Abstract
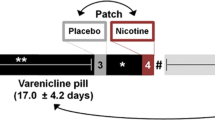
In prior studies we found that young, female smokers manifest poorer performance than non-smokers on attention-related tasks and that these findings can be moderated by variation in nicotinic acetylcholine receptor (nAChR) genes. We predicted that under controlled conditions (1) nicotine would improve functioning on attentional tasks in smokers who previously manifested relatively poor performance, and that (2) smokers who carry genetic variations associated with poorer attention performance would derive greater benefit from nicotine. To test these hypotheses, 31 young female smokers, who participated in our previous study, performed the Matching Familiar Figures Test (MFFT), Tower of London Test and Continuous Performance Task (CPT) in a double-blind, within-between subject design, placebo or nicotine (4 mg as gum) serving as the within factor and genetic profile as the between factor. Repeated measures ANCOVA controlling for attention deficit symptomatology, substance abuse and nicotine dependence showed better performance under nicotine among participants with higher levels of attention deficit symptoms (MFFT errors: P=0.04; CPT commissions: P=0.01) and nicotine dependence (CPT stability of response: P=0.04) and greater consumption of caffeine (CPT stability of response: P=0.04). An interactive effect of genetic profile was demonstrated for SNP rs2337980 in CHRNA7. These findings suggest that nicotine may have stronger short-term facilitating effects on attention in women who have more attention deficit symptoms and consume more nicotine and caffeine. This effect may be modified by a specific genetic make-up. Such individuals may be at increased risk for nicotine addiction and for greater difficulties in smoking cessation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Anderson P . Global use of alcohol, drugs and tobacco. Drug Alcohol Rev 2006; 25: 489–502.
World Health Organization. Report on the Global Tobacco Epidemic, 2008—the Mpower Package. World Health Organization: Geneva, Switzerland. (Available from: http://apps.who.int/bookorders/anglais/detart1.jsp?sesslan=1&codlan=1&codcol=93&codcch=220)
Israel Ministry of Health. Minister of Health Report About Smoking in Israel. Israel Ministry of Health: Jerusalem, Israel, 2007–2008. (Available from: http://www.health.gov.il/download/pages/smoke18052009.pdf (Hebrew))
US Centers for Disease Control and Prevention. Global Youth Tobacco Survey. US Centers for Disease Control and Prevention (CDC): Atlanta, GA, 2007. (Available from: http://www.cdc.gov/Tobacco/global/gyts/)
Payne S . Gender in Lung Cancer and Smoking Research. World Health Organization, Department of Gender, Women, Health Family and Community Health, 2005. (Available from: http://www.who.int/gender/documents/LungCancerlast2.pdf)
Israel Ministry of Health. Minister of Health Report About Smoking in Israel. Israel Ministry of Health: Jerusalem, Israel, 2004–2005. (Available from: http://www.health.gov.il/download/forms/a2752_ALL_310705.pdf (Hebrew))
Israel Ministry of Health. Minister of Health Report About Smoking in Israel. Israel Ministry of Health: Jerusalem, Israel, 2002–2003. (Available from: http://www.health.gov.il/Download/pages/isun2003.pdf (Hebrew))
Greenbaum L, Kanyas K, Karni O, Merbl Y, Olender T, Horowitz A et al. Why do young women smoke? I. Direct and interactive effects of environment, psychological characteristics and nicotinic cholinergic receptor genes. Mol Psychiatry 2006; 11: 312–322.
Lerer E, Kanyas K, Karni O, Ebstein R, Lerer B . Why do young women moke? II. Role of traumatic life experience, psychological characteristics and serotonergic genes. Mol Psychiatry 2006; 11: 771–781.
Yakir A, Rigbi A, Kanyas K, Pollak Y, Kahana G, Karni O et al. Why do young women smoke? III. Attention and impulsivity as neurocognitive predisposing factors. Eur Neuropsychopharmacol 2007; 17: 339–351.
Segman R, Kanyas K, Karni O, Lerer E, Goltser-Dubner T, Pavlov V et al. Why do young women smoke? IV. Role of genetic variation in the dopamine transporter and lifetime traumatic experience. Am J Med Genet B 2007; 144B: 533–540.
Rigbi A, Kanyas K, Yakir A, Greenbaum L, Pollak Y, Ben-Asher E et al. Why do young women smoke? V. Role of direct and interactive effects of nicotinic cholinergic receptor gene variation on neurocognitive function. Genes Brain Behav 2008; 7: 164–172.
Heishman SJ, Taylor RC, Hennigfield JE . Nicotine and smoking: a review of effects on human performance. Exp Clin Psychopharmacol 1994; 2: 345–395.
Heishman SJ . What aspects of human performance are truly enhanced by nicotine. Addiction 1998; 93: 317–320.
Levin DL, McClernon FG, Rezvani AH . Nicotine effects on cognitive function: behavioral characterization, pharmacological specification and anatomic localization. Psychopharmacology 2006; 184: 523–539.
Newhouse PA, Potter A, Singh A . Effects of nicotine stimulation on cognitive performance. Curr Opin Pharmacol 2004; 4: 36–46.
Sherwood N . Effects of nicotine on human psychomotor performance. Hum Psychopharmacol 1993; 8: 155–184.
Cincotta SL, Yorek MS, Moschak TM, Lewis SR, Rodefer JS . Selective nicotinic acetylcholine receptor agonists: potential therapies for neuropsychiatric disorders with cognitive dysfunction. Curr Opin Investig Drugs 2008; 9: 47–56.
Forgacs PB, Bodis-Wollner I . Nicotinic receptors and cognition in Parkinson's disease: the importance of neuronal synchrony. J Neural Transm 2004; 111: 1317–1331.
Ochoa EL, Lasalde-Dominicci J . Cognitive deficits in schizophrenia: focus on neuronal nicotinic acetylcholine receptors and smoking. Cell Mol Neurobiol 2007; 27: 609–639.
Sacco KA, Bannon KL, George TP . Nicotine receptor mechanisms and cognition in normal states and neuropsychiatric disorders. J Psychopharmacol 2004; 18: 457–474.
Wilens TE, Decker MW . Neuronal nicotinic receptor agonists for the treatment of attention-deficit/hyperactivity disorder: focus on cognition. Biochem Pharmacol 2007; 74: 1212–1223.
Kumari V, Postma P . Nicotine use in schizophrenia: the self medication hypotheses. Neurosci Biobehav Rev 2005; 29: 1021–1034.
Potter AS, Newhouse PA, Bucci DJ . Central nicotinic cholinergic systems: a role in the cognitive dysfunction in attention-deficit/hyperactivity disorder? Behav Brain Res 200615; 175: 201–211.
Mansvelder HD, van Aerde KI, Couey JJ, Brussaard AB . Nicotinic modulation of neuronal networks: from receptors to cognition. Psychopharmacology 2006; 184: 292–305.
Portugal GS, Gould TJ . Genetic variability in nicotinic acetylcholine receptors and nicotine addiction: converging evidence from human and animal research. Behav Brain Res 2008; 193: 1–16.
Espeseth T, Endestad T, Rootwelt H, Reinvang I . Nicotine receptor gene CHRNA4 modulates early event-related potentials in auditory and visual oddball target detection tasks. Neuroscience 2007; 147: 974–985.
Espeseth T, Greenwood PM, Reinvang I, Fjell AM, Walhovd KB, Westlye LT et al. Interactive effects of APOE and CHRNA4 on attention and white matter volume in healthy middle-aged and older adults. Cogn Affect Behav Neurosci 2006; 6: 31–43.
Greenwood PM, Fossella JA, Parasuraman R . Specificity of the effect of a nicotinic receptor polymorphism on individual differences in visuospatial attention. J Cogn Neurosci 2005; 17: 1611–1620.
Parasuraman R, Greenwood PM, Kumar R, Fossella J . Beyond heritability: neurotransmitter genes differentially modulate visuospatial attention and working memory. Psychol Sci 2005; 16: 200–207.
Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO . The Fagerström Test for Nicotine Dependence: a revision of the Fagerström Tolerance Questionnaire. Br J Addict 1991; 86: 1119–1127.
Kertzman S, Ben-Nahum Z, Sirota A . CogScan V4.0—Cognitive Scanning System. System Description. AnimaScan Ltd: Ashdod, Israel, 2003.
Brown TE . Brown Attention-Deficit Disorder Scales Manual. The Psychological Corporation: San Antonio, TX, 1996.
Murphy KR, Adler LA . Assessing attention-deficit/hyperactivity disorder in adults: focus on rating scales. J Clin Psychiatry 2004; 65 (Suppl 3): 12–17.
Barratt E . Barratt impulsiveness scale, version 11 (BSI-11). J Clin Psychol 1995; 51: 768–774.
Benowitz NL . Clinical pharmacology of nicotine: implications for understanding, preventing, and treating tobacco addiction. Clin Pharmacol Ther 2008; 83: 531–541.
Hukkanen J, Peyton III J, Benowitz NL . Metabolism and disposition kinetics of nicotine. Pharmacol Rev 2005; 57: 79–155.
Russel MAH . Nicotine intake by smokers: are rates of absorption or steady state levels more important?. In: Rand MJ, Thurau K (eds). The Pharmacology of Nicotine. IRL press: Oxford, UK, 1987, pp 375–402.
Kline P . An Easy Guide to Factor Analysis. Routledge: New York, NY, 1993.
Kollins SH, McClernon FJ, Fuemmeler BF . Association between smoking and attention-deficit/hyperactivity disorder symptoms in a population-based sample of young adults. Arch Gen Psychiatry 2005; 62: 1142–1147.
Pomerleau OF, Downey KK, Stelson FW, Pomerleau CS . Cigarette smoking in adult patients diagnosed with attention deficit hyperactivity disorder. J Subst Abuse 1995; 7: 373–378.
McClernon FJ, Kollins SH . ADHD and smoking: from genes to brain to behavior. Ann N Y Acad Sci 2008; 1141: 131–147.
Cauli O, Morelli M . Caffeine and the dopaminergic system. Behav Pharmacol 2005; 16: 63–77.
Swanson JA, Lee JW, Hopp JW . Caffeine and nicotine: a review of their joint use and possible interactive effects in tobacco withdrawal. Addict Behav 1994; 19: 229–256.
Riccio CA, Waldrop JJ, Reynolds CR, Lowe P . Effects of stimulants on the continuous performance test (CPT): implications for CPT use and interpretation. J Neuropsychiatry Clin Neurosci 2001; 13: 326–335.
Tucha O, Lange KW . Effects of nicotine chewing gum on a real-life motor task: a kinematic analysis of handwriting movements in smokers and non-smokers. Psychopharmacology (Berl) 2004; 173: 49–56.
Acknowledgements
This study was supported in part by a grant from the Professor Milton Rosenbaum Endowment Fund for Research in the Psychiatric Sciences (to YP).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the The Pharmacogenomics Journal website
Supplementary information
Rights and permissions
About this article
Cite this article
Rigbi, A., Yakir, A., Sarner-Kanyas, K. et al. Why do young women smoke? VI. A controlled study of nicotine effects on attention: pharmacogenetic interactions. Pharmacogenomics J 11, 45–52 (2011). https://doi.org/10.1038/tpj.2010.15
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tpj.2010.15
Keywords
This article is cited by
-
Associations between genetic variations and global motion perception
Experimental Brain Research (2019)