Abstract
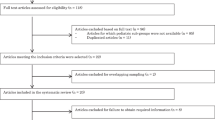
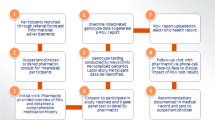
Warfarin is used in paediatric populations, but dosing algorithms incorporating pharmacogenetic data have not been developed for children. Previous studies have produced estimates of the effect of polymorphisms in Cytochrome P450 2C9 (CYP2C9) and vitamin K epoxide reductase complex subunit 1 (VKORC1) on stable warfarin dosing, but data on time in therapeutic range, initial dosing and adverse effects are limited. Participants (n=97) were recruited, and routine clinical data and salivary DNA samples were collected from all participants and analysed for CYP2C9*2, *3 and VKORC1-1639 polymorphisms.VKORC1 -1639 was associated with a greater proportion of the first 6 months’ treatment time spent within the target International Normalised Ratio (INR) range, accounting for an additional 9.5% of the variance in the proportion of time. CYP2C9*2 was associated with a greater likelihood of INR values exceeding the target range during the initiation of treatment (odds ratio (OR; per additional copy) 4.18, 95% confidence interval (CI) 1.42, 12.34). CYP2C9*2 and VKORC1-1639 were associated with a lower dose requirement, and accounted for almost 12% of the variance in stable dose. VKORC1-1639 was associated with an increased likelihood of mild bleeding complications (OR (heterozygotes vs homozygotes) 4.53, 95% CI 1.59, 12.93). These data show novel associations between VKORC1-1639 and CYP2C9*2 and INR values in children taking warfarin, as well as replicating previous findings with regard to stable dose requirements. The development of pharmacogenomic dosing algorithms for children using warfarin has the potential to improve clinical care in this population.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Monagle P, Michelson AD, Bovill E, Andrew M . Antithrombotic therapy in children. Chest 2001; 119: 344S–370S.
the British Committee for Standards in Haemotology Baglin TP, Keeling DM, Watson HG . Guidelines on oral anticoagulation: third edition. Br J Haematol 1998; 101: 374–387.
Andrew M, Marzinotto V, Brooker LA, Adams M, Ginsberg J, Freedom R et al. Oral anticoagulation therapy in pediatric-patients—a prospective-study. Thromb Haemost 1994; 71: 265–269.
Buck ML . Anticoagulation with warfarin in infants and children. Ann Pharmacother 1996; 30: 1316–1322.
Streif W, Andrew M, Marzinotto V, Massicotte P, Chan AKC, Julian JA et al. Analysis of warfarin therapy in pediatric patients: a prospective cohort study of 319 patients. Blood 1999; 94: 3007–3014.
Bonduel M, Sciuccati G, Hepner M, Torres AF, Pieroni G, Frontroth JP et al. Acenocoumarol therapy in pediatric patients. J Thromb Haemost 2003; 1: 1740–1743.
Tait RC, Ladusans EJ, ElMetaal M, Patel RG, Will AM . Oral anticoagulation in paediatric patients: dose requirements and complications. Arch Dis Child 1996; 74: 228–231.
Wadelius M, Pirmohamed M . Pharmacogenetics of warfarin: current status and future challenges. Pharmacogenomics J 2007; 7: 99–111.
Klein TE, Altman RB, Eriksson N, Gage BF, Kimmel SE, Lee MTM et al. Estimation of the warfarin dose with clinical and pharmacogenetic data. N Engl J Med 2009; 360: 753–764.
Sconce EA, Khan TI, Wynne HA, Avery P, Monkhouse L, King BP et al. The impact of CYP2C9 and VKORC1 genetic polymorphism and patient characteristics upon warfarin dose requirements: proposal for a new dosing regimen. Blood 2005; 106: 2329–2333.
Li C, Schwarz UI, Ritchie MD, Roden DM, Stein CM, Kurnik D . Relative contribution of CYP2C9 and VKORC1 genotypes and early INR response to the prediction of warfarin sensitivity during initiation of therapy. Blood 2009; 113: 3925–3930.
Limdi N, McGwin G, Goldstein JA, Beasley TM, Arnett DK, Adler BK et al. Influence of CYP2C9 and VKORC1 1173C/T genotype on the risk of hemorrhagic complications in African-American and European-American patients on warfarin. Clin Pharmacol Ther 2008; 83: 312–321.
Limdi NA, Karnett D, Goldstein JA, Beasley TM, McGwin G, Adler BK et al. Influence of CYP2C9 and VKORC1 on warfarin dose, anticoagulation attainment and maintenance among European-Americans and African-Americans. Pharmacogenomics 2008; 9: 511–526.
Obayashi K, Nakamura K, Kawana J, Ogata H, Hanada K, Kurabayashi M et al. VKORC1 gene variations are the major contributors of variation in warfarin dose in Japanese patients. Clin Pharmacol Ther 2006; 80: 169–178.
Rieder MJ, Reiner AP, Gage BF, Nickerson DA, Eby CS, McLeod HL et al. Effect of VKORC1 haplotypes on transcriptional regulation and warfarin dose. N Engl J Med 2005; 352: 2285–2293.
Veenstra DL, You JHS, Rieder MJ, Farin FM, Wilkerson HW, Blough DK et al. Association of Vitamin K epoxide reductase complex 1 (VKORC1) variants with warfarin dose in a Hong Kong Chinese patient population. Pharmacogenet Genomics 2005; 15: 687–691.
Cavallari LH, Momary KM, Patel SR, Shapiro NL, Nutescu E, Viana MAG . Pharmacogenomics of warfarin dose requirements in Hispanics. Blood Cells Mol Dis 2011; 46: 147–150.
Jorgensen AL, Al-Zubiedi S, Zhang JE, Keniry A, Hanson A, Hughes DA et al. Genetic and environmental factors determining clinical outcomes and cost of warfarin therapy: a prospective study. Pharmacogenet Genomics 2009; 19: 800–812.
Tan G-M, Wu E, Lam Y-Y, Yan BP . Role of warfarin pharmacogenetic testing in clinical practice. Pharmacogenomics 2010; 11: 439–448.
You JHS, Wong RSM, Waye MMY, Mu YW, Lim CK, Choi KC et al. Warfarin dosing algorithm using clinical, demographic and pharmacogenetic data from Chinese patients. J Thromb Thrombolysis 2011; 31: 113–118.
Pirmohamed M, Burnside G, Eriksson N, Jorgensen AL, Toh CH, Nicholson T et al. A randomized trial of genotype-guided dosing of warfarin. N Engl J Med 2013; 369: 2294–2303.
Manco-Johnson MJ . How I treat venous thrombosis in children. Blood 2006; 107: 21–29.
Payne JH . Aspects of anticoagulation in children. Br J Haematol 2010; 150: 259–277.
Thornburg CD, Jones E, Bomgaars L, Gage BF . Pediatric warfarin practice and pharmacogenetic testing. Thromb Res 2010; 126: E144–E146.
Biss TT, Avery PJ, Brandao LR, Chalmers EA, Williams MD, Grainger JD et al. VKORC1 and CYP2C9 genotype and patient characteristics explain a large proportion of the variability in warfarin dose requirement among children. Blood 2012; 119: 868–873.
Moreau C, Bajolle F, Siguret V, Lasne D, Golmard JL, Elie C et al. Vitamin K antagonists in children with heart disease: height and VKORC1 genotype are the main determinants of the warfarin dose requirement. Blood 2012; 119: 861–867.
Nowak-Gottl U, Dietrich K, Schaffranek D, Eldin NS, Yasui Y, Geisen C et al. In pediatric patients, age has more impact on dosing of vitamin K antagonists than VKORC1 or CYP2C9 genotypes. Blood 2010; 116: 6101–6105.
Biss TT, Avery PJ, Williams MD, BrandÃO LR, Grainger JD, Kamali F . The VKORC1 and CYP2C9 genotypes are associated with over-anticoagulation during initiation of warfarin therapy in children. J Thromb Haemost 2013; 11: 373–375.
Bradbury MJE, Taylor G, Short P, Williams MD . A comparative study of anticoagulant control in patients on long-term warfarin using home and hospital monitoring of the international normalised ratio. Arch Dis Child 2008; 93: 303–306.
Murray M, Keenan R, Billington R . Standard Operating Procedure (SOP) for the Management of Children on Warfarin at a Paediatric Regional Anticoagulation Centre. Alder Hey Children’s Hospital: Liverpool, 2005.
Rosendaal FR, Cannegieter SC, Van der Meer FJM, Briet E . A method to determine the optimal intensity of oral anticoagulant therapy. Thromb Haemost 1993; 69: 236–239.
Fihn SD, Callahan CM, Martin DC, McDonell MB, Henikoff JG, White RH . The risk for and severity of bleeding complications in elderly patients treated with warfarin. The National Consortium of Anticoagulation Clinics. Ann Intern Med 1996; 124: 970–979.
R Development Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing: Vienna, Austria, 2011.
van Buuren S, Groothuis-Oudshoorn K . mice: Multivariate Imputation by Chained Equations in R. J Stat Softw 45: 1–67.
Benjamini Y, Hochberg Y . Controlling the false discovery rate—a practical and powerful approach to multiple testing. J R Statist Soc B 1995; 57: 289–300.
Koukouritaki SB, Manro JR, Marsh SA, Stevens JC, Rettie AE, McCarver DG et al. Developmental expression of human hepatic CYP2C9 and CYP2C19. J Pharmacol Exp Ther 2004; 308: 965–974.
Schwarz UI, Ritchie MD, Bradford Y, Li C, Dudek SM, Frye-Anderson A et al. Genetic determinants of response to warfarin during initial anticoagulation. N Engl J Med 2008; 358: 999–1008.
Heneghan C, Ward A, Perera R, Bankhead C, Fuller A, Stevens R et al. Self-monitoring of oral anticoagulation: systematic review and meta-analysis of individual patient data. Lancet 379: 322–334.
Sanderson S, Emery J, Higgins J . CYP2C9 gene variants, drug dose, and bleeding risk in warfarin-treated patients: a HuGEnet[trade] systematic review and meta-analysis. Genet Med 2005; 7: 97–104.
Jorgensen AL, FitzGerald RJ, Oyee J, Pirmohamed M, Williamson PR . Influence of CYP2C9 and VKORC1 on patient response to warfarin: a systematic review and meta-analysis. PLoS One 2012; 7: e44064.
Kimmel SE, French B, Kasner SE, Johnson JA, Anderson JL, Gage BF et al. A pharmacogenetic versus a clinical algorithm for warfarin dosing. N Engl J Med 2013; 369: 2283–2293.
Acknowledgements
This work was funded by the MRC Centre for Drug Safety Science (CDSS) at the University of Liverpool and the Department of Health Chair in Pharmacogenetics.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the The Pharmacogenomics Journal website
Supplementary information
PowerPoint slides
Rights and permissions
About this article
Cite this article
Hawcutt, D., Ghani, A., Sutton, L. et al. Pharmacogenetics of warfarin in a paediatric population: time in therapeutic range, initial and stable dosing and adverse effects. Pharmacogenomics J 14, 542–548 (2014). https://doi.org/10.1038/tpj.2014.31
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tpj.2014.31
This article is cited by
-
Association between gene polymorphisms and initial warfarin therapy in patients after heart valve surgery
Pharmacological Reports (2024)
-
Deciphering Genetic Variants of Warfarin Metabolism in Children With Ventricular Assist Devices
Pediatric Cardiology (2021)
-
CYP2C9, VKORC1, and CYP4F2 polymorphisms and pediatric warfarin maintenance dose: a systematic review and meta-analysis
The Pharmacogenomics Journal (2020)
-
Height, VKORC1 1173, and CYP2C9 Genotypes Determine Warfarin Dose for Pediatric Patients with Kawasaki Disease in Southwest China
Pediatric Cardiology (2019)
-
Personalised Warfarin Dosing in Children Post-cardiac Surgery
Pediatric Cardiology (2019)