intestinal tumorigenesis in Min mice. Cancer Res 60: 4705–4708
Church RD, Yu J, Fleshman JW, Shannon WD, Govindan R, McLeod HL (2004) RNA profiling of cyclooxygenases 1 and 2 in colorectal cancer. Br J Cancer 91: 1015–1018
Cormier RT, Hong KH, Halberg RB, Hawkins TL, Richardson P, Mulherkar R, Dove WF, Lander ES (1997) Secretory phospholipase Pla2g2a confers resistance to intestinal tumorigenesis. Nat Genet 17: 88–91
Cummings BS (2007) Phospholipase A2 as targets for anti-cancer drugs. Biochem Pharmacol 74: 949–959
Dimberg J, Samuelsson A, Hugander A, Soderkvist P (1998) Gene expression of cyclooxygenase-2, group II and cytosolic phospholipase A2 in human colorectal cancer. Anticancer Res 18: 3283–3287
Dixon DA, Balch GC, Kedersha N, Anderson P, Zimmerman GA, Beauchamp RD, Prescott SM (2003) Regulation of cyclooxygenase-2 expression by the translational silencer TIA-1. J Exp Med 198: 475–481
Dong M, Johnson M, Rezaie A, Ilsley JN, Nakanishi M, Sanders MM, Forouhar F, Levine J, Montrose DC, Giardina C, Rosenberg DW (2005) Cytoplasmic phospholipase A2 levels correlate with apoptosis in human colon tumorigenesis. Clin Cancer Res 11: 2265–2271
Fearon ER, Vogelstein B (1990) A genetic model for colorectal tumorigenesis. Cell 61: 759–767
Glebov OK, Rodriguez LM, Nakahara K, Jenkins J, Cliatt J, Humbyrd CJ, DeNobile J, Soballe P, Simon R, Wright G, Lynch P, Patterson S, Lynch H, Gallinger S, Buchbinder A, Gordon G, Hawk E, Kirsch IR (2003) Distinguishing right from left colon by the pattern of gene expression. Cancer Epidemiol Biomarkers Prev 12: 755–762
Gorovetz M, Baekelandt M, Berner A, Trope CG, Davidson B, Reich R (2006) The clinical role of phospholipase A2 isoforms in advanced-stage ovarian carcinoma. Gynecol Oncol 103: 831–840
Graff JR, Konicek BW, Deddens JA, Chedid M, Hurst BM, Colligan B, Neubauer BL, Carter HW, Carter JH (2001) Expression of group IIa secretory phospholipase A2 increases with prostate tumor grade. Clin Cancer Res 7: 3857–3861
Gustafsson A, Hansson E, Kressner U, Nordgren S, Andersson M, Wang W, Lonnroth C, Lundholm K (2007) EP1-4 subtype, COX and PPAR gamma receptor expression in colorectal cancer in prediction of disease-specific mortality. Int J Cancer 121: 232–240
Haas U, Podda M, Behne M, Gurrieri S, Alonso A, Furstenberger G, Pfeilschifter J, Lambeau G, Gelb MH, Kaszkin M (2005) Characterization and differentiation-dependent regulation of secreted phospholipases A in human keratinocytes and in healthy and psoriatic human skin. J Invest Dermatol 124: 204–211
Henderson Jr WR, Chi EY, Bollinger JG, Tien YT, Ye X, Castelli L, Rubtsov YP, Singer AG, Chiang GK, Nevalainen T, Rudensky AY, Gelb MH (2007) Importance of group X-secreted phospholipase A2 in allergen-induced airway inflammation and remodeling in a mouse asthma model. J Exp Med 204: 865–877
Ilsley JN, Nakanishi M, Flynn C, Belinsky GS, De Guise S, Adib JN, Dobrowsky RT, Bonventre JV, Rosenberg DW (2005) Cytoplasmic phospholipase A2 deletion enhances colon tumorigenesis. Cancer Res 65: 2636–2643
Kolligs FT, Bommer G, Goke B (2002) Wnt/beta-catenin/tcf signaling: a critical pathway in gastrointestinal tumorigenesis. Digestion 66: 131–144
Krause WF, DuBois RN (2001) The molecular basis for prevention of colorectal cancer. Clin Colorectal Cancer 1: 47–54
Laye JP, Gill JH (2003) Phospholipase A2 expression in tumours: a target for therapeutic intervention? Drug Discov Today 8: 710–716
Leung SY, Chen X, Chu KM, Yuen ST, Mathy J, Ji J, Chan AS, Li R, Law S, Troyanskaya OG, Tu IP, Wong J, So S, Botstein D, Brown PO (2002) Phospholipase A2 group IIA expression in gastric adenocarcinoma is associated with prolonged survival and less frequent metastasis. Proc Natl Acad Sci USA 99: 16203–16208
Levy L, Neuveut C, Renard CA, Charneau P, Branchereau S, Gauthier F, Van Nhieu JT, Cherqui D, Petit-Bertron AF, Mathieu D, Buendia MA (2002) Transcriptional activation of interleukin-8 by beta-catenin-Tcf4. J Biol Chem 277: 42386–42393
Li Y, Elashoff D, Oh M, Sinha U, St John MA, Zhou X, Abemayor E, Wong DT (2006) Serum circulating human mRNA profiling and its utility for oral cancer detection. J Clin Oncol 24: 1754–1760
Lindor NM, Burgart LJ, Leontovich O, Goldberg RM, Cunningham JM, Sargent DJ, Walsh-Vockley C, Petersen GM, Walsh MD, Leggett BA, Young JP, Barker MA, Jass JR, Hopper J, Gallinger S, Bapat B, Redston M, Thibodeau SN (2002) Immunohistochemistry versus microsatellite instability testing in phenotyping colorectal tumors. J Clin Oncol 20: 1043–1048
MacPhee M, Chepenik PK, Liddel AR, Nelson KK, Siracusa DL, Buchberg MA (1995) The secretory phospholipase A2 gene is a candidate for the mom1 locus, a major modifier of Apcmin-induced intestinal neoplasia. Cell 81: 957–966
Mallat Z, Steg PG, Benessiano J, Tanguy ML, Fox KA, Collet JP, Dabbous OH, Henry P, Carruthers KF, Dauphin A, Arguelles CS, Masliah J, Hugel B, Montalescot G, Freyssinet JM, Asselain B, Tedgui A (2005) Circulating secretory phospholipase A2 activity predicts recurrent events in patients with severe acute coronary syndromes. J Am Coll Cardiol 46: 1249–1257
Masuda S, Murakami M, Ishikawa Y, Ishii T, Kudo I (2005a) Diverse cellular localizations of secretory phospholipase A2 enzymes in several human tissues. Biochim Biophys Acta 1736: 200–210
Masuda S, Murakami M, Mitsuishi M, Komiyama K, Ishikawa Y, Ishii T, Kudo I (2005b) Expression of secretory phospholipase A2 enzymes in lungs of humans with pneumonia and their potential prostaglandin-synthetic function in human lung-derived cells. Biochem J 387: 27–38
Mills GB, Moolenaar WH (2003) The emerging role of lysophosphatidic acid in cancer. Nat Rev Cancer 3: 582–591
Morioka Y, Ikeda M, Saiga A, Fujii N, Ishimoto Y, Arita H, Hanasaki K (2000) Potential role of group X secretory phospholipase A2 in cyclooxygenase-2-dependent PGE2 formation during colon tumorigenesis. FEBS Lett 487: 262–266
Murakami M, Masuda S, Shimbara S, Ishikawa Y, Ishii T, Kudo I (2005) Cellular distribution, post-translational modification, and tumorigenic potential of human group III secreted phospholipase A(2). J Biol Chem 280: 24987–24998
Nam MJ, Kee MK, Kuick R, Hanash SM (2005) Identification of defensin alpha6 as a potential biomarker in colon adenocarcinoma. J Biol Chem 280: 8260–8265
Nelson AR, Fingleton B, Rothenberg ML, Matrisian LM (2000) Matrix metalloproteinases: biologic activity and clinical implications. J Clin Oncol 18: 1135–1149
Nevalainen TJ, Eerola LI, Rintala E, Laine VJ, Lambeau G, Gelb MH (2005) Time-resolved fluoroimmunoassays of the complete set of secreted phospholipases A2 in human serum. Biochim Biophys Acta 1733: 210–223
Osterstrom A, Dimberg J, Fransen K, Soderkvist P (2002) Expression of cytosolic and group X secretory phospholipase A(2) genes in human colorectal adenocarcinomas. Cancer Lett 182: 175–182
Rakoff-Nahoum S, Medzhitov R (2007) Regulation of spontaneous intestinal tumorigenesis through the adaptor protein MyD88. Science 317: 124–127
Rouault M, Bollinger JG, Lazdunski M, Gelb MH, Lambeau G (2003) Novel mammalian group XII secreted phospholipase A2 lacking enzymatic activity. Biochemistry 42: 11494–11503
Rouault M, Le Calvez C, Boilard E, Surrel F, Singer A, Ghomashchi F, Bezzine S, Scarzello S, Bollinger J, Gelb MH, Lambeau G (2007) Recombinant production and properties of binding of the full set of mouse secreted phospholipases A2 to the mouse M-type receptor. Biochemistry 46: 1647–1662
Shida D, Watanabe T, Aoki J, Hama K, Kitayama J, Sonoda H, Kishi Y, Yamaguchi H, Sasaki S, Sako A, Konishi T, Arai H, Nagawa H (2004) Aberrant expression of lysophosphatidic acid (LPA) receptors in human colorectal cancer. Lab Invest 84: 1352–1362
Smith MW, Yue ZN, Geiss GK, Sadovnikova NY, Carter VS, Boix L, Lazaro CA, Rosenberg GB, Bumgarner RE, Fausto N, Bruix J, Katze MG (2003) Identification of novel tumor markers in hepatitis C virus-associated hepatocellular carcinoma. Cancer Res 63: 859–864
Spirio LN, Kutchera W, Winstead MV, Pearson B, Kaplan C, Robertson M, Lawrence E, Burt RW, Tischfield JA, Leppert MF, Prescott SM, White R (1996) Three secretory phospholipase A2 genes that map to human chromosome 1P35–36 are not mutated in individuals with attenuated adenomatous polyposis coli. Cancer Res 56: 955–958
Suzuki H, Watkins DN, Jair KW, Schuebel KE, Markowitz SD, Chen WD, Pretlow TP, Yang B, Akiyama Y, Van Engeland M, Toyota M, Tokino T, Hinoda Y, Imai K, Herman JG, Baylin SB (2004) Epigenetic inactivation of SFRP genes allows constitutive WNT signaling in colorectal cancer. Nat Genet 36: 417–422
Sved P, Scott KF, McLeod D, King NJ, Singh J, Tsatralis T, Nikolov B, Boulas J, Nallan L, Gelb MH, Sajinovic M, Graham GG, Russell PJ, Dong Q (2004) Oncogenic action of secreted phospholipase A2 in prostate cancer. Cancer Res 64: 6934–6940
Terada H, Urano T, Konno H (2005) Association of interleukin-8 and plasminogen activator system in the progression of colorectal cancer. Eur Surg Res 37: 166–172
Valentin E, Singer AG, Ghomashchi F, Lazdunski M, Gelb MH, Lambeau G (2000) Cloning and recombinant expression of human group IIF secreted phospholipase A2. Biochem Biophys Res Commun 279: 223–228
Wendum D, Svrcek M, Rigau V, Boelle PY, Sebbagh N, Parc R, Masliah J, Trugnan G, Flejou JF (2003) COX-2, inflammatory secreted PLA2, and cytoplasmic PLA2 protein expression in small bowel adenocarcinomas compared with colorectal adenocarcinomas. Mod Pathol 16: 130–136
Wheatley SP, McNeish IA (2005) Survivin: a protein with dual roles in mitosis and apoptosis. Int Rev Cytol 247: 35–88
Wiesner GL, Daley D, Lewis S, Ticknor C, Platzer P, Lutterbaugh J, MacMillen M, Baliner B, Willis J, Elston RC, Markowitz SD (2003) A subset of familial colorectal neoplasia kindreds linked to chromosome 9q22.2–31.2. Proc Natl Acad Sci USA 100: 12961–12965
Williams NS, Gaynor RB, Scoggin S, Verma U, Gokaslan T, Simmang C, Fleming J, Tavana D, Frenkel E, Becerra C (2003) Identification and validation of genes involved in the pathogenesis of colorectal cancer using cDNA microarrays and RNA interference. Clin Cancer Res 9: 931–946
Wootton PT, Arora NL, Drenos F, Thompson SR, Cooper JA, Stephens JW, Hurel SJ, Hurt-Camejo E, Wiklund O, Humphries SE, Talmud PJ (2007) Tagging SNP haplotype analysis of the secretory PLA2-V gene, PLA2G5, shows strong association with LDL and oxLDL levels, suggesting functional distinction from sPLA2-IIA: results from the UDACS study. Hum Mol Genet 16: 1437–1444
Yan M, Rerko RM, Platzer P, Dawson D, Willis J, Tong M, Lawrence E, Lutterbaugh J, Lu S, Willson JK, Luo G, Hensold J, Tai HH, Wilson K, Markowitz SD (2004) 15-Hydroxyprostaglandin dehydrogenase, a COX-2 oncogene antagonist, is a TGF-beta-induced suppressor of human gastrointestinal cancers. Proc Natl Acad Sci USA 101: 17468–17473
Yanaru-Fujisawa R, Matsumoto T, Kukita Y, Nakamura S, Yao T, Hayashi K, Iida M (2007) Impact of phospholipase A2 group IIa gene polymorphism on phenotypic features of patients with familial adenomatous polyposis. Dis Colon Rectum 50: 223–231
Yang M, Zhong WW, Srivastava N, Slavin A, Yang J, Hoey T, An S (2005) G protein-coupled lysophosphatidic acid receptors stimulate proliferation of colon cancer cells through the {beta}-catenin p. Proc Natl Acad Sci USA 102: 6027–6032
Acknowledgements
We thank Mrs Sylvie Dumont for helping in IHC experiments, the Cancer Est Tissue Bank for providing some of the tissue samples and Dr Glenn Belinsky for preparing some colon tumour specimens. Dr Bernard Mari and Dr Claude Auriault are greatly acknowledged for fruitful discussions. This work was supported in part by the Centre National de la Recherche Scientifique (CNRS) to GL, the Association pour la Recherche sur le Cancer (ARC) to GL and the NIH Grant CA-114635 to DWR.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Mounier, C., Wendum, D., Greenspan, E. et al. Distinct expression pattern of the full set of secreted phospholipases A2 in human colorectal adenocarcinomas: sPLA2-III as a biomarker candidate. Br J Cancer 98, 587–595 (2008). https://doi.org/10.1038/sj.bjc.6604184
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6604184
Keywords
This article is cited by
-
Identifying prognostic characteristics of m6A-related glycolysis gene and predicting the immune infiltration landscape in bladder cancer
Cancer Cell International (2023)
-
Interplay between C1-inhibitor and group IIA secreted phospholipase A2 impairs their respective function
Immunologic Research (2023)
-
Simulating the restoration of normal gene expression from different thyroid cancer stages using deep learning
BMC Cancer (2022)
-
Group III phospholipase A2 downregulation attenuated survival and metastasis in ovarian cancer and promotes chemo-sensitization
Journal of Experimental & Clinical Cancer Research (2021)
-
Differential effects of sPLA2-GV and GX on cellular proliferation and lipid accumulation in HT29 colon cancer cells
Molecular and Cellular Biochemistry (2018)