Abstract
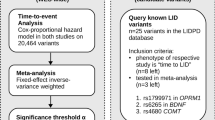
We implemented a two-step approach to detect potential predictor gene variants for neuroleptic-induced tardive dyskinesia (TD) in schizophrenic subjects. First, we screened associations by using a genome-wide (Illumina HumanHapCNV370) SNP array in 61 Japanese schizophrenia patients with treatment-resistant TD and 61 Japanese schizophrenia patients without TD. Next, we performed a replication analysis in 36 treatment-resistant TD and 138 non-TD subjects. An association of an SNP in the DPP6 (dipeptidyl peptidase-like protein-6) gene, rs6977820, the most promising association identified by the screen, was significant in the replication sample (allelic P=0.008 in the replication sample, allelic P=4.6 × 10−6, odds ratio 2.32 in the combined sample). The SNP is located in intron-1 of the DPP6 gene and the risk allele was associated with decreased DPP6 gene expression in the human postmortem prefrontal cortex. Chronic administration of haloperidol increased Dpp6 expression in mouse brains. DPP6 is an auxiliary subunit of Kv4 and regulates the properties of Kv4, which regulates the activity of dopaminergic neurons. The findings of this study indicate that an altered response of Kv4/DPP6 to long-term neuroleptic administration is involved in neuroleptic-induced TD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Browne S, Roe M, Lane A, Gervin M, Morris M, Kinsella A et al. Quality of life in schizophrenia: relationship to sociodemographic factors, symptomatology and tardive dyskinesia. Acta Psychiatr Scand 1996; 94: 118–124.
Rosenheck RA . Evaluating the cost-effectiveness of reduced tardive dyskinesia with second-generation antipsychotics. Br J Psychiatry 2007; 191: 238–245.
Tenback DE, van Harten PN, Slooff CJ, van Os J . Evidence that early extrapyramidal symptoms predict later tardive dyskinesia: a prospective analysis of 10,000 patients in the European Schizophrenia Outpatient Health Outcomes (SOHO) study. Am J Psychiatry 2006; 163: 1438–1440.
de Leon J . The effect of atypical versus typical antipsychotics on tardive dyskinesia: a naturalistic study. Eur Arch Psychiatry Clin Neurosci 2007; 257: 169–172.
Remington G . Tardive dyskinesia: eliminated, forgotten, or overshadowed? Curr Opin Psychiatry 2007; 20: 131–137.
Correll CU, Schenk EM . Tardive dyskinesia and new antipsychotics. Curr Opin Psychiatry 2008; 21: 151–156.
Inada T, Koga M, Ishiguro H, Horiuchi Y, Syu A, Yoshio T et al. Pathway-based association analysis of genome-wide screening data suggest that genes associated with the gamma-aminobutyric acid receptor signaling pathway are involved in neuroleptic-induced, treatment-resistant tardive dyskinesia. Pharmacogenet Genomics 2008; 18: 317–323.
Menza MA, Grossman N, Van Horn M, Cody R, Forman N . Smoking and movement disorders in psychiatric patients. Biol Psychiatry 1991; 30: 109–115.
Muller DJ, Shinkai T, De Luca V, Kennedy JL . Clinical implications of pharmacogenomics for tardive dyskinesia. Pharmacogenomics J 2004; 4: 77–87.
Malhotra AK, Murphy Jr GM, Kennedy JL . Pharmacogenetics of psychotropic drug response. Am J Psychiatry 2004; 161: 780–796.
Klawans HL, Goetz CG, Perlik S . Tardive dyskinesia: review and update. Am J Psychiatry 1980; 137: 900–908.
Gerlach J, Casey DE . Tardive dyskinesia. Acta Psychiatr Scand 1988; 77: 369–378.
Saito T, Ishizawa H, Tsuchiya F, Ozawa H, Takahata N . Neurochemical findings in the cerebrospinal fluid of schizophrenic patients with tardive dyskinesia and neuroleptic-induced parkinsonism. Jpn J Psychiatry Neurol 1986; 40: 189–194.
Haleem DJ . Serotonergic modulation of dopamine neurotransmission: a mechanism for enhancing therapeutics in schizophrenia. J Coll Physicians Surg Pak 2006; 16: 556–562.
Tammenmaa IA, McGrath JJ, Sailas E, Soares-Weiser K . Cholinergic medication for neuroleptic-induced tardive dyskinesia. Cochrane Database Syst Rev 2002: CD000207.
Arranz MJ, de Leon J . Pharmacogenetics and pharmacogenomics of schizophrenia: a review of last decade of research. Mol Psychiatry 2007; 12: 707–747.
Aberg K, Adkins DE, Bukszar J, Webb BT, Caroff SN, Miller del D et al. Genomewide association study of movement-related adverse antipsychotic effects. Biol Psychiatry 2010; 67: 279–282.
Greenbaum L, Alkelai A, Rigbi A, Kohn Y, Lerer B . Evidence for association of the GLI2 gene with tardive dyskinesia in patients with chronic schizophrenia. Mov Disord 2010; 25: 2809–2817.
Syu A, Ishiguro H, Inada T, Horiuchi Y, Tanaka S, Ishikawa M et al. Association of the HSPG2 gene with neuroleptic-induced tardive dyskinesia. Neuropsychopharmacology 2010; 35: 1155–1164.
Association AP . Diagnostic and Statistical Manual of Mental Disorders, 4th revision. American Psychiatric Association: Washington, DC 1994.
Itoh H, Yagi G, Ogita K, Ohtsuka N, Sakurai S, Tashiro I et al. Study on the efficacy and safety of treatment with anti-psychotic drugs: an international comparative examination. Annu Rep Pharmacopsychiatry Res Found 1977; 9: 218–225.
Schooler NR, Kane JM . Research diagnoses for tardive dyskinesia. Arch Gen Psychiatry 1982; 39: 486–487.
Ishiguro H, Koga M, Horiuchi Y, Noguchi E, Morikawa M, Suzuki Y et al. Supportive evidence for reduced expression of GNB1L in schizophrenia. Schizophr Bull 2008; 36: 756–765.
Koga M, Ishiguro H, Yazaki S, Horiuchi Y, Arai M, Niizato K et al. Involvement of SMARCA2/BRM in the SWI/SNF chromatin-remodeling complex in schizophrenia. Hum Mol Genet 2009; 18: 2483–2494.
Marshall CR, Noor A, Vincent JB, Lionel AC, Feuk L, Skaug J et al. Structural variation of chromosomes in autism spectrum disorder. Am J Hum Genet 2008; 82: 477–488.
van Es MA, van Vught PW, Blauw HM, Franke L, Saris CG, Van den Bosch L et al. Genetic variation in DPP6 is associated with susceptibility to amyotrophic lateral sclerosis. Nat Genet 2008; 40: 29–31.
Tsai HT, Caroff SN, Miller del D, McEvoy J, Lieberman JA, North KE et al. A candidate gene study of tardive dyskinesia in the CATIE schizophrenia trial. Am J Med Genet B Neuropsychiatr Genet 2010; 153B: 336–340.
Zagha E, Ozaita A, Chang SY, Nadal MS, Lin U, Saganich MJ et al. DPP10 modulates Kv4-mediated A-type potassium channels. J Biol Chem 2005; 280: 18853–18861.
Clark BD, Kwon E, Maffie J, Jeong HY, Nadal M, Strop P et al. DPP6 localization in brain supports function as a Kv4 channel associated protein. Front Mol Neurosci 2008; 1: 8.
Kim J, Nadal MS, Clemens AM, Baron M, Jung SC, Misumi Y et al. Kv4 accessory protein DPPX (DPP6) is a critical regulator of membrane excitability in hippocampal CA1 pyramidal neurons. J Neurophysiol 2008; 100: 1835–1847.
Nadal MS, Ozaita A, Amarillo Y, Vega-Saenz de Miera E, Ma Y, Mo W et al. The CD26-related dipeptidyl aminopeptidase-like protein DPPX is a critical component of neuronal A-type K+ channels. Neuron 2003; 37: 449–461.
Maffie J, Rudy B . Weighing the evidence for a ternary protein complex mediating A-type K+ currents in neurons. J Physiol 2008; 586 (Part 23): 5609–5623.
Zhang H, Rodgers EW, Krenz WD, Clark MC, Baro DJ . Cell specific dopamine modulation of the transient potassium current in the pyloric network by the canonical D1 receptor signal transduction cascade. J Neurophysiol 2010; 104: 873–884.
Hahn J, Tse TE, Levitan ES . Long-term K+ channel-mediated dampening of dopamine neuron excitability by the antipsychotic drug haloperidol. J Neurosci 2003; 23: 10859–10866.
Acknowledgements
This study was supported by grants from the Mitsubishi Pharma Research Foundation, Kakenhi 23390285, and the Collaborative Research Project (2011-2201) of the Brain Research Institute, Niigata University. Australian human brain tissues were provided by the NSW Tissue Resource Centre, which is supported by The University of Sydney, Neuroscience Institute of Schizophrenia and Allied Disorders, National Institute of Alcohol Abuse and Alcoholism and the NSW Department of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare that no financial support or compensation has been received from any individual or corporate entity over the past 3 years for research or professional service, and there are no personal financial holdings that could be perceived as constituting a potential conflict of interest.
Additional information
Supplementary Information accompanies the paper on the The Pharmacogenomics Journal website
Supplementary information
Rights and permissions
About this article
Cite this article
Tanaka, S., Syu, A., Ishiguro, H. et al. DPP6 as a candidate gene for neuroleptic-induced tardive dyskinesia. Pharmacogenomics J 13, 27–34 (2013). https://doi.org/10.1038/tpj.2011.36
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tpj.2011.36
Keywords
This article is cited by
-
Genome wide study of tardive dyskinesia in schizophrenia
Translational Psychiatry (2021)
-
Population structure and pharmacogenomic risk stratification in the United States
BMC Biology (2020)
-
The genetics of drug-related movement disorders, an umbrella review of meta-analyses
Molecular Psychiatry (2020)
-
Possible association between DBH 19 bp insertion/deletion polymorphism and clinical symptoms in schizophrenia with tardive dyskinesia
Journal of Neural Transmission (2015)
-
DPP6 gene disruption in a family with Gilles de la Tourette syndrome
neurogenetics (2014)