Abstract
The aim is to analyse the clinical presentation, treatment and outcomes in patients with Paget’s disease with invasive ductal carcinoma (PD-IDC), with special emphasis on the role of surgical treatment. Using data obtained by the Surveillance, Epidemiology, and End Results (SEER) program from 2010–2013, we investigated the differences in characteristics, overall survival (OS), and breast cancer-specific mortality (BCSM) between patients with PD-IDC and those with invasive ductal carcinoma (IDC). Compared with IDC group, patients with PD-IDC had a better prognosis and lower mortality in adjusted analyses. In the multivariate analysis of cases with PD-IDC, history of ALND was significantly associated with OS while Her2 status were associated with BCSM. Further, subgroup analysis demonstrated no difference between surgical treatment subgroups for either OS or BCSM. The results demonstrated that PD-IDC appears to alter the association between prognosis and Her2 status. Meanwhile, breast-conserving surgery with radiotherapy may be a feasible treatment alternative and sentinel lymph node biopsy should be considered as an appropriate treatment for patients with PD-IDC.
Similar content being viewed by others
Introduction
Paget’s disease (PD) of the breast is rare, accounting for 1–3% of all breast malignancies. Paget’s disease is characterized by the eczematous eruption and ulceration of the nipple or areola1,2,3. Due to its rare occurrence, diagnosis of PD may be a delayed or misdiagnosed as benign dermatosis. Breast imaging examination should be used to identify the presence of concomitant breast cancer, and nipple skin biopsy may provide further definitive diagnosis.
In the majority of patients, PD has been found in association with invasive breast cancer or ductal carcinoma in situ, with concomitant disease identified in up to 82% to 93%4,5. Additionally, several studies have found Paget’s disease with invasive ductal carcinoma (PD-IDC) to be associated with tumours that are larger in size and higher in grade as well as negative oestrogen receptor (ER) and progesterone receptor (PR) but positive human epidermal growth factor receptor 2 (Her2) status. Further, diagnosis of PD-IDC may be associated with reduced survival6,7,8,9.
Traditional treatment for PD-IDC has been mastectomy due to the common occurrence of sonographically and mammographically hidden multifocal and multicentric malignancies located in breast tissue far from the nipple. However, with the development of imaging technology, breast conservation surgery (BCS) has been found to be a feasible surgical option with low risk for local recurrence in selected patients5,10,11. In addition to BCS, sentinel lymph node biopsy (SLNB) may be effective in patients with PD; however, its role in PD treatment remains unclear. Based on current standards, SLNB has been recommended as a less invasive method than axillary lymph node dissection (ALND) for the staging of patients with early IDC. We speculate SLNB may be effective in detecting ALNs in patients with PD-IDC as well.
For these reasons, the aim of this study was to analyse the clinical presentation, treatment and outcome in patients with PD-IDC, with special emphasis on the role of BCS and SLNB in PD-IDC treatment.
Results
Clinical and Tumour Characteristics
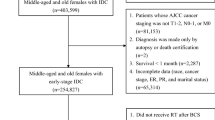
A total of 180253 breast cancer patients were eligible during the 2010–2013 study period. We excluded from the analysis 617 patients whose survival times were classified as unknown. A total of 179776 IDC and 477 PD-IDC patients had information available and were included in this study.
Differences in patient demographics, cancer characteristics, treatments, and outcomes between histological subgroups are summarized in Table 1. Compared with IDC, patients with PD-IDC were more likely to have more lymph node involvement and tumours of a higher grade, more advanced stage, and larger size (each P < 0.05). PD-IDC tumours were more likely to be HR-negative and Her2-positive when compared with IDC tumours. Among the treatment options, patients with PD-IDC were more likely to undergo a mastectomy and axillary lymph node dissection but less likely to undergo radiotherapy when compared with IDC patients (P < 0.05).
Survival Analysis
Weighted Kaplan-Meier analysis was used to determine OS and BCSM within histological subgroups. At a follow-up time, patients with PD-IDC had an OS of 89.5%, while patient sin the IDC group had an OS of 92.8% (P < 0.05). Further, the BCSM rate was 7.4% within the PD-IDC group compared with 4.5% within the IDC group (P < 0.05) (Table 1). However, patients with PD-IDC had a better prognosis and lower mortality compared with the IDC group in adjusted analyses (Fig. 1). Due to tumour heterogeneity and sample capacity disparity, these may prevent the robustness of the conclusions12. Then, we generated 3 independent cohorts by randomly selecting considerable samples from the entirety. Each cohort was required to maintain the same ratio of various factors as that of the original set, without sample overlap among the cohorts. We further analysed the clinicopathologic features and performed survival curves compared each cohort to PD-IDC group (Supplementary 1 and 2). And the results further revealed that patients with PD-IDC had a better prognosis compared with those with IDC.
We performed multivariate analysis to evaluate prognostic factors of OS and BCSM in cases with PD-IDC (Table 2). In the multivariate model, tumour stage and history of LN surgery were significantly associated with OS, while age at diagnosis, tumour stage and Her2 status were associated with BCSM (P < 0.05). Among patients, Her2 positive cancer was significantly associated with a higher rate of BCSM, as showed in Fig. 2 (OS, P = 0.217, aHR = 2.096; BCSM, P = 0.024, aHR = 5.169).
Effect of Surgical Treatment on Survival Outcomes
For patients with PD-IDC, the results of multivariate analysis suggested that SLNB was significantly associated with OS during the follow-up period (P = 0.028). Further, we analysed survival outcomes by surgical treatment subgroups. We defined two subgroups based on different surgical treatments: one included patients who underwent BCS with radiotherapy and mastectomy (M), and the other was separated into M + ALND, M + SLNB, BCS + ALND and BCS + SLNB. The results demonstrated no difference between these subgroups for OS or BCSM (Fig. 3).
Discussion
In this large population-based cohort of cases diagnosed with PD-IDC, we identified improved survival when adjusting for other factors relative to patients with IDC alone. In addition, our analysis of Her2 status demonstrated the PD-IDC patients with Her2 positive cancer were at significantly greater risk of BCSM, as were patients with advanced tumour stage. In our series, there was no difference between surgical treatment subgroups.
In the current study, patients with PD-IDC tended to have a more extensive lymph node involvement and distant metastases and tumours that were higher in grade, more advanced in stage, larger in size, and more frequently HR-positive and that had higher levels of Her2 expression compared to those with IDC. Kothari et al.13 reported that patients with PD-IDC had a significantly lower survival (10-year OS 49%) than patients with IDC only (64%). They attributed the poorer survival outcomes in patients with PD-IDC to higher levels of Her2-positive expression. Further, they compared the survival of patients with PD to the survival of those with IDC after adjusting for Her2 status and other factors. When controlling for Her2 status, the two groups had a similar OS. However, we analysed common prognostic factors as well as Her2 status. The results showed that patients with PD-IDC had significantly better survival outcomes than those with IDC alone, and patients with Her2-positive cancer had a higher BCSM but similar OS to patients with Her2-negative cancer after adjusting for other prognostic factors. This result differed from Kothari’s study, and this discrepancy may be due to the inclusion of different variables within the two studies. For instance, we included HR status and history of SLNB as variables within our analyses.
Surgical treatment of PD-IDC has been controversial. Historically, patients with PD were predominately treated with mastectomy for two main reasons: the high incidence of potential multifocality and contraindication for BCS patients with centrally located breast cancer. Several studies have revealed that local excision alone was not an appropriate surgical approach for patients with PD of the nipple3,10. However, the consensus has been that BCS may be effective in selected patients. The previously reported techniques for BCS in patients with PD have varied widely and include nipple excision and central segmentectomy as well as resection plus radiation. There is a place for BCS in selected patients with PD of the breast, especially those with no mass. Long-term follow-up of patients with PD following BCS with radiotherapy has only once been previously reported14. This study found that breast cancer-specific survival (BCSS) rate was 91%, 83%, and 76% at 5, 10, and 15 years, respectively. In an analysis using SEER data, Chen et al. found a 15-year BCSS up to 61% (95% CI, 53–68%) in patients with PD-IDC diagnosed between 1988 and 2002. Further, there was no statistically difference in survival between central lumpectomy and mastectomy after adjusting for tumour characteristics6. Similarly, these studies supported the use of BCS with radiotherapy as a feasible alternative for patients with PD-IDC. Although SLNB may still be considered a controversial treatment in patients with PD, SLNB has become a common approach in patients with breast cancer and appears to be a feasible treatment option15,16. When IDC has been identified and a mastectomy has been completed, SLNB should still be routinely employed in axillary node negative DCIS patients17,18. In the present study, patients undergoing SLNB had similar survival to those receiving ALND regardless of surgical mode of their breast cancer treatment. Current National Comprehensive Cancer Network (NCCN) guidelines encouraged axillary staging in patients with PD-IDC, while axillary assessment was not found to be necessary for PD-DCIS undergoing BCS19,20. Further study regarding the potential benefits of SLNB in patients with PD-IDC is warranted.
A previous examination of the molecular profiles of PD suggest that the luminal B subtype was most frequently identified21; however, other studies have reported the HER2-positive (nonluminal) subtype to be more common in primary PD22. Some studies have found that tumours in patients with PD were positive for c-erbB-2, cyclin D1, Ki-67 and p16, which have been associated with more aggressive tumour behaviour, and simultaneously had low level expression of Bcl-2 or ER and PR, which has been associated with a better prognosis21,23. Additional molecular studies are required, and differences in survival outcomes must continue to be monitored.
The main limitations of this study were a small sample size, heterogeneous population and retrospective methodology. The information regarding systemic therapy was insufficient, and follow-up was limited. This may have impacted our results, as Her2-targeted therapy and novel adjuvant radiation may significantly improve survival when fully utilized in the management of PD. Additionally, this study did not include specific information regarding the type of axillary operation and thus used number of lymph nodes excised as a proxy.
Despite these limitations, our study demonstrated that PD-IDC appears to alter the association between prognosis and HER2 status. Meanwhile, BCS with radiotherapy may be a feasible treatment alternative, as it resulted in survival rates similar to those achieved with mastectomy, and SLNB should be considered as an appropriate treatment for patients with PD-IDC. However, surgical treatment plans should be selected based on the results of clinical and imaging assessments. Further studies are needed to minimize variation in treatment of PD-IDC and to establish a standardized management approach for PD-IDC.
Materials and Methods
Data source and study design
We obtained data from the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) programme database collected between 2010 and 2013. Her2 status was initially collected by SEER in 2010; therefore, we used 2010 as the starting point for our study. We used the International Classification of Diseases for Oncology, 3rd edition (ICD-O-3) histopathology codes to extract data for all cases with Paget’s disease with invasive ductal carcinoma (PD-IDC) (code 8541). Data from patients with ductal carcinoma of no special type (ICD-O-3 code 8500) was obtained to serve as a control group. We selected cases with known hormone receptor (HR) and Her2 status. Patients who did not receive surgery, had ICD of unknown type or were diagnosed at autopsy were excluded.
Type of surgery were categorized as BCS (primary site surgery codes 20–24) of mastectomy (primary site surgery codes 30–80). Because the type of axillary surgery was not reported within SEER, removal of 1–5 lymph nodes was regarded as sentinel lymph node biopsy (SLNB) and removal of >5 lymph nodes removed was regarded as axillary lymph node dissection (ALND), as in previous studies24.
Demographic variables included age at diagnosis (<35, 35–49, 50–64, >65 years) and race (white, black, other). Cancer characteristics included stage (I, II, III, IV, unknown), grade (well, moderately, poorly, undifferentiated, unknown), T stage (T0/T1, T2, T3, T4, NA), N stage (N0, N1, N2, N3, NX, NA), distant metastasis (M0, M1, NA), laterality (right, left, paired, bilateral, unknown), and HR and Her2 status (positive, negative, borderline, unknown). Receipt of radiation therapy (no, yes, unknown) was collected to characterize treatment. Tumour subtypes were characterized by a breast subtype variable and defined as HR+/Her2−, HR+/Her2+, HR−/Her2+ and triple-negative (TN).
The two main outcomes in our study were overall survival (OS) and breast cancer-specific mortality (BCSM). Vital status was recorded as “alive” or “dead” in the SEER dataset. Survival time (in months) was calculated for each patient using the “Completed Months of Follow-up” variable in the SEER database. Overall survival (OS) was determined by the proportion of patients alive at the end of the study period or their last follow-up. Breast cancer-specific mortality (BCSM) was determined by the proportion of patients whose cause of death was due to breast cancer relative to that of patients who were alive at the end of the study period or their last follow-up or died due to other causes. Cases without survival times were classified as unknown and removed from the study.
Statistical analysis
Patient demographics and cancer- and treatment-related characteristics were compared between histological subgroups using chi-square or Fisher’s exact tests. Survival outcomes (OS and BCSM) were estimated using the weighted Kaplan–Meier method, and variables were compared between histological and HER2 status subgroups using log-rank tests. Univariate and multivariate Cox proportional hazard regression models were used to obtain HRs and their respective 95% confidence intervals and estimate relative risk, and these approaches were applied to evaluate the relationship between potential covariates and either OS or BCSM. All statistical analyses were performed and probability of survival curves were generated using SPSS 19.0 (IBM Corporation, Armonk, NY). A two-sided P value < 0.05 was considered statistically significant.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional Information
How to cite this article: Wu, Q. et al. Surgical treatment in Paget’s disease with invasive ductal carcinoma: an observational study based on SEER. Sci. Rep. 7, 45510; doi: 10.1038/srep45510 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Ashikari, R., Park, K., Huvos, A. G. & Urban, J. A. Paget’s disease of the breast. Cancer 26, 680–685 (1970).
Nance, F. C., DeLoach, D. H., Welsh, R. A. & Becker, W. F. Paget’s disease of the breast. Annals of surgery 171, 864–874 (1970).
Dixon, A. R., Galea, M. H., Ellis, I. O., Elston, C. W. & Blamey, R. W. Paget’s disease of the nipple. The British journal of surgery 78, 722–723 (1991).
Kollmorgen, D. R., Varanasi, J. S., Edge, S. B. & Carson, W. E. 3rd . Paget’s disease of the breast: a 33-year experience. Journal of the American College of Surgeons 187, 171–177 (1998).
Kawase, K. et al. Paget’s disease of the breast: there is a role for breast-conserving therapy. Annals of surgical oncology 12, 391–397, doi: 10.1245/ASO.2005.05.026 (2005).
Chen, C. Y., Sun, L. M. & Anderson, B. O. Paget disease of the breast: changing patterns of incidence, clinical presentation, and treatment in the U.S. Cancer 107, 1448–1458, doi: 10.1002/cncr.22137 (2006).
Sakorafas, G. H., Blanchard, K., Sarr, M. G. & Farley, D. R. Paget’s disease of the breast. Cancer treatment reviews 27, 9–18, doi: 10.1053/ctrv.2000.0203 (2001).
Durkan, B., Bresee, C., Bose, S., Phillips, E. H. & Dang, C. M. Paget’s disease of the nipple with parenchymal ductal carcinoma in situ is associated with worse prognosis than Paget’s disease alone. The American surgeon 79, 1009–1012 (2013).
Ortiz-Pagan, S. et al. Effect of Paget’s disease on survival in breast cancer: an exploratory study. Arch Surg 146, 1267–1270, doi: 10.1001/archsurg.2011.278 (2011).
Bijker, N. et al. Breast-conserving therapy for Paget disease of the nipple: a prospective European Organization for Research and Treatment of Cancer study of 61 patients. Cancer 91, 472–477 (2001).
Li, Y. J., Huang, X. E. & Zhou, X. D. Local Breast Cancer Recurrence after Mastectomy and Breast-Conserving Surgery for Paget’s Disease: A Meta-Analysis. Breast care 9, 431–434, doi: 10.1159/000368431 (2014).
Li, J. et al. Identification of high-quality cancer prognostic markers and metastasis network modules. Nature communications 1, 34, doi: 10.1038/ncomms1033 (2010).
Kothari, A. S. et al. Paget disease of the nipple: a multifocal manifestation of higher-risk disease. Cancer 95, 1–7, doi: 10.1002/cncr.10638 (2002).
Marshall, J. K. et al. Conservative management of Paget disease of the breast with radiotherapy: 10- and 15-year results. Cancer 97, 2142–2149, doi: 10.1002/cncr.11337 (2003).
Sukumvanich, P. et al. The role of sentinel lymph node biopsy in Paget’s disease of the breast. Annals of surgical oncology 14, 1020–1023, doi: 10.1245/s10434-006-9056-2 (2007).
Laronga, C. et al. Paget’s disease in the era of sentinel lymph node biopsy. American journal of surgery 192, 481–483, doi: 10.1016/j.amjsurg.2006.06.023 (2006).
American College Of, R. Practice guideline for the management of ductal carcinoma in-situ of the breast (DCIS). Journal of the American College of Surgeons 205, 145–161, doi: 10.1016/j.jamcollsurg.2007.02.056 (2007).
Pezzi, C. M. et al. Breast conservation surgery using nipple-areolar resection for central breast cancers. Arch Surg 139, 32–37, discussion 38, doi: 10.1001/archsurg.139.1.32 (2004).
Gradishar, W. J. et al. Breast Cancer, Version 1.2016. Journal of the National Comprehensive Cancer Network: JNCCN 13, 1475–1485 (2015).
Gradishar, W. J. et al. Breast Cancer Version 2.2015. Journal of the National Comprehensive Cancer Network: JNCCN 13, 448–475 (2015).
Fu, W., Lobocki, C. A., Silberberg, B. K., Chelladurai, M. & Young, S. C. Molecular markers in Paget disease of the breast. Journal of surgical oncology 77, 171–178 (2001).
Goldhirsch, A. et al. Strategies for subtypes–dealing with the diversity of breast cancer: highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Annals of oncology: official journal of the European Society for Medical Oncology/ESMO 22, 1736–1747, doi: 10.1093/annonc/mdr304 (2011).
Buxant, F. & Noel, J. C. Pl6 expression in Paget’s disease of the breast. European journal of gynaecological oncology 29, 441–443 (2008).
Wang, J. et al. Outcomes of sentinel lymph node dissection alone vs. axillary lymph node dissection in early stage invasive lobular carcinoma: a retrospective study of the surveillance, epidemiology and end results (SEER) database. PloS one 9, e89778, doi: 10.1371/journal.pone.0089778 (2014).
Acknowledgements
We thank American Journal Experts (AJE) for assistance in improving the quality of language. We also thank Yimin Zhang for assistance in revising the statistical method. This work was partially supported by a National Natural Science Foundation of China (NSFC) grant and a National Major Scientific Instruments and Equipment Development Projects (Grant NO: 2012YQ160203) to Dr. Shengrong Sun (Grant NO: 81471781). This work was also supported by a NSFC grant to Dr. Juanjuan Li (Grant NO: 81302314).
Author information
Authors and Affiliations
Contributions
Original idea by Ding Xiaojun and Wu Qi. Wu Qi and Zhu Shan designed and gathered the data. Li Juanjuan, Wu Juan, Sun Si and Liu Qian performed statistical analysis, figures, which was reviewed and approved by Yao Feng and Sun Shengrong. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Wu, Q., Ding, X., Li, J. et al. Surgical treatment in Paget’s disease with invasive ductal carcinoma: an observational study based on SEER. Sci Rep 7, 45510 (2017). https://doi.org/10.1038/srep45510
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep45510
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.