Abstract
Borderline personality disorder (BOR) is determined by environmental and genetic factors, and characterized by affective instability and impulsivity, diagnostic symptoms also observed in manic phases of bipolar disorder (BIP). Up to 20% of BIP patients show comorbidity with BOR. This report describes the first case–control genome-wide association study (GWAS) of BOR, performed in one of the largest BOR patient samples worldwide. The focus of our analysis was (i) to detect genes and gene sets involved in BOR and (ii) to investigate the genetic overlap with BIP. As there is considerable genetic overlap between BIP, major depression (MDD) and schizophrenia (SCZ) and a high comorbidity of BOR and MDD, we also analyzed the genetic overlap of BOR with SCZ and MDD. GWAS, gene-based tests and gene-set analyses were performed in 998 BOR patients and 1545 controls. Linkage disequilibrium score regression was used to detect the genetic overlap between BOR and these disorders. Single marker analysis revealed no significant association after correction for multiple testing. Gene-based analysis yielded two significant genes: DPYD (P=4.42 × 10−7) and PKP4 (P=8.67 × 10−7); and gene-set analysis yielded a significant finding for exocytosis (GO:0006887, PFDR=0.019; FDR, false discovery rate). Prior studies have implicated DPYD, PKP4 and exocytosis in BIP and SCZ. The most notable finding of the present study was the genetic overlap of BOR with BIP (rg=0.28 [P=2.99 × 10−3]), SCZ (rg=0.34 [P=4.37 × 10−5]) and MDD (rg=0.57 [P=1.04 × 10−3]). We believe our study is the first to demonstrate that BOR overlaps with BIP, MDD and SCZ on the genetic level. Whether this is confined to transdiagnostic clinical symptoms should be examined in future studies.
Similar content being viewed by others
Introduction
Borderline personality disorder (BOR; for the sake of readability, we have decided to use the rather unconventional abbreviation ‘BOR’ for Borderline Personality Disorder and the abbreviation ‘BIP’ for Bipolar Disorder) is a complex neuropsychiatric disorder with a lifetime prevalence of around 3%.1 Untreated cases often have a chronic and severely debilitating clinical course.1 BOR affects up to 20% of all psychiatric inpatients, and is associated with high health-care utilization. BOR therefore represents a substantial socio-economic burden.2, 3
BOR is characterized by affective instability, emotional dysregulation and poor interpersonal functioning.3 Suicide rates in BOR range between 6 and 8%, and up to 90% of patients engage in non-suicidal self-injurious behavior.4 Other prototypical features include high-risk behaviors and impulsive aggression. Current theories view dysfunctions in emotion processing, social interaction and impulsivity as core psychological mechanisms of BOR.5
To date, genetic research into BOR has been limited. Available genetic studies have involved small samples and focused on candidate genes, while no genome-wide association study (GWAS) of BOR patients has yet been performed.6 However, Lubke et al.7 conducted a GWAS of borderline personality features using data from three cohorts comprising n=5802, n=1332 and n=1301 participants, respectively. Using the borderline subscale of the Personality Assessment Inventory (PAI-BOR), four borderline personality features (affect instability, identity problems, negative relations and self-harm) were assessed. The most promising signal in the combined analysis of two samples was for seven SNPs in the gene SERINC5, which encodes a protein involved in myelination. Two of the SNPs could be replicated in the third sample. Interestingly, here, the effect was highest for the affect instability items, that is, features that are key characteristics of manic phases of bipolar disorder (BIP).
Understanding of the pathogenesis of BOR remains limited. Both environmental and genetic factors are known to have a role in BOR etiology. Familial aggregation has been demonstrated,8, 9 and heritability estimates from twin studies range from 35 to 65%, with higher heritability estimates being obtained with self-ratings.10, 11, 12
The potential comorbidity between BOR and BIP is part of an ongoing debate. For example, Fornaro et al.13 report substantial comorbidity of ~20% with BIP, whereas Tsanas et al.14 find clear symptomatic differences between these two diagnostic groups. BOR displays an overlap of some symptoms with BIP, such as affective instability. In contrast, features such as dissociative symptoms, a feeling of chronic emptiness and identity disturbances are specific to BOR.15 To date, no twin or family study has generated conclusive results concerning a genetic overlap between the two disorders.16, 17 However, a twin study18 and a large-population-based study using polygenic risk score analyses19 indicate a genetic overlap between borderline personality features and neuroticism, an established risk factor for BIP and other psychiatric disorders.20
To the best of our knowledge, the present study represents the first case–control GWAS in BOR, and was performed in one of the largest BOR patient samples worldwide. Given the limited heritability and the expected complex genetic architecture of BOR, the sample is too small to generate significant results for single markers. Instead, the main aim of the investigation was to detect (i) genes and gene sets with a potential involvement in BOR; and (ii) potential genetic overlap with BIP. As a substantial overlap of common risk variants exists between BIP and schizophrenia (SCZ), and to a lesser extent between BIP and major depressive disorder (MDD), and as there is also a high comorbidity of BOR and MDD, a further aim of the study was to determine whether any observed genetic overlap between BOR and BIP, MDD and SCZ was driven by disorder-specific genetic factors using linkage disequilibrium (LD)-score regression and polygenic risk scores (PRS).
Materials and methods
Participants
The present sample comprised 1075 BOR patients and 1675 controls.21 All the participants provided written informed consent before inclusion. The study was approved by the respective local ethics committees.
The patients were recruited at the following German academic institutions: Department of Psychosomatic Medicine, Central Institute of Mental Health, Mannheim (n=350); Department of Psychiatry and Psychotherapy, University Medical Center Mainz (n=231); and the Department of Psychiatry, Charité, Campus Benjamin Franklin, Berlin (n=494). Inclusion criteria for patients were: age 16 to 65 years; Central European ancestry; and a lifetime DSM-IV diagnosis of BOR. The control sample comprised 1583 unscreened blood donors from Mannheim, and 92 subjects recruited by the University Medical Center Mainz.
Clinical assessment
The diagnoses of BOR were assigned according to DSM-IV criteria and on the basis of structured clinical interviews. The diagnostic criteria for BOR were assessed using the German version of the IPDE22 or the SKID-II.23 All the diagnostic interviews were conducted by trained and experienced raters. BOR patients with a comorbid diagnosis of BIP or SCZ assessed with SKID-I23 were excluded.
Genotyping
Automated genomic DNA extraction was performed using the chemagic Magnetic Separation Module I (Chemagen Biopolymer-Technologie, Baesweiler, Germany). Genotyping was performed using the Infinium PsychArray-24 Bead Chip (Illumina, San Diego, CA, USA).
Quality control and imputation
A detailed description of the quality control and imputation procedures is provided elsewhere.24
Briefly, quality control parameters for the exclusion of subjects and single-nucleotide polymorphisms (SNPs) were: subject missingness >0.02; autosomal heterozygosity deviation (|Fhet|>0.2); SNP missingness >0.02; difference in SNP missingness between cases and controls >0.02; and SNP Hardy–Weinberg equilibrium (P<10−6 in controls; P<10−10 in cases).
Genotype imputation was performed using the pre-phasing/imputation stepwise approach in IMPUTE2/SHAPEIT (default parameters and a chunk size of 3 Mb),25, 26 using the 1000 Genomes Project reference panel (release ‘v3.macGT1’).27
Relatedness testing and population structure analysis were performed using a SNP subset that fulfilled strict quality criteria (INFO >0.8, missingness <1%, minor allele frequency >0.05), and which had been subjected to LD pruning (r2>0.02). This subset comprised 63 854 SNPs. In cryptically related subjects, one member of each pair (ðhat>0.2) was removed at random following the preferential retention of cases over controls. Principal components (PCs) were estimated from genotype data (see Supplementary Figures 1–6), and phenotype association was tested using logistic regression. The impact of the PCs on genome-wide test statistics was assessed using λ.
Association analysis
Including the first four PCs as covariates, an additive logistic regression model was used to test single marker associations, as implemented in PLINK.28 The P-value threshold for genome-wide significance was set at 5 × 10−8.
Gene-based analysis
To determine whether genes harbored an excess of variants with small P-values, a gene-based test was performed with MAGMA Version 1.04 (http://ctg.cncr.nl/software/magma)29 using genotyped markers only, filtered with a minor allele frequency >1% (n=284 220). This test uses summary data and takes LD between variants into account. SNPs within ±10 kb of the gene boundary were assigned to each gene. Obtained P-values were Bonferroni-corrected for the number of tested genes (n=17 755, P=2.8 × 10−6).
Gene-set analysis
Gene-set-based analysis was implemented using genotyped markers only, filtered as above. As in the gene-based analysis, SNPs within ±10 kb of the gene boundary were assigned to each gene. Gene-set analyses were carried out using Gene Ontology (GO, http://software.broadinstitute.org/gsea/msigdb/) terms.
The discovery gene-set-based analysis was carried out using i-GSEA4GWASv2 (http://gsea4gwas-v2.psych.ac.cn/).30 The size of the gene sets was restricted to 20–200 genes, and the major histocompatibility complex region was excluded. In total, 674 gene sets were tested. The results were adjusted for multiple testing using false discovery rate (FDR). To validate the significant finding, the respective gene set was investigated with (i) GSA-SNP, using the P-value of the second-best SNP in each gene (https://gsa.muldas.org)31 and (ii) MAGMA using summary data and a nominal P-value threshold of P<0.05.
LD-score regression
To investigate a possible genetic overlap between BOR and SCZ, BIP and MDD, LD-score regression was performed.32 Genetic correlations between BOR and (i) BIP, (ii) SCZ and (iii) MDD were calculated33 using the result files of the Psychiatric Genomics Consortium (PGC) meta-analyses for SCZ (33 640 cases and 43 456 controls),34 BIP (20 352 cases and 31 358 controls)35 and MDD (16 823 cases and 25 632 controls).35 There was no overlap in cases or controls of the present BOR GWAS sample with the PGC samples.
Polygenic risk score
To determine the impact of polygenic risk on BOR and subgroups (that is, BOR with and without MDD), PRS were calculated for each subject based on the above-mentioned PGC data sets.
To obtain a highly informative SNP set with minimal statistical noise, the following were excluded: low frequency SNPs (minor allele frequency <0.1); low-quality variants (imputation INFO <0.9) and indels. Subsequently, these SNPs were clumped discarding markers within 500 kb of, and in high LD (r2⩾0.1) with, another more significant marker. From the major histocompatibility complex region, only one variant with the strongest significance was retained. PRS were calculated as described elsewhere.36 This involved P-value thresholds 5 × 10−8, 1 × 10−6, 1 × 10−4, 0.001, 0.01, 0.05, 0.1, 0.2, 0.5 and 1.0, and multiplication of the natural logarithm of the odds ratio of each variant by the imputation probability for the risk allele. The resulting values were then totaled. For each subject, this resulted in one PRS for SCZ, MDD and BIP for each P-value threshold.
In a first step, the association of the PRS for BIP, SCZ and MDD with BOR case–control status was analyzed using standard logistic regression and by including the four PCs as covariates. For each P-value threshold, the proportion of variance explained (Nagelkerke’s R2) in BOR case–control status was computed by comparison of a full model (covariates+PRS) score to a reduced model (covariates only).
For further exploratory analysis, the P<0.05 PRS for each disorder was selected (that is, including all markers that reached nominal significance in the training samples). To determine whether the different scores contribute independently to the case–control status, a regression including the PRS for MDD, SCZ and BIP and the four PCs was computed. In a secondary analysis, two further models were computed. These included the PRS for BIP and the PRS of either MDD or SCZ, while controlling for the four PCs.
Furthermore, PRS were analyzed by differentiating between controls, and patients with or without comorbid MDD. For each PRS, a linear model was computed using the PRS as a dependent variable, disease state as an independent variable and the four PCs as covariates. Differences between groups were assessed using post hoc tests (Bonferroni-corrected).
Results
Sample characteristics
Genetic quality control led to the exclusion of 207 subjects. Reasons for exclusion were: (i) insufficient data quality (low call rate), n=6; (ii) relatedness, n=63; and (iii) population outlier status, n=138. After quality control, the sample comprised 998 BOR cases (914 female/84 male) and 1545 controls (868 female/677 male). Mean age for cases was 29.58 years (range: 18–65 years, standard deviation (s.d.=8.64)). Mean age for controls was 44.19 years (range: 18–72 years, s.d.=13.24; details see Supplementary Table 1). Of the 998 cases, 666 had comorbid lifetime MDD, and 262 did not (data missing for 40 cases).
Single marker analysis
A total of 10 736 316 single markers were included in the analysis. As expected for GWAS on a complex psychiatric disorder with the current sample size, the single marker analysis revealed no significant hit after correction for multiple testing (see Figures 1 and 2). The most significant marker was rs113507694 in DPPA3 on chromosome 12 (P=2.01 × 10−07; odds ratio =0.35, minor allele frequency =0.03, INFO =0.59). Single markers with P<1 × 10−5 are listed in Supplementary Table 2.
Manhattan plot showing association results. Manhattan plot of the case–control analysis (998 cases; 1545 controls). For each single-nucleotide polymorphism (SNP), the chromosomal position is shown on the x axis, and the –log10 P-value on the y axis. The red line indicates genome-wide significance (P<5 × 10−8) and the blue line indicates suggestive evidence for association (P<1 × 10−5).
Gene-based analysis
In the gene-based analysis, a total of 17 755 genes were tested. Two genes showed significant association with BOR after correction for multiple testing: the gene coding for Plakophilin-4 on chromosome 2 (PKP4; P=8.24 × 10−7); and the gene coding for dihydropyrimidine dehydrogenase on chromosome 1 (DPYD, P=1.20 × 10−6). The most significant genes (P<5 × 10−4) are listed in Table 1. The top hit of the previous GWAS of borderline personality features, SERINC5, achieved nominal significance in the present study (Puncorrected=0.016).
Gene-set analysis
Gene-set analysis with i-GSEA4GWASv2 revealed one significant gene set: exocytosis (GO: 0006887; PFDR=0.019). Of 25 genes in this gene set, 22 were mapped with variants and 15 showed nominally significant associations. Details on significant and nonsignificant genes in this gene set are provided in Supplementary Table 3. All gene sets with Puncorrected<0.01 are shown in Table 2. A technical replication analysis with GSA-SNP and MAGMA confirmed the gene-set exocytosis (GSA-SNP: Puncorrected=2.32 × 10−4; MAGMA: Puncorrected=0.056).
LD-score regression
Significant genetic correlations with BOR were found for BIP (rg=0.28; s.e.=0.094; P=2.99 × 10−3), MDD (rg=0.57; s.e.=0.18; P=1.04 × 10−3) and SCZ (rg=0.34; s.e.=0.082; P=4.37 × 10−5). A meta-analytic comparison revealed no significant differences between the correlations (all P>0.13).
Polygenic risk score
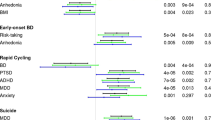
PRS analysis revealed significant associations with BOR for the PRS of BIP, MDD and SCZ. SCZ PRS were significant for all investigated thresholds. BIP and MDD scores were significant for all PRS that included SNPs with P-values higher than 0.0001 and 0.001, respectively (see Supplementary Table 4). The share of variance explained in BOR case–control status (Nagelkerke’s R2) by the respective PRS was up to 0.86% for BIP; up to 3.1% for SCZ; and up to 2.1% for MDD (see Figure 3 and Supplementary Table 4).
Polygenic risk score analysis. The proportion of variance explained in case–control status (y axis; Nagelkerke’s R2) by the PRS for BIP, SCZ and MDD is depicted for the different P-value cutoffs used in the calculation of the PRS. Principal components were included in the models to control for population stratification. 1*, P<0.05; 2*, P<0.001; 3*, P<1 × 10−4; 4*, P<1 × 10−6; 5*, P<1 × 10−8; 6*, P<1 × 10−10; 7*, P<1 × 10−12. BIP, bipolar disorder; MDD, major depressive disorder; NS, nonsignificant; PRS, polygenic risk score; SCZ, schizophrenia.
Simultaneous addition of the PRS for SCZ, BIP and MDD (threshold P<0.05) to the regression model explained 4.4% of the variance (Nagelkerke’s R2) in BOR case–control status. The PRS for SCZ and the PRS for MDD were significant predictors (P=9.78 × 10−9 and P=1.9 × 10−7, respectively). The PRS for BIP was not a significant predictor in this model (P=0.28).
A secondary analysis was then performed including (i) BIP PRS with MDD PRS and (ii) BIP PRS with SCZ PRS. Here, BIP PRS explained variance independently of MDD PRS (P=0.0067), but not of SCZ PRS (P=0.11).
Differentiation between cases with and without comorbid MDD and controls revealed significant effects of BOR diagnosis on PRS for BIP, SCZ and MDD (all P<0.001, see Figure 4). Post hoc analyses revealed no differences in PRS for the BIP, SCZ or MDD PRS of the BOR subgroup with comorbid MDD compared with the BOR subgroup without MDD (all P>0.5).
Polygenic risk score analysis in subgroups. Mean z-standardized PRS and standard error (s.e.) for BIP, SCZ and MDD are shown in the control group, all cases, and in cases with and without comorbid MDD. PRS with a P-value threshold of P=0.05 were selected for this comparison and principal components were included in the models to control for population stratification. The numbers at the top of each bar indicate the significance of the difference in the respective PRS in comparison with the control group. 1*, P<0.05; 2*, P<0.001; 3*, P<1 × 10−4; 4*, P<1 × 10−6; 5*, P<1 × 10−8; 6*, P<1 × 10−10; 7*, P<1 × 10−12. BIP, bipolar disorder; BOR, borderline personality disorder; MDD, major depressive disorder; NS, nonsignificant; PRS, polygenic risk score; SCZ, schizophrenia.
Compared with controls, PRS for SCZ and MDD were significantly increased in the BOR subgroups with and without comorbid MDD (all P<0.001). The PRS for BIP only showed a significant difference to controls in the BOR subgroup with comorbid MDD (P<0.001, see Figure 4).
Discussion
The present study is the first case–control GWAS of BOR. As expected, no genome-wide significant association was found for any single marker. In the gene-based test, however, two genes achieved genome-wide significance: dihydropyrimidine dehydrogenase (DPYD) and Plakophilin-4 (PKP4). DPYD encodes a pyrimidine catabolic enzyme, which is the initial and rate-limiting factor in the pathway of uracil and thymidine catabolism. Genetic deficiency of this enzyme results in an error in pyrimidine metabolism.37 This is associated with thymine–uraciluria and an increased risk of toxicity in cancer patients receiving 5-fluorouracil chemotherapy (http://www.ncbi.nlm.nih.gov/gene/1806). Recent PGC meta-analyses revealed an association between DPYD and SCZ and BIP.34, 38, 39 DPYD contains a binding site for the micro-RNA miR-137, which has previously been associated with schizophrenia,40 and a previous exome-sequencing study reported two putative functional de novo variants in DPYD in cases with SCZ.41 PKP4 is involved in the regulation of cell adhesion and cytoskeletal organization.42 In pathway analyses of PGC GWAS data, cell adhesion was associated with BIP,43 and SCZ,44 whereas cell junction was implicated in MDD, as well as in an integrative pathway analysis of all three disorders.45
SERINC5, which was the top hit of the previous GWAS of Borderline personality features,7 achieved nominal significance in the present study. The protein SERINC5 incorporates serine into newly forming membrane lipids, and is enriched in myelin in the brain.46 Previous research suggests that decreased myelination is associated with a reduced capacity for social interaction.7, 47
The gene-set analyses yielded significant results for exocytosis. In neuronal synapses, exocytosis is triggered by an influx of calcium and critically underlies synaptic signaling. Dysregulated neuronal signaling and exocytosis are core features of neurodevelopmental psychiatric disorders such as the autism spectrum disorders and intellectual disability.48, 49 Moreover, recent findings from large meta-analyses have implicated dysregulated neuronal signaling and exocytosis in the molecular mechanisms of BIP, SCZ and MDD.48, 50, 51 These processes may now represent promising starting points for further research into BOR.
The most interesting finding of this study is that BOR showed a genetic overlap with BIP, SCZ and MDD. Notably, BIP did not show a higher correlation with BOR (rg=0.28) than SCZ (rg=0.34) or MDD (rg=0.57). In view of the present sample size, these values must be viewed with caution. A more accurate estimation of these correlations will require calculations in larger cohorts.
Although comorbid BIP was excluded in the present BOR patients, the possibility that the observed genetic overlap between BOR and BIP was at least partly attributable to misdiagnosis cannot be excluded. However, an alternative explanation appears more likely, that is, that disorders currently categorized as BOR and BIP share a common genetic background, and they also do so with SCZ and MDD. This hypothesis is supported by the present observation of a genetic overlap between BOR and SCZ, two disorders that are rarely misdiagnosed by psychiatrists, despite the presence of common psychotic symptoms.
An explanation could also be that the genetic commonality between BOR and BIP, SCZ, and MDD might be due to a common effect of MDD. Prior to the introduction of DSM-IV, a history of MDD was required for a diagnosis of BIP, and MDD has a high prevalence in patients with SCZ (25-85%).52, 53 Therefore, the MDD genetic risk variants that are common to BOR, BIP, and SCZ may be responsible for the observed overlap. For this reason, we conducted two further analyses. First, we compared PRS of BIP, SCZ and MDD in subsamples of BOR patients with (~60%) and without comorbid MDD. Here, no differences in any of the PRS were found. Second, we performed a joint analysis of PRS of BIP, SCZ and MDD in a logistic regression analysis in BOR patients vs controls. Here, no differences were found in any of the PRS. Second, we performed a joint analysis of the PRS of BIP, SCZ and MDD in a logistic regression analysis in BOR patients vs controls. Here, both the SCZ and the MDD risk score explained variance in BOR case–control status independently. Secondary analysis revealed that the BIP risk score explained variance independently of the MDD risk score but not of the SCZ risk score. These results indicate that comorbidity with MDD does not explain the genetic overlap between BOR and BIP, SCZ and MDD. However, the training sets differ in terms of their power to detect underlying risk variants, and therefore the derived PRS differ in terms of the variance they can explain.
It must be noted, that in the PGC-BIP, -SCZ and -MDD samples, controls are partly overlapping. However, it is unlikely that this drives the genetic correlation of BOR with those disorders as the overlap of controls in these samples is rather small (under 10%).54 Also, the joint logistic regression analysis demonstrated that polygenic risk for SCZ and MDD contributed independently to the BOR risk (see above).
The present study had several limitations. First, despite being one of the largest BOR samples available worldwide, the sample size was small in terms of the estimation of heritability. Replication of the present results is warranted in larger, independent cohorts. This should include the investigation of non-European samples. Second, no information was available on the presence of common clinical features such as psychotic symptoms and affect instability. This precluded detailed analysis of the identified genetic overlap. Future studies in larger cohorts should also investigate more detailed phenotypes, including comorbid axis I and axis II disorders, such as addiction and personality disorders, respectively. Third, the observation that psychiatric patients often establish non-random relationships with persons affected by the same or another psychiatric disorder,55 and therefore have offspring with a higher genetic risk for psychiatric disorders, might contribute to the observed genetic correlation of BOR with BIP, SCZ and MDD. However, the LD-score method does not investigate the impact of assortative mating.32 Therefore, assessment of the degree to which this phenomenon may have influenced the genetic correlation estimates was beyond the scope of the present study.
Despite these limitations, the results indicate that neither comorbidity with MDD nor risk variants that are exclusive to MDD explain the genetic overlap between BOR and BIP, SCZ and MDD. Future investigations of larger data sets for BOR and other psychiatric disorders are warranted to refine the analysis of shared and specific genetic risk.
Future studies are warranted to delineate the communalities and specificities of the respective disorders.
Conclusion
In summary, the present study is the first GWAS of patients diagnosed with BOR. The results suggest promising novel genes and a novel pathway for BOR, and demonstrate that, rather than being a discrete entity, BOR has an etiological overlap with the major psychoses. The genetic overlap with BIP is consistent with the observation that some diagnostic criteria for BOR overlap with those for BIP. The overlap between BOR and SCZ and MDD is consistent with previous observations of genetic overlap of other psychiatric disorders.56 Given that BOR patients display specific clinical symptoms not observed in patients with other psychiatric disorders, knowledge of shared and non-shared genetic and clinical features will be important for the development of personalized treatment approaches.
References
Tomko RL, Trull TJ, Wood PK, Sher KJ . Characteristics of borderline personality disorder in a community sample: comorbidity, treatment utilization, and general functioning. J Pers Disord 2014; 28: 734–750.
Bohus M, Schmahl C . [Psychopathology and treatment of borderline personality disorder]. Nervenarzt 2007; 78: 1069–1080.
Lieb K, Zanarini MC, Schmahl C, Linehan MM, Bohus M . Borderline personality disorder. Lancet 2004; 364: 453–461.
Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice G, Weinberg I, Gunderson JG . The 10-year course of physically self-destructive acts reported by borderline patients and axis II comparison subjects. Acta Psychiatr Scand 2008; 117: 177–184.
Tsanas A, Saunders KE, Bilderbeck AC, Palmius N, Osipov M, Clifford GD et al. Daily longitudinal self-monitoring of mood variability in bipolar disorder and borderline personality disorder. J Affect Disord 2016; 205: 225–233.
Calati R, Gressier F, Balestri M, Serretti A . Genetic modulation of borderline personality disorder: systematic review and meta-analysis. J Psychiatr Res 2013; 47: 1275–1287.
Lubke GH, Laurin C, Amin N, Hottenga JJ, Willemsen G, van Grootheest G et al. Genome-wide analyses of borderline personality features. Mol Psychiatry 2014; 19: 923–929.
Gunderson JG, Zanarini MC, Choi-Kain LW, Mitchell KS, Jang KL, Hudson JI . Family study of borderline personality disorder and its sectors of psychopathology. Arch Gen Psychiatry 2011; 68: 753–762.
Torgersen S, Lygren S, Oien PA, Skre I, Onstad S, Edvardsen J et al. A twin study of personality disorders. Compr Psychiatry 2000; 41: 416–425.
Distel MA, Willemsen G, Ligthart L, Derom CA, Martin NG, Neale MC et al. Genetic covariance structure of the four main features of borderline personality disorder. J Pers Disord 2010; 24: 427–444.
Kendler KS, Myers J, Reichborn-Kjennerud T . Borderline personality disorder traits and their relationship with dimensions of normative personality: a web-based cohort and twin study. Acta Psychiatr Scand 2011; 123: 349–359.
Reichborn-Kjennerud T, Ystrom E, Neale MC, Aggen SH, Mazzeo SE, Knudsen GP et al. Structure of genetic and environmental risk factors for symptoms of DSM-IV borderline personality disorder. JAMA Psychiatry 2013; 70: 1206–1214.
Fornaro M, Orsolini L, Marini S, De Berardis D, Perna G, Valchera A et al. The prevalence and predictors of bipolar and borderline personality disorders comorbidity: systematic review and meta-analysis. J Affect Disord 2016; 195: 105–118.
Ghaemi SN, Dalley S, Catania C, Barroilhet S . Bipolar or borderline: a clinical overview. Acta Psychiatr Scand 2014; 130: 99–108.
Ghaemi SN, Barroilhet S . Confusing borderline personality with severe bipolar illness. Acta Psychiatr Scand 2015; 132: 281–282.
Loranger AW, Oldham JM, Tulis EH . Familial transmission of DSM-III borderline personality disorder. Arch Gen Psychiatry 1982; 39: 795–799.
Pope HG Jr ., Jonas JM, Hudson JI, Cohen BM, Gunderson JG . The validity of DSM-III borderline personality disorder. A phenomenologic, family history, treatment response, and long-term follow-up study. Arch Gen Psychiatry 1983; 40: 23–30.
Distel MA, Trull TJ, Willemsen G, Vink JM, Derom CA, Lynskey M et al. The five-factor model of personality and borderline personality disorder: a genetic analysis of comorbidity. Biol Psychiatry 2009; 66: 1131–1138.
Gale CR, Hagenaars SP, Davies G, Hill WD, Liewald DC, Cullen B et al. Pleiotropy between neuroticism and physical and mental health: findings from 108 038 men and women in UK Biobank. Transl Psychiatry 2016; 6: e791.
Malouff JM, Thorsteinsson EB, Rooke SE, Schutte NS . Alcohol involvement and the Five-Factor model of personality: a meta-analysis. J Drug Educ 2007; 37: 277–294.
Witt S, Dukal H, Hohmeyer C, Radosavljevic-Bjelic S, Schendel D, Frank J et al. Biobank of Psychiatric Diseases Mannheim - BioPsy. Open J Bioresour 2016; 3: e2.
Loranger A, Sartorius N, Andreoli A, Berger P, Buchheim P, Chanabasavanna S . German Version of the International Personality Disorder Examination: IPDE. WHO: Geneva, Switzerland, 1998.
First MB, Spitzer RL, Robert L, Gibbon M, Williams JB . Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. Biometrics Research, New York State Psychiatric Institute: New York, NY, USA, 2002.
Consortium SWGotPG. Biological insights from 108 schizophrenia-associated genetic loci. Nature 2014; 511: 421–427.
Howie B, Marchini J, Stephens M . Genotype imputation with thousands of genomes. G3 Genes Genomes Genetics 2011; 1: 457–470.
Delaneau O, Marchini J, Zagury J-F . A linear complexity phasing method for thousands of genomes. Nat Methods 2012; 9: 179–181.
Abecasis GR, Altshuler D, Auton A, Brooks LD, Durbin RM, Gibbs RA et al. A map of human genome variation from population-scale sequencing. Nature 2010; 467: 1061–1073.
Purcell S, Neale B, Todd-Brown K, Thomas L, Ferreira MA, Bender D et al. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet 2007; 81: 559–575.
de Leeuw CA, Mooij JM, Heskes T, Posthuma D . MAGMA: generalized gene-set analysis of GWAS data. PLoS Comput Biol 2015; 11: e1004219.
Zhang K, Cui S, Chang S, Zhang L, Wang J . i-GSEA4GWAS: a web server for identification of pathways/gene sets associated with traits by applying an improved gene set enrichment analysis to genome-wide association study. Nucleic Acids Res 2010; 38 (Web Server issue): W90–W95.
Nam D, Kim J, Kim SY, Kim S . GSA-SNP: a general approach for gene set analysis of polymorphisms. Nucleic Acids Res 2010; 38 (Web Server issue): W749–W754.
Bulik-Sullivan BK, Loh P-R, Finucane HK, Ripke S, Yang J et al, Schizophrenia Working Group of the Psychiatric Genomics C. LD score regression distinguishes confounding from polygenicity in genome-wide association studies. Nat Genet 2015; 47: 291–295.
Bulik-Sullivan B, Finucane HK, Anttila V, Gusev A, Day FR, Loh PR et al. An atlas of genetic correlations across human diseases and traits. Nat Genet 2015; 47: 1236–1241.
Schizophrenia Working Group of the Psychiatric Genomics C. Biological insights from 108 schizophrenia-associated genetic loci. Nature 2014; 511: 421–427.
Abstracts of the XXIIIrd World Congress of Psychiatric Genetics (WCPG): final symposia and penary abstracts. Eur Neuropsychopharmacol 2015; 13 & 23.
International Schizophrenia C, Purcell SM, Wray NR, Stone JL, Visscher PM, O'Donovan MC et al. Common polygenic variation contributes to risk of schizophrenia and bipolar disorder. Nature 2009; 460: 748–752.
Edwards L, Gupta R, Filipp FV . Hypermutation of DPYD deregulates pyrimidine metabolism and promotes malignant progression. Mol Cancer Res 2016; 14: 196–206.
Duan J, Shi J, Fiorentino A, Leites C, Chen X, Moy W et al. A rare functional noncoding variant at the GWAS-implicated MIR137/MIR2682 locus might confer risk to schizophrenia and bipolar disorder. Am J Hum Genet 2014; 95: 744–753.
Ripke S, O'Dushlaine C, Chambert K, Moran JL, Kahler AK, Akterin S et al. Genome-wide association analysis identifies 13 new risk loci for schizophrenia. Nat Genet 2013; 45: 1150–1159.
Schizophrenia Psychiatric Genome-Wide Association Study (GWAS) Consortium. Genome-wide association study identifies five new schizophrenia loci. Nat Genet 2011; 43: 969–976.
Xu B, Ionita-Laza I, Roos JL, Boone B, Woodrick S, Sun Y et al. De novo gene mutations highlight patterns of genetic and neural complexity in schizophrenia. Nat Genet 2012; 44: 1365–1369.
Keil R, Schulz J, Hatzfeld M . p0071/PKP4, a multifunctional protein coordinating cell adhesion with cytoskeletal organization. Biol Chem 2013; 394: 1005–1017.
Kao CF, Chen HW, Chen HC, Yang JH, Huang MC, Chiu YH et al. Identification of susceptible loci and enriched pathways for bipolar II disorder using genome-wide association studies. Int J Neuropsychopharmacol 2016; 19: pyw064.
Zhang Z, Yu H, Jiang S, Liao J, Lu T, Wang L et al. Evidence for association of cell adhesion molecules pathway and NLGN1 polymorphisms with schizophrenia in Chinese Han population. PLoS ONE 2015; 10: e0144719.
Network, Pathway Analysis Subgroup of Psychiatric Genomics C. Psychiatric genome-wide association study analyses implicate neuronal, immune and histone pathways. Nat Neurosci 2015; 18: 199–209.
Krueger WH, Gonye GE, Madison DL, Murray KE, Kumar M, Spoerel N et al. TPO1, a member of a novel protein family, is developmentally regulated in cultured oligodendrocytes. J Neurochem 1997; 69: 1343–1355.
Liu J, Dietz K, DeLoyht JM, Pedre X, Kelkar D, Kaur J et al. Impaired adult myelination in the prefrontal cortex of socially isolated mice. Nat Neurosci 2012; 15: 1621–1623.
Cupertino RB, Kappel DB, Bandeira CE, Schuch JB, da Silva BS, Muller D et al. SNARE complex in developmental psychiatry: neurotransmitter exocytosis and beyond. J Neural Transm (Vienna) 2016; 123: 867–883.
Pescosolido MF, Gamsiz ED, Nagpal S, Morrow EM . Distribution of disease-associated copy number variants across distinct disorders of cognitive development. J Am Acad Child Adolesc Psychiatry 2013; 52: 414–430.e14.
Zhao Z, Xu J, Chen J, Kim S, Reimers M, Bacanu SA et al. Transcriptome sequencing and genome-wide association analyses reveal lysosomal function and actin cytoskeleton remodeling in schizophrenia and bipolar disorder. Mol Psychiatry 2015; 20: 563–572.
Sullivan PF, de Geus EJ, Willemsen G, James MR, Smit JH, Zandbelt T et al. Genome-wide association for major depressive disorder: a possible role for the presynaptic protein piccolo. Mol Psychiatry 2009; 14: 359–375.
Bosanac P, Castle DJ . Schizophrenia and depression. Med J Australia 2013; 199 (6 Suppl): S36–S39.
Buckley PF, Miller BJ, Lehrer DS, Castle DJ . Psychiatric comorbidities and schizophrenia. Schizophr Bull 2009; 35: 383–402.
Anttila V, Bulik-Sullivan B, Finucane HK, Bras J, Duncan L, Escott-Price V et al. Analysis of shared heritability in common disorders of the brain. bioRciv 2016.
Nordsletten AE, Larsson H, Crowley JJ, Almqvist C, Lichtenstein P, Mataix-Cols D . Patterns of nonrandom mating within and across 11 major psychiatric disorders. JAMA Psychiatry 2016; 73: 354–361.
Cross-Disorder Group of the Psychiatric Genomics C, Lee SH, Ripke S, Neale BM, Faraone SV, Purcell SM et al. Genetic relationship between five psychiatric disorders estimated from genome-wide SNPs. Nat Genet 2013; 45: 984–994.
Acknowledgements
We thank all patients and control subjects for their participation. We thank the KFO 256 workgroup of the CIMH, and Bipolar Disorder Working Group-, the Major Depression Working Group- and the Schizophrenia Working Group of the Psychiatric Genomics Consortium (PGC-BIP, PGC-MDD, PGC-SCZ) for providing access to the relevant data. The Romanian sample was funded by UEFISCDI, Romania, grant no. 89/2012 to MGS. The CoLaus|PsyCoLaus study was and is supported by research grants from GlaxoSmithKline, the Faculty of Biology and Medicine of Lausanne and the Swiss National Science Foundation (grants 3200B0–105993, 3200B0-118308, 33CSCO-122661, 33CS30-139468 and 33CS30-148401). The study was supported by the German Federal Ministry of Education and Research (BMBF) through the Integrated Network IntegraMent (Integrated Understanding of Causes and Mechanisms in Mental Disorders), under the auspices of the e:Med Programme (grant 01ZX1314A to MMN and SC; grant 01ZX1314G to MR). The study was supported by the German Research Foundation (DFG; grant FOR2107; RI908/11-1 to MR; WI3429/3-1 to SHW; NO246/10-1 to MMN; DA1151/5-1 to UD; KFO 256 BO 1487/12-1 to MB;.SFB 779 TP A08 to BHS).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
JIN Jr is an investigator for Assurex and a consultant for Janssen. AT has received consultancy fees from Janssen and Novartis. The remaining authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Translational Psychiatry website
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Witt, S., Streit, F., Jungkunz, M. et al. Genome-wide association study of borderline personality disorder reveals genetic overlap with bipolar disorder, major depression and schizophrenia. Transl Psychiatry 7, e1155 (2017). https://doi.org/10.1038/tp.2017.115
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tp.2017.115
This article is cited by
-
The role of thyroid function in borderline personality disorder and schizophrenia: a Mendelian Randomisation study
Borderline Personality Disorder and Emotion Dysregulation (2024)
-
Persistent thinness and anorexia nervosa differ on a genomic level
European Journal of Human Genetics (2024)
-
Overlapping genetic influences between creativity and borderline personality symptoms in a large Dutch sample
Scientific Reports (2024)
-
Psychological trauma as a transdiagnostic risk factor for mental disorder: an umbrella meta-analysis
European Archives of Psychiatry and Clinical Neuroscience (2023)
-
Integrative analyses highlight functional regulatory variants associated with neuropsychiatric diseases
Nature Genetics (2023)