Abstract
Zika virus co-circulates with dengue in tropical and sub-tropical regions. Cases of co-infection by dengue and Zika have been reported, the implication of this co-infection for an integrated intervention program for controlling both dengue and Zika must be addressed urgently. Here, we formulate a mathematical model to describe the transmission dynamics of co-infection of dengue and Zika with particular focus on the effects of Zika outbreak by vaccination against dengue among human hosts. Our analysis determines specific conditions under which vaccination against dengue can significantly increase the Zika outbreak peak, and speed up the Zika outbreak peak timing. Our results call for further study about the co-infection to direct an integrated control to balance the benefits for dengue control and the damages of Zika outbreak.
Similar content being viewed by others
Introduction
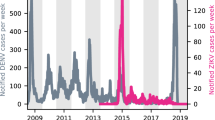
Dengue and Zika are both vector-borne diseases in tropical and sub-tropical regions with a common vector, dengue and Zika both belong to the family Flaviviridae and genus Flavivirus. Dengue is a prevalent disease being transmitted by the bite of a mosquito infected with one of the four serotypes1,2 while Zika is an emerging disease. Zika virus was first isolated in Uganda in 19473, and there was an outbreak of Zika in Yap, Federated States of Micronesia4 in 2007, and in French Polynesia5 till 2013. By the end of January 2016, autochthonous circulation of Zika was reported in more than 20 countries or territories in South, Central, and North America and the Caribbean6,7,8,9,10,11,12, leading to the declaration of WHO that Zika virus is a global public health emergency13.
Recent clinical and experimental evidences support immunological cross-reactivity between dengue and Zika14,15,16,17. In particular, these evidences show that plasma to dengue was able to drive antibody-dependent enhancement of Zika infection. Co-circulation of multiple serotypes of dengue and dengue-Zika co-circulation have previously been reported in refs 18, 19, 20. In particular, co-infection of dengue and Zika were observed in two patients during the Zika outbreak in New Caledonia in 201418, and in two patients during the Zika outbreak in Tuparetama of Brazil in 201519. The co-circulation could be a potentially series public concern given that more than a third of the world’s population lives in countries where dengue is endemic21, with the dengue belt covering Central America, most of South America, sub-Saharan Africa, India, and South East Asia. Relevant to this co-infection is the development of vaccine products against dengue by Sanofi Pasteur, and the clinical trials by Butantan and Takeda. Thus, it is an important urgent issue for public health decision makers to know how dengue immunization program impacts Zika transmission when co-circulation becomes wide spread. Specially, under which conditions implemented dengue immunization control programs may boost the outbreak of Zika is no longer a thought-provoking issue. Developing a framework to address this issue through a mathematical model is the main objective of this study.
Much progress has been made for modelling dengue infection dynamics including the role of cross-reactive antibodies for the four different dengue serotypes as discussed in the review paper22. The dengue transmission dynamics becomes very complex because of the co-circulating serotypes in many endemic areas, and the absence of long-term cross-immunity23,24,25,26. In 1997, Feng et al.27 proposed a two-stain model with the vector population being subdivided into a susceptible class and two serotype-specific infectious classes and the host populations being described by the SIR-type model for each serotype. Esteva and Vargas28 considered a further model by including an explicit state for individuals who recovered from primary infections. Nuraini et al.29 and Sriprom et al.30 extended Esteva’s model by accounting for two separate symptomatic and asymptomatic compartments for secondary infections. A four-serotype model was considered in these papers31,32,33. Different from these previous studies, recently developed mathematical models have emphasized the evaluation of the impact of co-circulation of the four serotypes mainly among hosts34,35,36,37,38,39,40. In contrast to dengue, the epidemiology of Zika among humans remains poorly understood, despite some recent outbreaks of modelling activities41,42,43,44.
We should mention that mathematical models of co-infection of two infectious diseases among humans have been developed in many different settings45, including co-infection of HIV with TB46,47,48,49,50,51, HCV52,53, two strains of HIV54, HDV and HBV55, multi-strains of influenza56,57. To our best knowledge, our work here is the first attempt to develop a mathematical model to address the co-infection of dengue and Zika and its implication to Zika prevalence. Our purpose here is to propose a mathematical model of co-infection of dengue and Zika with particular focus on the potential impact and implication for Zika outbreak of vaccination against dengue in humans.
Preliminaries
We stratify the total human population, Nh(t), into:
S(t): the number of humans susceptible to both dengue and Zika at time t;
Id(a, t): the number of dengue-infected humans with infection age a at time t, who can also be infected by Zika virus and move to Idz(a, b, t);
Iz(b, t): the number of Zika-infected humans with infection age b at time t, who can also be infected by dengue and move to Idz(a, b, t);
Idz(a, b, t): the number of dengue and Zika-infected humans with dengue infection age a and Zika infection age b at time t;
Rd(t): the number of humans recovered from dengue at time t, who can also be infected by Zika and move to  ;
;
Rz(t): the number of humans recovered from Zika at time t, who can also be infected by dengue and move to  ;
;
 : the number of Zika-infected humans with Zika-infection age b, at time t, who are immune to dengue;
: the number of Zika-infected humans with Zika-infection age b, at time t, who are immune to dengue;
 : the number of dengue-infected humans with dengue-infection age a, at time t, who are immune to Zika;
: the number of dengue-infected humans with dengue-infection age a, at time t, who are immune to Zika;
Rdz(t): the number of humans recovered from dengue and Zika at time t, who can neither be infected by dengue nor Zika.
Mosquito population Nm is divided into Sm, Imd, Imz, Imdz, representing the density of mosquitos who are susceptible, infected with dengue only, infected with Zika only, infected with both dengue and Zika. The transmission diagram of co-infection of dengue and Zika among humans and mosquitos is shown in Fig. 1.
We start with an intuitive view about the effects of vaccination against dengue among humans on the outbreak of Zika through a very simple static transmission model illustrated in Fig. 2. Here the susceptible humans (S) can be infected with Zika virus via three different routes, namely
Sub-flow diagram of Zika infection among humans.
Here, we assume that the susceptible humans (S) are infected by dengue with a ratio of Pd on average and by Zika with a ratio of Pz on average. We further assume that the class Id will be infected with Zika at a ratio of Pdz while the other part will recover to Rd. Moreover, we assume that the individuals in compartment Rd can be further infected with Zika at a ratio of  .
.

Let the initial number of susceptible humans (S) be S0. If we do not inoculate against dengue, then the final average number of humans infected with Zika virus through the above three routes (i.e. Iz, Idz,  ) can be calculated as
) can be calculated as

Therefore, the total number of humans infected with Zika virus should be

Now we assume that the coverage rate of dengue vaccine is Pc and the efficacy rate of dengue vaccine is P0. Then the effective coverage rate of dengue vaccine is Pv = P0Pc. The portion of susceptible humans successfully inoculated with dengue vaccine will directly transfer to the compartment Rd. Therefore, the final average numbers of Iz, Idz and  become
become

Then, the total number of humans infected with Zika virus after vaccination against dengue should be

Comparing equation (2) with equation (4), we can see that with the implementation of vaccination of dengue the final numbers of Iz and Idz decrease while the final number of  increases. To determine whether the total number of humans infected with Zika is increased or not, we let
increases. To determine whether the total number of humans infected with Zika is increased or not, we let

where  is the ratio at which the part of the susceptible humans inoculated with dengue vaccine are infected with Zika,
is the ratio at which the part of the susceptible humans inoculated with dengue vaccine are infected with Zika,  is the total ratio at which the susceptible humans are infected with Zika through the above mentioned three routes described in (1). It follows from equation (6) that if
is the total ratio at which the susceptible humans are infected with Zika through the above mentioned three routes described in (1). It follows from equation (6) that if  (i.e.
(i.e.  , as shown in the red region of Fig. 3(A)), then the higher ratio the susceptible humans are inoculated with dengue vaccine, the more the total number of humans are infected with Zika virus compared with the case without dengue vaccination, as shown in Fig. 3(B,C); if
, as shown in the red region of Fig. 3(A)), then the higher ratio the susceptible humans are inoculated with dengue vaccine, the more the total number of humans are infected with Zika virus compared with the case without dengue vaccination, as shown in Fig. 3(B,C); if  (i.e.
(i.e.  , as shown in the green region of Fig. 3(A)), inoculating dengue vaccine can decrease relatively the total number of humans infected with Zika virus, as shown in Fig. 3(B,D). This discussion, based on a static infection outcome analysis, suggests a likely scenario that, under certain conditions, vaccination against dengue can significantly boost the outbreak of Zika. Our analysis below is to theoretically and numerically examine these conditions with our proposed transmission dynamics model.
, as shown in the green region of Fig. 3(A)), inoculating dengue vaccine can decrease relatively the total number of humans infected with Zika virus, as shown in Fig. 3(B,D). This discussion, based on a static infection outcome analysis, suggests a likely scenario that, under certain conditions, vaccination against dengue can significantly boost the outbreak of Zika. Our analysis below is to theoretically and numerically examine these conditions with our proposed transmission dynamics model.
(A) Schematic scenarios which show that vaccination against dengue can increase the total number of Zike infections if the parameters Pz and  are located in the red region while it can decrease the total number of Zika infections in the green region; (B) The relationship of the total number of Zika infections to the ratio
are located in the red region while it can decrease the total number of Zika infections in the green region; (B) The relationship of the total number of Zika infections to the ratio  with or without vaccination against dengue. Here, Pz = 0.3 and Pv = 0.7; (C) The relationship of ΔZ to the effective coverage rate of dengue vaccine Pv while the parameters Pz and
with or without vaccination against dengue. Here, Pz = 0.3 and Pv = 0.7; (C) The relationship of ΔZ to the effective coverage rate of dengue vaccine Pv while the parameters Pz and  are chosen in the red region of (A) with Pz = 0.3; (D) The relationship of ΔZ to the effective coverage rate of dengue vaccine Pv while the parameters Pz and
are chosen in the red region of (A) with Pz = 0.3; (D) The relationship of ΔZ to the effective coverage rate of dengue vaccine Pv while the parameters Pz and  are chosen in the green region of (A) with Pz = 0.3. Other parameters in (A–D) are fixed as Pd = 0.3, Pdz = 0.1, S0 = 100000.
are chosen in the green region of (A) with Pz = 0.3. Other parameters in (A–D) are fixed as Pd = 0.3, Pdz = 0.1, S0 = 100000.
Model formulation
We assume a SI-type model for dengue and Zika co-infection for the mosquito population. The model equations for mosquitos give

Here, Λ is the recruitment rate of mosquitos, and the definitions for other parameters are listed in Table 1. We assume SIR-type model for dengue and Zika co-infection in human population and formulate the following age-structured model to describe the dynamics of co-infection of dengue and Zika among humans:

Here γd(a) is the recover rate at which individuals in the compartment Id with dengue-infection age a recover to the class Rd, γz(b) denotes the recover rate at which individuals in the class Iz with Zika-infection age b move to the compartment Rz,  represents the recover rate at which individuals in the class
represents the recover rate at which individuals in the class  with Zika-infection age b recover to the compartment Rdz, and
with Zika-infection age b recover to the compartment Rdz, and  is the recover rate at which individuals in the class
is the recover rate at which individuals in the class  with dengue-infection age a move to compartment Idz, γdz(a, b) denotes the recover rate at which individuals in the class Idz with time-since-infection a for dengue and time-since-infection b for Zika recover to the compartment Rdz directly, γdz(a) represents the recover rate at which individuals in the class Idz transit to the compartment
with dengue-infection age a move to compartment Idz, γdz(a, b) denotes the recover rate at which individuals in the class Idz with time-since-infection a for dengue and time-since-infection b for Zika recover to the compartment Rdz directly, γdz(a) represents the recover rate at which individuals in the class Idz transit to the compartment  due to recovery of dengue, and γdz(b) is the recover rate at which individuals in the class Idz transit to the compartment
due to recovery of dengue, and γdz(b) is the recover rate at which individuals in the class Idz transit to the compartment  due to recovery of Zika. The definitions for other parameters independent of infection ages are given in Table 1. Here, the condition Idz(0, 0, t) = 0 means that the susceptible individuals can not be infected with dengue and Zika in the same time.
due to recovery of Zika. The definitions for other parameters independent of infection ages are given in Table 1. Here, the condition Idz(0, 0, t) = 0 means that the susceptible individuals can not be infected with dengue and Zika in the same time.
We assume that

and

Define  , i.e. the total number of humans who are infected with dengue at time t, and can further be infected by Zika. Then, we have
, i.e. the total number of humans who are infected with dengue at time t, and can further be infected by Zika. Then, we have

Further, if we assume that the recover rate γd(a) is independent of dengue-infection age a, that is, γd, we have  . Then formula (9) yields
. Then formula (9) yields

Similarly, if the recover rate γz(b) is independent of Zika-infection age b, the total number of humans infected with Zika, given by  , reads
, reads

With similar calculation, we can get the derivative of the compartment Idz(t) as follows:

Also, when we assume that the recover rates γdz(a, b), γdz(a) and γdz(b) are all constants, denoted by  and
and  , respectively, then formula (12) gives
, respectively, then formula (12) gives

Moreover, define the total number of humans who are immune to dengue but infected with Zika as  and the total number of humans who are immune to Zika but infected with dengue as
and the total number of humans who are immune to Zika but infected with dengue as  . By assuming the recover rates
. By assuming the recover rates  and
and  being independent of infection ages (i.e.,
being independent of infection ages (i.e.,  and
and  ), we easily obtain that
), we easily obtain that

and

Based on the above assumptions and discussions, the double age-structured model is reduced to the following ODE model:

We call model (16) with model (7) as system S*. It follows from model (16) that the total number of humans Nh(t) is a constant, denoted by Nh. Let  and Imd = Imz = Imdz = 0. Then we can show that system S* has a disease-free equilibrium, which gives
and Imd = Imz = Imdz = 0. Then we can show that system S* has a disease-free equilibrium, which gives

Using the next generation matrix introduced in papers58,59, we can calculate the basic reproduction number for system S*, denoted by R0 (see electronic supplementary information for details). This is the spectral radius of the next generation matrix and given by

Here,  and
and  are the basic reproduction numbers for the dengue-only model and Zika-only model, respectively. Consequently, when Rz > 1 (Rd > 1), then there is an outbreak of Zika (dengue) while the number of Zika (dengue) infections will directly decrease to zero if Rz < 1 (Rd < 1).
are the basic reproduction numbers for the dengue-only model and Zika-only model, respectively. Consequently, when Rz > 1 (Rd > 1), then there is an outbreak of Zika (dengue) while the number of Zika (dengue) infections will directly decrease to zero if Rz < 1 (Rd < 1).
Main Results
In this section, we carry out numerical simulations for the dynamic system S* in order to examine effect of dengue vaccination on the outbreak of Zika. In our simulations, we vary three parameters βdz, βrz and Λ, and fix all the other parameter values as follows:

Let the initial values IV(0) for system S* be given by

Let the effective coverage rate of vaccination against dengue among humans be Pv. When inoculating dengue vaccine to humans at the outset of the outbreak of dengue and Zika, the initial conditions of model S* become as  with
with  while other vector components remaining unchanged.
while other vector components remaining unchanged.
We first simulate system S* by fixing the parameters βdz and βrz as 0.18 and 0.05, respectively. We examine the variation of  with parameter Λ with or without inoculating dengue vaccine, as shown in Fig. 4. As we can see, when the parameter Λ varies in the interval from 10000 to 1000000 vaccination against dengue can lead to two opposite results for the outbreak of Zika. That is, when Λ is relatively low, the effect of dengue vaccine on the outbreak of Zika is not noticeable. However, if Λ increases to relatively large, vaccination against dengue among humans will significantly boost the outbreak of Zika with a much higher outbreak peak compared with that without vaccination. The lower and upper bounds of this parameter value are determined from intensive numerical simulations to clearly illustrate these two opposite scenarios. In particular, we plot solutions to system S* (shown in Figs 5 and 6) with Λ being fixed as 10000 and 1000000 (the lower and higher boundary value of the interval of Λ chosen in Fig. 4), respectively. Figures 5(H) and 6(H) demonstrate these two opposite situations: dengue vaccination results in the number of human infected with Zika either decline or increase. It follows from Figs 5 and 6 that vaccination against dengue among humans will always reduce the number of humans infected with dengue (including the compartments Id,
with parameter Λ with or without inoculating dengue vaccine, as shown in Fig. 4. As we can see, when the parameter Λ varies in the interval from 10000 to 1000000 vaccination against dengue can lead to two opposite results for the outbreak of Zika. That is, when Λ is relatively low, the effect of dengue vaccine on the outbreak of Zika is not noticeable. However, if Λ increases to relatively large, vaccination against dengue among humans will significantly boost the outbreak of Zika with a much higher outbreak peak compared with that without vaccination. The lower and upper bounds of this parameter value are determined from intensive numerical simulations to clearly illustrate these two opposite scenarios. In particular, we plot solutions to system S* (shown in Figs 5 and 6) with Λ being fixed as 10000 and 1000000 (the lower and higher boundary value of the interval of Λ chosen in Fig. 4), respectively. Figures 5(H) and 6(H) demonstrate these two opposite situations: dengue vaccination results in the number of human infected with Zika either decline or increase. It follows from Figs 5 and 6 that vaccination against dengue among humans will always reduce the number of humans infected with dengue (including the compartments Id,  , and Idz), and hence leads to a reduction in the total number of humans infected with dengue (i.e.
, and Idz), and hence leads to a reduction in the total number of humans infected with dengue (i.e.  ). However, vaccination against dengue may increase the number of individuals in the compartment
). However, vaccination against dengue may increase the number of individuals in the compartment  . This explains the two opposite results about the effects of the dengue vaccination on the Zika outbreak. Note that when Λ = 1000000, with which vaccination against dengue can significantly boost the Zika outbreak, we can calculate that Rd = Rz = 2.82, within the range of basic reproduction numbers for dengue and Zika in the literatures42,60,61,62,63,64.
. This explains the two opposite results about the effects of the dengue vaccination on the Zika outbreak. Note that when Λ = 1000000, with which vaccination against dengue can significantly boost the Zika outbreak, we can calculate that Rd = Rz = 2.82, within the range of basic reproduction numbers for dengue and Zika in the literatures42,60,61,62,63,64.
The value of  in time and with respect to the recruitment rate of mosquitos Λ being varied in the interval [10000, 1000000].
in time and with respect to the recruitment rate of mosquitos Λ being varied in the interval [10000, 1000000].
The mesh surface represents the solutions without inoculating dengue vaccine to susceptible humans while the other one are the solutions when the susceptible humans are inoculated with dengue vaccine at a ratio of 0.7. Parameters βdz and βrz are fixed as 0.18, 0.05, respectively.
Solutions of model S* with the solid lines being the solutions without vaccination and the dashed lines being the solutions after inoculating the dengue vaccine at the ratio of Pv = 0.7.
Here we fixed Λ = 1000000 and all the other parameters as the same as those in Fig. 5.
Further, we examine the effects of the effective coverage rate Pv on the outbreak of Zika. Fix parameters βdz = 0.05, βrz = 0.18, Λ = 10000 and let the parameter Pv vary, Fig. 7(A) shows that a higher effective coverage rate of vaccination can result in a much higher peak of the outbreak of Zika. Moreover, if we choose Λ = 1000000, then we observe that with a higher rate of vaccination against dengue not only the peak of the outbreak of Zika can be significantly increased, but also the Zika outbreak peak much earlier, as shown in Fig. 7(B).
Considering the number of the accumulated Zika infections, we obtained two similar opposite results. Figure 7(C) shows that with a higher rate of vaccination against dengue the number of accumulated Zika infections will increase significantly, while Fig. 7(D) illustrates that vaccination against dengue may reduce the number of the accumulated Zika infections. In Fig. 7(D) we assumed that βrz = βz = 0.05 while in Fig. 7(C) we assumed that 0.18 = βrz > βz = 0.05 based on the emerging clinical evidence of enhancement14,15,16,17. Comparisons between these scenarios clearly indicate, under the conditions reflected by the parameter values, that dengue vaccination may indeed lead to significant increase in Zika infections.
Conclusion and Discussion
There are increasing evidence of co-infection of dengue and Zika. Due to similar transmission routes with the same host species, some intervention strategies such as vector control are effective for curbing both dengue and Zika. However, other interventions such as vaccination against one virus may be harmful to the control of another, specially when enhancement occurs to favor the spread of the virus not covered with vaccine. Our study examined the implication of this enhancement for Zika outbreaks when vaccination against dengue in humans is applied. We initially formulated a very simple static transmission model to give an intuitive illustration that vaccination against dengue among humans may significantly boost Zika transmission among the population.
In order to theoretically verify this illustration, we then proposed a dynamic model to describe the dynamics of co-infection of dengue and Zika. More specifically, we developed a novel model with double age-structures for dengue and Zika, extending the general age-structure model65,66,67 by incorporating compartments with specific dengue-infection and Zika-infection age. Under certain stage-specific homogenetical assumptions about the virus dynamics characteristics, we simplified our double age-structured model to an ODE model, for which the basic reproduction number can be calculated.
We also numerically investigated the dynamics of model S* and obtained some observations which are in agreement with the conclusions from the analysis of our static transmission model in Section 2. Figure 4 shows that vaccination against dengue among humans may result in the total number of humans infected with Zika virus decline or increase, depending on the parameter Λ, the recruitment rate of mosquitos. In particular, it significantly enlarges the peak of the outbreak of Zika when Λ is relatively large. It follows from Figs 5 and 6 that this enlarged outbreak of Zika by vaccination against dengue is due to multiple factors. Vaccination against dengue can reduce the numbers of Iz and Idz while it always increases the number of  . Thus the balance of increase in the number of
. Thus the balance of increase in the number of  and decrease in the number of Iz and Idz determines whether the total number of infected with Zika increase or not. Further, we observed that a higher rate of vaccination against dengue can also results in a higher and earlier peak of the outbreak of Zika, as shown in Fig. 7(A,B). Comparing Fig. 7(B) with Fig. 7(A), we observe that the conclusion that vaccination against dengue can boost Zika outbreak remains true for a wide range of mosquito index values (when the recruitment rate of mosquito decreases from 1000000 to 10000). This conclusion is also shown in Fig. S2 (electronic supplementary information) when the mosquito mortality rate μm varies. Comparison between Fig. 7(B) and Fig. 7(A) however also shows that reducing the mosquito indices can significantly decrease the magnitude of Zika outbreak as the number of Zika cases at the peak time can be reduced substantially. Therefore, given the simultaneous impact on both dengue and Zika outbreaks, vector control should be always implemented regardless of the availability of vaccine. Figure 7(C,D) further confirm that the accumulated Zika infections may be greater for a greater rate of vaccination of dengue vaccine to human. Sensitive analyses show that parameters βz, βdz, Λ and μm can significantly affect the outbreak of Zika, in terms of both the accumulated Zika infections and the daily number of Zika infections (see electronic supplementary information for details).
and decrease in the number of Iz and Idz determines whether the total number of infected with Zika increase or not. Further, we observed that a higher rate of vaccination against dengue can also results in a higher and earlier peak of the outbreak of Zika, as shown in Fig. 7(A,B). Comparing Fig. 7(B) with Fig. 7(A), we observe that the conclusion that vaccination against dengue can boost Zika outbreak remains true for a wide range of mosquito index values (when the recruitment rate of mosquito decreases from 1000000 to 10000). This conclusion is also shown in Fig. S2 (electronic supplementary information) when the mosquito mortality rate μm varies. Comparison between Fig. 7(B) and Fig. 7(A) however also shows that reducing the mosquito indices can significantly decrease the magnitude of Zika outbreak as the number of Zika cases at the peak time can be reduced substantially. Therefore, given the simultaneous impact on both dengue and Zika outbreaks, vector control should be always implemented regardless of the availability of vaccine. Figure 7(C,D) further confirm that the accumulated Zika infections may be greater for a greater rate of vaccination of dengue vaccine to human. Sensitive analyses show that parameters βz, βdz, Λ and μm can significantly affect the outbreak of Zika, in terms of both the accumulated Zika infections and the daily number of Zika infections (see electronic supplementary information for details).
Most existing studies on the multi-serotype models of vector-host transmission of dengue focus on the importance of subsequent infections with different dengue serotypes. It was assumed that the patients can be subsequently infected by another serotypes after recovering from one serotype. In our consideration of dengue-Zika co-infection, we extended these models by adding a new compartment of humans as well as mosquitos infected by both of Zika and dengue simultaneously. From our numerical analysis, the parameter βdz (i.e. the transmission rate of the compartment of mosquitos infected with dengue and Zika to susceptible humans), which is related to the newly added compartment Imdz, can have important influences on the dynamics of the co-infection model. For the models of co-infection of HIV with TB and HCV, a SI-type model is usually assumed as the basic model for each disease. In comparison with these models, our model with SIR-type for humans is different to handle the asymmetric vector-host interaction as discussed in ref. 27, and to allow recovered (or vaccinated) individuals from one virus to have higher risk of infection by another. Our analysis indicates that with a big recruitment rate of mosquitos Λ vaccination against dengue among humans can significantly boost the Zika outbreak (as shown in Fig. 6(H)), and cause the Zika outbreak peak coming early with a bigger mosquito to humans transmission rate βrz and lower βdz (as shown in Fig. 7(B)). It is important to note that a safe, effective and affordable dengue vaccine against the four strains offers an important tool to reach the WHO goal of reducing dengue morbidity by at least 25% and mortality by at least 50% by 202068. The first dengue vaccine, Dengvaxiar(CYD-TDV) (developed by Sanofi Pasteur), was licensed in Mexico in 201569; and two dengue vaccine candidates (developed by Butantan and Takeda) entered the Phase III trails in early 201670,71,72. Our study should not serve as a discouragement to the development of these dengue vaccine products, but rather we determine conditions under which dengue vaccination can contribute to the prevention and control of dengue without inducing significant increase in Zika infection.
Most published works focus on the benefits of the control strategies (such as treatments for only one or both diseases) to both diseases involved in the co-infection. For example, Derouich and Boutayeb73 considered a model of two subsequent infections of dengue at separate time intervals with continuous vaccination. They concluded that vaccination can be a control strategy for dengue. However, with consideration of co-infection and the current development of dengue vaccine, our results suggest that additional study on co-infection is urgently and critically needed.
Additional Information
How to cite this article: Tang, B. et al. Implication of vaccination against dengue for Zika outbreak. Sci. Rep. 6, 35623; doi: 10.1038/srep35623 (2016).
References
Kautner, I., Robinson, M. J. & Kuhnle, U. Dengue virus infection: Epidemiology, pathogenesis, clinical presentation, diagnosis, and prevention. J. Pediatr. 131, 516–524 (1997).
Halstead, S. B. Dengue. The Lancet 370, 1644–1652 (2007).
Dick, G. W., Kitchen, S. F. & Haddow, A. J. Zika virus (I). Isolations and serological specificity. Trans. R. Soc. Trop. Med. Hyg. 46, 509–520 (1952).
Johnson, A. J. et al. Genetic and serologic properties of Zika virus associated with an epidemic, Yap State, Micronesia, 2007. Emerg. Infect. Dis. 14, 1232–1239 (2008).
Cao-Lormeau, V. M. et al. Zika virus, French Polynesia, South Pacific, 2013. Emerg. Infect. Dis. 20, 1085–1086 (2014).
Musso, D. & Gubler, D. J. Zika Virus. Clin. Microbiol. Rev. 29(3), 487–524 (2016).
Campos, G. S., Bandeira, A. C. & Sardi, S. I. Zika virus outbreak, Bahia, Brazil. Emerg. Infect. Dis. 21, 1885–1886 (2015).
Zanluca C., Melo, V. C., Mosimann., A. L., Santos, G. I., Santos, C. N. & Luz, K. First report of autochthonous transmission of Zika virus in Brazil. Mem. Inst. Oswaldo. Cruz. 110, 569–572 (2015).
Enfissi, A., Codrington, J., Roosblad, J., Kazanji, M. & Rousset, D. Zika virus genome from the Americas. Lancet 387, 227–228 (2016).
World Health Organization. Zika virus outbreaks in the Americas. Wkly Epidemiol. Rec. 90, 609–616 (2015).
European Center for Disease Prevention and Control. Zika virus disease epidemic: potential association with microcephaly and Guillain- Barré syndrome (first update). European Centre for Disease Prevention and Control, Stockholm, Sweden (2016).
Hennessey, M., Fischer, M. & Staples, J. E. Zika virus spreads to new areas-region of the Americas, May 2015-January 2016. MMWR Morb. Mortal. Wkly Rep. 65, 55–58 (2016).
Gulland, A. Zika virus is a global public health emergency, declares WHO. BMJ 352, i657 (2016).
Priyamvada, L. et al. Human antibody responses after dengue virus infection are highly cross-reactive to Zika virus. Proc. Natl. Acad. Sci. USA 113(28), 7852–7857 (2016).
Dejnirattisai, W. et al. Dengue virus sero-cross-reactivity drives antibody dependent enhancement of infection with zika virus. Nat. Immunol. doi: 10.1038/ni.3515 (2016).
Charles, A. S. & Christofferson, R. C. Utility of a dengue-derived monoclonal antibody to enhance Zika infection in vitro. PLOS Currents Outbreaks doi: 10.1371/currents.outbreaks.4ab8bc87c945eb41cd8a49e127082620 (2016).
Paul, L. M. et al. Dengue virus antibodies enhance Zika virus infection. bioRxiv doi: http://dx.doi.org/10.1101/050112 (2016).
Dupont-Rouzeyrol, M. et al. Co-infection with Zika and Dengue Viruses in 2 Patients, New Caledonia, 2014. Emerg. Infect. Dis. 21(2), 381–382 (2015).
Pessôa, R. et al. Investigation Into an Outbreak of Dengue-like Illness in Pernambuco, Brazil, Revealed a Cocirculation of Zika, Chikungunya, and Dengue Virus Type 1. Medicine 95(12), e3201 (2016).
Vinodkumar, C. S. et al. Episode of coexisting infections with multiple dengue virus serotypes in central Karnataka, India. J. Infect. Public Health 6, 302–306 (2013).
Gulland, A. WHO urges countries in dengue belt to look out for Zika. BMJ 352, i595 (2016).
Andraud, M., Hens, N., Marais, C. & Beutels, P. Dynamic Epidemiological Models for Dengue Transmission: A Systematic Review of Structural Approaches. PLoS ONE 7(11), e49085 (2012).
Kouri, G. et al. Reemergence of dengue in Cuba: a 1997 epidemic in Santiago de Cuba. Emerg. Infect. Dis. 4, 89–92 (1998).
Sierra, B. et al. Secondary heterologous dengue infection risk: Disequilibrium between immune regulation and inflammation? Cell Immunol. 262, 134–140 (2010).
Wichmann, O. et al. Risk factors and clinical features associated with severe dengue infection in adults and children during the 2001 epidemic in Chonburi, Thailand. Trop. Med. Int. Health 9, 1022–1029 (2004).
Nogueira, R. M. et al. Dengue epidemic in the stage of Rio de Janeiro, Brazil, 1990-1: cocirculation of dengue 1 and dengue 2 serotypes. Epidemiol. Infect. 111, 163–170 (1993).
Feng, Z. & Velasco-Hernández, J. X. Competitive exclusion in a vector-host model for the dengue fever. J. Math. Biol. 35, 523–544 (1997).
Esteva, L. & Vargas, C. Coexistence of different serotypes of dengue virus. J. Math. Biol. 46, 31–47 (2003).
Nuraini, N., Soewono, E. & Sidarto, K. A. Mathematical Model of Dengue Disease Transmission with Severe DHF Compartment. Bull. Malays. Math. Sci. Soc. 30, 143–157 (2007).
Sriprom, M., Barbazan, P. & Tang, I. M. Destabilizing effect of the host immune status on the sequential transmission dynamic of the dengue virus infection. Math. Comput. Model. 45, 1053–1066 (2007).
Wearing, H. J. & Rohani, P. Ecological and immunological determinants of dengue epidemics. Proc. Natl. Acad. Sci. USA 103, 11802–11807 (2006).
Hu, K. et al. The effect of antibody-dependent enhancement,cross immunity,and vector population on the dynamics of dengue fever. J. Theor. Biol. 319, 62–74 (2013).
Knerer, G., Currie, C. S. M. & Brailsford, S. C. Impact of combined vector-control and vaccination strategies on transmission dynamics of dengue fever: a model-based analysis. Health Care Manag. Sci. 18, 205–217 (2015).
Billings, L. et al. Instabilities in multiserotype disease models with antibody-dependent enhancement. J. Theor. Biol. 246, 18–27 (2007).
Billings, L., Fiorillo, A. & Schwartz, I. B. Vaccinations in disease models with antibody-dependent enhancement. Math. Biosci. 211, 265–281 (2008).
Bianco, S. & Shaw, L. B. Asymmetry in the presence of migration stabilizes multistrain disease outbreaks. Bull. Math. Biol. 73, 248–260 (2011).
Wikramaratna, P. S., Simmons, C. P., Gupta, S. & Recker, M. The Effects of Tertiary and Quaternary Infections on the Epidemiology of Dengue. PLoS ONE 5, e12347 (2010).
Bianco, S., Shaw, L. B. & Schwartz, I. B. Epidemics with multistrain interactions: The interplay between cross immunity and antibody-dependent enhancement. Chaos 19, 043123–043129 (2009).
Bennett, S. N. et al. Epidemic Dynamics Revealed in Dengue Evolution. Mol. Biol. Evol. 27, 811–818 (2010).
Lourenco, J. & Recker, M. Viral and epidemiological determinants of the invasion dynamics of novel dengue genotypes. PLoS Negl. Trop. Dis. 4, e894 (2010).
Kucharski, A. J. et al. Transmission dynamics of Zika virus in island populations: a modelling analysis of the 2013–14 French Polynesia outbreak. PLoS Negl. Trop. Dis. 10(5), e0004726 (2016).
Gao, D. Z. et al. Prevention and control of Zika fever as a mosquito-borne and sexually transmitted disease. arXiv:1604.04008 (2016).
Funk, S. et al. Comparative analysis of dengue and Zika outbreaks reveals differences by setting and virus. bioRxiv doi: http://dx.doi.org/10.1101/043265 (2016).
Moreno, V., Espinoza, B. & Bichara, D. Role of short-term dispersal on the dynamics of Zika virus. arXiv:1603.00442v3 (2016).
Gao, D. Z., Porco, T. C. & Ruan S. G. Coinfection dynamics of two diseases in a single host population. J. Math. Anal. Appl. 442(1), 171–188 (2016).
Sharomi, O., Podder, C. N., Gumel, A. B. & Song, B. J. Mathematical analysis of the transmission dynamics of HIV/TB coinfection in the presence of treatment. Math. Biosci. Eng. 5(1), 145–174 (2008).
Kapitanov, G. A double age-structured model of the co-infection of tuberculosis and HIV. Math. Biosci. Eng. 12(1), 23–40 (2015).
Pinto, C. M. A. & Carvalho, A. R. M. New findings on the dynamics of HIV and TB coinfection models. Appl. Math. Comput. 242, 36–46 (2014).
Silva, C. J. & Rorres, D. F. M. A TB-HIV/AIDS coinfection model and optimal control treatment. Discrete Contin. Dyn. Syst. 35(9), 4639–4663 (2015).
Bacaër, N. et al. Modeling the joint epidemics of TB and HIV in a South African township. J. Math. Biol. 57, 557–593 (2015).
Martcheva, M. & Pilyugin, S. S. The role of coinfection in multidisease dynamics. SIAM J. Appl. Math. 66, 843–872 (2006).
Moualeu, D. P., Mbang, J., Ndoundam, R. & Bowong, S. Modeling and analysis of HIV and hepatitis C co-infections. J. Biol. Syst. 19(4), 1–41 (2011).
Carvalho, A. R. M. & Pinto, C. M. A. A coinfection model for HIV and HCV. Biosystems 124, 46–60 (2014).
Bhunu, C. P., Garira, W. & Magombedzem, G. Mathematical Analysis of a Two Strain HIV/AIDS Model with Antiretroviral Treatment. Acta Biotheor. 57, 361–381 (2009).
Packer, A., Forde, J., Hews, S. & Kuang, Y. Mathematical models of the interrelated dynamics of hepatitis D and B. Math. Biosci. 247, 38–46 (2014).
Merler, S., Poletti, P., Ajelli, M., Caprile, B. & Manfredi, P. Coinfection can trigger multiple pandemic waves. J. Theor. Biol. 254, 499–507 (2008).
Prosper, O. et al. Modeling control strategies for concurrent epidemics of seasonal and pandemic H1N1 infuenza. Math. Biosci. Eng. 8, 141–170 (2011).
Diekmann, O. & Heesterbeek, J. A. P. Mathematical Epidemiology of Infectious Diseases: Model Building, Analysis and Interpretation. Wiley, Chichester (2000).
Van den Driessche, P. & Watmough, J. Reproduction numbers and subthreshold endemic equilibria for compartmental models of disease transmission. Math. Biosci. 180, 29–48 (2002).
Chowell, G. et al. Estimation of the reproduction number of dengue fever from spatial epidemic data. Math. Biosci. 208, 571–589 (2007).
Massad, E., Burattini, M. N., Coutinho, F. A. & Lopez, L. F. Dengue and the risk of urban yellow fever reintroduction in Sao Paulo State, Brazil. Rev. Saude Publica 37(4), 477–484 (2003).
Nishiura, H. et al. Preliminary estimation of the basic reproduction number of Zika virus infection during Colombia epidemic, 2015-2016. Travel Med. Infect. Dis. 14(3), 274–276 (2016).
Chowell, G. et al. Using Phenomenological Models to Characterize Transmissibility and Forecast Patterns and Final Burden of Zika Epidemics. PLoS Currents Outbreaks doi: 10.1371/currents.outbreaks. f14b2217c902f453d9320a43a35b9583 (2016).
Nishiura, H. et al. Transmission potential of Zika virus infection in the South Pacific. Int. J. Infect. Dis. 45, 95–97 (2016).
Martcheva, M., Pilyugin, S. S. & Holt, R. D. Subthreshold and superthreshold coexistence of pathogen variants: The impact of host age-structure. Math. Biosci. 207, 58–77 (2007).
Rupnow, M. F., Shachter, R. D., Owens, D. K. & Parsonnet, J. A dynamic transmission model for predicting trends in Helicobacter pylori and associated diseases in the United States. Emerg. Infect. Dis. 6(3), 228–237 (2000).
Qesmi, R., ElSaadany, S., Heffernan, J. M. & Wu, J. H. A hepatitis B and C virus model with age since infection that exhibits backward bifurcation. SIAM J. Appl. Math. 71, 1509–1530 (2011).
WHO. http://www.who.int/immunization/research/development/dengue_q_and_a/en/ (accessed 23/08/2016) (2016).
Sanofi. http://hugin.info/152918/R/1975899/723110.PDF (2015).
Kirkpatrick, B. D. et al. The live attenuated dengue vaccine tv003 elicits complete protection against dengue in a human challenge model. Sci. Transl. 8(330), 330ra36 (2016).
Osorio, J. E., Wallace, D. & Stinchcomb D. T. A recombinant, chimeric tetravalent dengue vaccine candidate based on a dengue virus serotype 2 backbone. Expert Rev. Vaccines 15(4), 497–508 (2016).
Halstead, S. B. & Aguiar, M. Dengue vaccines: Are they safe for travelers? Travel Med. Infect. Dis. 14(4), 378–383 (2016).
Derouich, M. & Boutayeb, A. Dengue fever: Mathematical modelling and computer simulation. Appl. Math. Comput. 177, 528–544 (2006).
Acknowledgements
This project was supported by the National Natural Science Foundation of China (NSFC, 11571273, 11631012(YX)), by the Fundamental Research Funds for the Central Universities (08143042 (YX)), by the Canada Research Chair Program, the Natural Sciences and Engineering Research Council of Canada (JW), and the International Development Research Center (Ottawa, Canada, 104519-010).
Author information
Authors and Affiliations
Contributions
B.T., Y.X. and J.W. designed the study and carried out the analysis. B.T. performed numerical simulations. B.T., Y.X. and J.W. contributed to writing the paper.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Tang, B., Xiao, Y. & Wu, J. Implication of vaccination against dengue for Zika outbreak. Sci Rep 6, 35623 (2016). https://doi.org/10.1038/srep35623
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep35623
This article is cited by
-
Mathematical modeling on co-infection: transmission dynamics of Zika virus and Dengue fever
Nonlinear Dynamics (2023)
-
Impact of tetravalent dengue vaccination with screening, ADE, and altered infectivity on single-serotype dengue and Zika transmission
Journal of Mathematical Biology (2023)
-
Game-Theoretical Model of the Voluntary Use of Insect Repellents to Prevent Zika Fever
Dynamic Games and Applications (2022)
-
Modeling and analyzing cross-transmission dynamics of related information co-propagation
Scientific Reports (2021)
-
Coinfection, Altered Vector Infectivity, and Antibody-Dependent Enhancement: The Dengue–Zika Interplay
Bulletin of Mathematical Biology (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.










 for (A) βdz = 0.05, βrz = 0.18, Λ = 10000 and (B) βdz = 0.05, βrz = 0.18, Λ = 1000000. The accumulated number of humans infected with Zika for (C) βdz = 0.18, βrz = 0.18, Λ = 10000 and (D) βdz = 0.18, βrz = 0.05, Λ = 10000.
for (A) βdz = 0.05, βrz = 0.18, Λ = 10000 and (B) βdz = 0.05, βrz = 0.18, Λ = 1000000. The accumulated number of humans infected with Zika for (C) βdz = 0.18, βrz = 0.18, Λ = 10000 and (D) βdz = 0.18, βrz = 0.05, Λ = 10000.