Abstract
Sleep is modulated by several factors, including sex, age, and chronotype. It has been hypothesised that contemporary urban populations are under pressure towards shorter sleep duration and poorer sleep quality. Baependi is a small town in Brazil that provides a window of opportunity to study the influence of sleep patterns in a highly admixed rural population with a conservative lifestyle. We evaluated sleep characteristics, excessive daytime sleepiness, and chronotype using the Pittsburgh Sleep Quality Index, Epworth Sleepiness Scale and Morningness-Eveningness Questionnaire questionnaires, respectively. The sample consisted of 1,334 subjects from the Baependi Heart study (41.5% male; age: 46.5 ± 16.2 y, range: 18–89 years). Average self-reported sleep duration was 07:07 ± 01:31 (bedtime 22:32 ± 01:27, wake up time: 06:17 ± 01:25 hh:min), sleep quality score was 4.9 + 3.2, chronotype was 63.6 ± 10.8 and daytime sleepiness was 7.4 ± 4.8. Despite a shift towards morningness in the population, chronotype remained associated with reported actual sleep timing. Age and sex modulated the ontogeny of sleep and chronotype, increasing age was associated with earlier sleep time and shorter sleep duration. Women slept longer and later, and reported poorer sleep quality than men (p < 0.0001). This study provides indirect evidence in support of the hypothesis that sleep timing was earlier prior to full urbanisation.
Similar content being viewed by others
Introduction
Sleep has several physiological functions relevant to health. Several reports have suggested that poor sleep quality, short sleep duration, or inappropriate sleep timing are related to cardiovascular diseases (CVD)1, metabolic dysfunction2, immune dysregulation3 and cognitive impairment4. Sleep is known to be intimately regulated by circadian processes5. Consequently, the exposure to natural light-dark cycle is fundamental to the entrainment of circadian system and sleep-wake cycle6. However, sleep patterns and habits are also intimately associated with cultural and socio-economic factors, necessitating field studies evaluating a variety of populations7.
It has been proposed that electricity and urbanisation have changed human sleep behaviour and sleep patterns, such as timing and duration8. In modern metropoles, sleep complaints have increased progressively in the past decade, with a considerable delay in bedtime and wake up times9. For instance, two recent studies from representative samples of adults from urban populations of Chicago and São Paulo described average sleep duration shorter than 7 h10. A nationwide report from the National Sleep Awareness Roundtable in the United States also indicate that 35.3% of respondents were sleeping less than 7 h11. Evaluating sleep in populations from regions still undergoing urbanisation is crucial for developing a better understanding and knowledge of human sleep and its natural history. Studies have been performed with religiously conservative populations12, and also populations with limited access to electricity. Rubber tappers in the Amazon region of Brazil, for example, studied in two different conditions with and without access to electricity, presented sleep onset and wake up times very tightly associated with environmental light, furthermore, they presented advanced sleep timing when they had no access to electricity13. In another study, access to electric light was associated with a reduction of sleep duration in a hunter-gatherer community in Argentina14. In short, several studies suggested that access to electricity has delayed sleep timing14,15,16, and also shortened sleep duration14. Recently, however, an objective evaluation of sleep duration in three hunter-gatherer societies found average sleep durations between 5.1 and 7.1 hours17. Furthermore, these communities also showed significant seasonal patterns, and sleep timing was more likely to be associated with environmental temperature rather than with light (sunset or sunlight). Thus, there is no current strong consensus on the outcomes of urbanization on sleep patterns, and consequentially, more data from a greater diversity of communities are needed.
The Baependi heart study is a family-based cohort study designed to investigate cardiovascular disease and associated factors, specifically factors typical of Brazil18. This town is located at 21.5°S 44.5°W, with a photoperiod range between 10 h 40 min and 13 h 20 min, and an average insolation ranging between 4.09 and 5.59 kWh/m2/day (http://www.esrl.noaa.gov/gmd/grad/solcalc/). The traditional lifestyle, moderate and ongoing urbanisation, and very limited inward migration of this rural town make it a location of interest for the study of sleep quality and sleep characteristics. Since the beginning of this study in December 2005, a significant number of discoveries have been reported, such as the heritability of cardiovascular risk factors19, including sedentary behaviour20, smoking21, glycaemic control and arterial stiffness22, and obstructive sleep apnoea23. Moreover, we recently reported the heritability of chronotype in this population and found that genetic factors account for 48% of chronotype when adjusted for sex and age, or 38% when adjusted for sex, age and residential zone (rural versus municipal)24. Furthermore, we demonstrated a significant shift towards morningness in the frequency distribution of chronotypes in the Baependi Heart Study population. This raised the question of whether this diurnal preference was actually associated with significantly earlier self-reported bedtimes and wake up times (as opposed to self-reported preferred ones). Here, we have combined the primary datasets underlying these reports, the Morningness-Eveningness questionnaire (MEQ)25, the Pittsburgh Sleep Quality Index (PSQI)26, and sleepiness as assessed with the Epworth Sleepiness Scale (ESS)27. The quantitative answers to PSQI allowed us to consider self-reported rise and bed times.
Results
Population, lifestyle, demographic data, and sex comparisons
Table 1 describes the demographic characteristics of the sample, as well as the sleep measures collected. The entire study sample was 1,847 subjects, out of which 1,334 individuals were considered eligible for statistical comparisons. Subjects missing data-points in one or more questionnaires were excluded from this analysis. The age range of the sample was 18 to 89 years. 31.7% of subjects presented excessive daytime sleepiness (scores equal or above 10 on the ESS), and 34.9% presented scores equal or above 5 on the Pittsburgh Sleep Quality Index (PSQI), meaning that their sleep quality was classified as poor. Women had poorer self-reported sleep quality than men based on PSQI score (means ± standard deviation) (5.4 ± 3.3 vs 4.5 ± 2.9; p < 0.001, Cohen’s d value = 0.18), accounting for a small difference between the sexes. Consistent with this, more women had a PSQI score above 5 than men (39.9% vs 27.8%, Χ2 = 20.79; p < 001). Women also presented later wake up times (means ± standard deviation (06:26 ± 01:17) vs (06:04 ± 01:34); p < 0.01, Cohen’s d value = 0.17), meaning that this difference between sexes was small. Women spent more time in bed than men (means ± standard deviation (07:52 ± 1:26) vs (07:32±01:31) hour:min ± hour:min; p < 0.005, Cohen’s d value = 0.15). Self-reported sleep duration was longer in women than men (means ± standard deviation (07:13 ± 1:33) vs (06:57 ± 1:27) hour:min ± hour:min; p < 0.01); however, the difference was small according to the Cohen’s d value of 0.10.
Description of sleep quality – The PSQI and its components
To further explore the sleep quality in this population, we first evaluated the frequency distribution of PSQI scores by sex (Fig. 1 in Supplementary files). Compared to men, a significant (Χ2 = 20.80; p < 0.001) number of women presented scores above 5 in PSQI, meaning poor sleep quality. In order to investigate the relationship between sex and sleep quality, we analysed the score of the seven different components of the PSQI: Subjective sleep quality, sleep latency, self-reported sleep duration, sleep efficiency, sleep disturbances, use of sleep medication, and daytime dysfunction. Each component is derived from one or more questions and receives a score from 0 to 3, a lower the score indicates better sleep quality. Figure 1 presents the frequency distribution for PSQI classification and PSQI components according to sex. In general, women presented higher scores (worse sleep) for most of the components with the exception of sleep duration and sleep efficiency. Importantly, out of 1,334 questionnaires received, there was not a single score of 3 for subjective sleep quality, meaning that no one evaluated their sleep as “very bad” (Fig. 1B). However, over 60% of subjects from both sexes classified their sleep as “fairly good”.
Frequency distribution for PSQI category and components by sex.
(A) PSQI category. Subjects with scores ≥5 were classified as having poor sleep quality. A higher frequency of women presented poor sleep quality Χ2 = 20.80; p < 0.001. (B–H) show PSQI components. (B) Subjective sleep quality. There was a sex effect on how subjects rated their sleep, with women tending to declare poorer sleep quality X2 = 7.97; p < 0.05. (C) A higher proportion of women reported longer sleep latency X2 = 10.81; p < 0.05. (D) Sleep duration and (E) sleep efficiency, no statistical difference between the sexes. (F) Sleep disturbances, women were more prone to declare having sleep disturbances during the last month X2 = 20.37; p < 0.001; (G) Use of sleep medication: Men declared less use of sleep medication than women during the last month X2 = 29.95; p < 0.00. (H) Daytime dysfunction: A higher proportion of women declared having daytime dysfunction during the last month X2 = 44.89; p < 0.0001.
The frequency distribution analysis of PSQI categories also permit identification of the components sleep latency, sleep duration and sleep disturbances as the main contributors to high PSQI total scores. However, not a single subject described their sleep as “very bad”. Conversely, 23.3% of subjects presented sleep disturbances at least once in the past month, and 10.2% of the sample reported not having a single sleep disturbance episode. In order to identify the most prevalent sleep disturbance in this population, we evaluated the specific answers to the question regarding sleep disturbances (“During the past month, how often you had trouble sleep because you…”) Fig. 2 in Supplementary file presents a detailed description of the frequency of the different sources of sleep disturbance. Interestingly, the most commonly selected answers were waking up in the middle of the night, long sleep latency (>30 minutes), and having to get up to use the bathroom.
Frequency distribution histograms for self-reported sleep patterns derived from the PSQI (1,334 subjects were included).
The upper panel shows the entire population, and the lower panel the same dataset divided by sex. (A and D) show bedtime frequency distribution binned by 1-hour intervals from 19 h to after 04 h. (B and E) show sleep duration frequency distribution binned by 1-hour intervals from 02 h to >11 h of sleep duration. (C and E) show wake-up time frequency distribution binned by 1-hour intervals from 01 h to 11 h. There was higher proportion of male subjects going to bed before 23 h χ2 = 32.83; p < 0.0001 (D), and a higher proportion of male subjects presenting earlier wake up times Χ2 = 45.87; p < 0.001 (F).
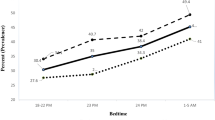
Description of self-reported sleep patterns
Next, to evaluate the sleep patterns of this population, we extracted the information from the PSQI related to the timing and duration of sleep: Bedtime, sleep duration, and wake up time. Self-reported bedtime, wake up time, and sleep duration were plotted in frequency distribution histograms, (Fig. 2). The sleep timings confirmed the “early bird” pattern of the majority of the sample with a large proportion (48%) of subjects presenting bedtimes between 22 and 23 h and wake-up times between 05 and 06 h. A large proportion (67%) of subjects also reported sleeping 7 or more hours.
The lower panel of Fig. 2 shows the frequency distributions of sleep timings according to sex. In general, a higher proportion of male subjects tended to present earlier bedtimes and wake up times (p < 0.01). Furthermore, a higher proportion of male subjects reported sleeping six to eight hours, while a higher proportion of women reporting sleep duration longer than nine hours (p = 0.06). This difference in distribution between short- and long-sleepers is obscured in the average sleep timing values in Table 1, which do not differ significantly between the sexes.
Chronotype associations with sleep patterns, sleep quality, and sleepiness
We classified chronotype using a variation of the method of Robilliard et al.28. In summary, we plotted MEQ scores as a function of age. Because of the previously reported kurtosis of MEQ at higher ages, caused by the imperfect compatibility between the high general morningness of this population and the design of the scale24, only subjects aged less than 60 years old were included in this analysis. A linear regression analysis of age and MEQ score was performed, and subjects presenting MEQ scores 20% above the regression line were categorized as Morning type (M-type) and those 20% below the regression line were Evening type (E-type). Subjects within 20% of the regression line were categorized as Neither type (N-type). See Fig. 3 in Supplementary file for a detailed description of chronotype categorization. One-way ANOVA confirmed that subjects categorized as M-types presented earlier bedtimes and wake up times in comparison to E-types (p < 0.0001 and p < 0.0001). M-types spent on average more time in bed (08:14 ± 1:10 h) than N-types (07:40 ± 1:20 h) and E-types (07:39 ± 1:33 h) (p < 0.05; Bonferroni post-hoc p < 0.01). Consistent with this, M-types also reported longer sleep duration (07:46 ± 1:24) than N-types (07:07 ± 1:28) and E-types (06:59 ± 1:42 h) (p < 0.001; Bonferroni post-hoc p < 0.001). Figure 3 summarizes the sleep patterns for the three categories of chronotype. Regarding sleep quality measured by PSQI, E-type (5.73 ± 3.64 h) subjects presented poorer sleep quality than M-types (4.01 ± 2.62 h) and N-types (4.7 ± 3.1 h) (p < 0.001). No effect of chronotype on sleepiness was found (p = 0.076).
Sleep patterns according to chronotype.
Means and standard error of the mean for Bed time and Wake up time extracted from the PSQI. E-types (N = 125) presented later bedtime in comparison to M-types (N = 97) and N-types (N = 830) subjects. M-types subjects also went to bed earlier than N-types. Bonferroni post-hoc comparisons for (a and b) produced p < 0.0001. E-types also presented later wake up time in comparison to M-types and N-types, Bonferroni post-hoc comparison for (c) yielded p < 0.0001.
Age and sex influence on sleep patterns and chronotype
To further evaluate the relationship between age and sex on sleep patterns and chronotype ontogeny, the sample was binned in 5 age groups (18–31y; 31–40y; 41–50y; 51–60y and 61 and up). Detailed information about the age groups is presented in Table S1.
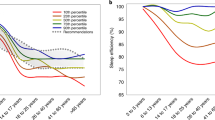
In this way, we evaluated the ontogeny of chronotype and sleep patterns according to sex. Figure 4 summarises the results for comparison of self-reported sleep duration, bedtime, wake up time, time in bed, chronotype, and sleep quality (PSQI score) across age and between sexes. Sex modulated self-reported sleep duration (p = 0.002). Sleep duration also varied according to age in the population (p < 0.001). The interaction between sex and age (p = 0.02) indicated an age-related sex difference in sleep duration (Fig. 4A). Self-reported bedtime was associated with age (p < 0.0001); however, there was no effect of sex (p = 0.29). An interaction between factors was found (p = 0.003), meaning that the age effect on bedtime is modulated by sex (Fig. 4B). Young male subjects presented later bedtimes than women of the same age group, whilst older men presented earlier bedtimes than older women. Sex also modulated wake up time (p < 0.0001); women woke up later than men. Wake up time was modulated by age as well, with older subjects waking up earlier (p < 0.0001); however, no interaction between sex and age was found (p = 0.43) (Fig. 4C). Age (p < 0.0001) and sex (p < 0.0001) also modulated time in bed in an interacting fashion (p < 0.01) (Fig. 4D). Sex was found to influence chronotype (p = 0.0006), and male subjects presented on average higher MEQ scores (greater morningness) than women. Chronotype also changed as a function of age (p < 0.0001) with scores for MEQ increasing with age. There was an interaction between age and sex (p = 0.01). Women aged 51–60 years old were significantly less prone to morningness than men (Bonferroni post hoc test, p = 0.01) (Fig. 4E). Sex modulated sleep quality, with female subjects presenting poorer sleep quality (p < 0.0001). Older subjects also presented poorer sleep quality (p < 0.0001). No interaction was found (Fig. 4E).
Age and sex influence sleep characteristics and chronotype.
Values are presented as means ± standard error (A) Self-reported sleep duration. Bonferroni post hoc test indicated a difference between means of sleep duration at the youngest (18–30y) and the oldest age bins (61-up) for both sexes. (B) Self-reported bedtime. Bonferroni post hoc test suggested a significant advance in bedtime of men from the age bin 18–30y to the 31–40y when women presented later bedtimes. (C) Self-reported wake-up time, Bonferroni post hoc test found significant differences between the youngest (18–30 years) to the second youngest (31–40 years) bins in both sexes, with significant sex differences emerging for the age bin 51–60 years. (D) Time in bed. Bonferroni post hoc test indicated a significant difference between sexes for the youngest age bin (18–30 years). (E) MEQ score, Bonferroni post-hoc testing yielded a statistically significant difference between sexes in the age bin 51–60y, when men reported more morningness. (F) PSQI score, no interaction was found, women presented increasingly poor sleep quality after 41–50 years in comparison to youngest age bin (18–30 years).
Age and sex comparisons also were performed for sleepiness. Sleepiness scores did not change according to age (p = 0.076) or differ between sexes (p = 0.91); consequently, no interaction between factors was found (p = 0.09) (for means and standard error please see Table S1).
Characterizing poor sleepers
Our initial hypothesis was that subjects from Baependi would present high sleep quality, based on consideration the mean of PSQI score for the entire sample (4.9 ± 3.2) one could accept our hypothesis. However, 34.9% of subjects were poor sleepers (scores >5 on PSQI). According to Fig. 4F, PSQI scores are subject to sex and age influences. In order to understand who the poor sleepers are in this population, we evaluated and compared sleep characteristics and chronotype of subjects classified as poor and good sleepers. Table 2 summarises our findings. E-types were significantly overrepresented amongst poor sleepers. Furthermore, poor sleepers also presented later bedtimes (p < 0.001), shorter sleep duration (p < 0.001), spent less time in bed (p = 0.01) and had longer sleep latency (p < 0.001) than subjects classified with good sleep quality.
Discussion
We set out to provide a quantitative and qualitative description of sleep patterns, and describe in detail the relationships between age, sex, and chronotype with sleep quality and timing in this rural population. We found that the self-reported mean bedtime and wake up times were 22:32 ± 01:27 (SD) and 06:17 ± 01:25 respectively, which was consistent with the previously reported morning preference of this population. Sleep duration was 07:07 ± 01:31(hh:min). Additionally, 31.7% of subjects presented with excessive daytime sleepiness and the mean Epworth Sleepiness Score (ESS) was 7.8 ± 4.8, below the threshold for excessive sleepiness. However the mean of PSQI score for the entire sample was 4.9 ± 3.2 and 34.9% were categorized with poor sleep quality. Age played a role in sleep quality — the older the subjects, the poorer sleep quality. Women presented poorer sleep quality than men, but no subject ranked their sleep quality as “very bad” on the Pittsburgh Sleep Quality Index. One of the main factors influencing the total PSQI scores may be sleep latency, which also increased with age. As presented in Fig. 1C there was a high proportion of subjects reporting latencies longer than 30 minutes. Chronotype was another important factor modulating sleep quality. E-types presented poor sleep quality than M-types and N-types.
The Baependi Heart Study population presented a high prevalence of self-reported poor sleep quality. The mean PSQI score for the full sample was 4.9 (3.2), which is higher than studies elsewhere including the control group in the validation of the Brazilian version for the PSQI questionnaire29 (which was 2.5). In other studies, the prevalence of poor sleep was lower in reports from Japan (9.5% of total men and 14.3% of total women having PSQI ≥ 6)30 and China (26.36% having PSQI ≥ 6)31. However, the prevalence of 34.9% of poor sleepers described here is similar to what has been reported in United States32,33 and Korea34. Notwithstanding this point, none of 1,334 subjects included in this report classified their own sleep quality as “very bad”. The mean of subjective sleepiness reported here is comparable to what was found in other studies in less urbanized populations (9.1 ± 3.4 for men and 7.6 ± 3.2 for women)12, but below what has been reported in highly urbanized centres (13.1 ± 2.3 for the entire population)34. Thus, our findings show that poor sleep quality is not necessarily less common in a small quiet rural town with a high prevalence of physical labour (it is worth noting that access to electricity is essentially universal in Baependi). Our results also indicate a strong ontogenetic influence on poor sleep quality. The age range in the study population was 18 to 89 years of age. Men presented mean PSQI score above the threshold for poor sleep quality at the 51–60 years age bin (see Table S1), while females crossed the threshold at the age bin of 41–50 years. These age differences in sleep quality are previously known9,35,36 and have been described worldwide36.
Sex also modulated sleep quality in our study sample. Women presented poorer sleep quality than men. Post-menopausal women presented higher prevalence of sleep disturbance (higher than 40% after 50 years of age37) in comparison to pre-menopausal women. Insomnia is a frequent sleep problem in midlife women, with prevalence around 20%38,39. We did not evaluate specific sleep disturbances or insomnia, although we found a higher prevalence of women reporting sleep latencies longer than 30 minutes more frequently than men (see Fig. 3 in Supplementary file). Also, PSQI scores higher than 5 have been reported as good predictor for primary insomnia40. In this way, further evaluation of the association between menopause and sleep quality should be performed in this population. Furthermore, there can be sex differences related to the way people respond to the questionnaire. In this sense, subjective sleep quality differs between men and women in this community, but it can not be inferred from the observations made here whether the subjective sleep quality differences entirely reflect differences in objective sleep quality.
Another finding of this study was the influence of sex on ontogeny of sleep patterns (bedtime, wake up time and sleep duration). Men and women did not differ significantly in diurnal preference until age of 50 years old when men presented higher morningness. A similar pattern of chronotype ontogeny was described in a very large Brazilian study showing that, although morningness increases with age in both men and women, it does so with different slopes, so that men (who start life with higher average eveningness) have a higher average morningness tendency from age 50 onwards24. However, as previously described24, the Baependi study population presents a general shift towards morningness. This trend can be seen even for the young age bin. The mean score for the youngest age bin in Baependi study was similar to the mean score of age bin >55 years in the previous report from Brazil on the ontogeny of chronotype, which was assembled from a much larger and more metropolitan, population sample, whereas subjects aged 55 and over in Baependi had a much higher morningness24.
Sleep timing and sleep duration were modulated by age and sex as mentioned before. Furthermore, these variables were also strongly associated with chronotype categories. Subjects from Baependi presented considerably earlier wake up and bed times similar to what have been reported in rural populations13,14,41,42, in contrast with late sleep timing reported in metropolitan locations9,43. It has been demonstrated that urbanisation may shift chronotype frequency distribution towards greater eveningness, and a previous study from our group reported the distribution of diurnal preference in Baependi to be shifted towards morningness24. This raised the question whether the actual sleep patterns of the Baependi population would also be shifted to morningness. The results presented here support this hypothesis. Being exposed to a natural high-amplitude light:dark cycle has a strong influence on circadian rhythms, including entrainment of sleep timing6. One can hypothesize that subjects living in areas such as the Baependi region, where they are highly exposed to the natural light:dark cycle, would cause sleep schedules to be significantly more synchronized by this zeitgeber. This is supported by our finding that not only are the preferred bed time and wake times advanced, but also the reported actual ones in comparison to urban areas9,35,43.
This study presents strengths and limitations worth mentioning. We report subjective data based on questionnaires. Although these instruments have been used for sleep research and in sleep clinics worldwide, they contain measures that are subjected to considerable variation in the subject’s personal interpretation. The life experience of Baependi residents may be uniquely reflected in some of their answers. Once supplemented with objective measures, such as actimetry and circadian phase markers, these datasets can be combined with the multiple layers of phenotype data from the Baependi study, and be related to health outcomes and major risk factors. The findings from this interesting cohort show that the presence of electrification does not obligately (or at least not immediately) lead to shifted chronotype distributions towards eveningness and chronotype and delayed sleep and wake timings. They also indicate that an earlier sleep phase does not equate to a perception of better sleep. Taken together, they justify the further investigation of the environmental and lifestyle factors associated with these observations. The longitudinal nature of the Baependi Heart Study will make it possible to investigate whether and how these parameters will change over future years.
Methods
The methodology for recruitment has been described in detail previously18. All participants were aged 18 or older and gave written informed consent before participation. This study protocol conformed to international ethics standards based on the Declaration of Helsinki and was approved by the local ethics committee (Hospital das Clínicas – Universidade de São Paulo, Brazil). This report is based on the evaluation of a sample from 95 genealogical families (as opposed to households), encompassing a total of 1,847 subjects from the Baependi Heart Study. It includes data from the second data collection wave of the Baependi study, when the sleep measures were included. The following instruments were applied as part of two booklets of questionnaires applied in two different sessions containing the following instruments: (i) the Portuguese version of Pittsburgh Sleep Quality Index (PSQI)44, (ii) the Epworth Sleepiness Scale (ESS) in a validated Brazilian Portuguese translation29 and (iii) the Morningness-Eveningness Questionnaire (MEQ)45 as previously described24.
The PSQI was developed to assess the quality and disturbances related to sleep over a period of 1 month. It is composed of seven different components: subjective sleep quality (C1), sleep latency (C2), sleep duration (C3), habitual sleep efficiency (C4), sleep disturbances (C5), use of sleeping medication (C6) and daytime dysfunction (C7). All the seven components are graded on scores from 0 to 3, and the sum of these components scores yields a global score from 0 to 21. The higher the global score, the worse the sleep quality; a score higher than 5 is associated with poor sleep quality26. Furthermore, the PSQI also asks subjects about their habitual sleep patterns, such as bedtime, wake up time, sleep duration, and sleep latency. The Morningness-Eveningness questionnaire aims to identify the chronotype (diurnal preference) of a person. However, to categorize subjects we used a variation of the method of Robilliard et al.28. In summary, we plotted MEQ score against age for all individuals in the study population aged between 18 and 60 years. Further, a linear regression analysis was performed and subjects away from the regression line were selected to be categorized as Morning type (20% above the regression line) or Evening type (20% bellow the regression line). Subjects in between lines were categorized as Neither type. The Fig. 3 in Supplementary file shows a detailed description for the categorization applied here. The Epworth sleepiness scale is compound by 8 situations in which subjects rate the likely to doze in ref. 27. The ESS produces a score from 0 to 24 and results equal or above 10 are considered excessive daytime sleepiness.
From the entire sample, data from 1,334 individuals were considered complete and eligible for statistical comparisons, the results of which are presented here. Data from subjects with missing one or more answers for more than one questionnaire were excluded. Data were analysed by comparison of means using Student’s t tests, one-way analysis of variance, and multiple factors analysis of variance. To evaluate distributions, Χ2 tests were applied. Age was considered as continuous variable for correlational analysis and the sample was binned into five age groups (18–30y, 31–40y, 41–50y, 51–60y and 61- years) to perform mean comparisons.
Additional Information
How to cite this article: Beijamini, F. et al. Timing and quality of sleep in a rural Brazilian family-based cohort, the Baependi Heart Study. Sci. Rep. 6, 39283; doi: 10.1038/srep39283 (2016).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Cappuccio, F. P., Cooper, D., Delia, L., Strazzullo, P. & Miller, M. A. Sleep duration predicts cardiovascular outcomes: A systematic review and meta-analysis of prospective studies. Eur. Heart J. 32, 1484–1492 (2011).
Knutson, K. L. Sleep duration and cardiometabolic risk: A review of the epidemiologic evidence. Best Pract. Res. Clin. Endocrinol. Metab. 24, 731–743 (2010).
Bryant, P. A., Trinder, J. & Curtis, N. Sick and tired: Does sleep have a vital role in the immune system? Nat. Rev. Immunol. 4, 457–67 (2004).
Walker, M. P. The Role of Sleep in Cognition and Emotion. Ann. N. Y. Acad. Sci. 1156, 168–197 (2009).
Beersma, D. G. M. & Gordijn, M. C. M. Circadian control of the sleep-wake cycle. Physiol. Behav. 90, 190–195 (2007).
Wright, K. P. et al. Entrainment of the Human Circadian Clock to the Natural Light-Dark Cycle. Curr. Biol. 23, 1554–1558 (2013).
Glaskin, K. & Chenhall, R. Sleep Around the World. (Palgrave Macmillan). doi: 10.1057/9781137315731.
Czeisler, C. A. Perspective: Casting light on sleep deficiency. Nature 497, S13–S13 (2013).
Santos-Silva, R. et al. Increasing trends of sleep complaints in the city of Sao Paulo, Brazil. Sleep Med. 11, 520–524 (2010).
Carnethon, M. R. et al. Disparities in sleep characteristics by race/ethnicity in a population-based sample: Chicago Area Sleep Study. Sleep Med. 18, 50–5 (2016).
Centers for Disease Control and Prevention - Unhealthy sleep-related behaviors–12 States, 2009. Centers for Disease Control and Prevention 60 (2011).
Evans, D. S. et al. Habitual sleep/wake patterns in the Old Order Amish: heritability and association with non-genetic factors. Sleep 34, 661–669 (2011).
Moreno, C. R. C. et al. Sleep patterns in Amazon rubber tappers with and without electric light at home. Sci. Rep. 5, 14074 (2015).
de la Iglesia, H. O. et al. Access to Electric Light Is Associated with Shorter Sleep Duration in a Traditionally Hunter-Gatherer Community. J. Biol. Rhythms 30, 342–350 (2015).
Peixoto, T. A. C., da Silva, A. G. T., Carskadon, M. A. & Louzada, F. M. Adolescents living in homes without electric lighting have earlier sleep times. Behav. Sleep Med. 7, 73–80 (2009).
Knutson, K. L. Sleep duration, quality, and timing and their associations with age in a community without electricity in haiti. Am. J. Hum. Biol. 26, 80–86 (2014).
Yetish, G. et al. Natural Sleep and Its Seasonal Variations in Three Pre-industrial Societies. Curr. Biol. 25, 2862–2868 (2015).
Egan, K. J. et al. Cohort profile: the Baependi Heart Study - a family-based, highly admixed cohort study in a rural Brazilian town. BMJ Open, doi: 10.1038/clpt.2013.24.52 (2016).
de Oliveira, C. M., Pereira, A. C., de Andrade, M., Soler, J. M. & Krieger, J. E. Heritability of cardiovascular risk factors in a Brazilian population: Baependi Heart Study. BMC Med. Genet. 9, 32 (2008).
Horimoto, A. R. V. R. et al. Heritability of physical activity traits in Brazilian families: the Baependi Heart Study. BMC Med. Genet. 12, 155 (2011).
Horimoto, A. R. et al. Genetic analyses of smoking initiation, persistence, quantity, and age-at-onset of regular cigarette use in Brazilian families: the Baependi Heart Study. BMC Med. Genet. 13, 9 (2012).
de Oliveira Alvim, R. et al. Glycemic control and arterial stiffness in a Brazilian rural population: Baependi Heart Study. Diabetol. Metab. Syndr. 7, 86 (2015).
de Paula, L. K. G. et al. Heritability of Obstructive Sleep Apnea in a rural population. CHEST J. 23, 575–575 (2015).
von Schantz, M. et al. Distribution and heritability of diurnal preference (chronotype) in a rural Brazilian family-based cohort, the Baependi study. Sci. Rep. 5, 9214 (2015).
Horne, J. A. & Ostberg, O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int. J. Chronobiol. 4, 97–110 (1976).
Buysse, D. J., Reynolds, C. F. 3Rd, Monk, T. H., Berman, S. R. & Kupfer, D. J. The Pittsburgh Sleep Quality Index: A New Instrument for Psychiatric Practice and Research. Psychiatry Res 28, 193–213 (1989).
Johns, M. W. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14, 540–545 (1991).
Robilliard, D. L. et al. The 3111 Clock gene polymorphism is not associated with sleep and circadian rhythmicity in phenotypically characterized human subjects. J. Sleep Res. 11, 305–312 (2002).
Bertolazi, A. et al. Portuguese-language version of the Epworth sleepiness scale: validation for use in Brazil. J. Bras. Pneumol. 35, 877–883 (2009).
Okubo, N. et al. Relationship between self-reported sleep quality and metabolic syndrome in general population. BMC Public Health 14, 562 (2014).
Liu, R.-Q. et al. Poor sleep quality associated with high risk of hypertension and elevated blood pressure in China: results from a large population-based study. Hypertens. Res. 39, 54–59 (2016).
Wong, P. M., Hasler, B. P., Kamarck, T. W., Muldoon, M. F. & Manuck, S. B. Social Jetlag, Chronotype, and Cardiometabolic Risk. J. Clin. Endocrinol. Metab. 100, 4612–4620 (2015).
Lauderdale, D. S. et al. Cross-sectional and Longitudinal Associations Between Objectively Measured Sleep Duration and Body Mass Index: The CARDIA Sleep Study. Am. J. Epidemiol. 170, 805–813 (2009).
Hwangbo, Y., Kim, W. J., Chu, M. K., Yun, C. H. & Yang, K. I. Habitual Sleep Duration, Unmet Sleep Need, and Excessive Daytime Sleepiness in Korean Adults. J. Clin. Neurol. 12, 194–200 (2016).
van de Straat, V. & Bracke, P. How well does Europe sleep? A cross-national study of sleep problems in European older adults. Int. J. Public Health 60, 643–650 (2015).
Stranges, S., Tigbe, W., Gómez-Olivé, F. X., Thorogood, M. & Kandala, N.-B. Sleep Problems: An Emerging Global Epidemic? Findings From the INDEPTH WHO-SAGE Study Among More Than 40,000 Older Adults From 8 Countries Across Africa and Asia. Sleep 66, A42–A42 (2012).
Hall, M. H., Kline, C. E. & Nowakowski, S. Insomnia and sleep apnea in midlife women: prevalence and consequences to health and functioning. F1000Prime Rep. 7, 63 (2015).
Zhang, B. & Wing, Y.-K. Sex differences in insomnia: a meta-analysis. Sleep 29, 85–93 (2006).
Backhaus, J., Junghanns, K., Broocks, A., Riemann, D. & Hohagen, F. Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J. Psychosom. Res. 53, 737–740 (2002).
Duarte, L. L. et al. Chronotype ontogeny related to gender. Braz. J. Med. Biol. Res. 47, 316–20 (2014).
Kohatsu, N. D. et al. Sleep Duration and Body Mass Index in a Rural Population. Arch Intern Med 166, 1701–1705 (2006).
Habte-Gabr, E. et al. Sleep Patterns in Rural Elders: Health, and Psychobehavioral Demographic, Correlates. J. Clin. Epidemiol. 44, 5–13 (1991).
Tufik, S., Santos-Silva, R., Taddei, J. A. & Bittencourt, L. R. A. Obstructive Sleep Apnea Syndrome in the Sao Paulo Epidemiologic Sleep Study. Sleep Med. 11, 441–446 (2010).
Bertolazi, A. N. et al. Validation of the Brazilian Portuguese version of the Pittsburgh Sleep Quality Index. Sleep Med. 12, 70–75 (2011).
Horne, J. A. & Östberg, O. A Self-Assessment questionnaire to determine morningngess-eveningness in human circadian rhythms. Int. J. Chronobiol. 4, 97–110 (1976).
Acknowledgements
We are very thankful to the population of Baependi for their participation in the Baependi Heart Study. This study was supported by awards from CNPq to FB, HV and MvS (400791/2015-5), and by the Global Innovation Initiative to MvS (jointly funded by the British Council and the UK Department of Business and Skills), and by grants from Fundação de Amparo a Pesquisa do Estado de São Paulo (FAPESP, 2013/17368-0, to ACP), and Hospital Samaritano Society [Grant 25000.180.664/2011-35], through the Ministry of Health to Support Program Institutional Development of the Unified Health System (SUS-PROADI).
Author information
Authors and Affiliations
Contributions
Beijamini F., Data analysis, manuscript preparation. Egan, K., J., Data analysis and manuscript preparation. De Paula L.K.G., Data collection. Taporoski, T.P., Data collection, manuscript preparation. Negrão, A.B., Study design and manuscript preparation. Horimoto, A.R.V.R., Data analysis and interpretation. Duarte N.E., Data analysis and interpretation. Vallada, H., Data analysis and manuscript preparation. Krieger, J.E., Study design and manuscript preparation. Knutson, K.L., Study design, data analysis and manuscript preparation. Lorenzi-Filho, G., Study design and manuscript preparation. Pedrazzoli, M., Study design and manuscript preparation. Pereira, A.C., Study design and manuscript preparation. von Schantz, M. Study design, data analysis and manuscript preparation.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Beijamini, F., Knutson, K., Lorenzi-Filho, G. et al. Timing and quality of sleep in a rural Brazilian family-based cohort, the Baependi Heart Study. Sci Rep 6, 39283 (2016). https://doi.org/10.1038/srep39283
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep39283
This article is cited by
-
Sleepiness, sleep deprivation, quality of life, mental symptoms and perception of academic environment in medical students
BMC Medical Education (2021)
-
Sleep and light exposure across different levels of urbanisation in Brazilian communities
Scientific Reports (2018)
-
Comparison between an African town and a neighbouring village shows delayed, but not decreased, sleep during the early stages of urbanisation
Scientific Reports (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.