Abstract
The objective of this study is to investigate the association between osteoarthritis (OA) and all-cause mortality in worldwide populations and to develop recommendations according to GRADE evidence levels. Literature search through Nov 2015 was performed using the electronic databases (including MEDLINE, EMBASE, EBSCO and Cochrane library). The prospective cohort trials that investigated the association between the symptomatic OA (SxOA) or radiological OA (ROA) and all-cause mortality were identified. Hazard ratios (HR) of all-cause mortality in patients with RxOA or ROA were pooled respectively. The evidence quality was evaluated using the GRADE system, while the recommendations were taken according to the quality. Nine of the published literature met the eligible criteria. Meta-analysis revealed that there was no significant difference in the association between SxOA and all-cause mortality (HR = 0.91, 95% CI: 0.68–1.23) and between ROA and all-cause mortality (HR = 1.13, 95% CI: 0.95–1.35). The overall GARDE evidence quality was very low, which will lower our confidence in taking recommendations. To summarize, there was no reliable and confident evidence existed currently in respect of the association between OA and all-cause mortality. Due to the very low level of evidence quality currently, high-quality studies are still required.
Similar content being viewed by others
Introduction
Osteoarthritis (OA) is a common disease with rising prevalence, which results in cause of disability among the older people1,2,3. In epidemiology, half of the world’s population aged 65 years or older has OA, which is the most prevalent disorder of articulating joints in humans. It is commonly believed that OA rarely associated with mortality in the elderly and is often considered a physiological condition of ageing4. Thus, all-cause mortality had not been a major area of investigation in OA. However, more attention was paid to the association between OA and risk of all-cause mortality recently5,6.
Although several studies were conducted to validate whether OA is a risk factor for all-cause mortality, there is still in controversy. Nuesch et al.7 reported that all-cause mortality was found among subjects surveyed from the general population with symptomatic hip or knee OA (SxOA). However, Liu and colleagues examined all-cause mortality in persons with SxOA using data from the Genetics ARthrosis and Progression (GARP) study and Osteoarthritis Care Clinic (OCC) study. The result showed that patients with OA are not at higher risk of death than the general population8. Our previous study demonstrated that knee SxOA was associated with an significantly increased risk of all-cause mortality among the people in the rural areas of China and no such association was observed for radiological knee OA (ROA)6.
As mentioned above, whether or not OA is associated with an increased risk of all-cause mortality is still conflicting. Therefore, the objective of the present study is to assess the evidence from relevant studies that examine the relation between OA and risk of all-cause mortality in worldwide populations by meta-analysis approach and to develop recommendations according to GRADE (Grading of Recommendations, Assessment, Development and Evaluation) system9,10.
Material and Methods
Literature search strategy
To assemble all of the potential published studies, Electronic databases including MEDLINE, EMBASE, EBSCO and Cochrane library were searched for all studies published between JAN 1980 and Nov 2015 that investigate the relationship between OA and all-cause mortality in populations. The following MeSH items or free words were taken to balance the search sensitivity and specificity: osteoarthritis, risk, mortality, all-cause mortality and death rates. Gray studies were identified from the reference of included literature through the manual review. Articles published in languages other than English were also excluded.
Inclusive and exclusive criteria
Primary studies were considered eligible for inclusion if they met the following criteria:
-
1
Study design was a prospective cohort study;
-
2
Studies were included if they investigated the association between the RxOA or ROA and risk of all-cause mortality. SxOA was defined if both pain and ROA were present at the joints;
-
3
The outcome was all-cause mortality;
-
4
The hazard ratio (HR) or risk ratio (RR) and its corresponding 95% confidence interval (95% CI) were reported.
No available data, duplicate studies, reviews, rheumatoid arthritis concerned and non-comparable studies were excluded.
Study selection
Two reviewers (D.X. and Q.L.) independently screened the titles and abstracts for the eligibility criteria. Subsequently, the full text of the studies that potentially met the inclusion criteria were read and the literature was reviewed to determine the final inclusion. Any disagreement was resolved by reaching a consensus through discussion.
Date extraction
Two researchers (D.X. and K.Y.X.) independently extracted the data from each included literature by the use of a standard data extraction form. The following items were extracted: title, authors, study design, follow-up duration, sample size, age, country, anatomy location, covariates adjusted and all-cause mortality parameters.
Outcomes
The pooled hazard ratios of all-cause mortality in patients with RxOA or ROA were the outcomes of the present study.
Assessment of methodological quality
The quality assessment of the included studies was independently conducted by two authors (D.X. and Y.K.X). Disagreements were resolved by discussion or consensus. The methodological quality was assessed using the Newcastle-Ottawa form11, which was a valid instrument designed to assess the quality of cohort studies. The Newcastle-Ottawa form assigns a maximum of four points for selection, two points for comparability and three points for exposure or outcome. Newcastle-Ottawa form scores of 7 were considered as high-quality studies and of 5–6 as moderate quality11.
Data analysis
Pooling data was analyzed by STATA 12.0 (Statacorp, college station, Tex). The assessment for statistics heterogeneity was estimated depending on chi-square and I-square test. When the chi-square was p > 0.05, or I-square < 20% indicating low statistical heterogeneity, a fixed effect model was applied. A random effect model was taken when chi-square was p < 0.05 and I-square > 20%. Furthermore, a sensitivity analysis was carried out by removing one study in each turn, the rest of the studies were analyzed to evaluate whether the results were affected statistically significantly. HR and 95% CI were used to measure the association between OA and all-cause mortality for all studies. If included studies reported several multivariable-adjusted HR, we used the most fully adjusted for potential confounders in the present meta-analysis. RR was used as substitute of HR, when some studies did not directly report HR12. A P-value < 0.05 was considered statistically significant. Publication bias was conducted statistically via Begg funnel plots, which measures the degree of funnel plot asymmetry13,14.
GRADE Evidence synthesis
The levels of evidence quality were estimated according to the guidelines of the GRADE working group9. Although the GRADE system acknowledges the primacy of randomized controlled trials, it also recognizes circumstances in which observational studies generate high quality evidence of treatment effects15. A sequential assessment of the evidence quality was applied in GRADE system and a subsequent judgment on the strength of the recommendations is followed by previous evidence quality assessment. The evidence grades are classified into the four categories: (1) high grade: further research is unlikely to change confidence in the effect estimate; (2) moderate grade: further research is likely to alter confidence in the effect estimate and may change the estimate; (3) low grade: further research is likely to significantly alter confidence in the effect estimate and to change the estimate; and (4) very low grade: any effect estimate is uncertain. The lowest evidence quality for any of the outcomes was used to rate the overall evidence quality according to the GRADE working group. The strengths of the recommendations were taken according to the overall evidence quality. GRADEpro Version 3.6 software was used in grading evidence and taking recommendations.
Results
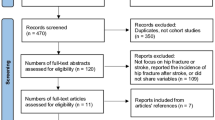
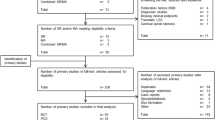
Literature search
A total of 414 titles and abstracts were preliminarily identified with the first search strategy, of which 9 of the published literature6,7,8,16,17,18,19,20,21 ultimately met the eligibility criteria (Fig. 1). One of the included literatures contained two trials based on two patients’ databases respectively. All of the included studies investigated the association between the SxOA/ROA and all-cause mortality.
Study characteristics
The characteristics of the included studies are summarized in Table 1. The individual sample sizes ranged from 181 to 1670 patients with OA. The mean follow-up ranged from 3.9 to 21 years. Six studies were performed to investigate the relationship between the SxOA and all-cause mortality, while other five studies between the ROA and all-cause mortality. All of the included studies had defined the inclusion and exclusion criteria. Only two included studies included both SxOA and ROA patients. There were 3 studies performed in the USA and 1 each in China, Netherlands, England, Italy, Japan and Finland. Two studies recruited patients with knee OA, 2 with hand OA, 1 each with hip OA and hip/knee OA and others with hand, knee, hip, or spine OA. Only one study recruited female patients, while others included both male and female. Only one study conducted two trials in male and female patients respectively.
Quality assessment and publication bias
Using the Newcastle-Ottawa form, all but three studies were identified as high quality. The results of quality assessment were presented in Table 2. The publication bias was estimated for overall populations by HR of all-cause mortality. No significant publication bias was demonstrated for overall populations by Begg rank correlation method (P = 0.65).
Meta-analysis
In seven studies providing all-cause mortality in RxOA patients, the pooled HR was 0.91 (95% CI: 0.68–1.23). There was no significant difference in HR of all-cause mortality between the SxOA and control groups (Fig. 2). Six trials reported the all-cause mortality in ROA patients. There was no statistically significant difference between the ROA patients and control groups (HR = 1.13, 95% CI: 0.95–1.35) (Fig. 3).
GRADE Evidence synthesis and recommendation strengths
The above two important outcomes in the present meta-analysis were evaluated using the GRADE system. The level of evidence quality for each outcome was very low (Table 3). Therefore, the level of overall evidence quality was very low eventually. This finding may lower the confidence in any recommendations.
Discussion
All-cause mortality is a major area of research in OA. However, there has been no consensus regarding whether OA is an independent risk factor for mortality. Furthermore, there have been no recommendations for all-cause mortality in OA patients based on the current evidence. There is a need for an evidence base to help patients or clinician understand the relationship between OA and all-cause mortality and make their clinical decisions. To the best of our knowledge, the present study is the first meta-analysis that uses the GRADE system to evaluate the quality of the evidence investigating the association between OA and risk of all-cause mortality.
To date, nine articles including 10 prospective studies have examined the association between OA and risk of all-cause mortality. Five of them only reported the association between SxOA and mortality, while three between ROA and mortality. Two studies reported the relationship between SxOA/ROA and mortality. In the present study, we conducted meta-analysis according to SxOA and ROA patients respectively. Random effects model was used to conduct statistical analysis because of significant heterogeneity among studies. Thus, more weight was placed on the studies with more sample size. Random effect analysis can lower the risk of bias and get the pooled data conservatively. Although the results showed that SxOA and ROA were not significantly associated with increased risk of mortality, the overall evidence quality was very low. The GRADE evidence quality of pooled results will lower our confidence in clinical decision. The studies were carried out in various durations of follow up, different geographical locations and with different OA inclusion criteria. The pooled estimate of primary outcomes was consistent across sensitivity analyses and without significant publication bias.
Four included studies6,7,16,19 reported the association between SxOA or ROA in the lower limbs and mortality. Because of limited number of included studies involved lower limbs, we cannot conduct subgroup meta-analysis. Although pooled results were not performed in lower limbs, the individual study reported the significant association between the OA in lower limbs and increased risk of mortality, especially in knee SxOA. Lower limbs OA will lower the levels of physical activity, which will influence the survival rate. Therefore, participating in recommended levels of physical activity is associated with reduced risk of mortality22. Because of lower evidence quality, we did not have confidence in recommendation currently.
Danielsson et al.23 reported that death rates were higher than expected in persons with ROA of the knees but not of the hips. However, Cerhan et al.24 showed that the presence of OA of the hands and bilateral knees was associated with reduced survival, while the presence of OA of the hips and feet was not. The reason might be that reduced survival is attributed to either lower levels of physical activity or the use of medications in patients with OA24. In Haara et al. study20, women with SxOA involving distal interphalangeal joints had an increased mortality, but neither men nor women with ROA of thumb carpometacarpal joint had an increased risk of mortality. Some studies reported that lower levels of physical activity due to disability among the patients with lower limb OA and the use of non-steroidal anti-inflamatory drugs (NSAIDs) explained the increased risk of mortality from heart disease6,25. Kerr et al.26 found that was using NSAIDs associated with an increased risk of mortality from gastrointestinal. In a longitudinal study27, the adjusted hazard ratio of celecoxib, diclofenac, meloxicam, rofecoxib and non-selective NSAIDs were 1.39, 1.44, 1.49, 1.58 and 1.76 respectively. Thus, Kerr et al.27 reported that there was a significant increased mortality risk for those exposed to either COX-2-selective or non-selective NSAIDs.
Our previous study6 reported that knee SxOA was associated with an increased risk of all-cause mortality among the residents in the rural areas of China. The reason may be that SxOA patients are likely to suffer from physical disability. Lack of walking disability is one of the risk factors for death from cardiovascular diseases. Furthermore, SxOA patients are commonly take NSAIDs to relieve their joint symptoms, which will increase the risk of morality.
Some degree of clinical heterogeneity was induced by the different anatomical location, medical co-morbidities, ethnicity, genetic background, nutritional status of patients, follow-up duration and diagnosis criteria for OA. Heterogeneity, to some extent, may have also been caused by study design. One of the major heterogeneity was the several anatomical location of OA during patient recruitment. We cannot perform subgroup analysis according to anatomical location due to two studies in knee, one in hip and others in knee, hip, hand or spine. Because of limited information got from original studies, heterogeneity cannot be completely resolved.
Although the above kinds of heterogeneity may palace an influence on the pooled results of meta-analysis, the evidence quality was summarized according to the current evidence. Because of clinical heterogeneity and limited information, we, therefore, drew the conclusion that the GRADE evidence quality was very low. The present evidence quality meant that reliable and confident evidence did not exist currently in respect of the association between OA and all-cause mortality. Moreover, the very low GRADE evidence quality need further high-quality studies to be complemented.
The methodological quality assessment for original studies identified a number of limitations to the current evidence base. (1) The diagnosis of osteoarthritis in some studies20,21 was recorded by a general practitioner and was not validated based on published classification criteria. (2) Some individuals with asymptomatic osteoarthritis would be misclassified into the control group, which will lead to a bias21. (3) The various duration of follow-up would place a bias on the current results. (4) Clinical heterogeneity may be caused by the preexisting conditions of the patients, various diagnosis for OA, the experience level of the evaluators, severity of OA, medical commodities, smoking and the economic level. The above confounding factors might have an impact on the present outcomes. (5) Meta-analyses of observational studies are subject to bias and provide inappropriate estimates for effects size when compared to interventional studies such as RCT. While the results of this meta-analysis should be considered appropriate, these limitations should be considered when interpreting the findings.
In the GRADE system of rating the quality of evidence, each observational study began as low quality evidence but was rated up by three categories of items. Firstly, the included studies did not yield large or very large estimates of the magnitude of an exposure effect, we may not be confident about the results. Secondly, there was no evidence that the influence of all plausible confounding would reduce a demonstrated effect or suggest a spurious effect. Thirdly, an exposure-response gradient was not present, accordingly upgrade the quality of evidence was not for this outcome. We consider that the above factors could significantly influence the stability of the outcomes. The above factors of GRADE evidence quality did not account for the upgraded evidence quality. Therefore, the overall GRADE evidence quality was very low. It indicates that the there is no exact evidence involving the association between OA and all-cause mortality. High-quality clinical trials are required to verify the above area of OA. To some extent, the present study is meaningful for taking clinical recommendation.
According to the very low GRADE evidence quality, the present meta-analysis of cohort studies showed that reliable and confident evidence do not exist currently in respect of the association between OA and all-cause mortality. The increasing prevalence of OA worldwide calls for further high-quality studies to investigate the effects of OA on mortality.
Additional Information
How to cite this article: Xing, D. et al. Osteoarthritis and all-cause mortality in worldwide populations: grading the evidence from a meta-analysis Sci. Rep. 6, 24393; doi: 10.1038/srep24393 (2016).
References
Sacks, J. J., Luo, Y. H. & Helmick, C. G. Prevalence of specific types of arthritis and other rheumatic conditions in the ambulatory health care system in the United States, 2001–2005. Arthritis Care Res (Hoboken) 62, 460–464 (2010).
Lawrence, R. C. et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 58, 26–35 (2008).
Helmick, C. G. et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part I. Arthritis Rheum. 58, 15–25 (2008).
Hootman, J. M., Helmick, C. G. & Brady, T. J. A public health approach to addressing arthritis in older adults: the most common cause of disability. Am J Public Health 102, 426–433 (2012).
Kluzek, S. et al. Painful knee but not hand osteoarthritis is an independent predictor of mortality over 23 years follow-up of a population-based cohort of middle-aged women. Ann. Rheum. Dis. doi: 10.1136/annrheumdis-2015-208056 (2015).
Liu, Q. et al. Knee osteoarthritis and all-cause mortality: the Wuchuan Osteoarthritis Study. Osteoarthr. Cartil. 23, 1154–1157 (2015).
Nuesch, E., Dieppe, P., Reichenbach, S., Williams, S., Iff, S. & Juni, P. All cause and disease specific mortality in patients with knee or hip osteoarthritis: population based cohort study. BMJ 342, d1165 (2011).
Liu, R. et al. Mortality in osteoarthritis patients. Scand. J. Rheumatol. 44, 70–73 (2015).
Atkins, D. et al. Grading quality of evidence and strength of recommendations. BMJ 328, 1490 (2004).
Atkins, D. et al. Systems for grading the quality of evidence and the strength of recommendations I: critical appraisal of existing approaches The GRADE Working Group. BMC Health Serv Res 4, 38 (2004).
Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 25, 603–605 (2010).
Spruance, S. L., Reid, J. E., Grace, M. & Samore, M. Hazard ratio in clinical trials. Antimicrob. Agents Chemother. 48, 2787–2792 (2004).
Song, F. & Gilbody, S. Bias in meta-analysis detected by a simple, graphical test. Increase in studies of publication bias coincided with increasing use of meta-analysis. BMJ 316, 471 (1998).
Begg, C. B. & Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 50, 1088–1101 (1994).
Kunz, R. Randomized trials and observational studies: still mostly similar results, still crucial differences. J Clin Epidemiol 61, 207–208 (2008).
Barbour, K. E. et al. Hip Osteoarthritis and the Risk of All-Cause and Disease-Specific Mortality in Older Women: A Population-Based Cohort Study. Arthritis & rheumatology 67, 1798–1805 (2015).
Haugen, I. K. et al. Hand osteoarthritis in relation to mortality and incidence of cardiovascular disease: data from the Framingham heart study. Ann. Rheum. Dis. 74, 74–81 (2015).
Cacciatore, F. et al. Long-term mortality in frail elderly subjects with osteoarthritis. Rheumatology (Oxford) 53, 293–299 (2014).
Tsuboi, M., Hasegawa, Y., Matsuyama, Y., Suzuki, S., Suzuki, K. & Imagama, S. Do musculoskeletal degenerative diseases affect mortality and cause of death after 10 years in Japan. J. Bone Miner. Metab. 29, 217–223 (2011).
Haara, M. M. et al. Osteoarthritis of finger joints in Finns aged 30 or over: prevalence, determinants and association with mortality. Ann. Rheum. Dis. 62, 151–158 (2003).
Holbrook, T. L., Wingard, D. L. & Barrett-Connor, E. Self-reported arthritis among men and women in an adult community. J Community Health 15, 195–208 (1990).
Leitzmann, M. F. et al. Physical activity recommendations and decreased risk of mortality. Arch. Intern. Med. 167, 2453–2460 (2007).
Danielsson, L. & Hernborg, J. Morbidity and mortality of osteoarthritis of the knee (gonarthrosis) in Malmo, Sweden. Clin. Orthop. Relat. Res . 69, 224–226 (1970).
Cerhan, J. R., Wallace, R. B., el-Khoury, G. Y., Moore, T. E. & Long, C. R. Decreased survival with increasing prevalence of full-body, radiographically defined osteoarthritis in women. Am. J. Epidemiol. 141, 225–234 (1995).
Kumar, N. et al. Causes of death in patients with rheumatoid arthritis: comparison with siblings and matched osteoarthritis controls. J. Rheumatol. 34, 1695–1698 (2007).
Kerr, S. J., Rowett, D. S., Sayer, G. P., Whicker, S. D., Saltman, D. C. & Mant, A. All-cause mortality of elderly Australian veterans using COX-2 selective or non-selective NSAIDs: a longitudinal study. Br J Clin Pharmacol 71, 936–942 (2011).
Kerr, S. J., Rowett, D. S., Sayer, G. P., Whicker, S. D., Saltman, D. C. & Mant, A. All-cause mortality of elderly Australian veterans using COX-2 selective or non-selective NSAIDs: a longitudinal study. Br J Clin Pharmacol 71, 936–942 (2011).
Acknowledgements
This work was supported by funding from National Natural Science Foundation of China (no. 81501919).
Author information
Authors and Affiliations
Contributions
D.X. and Y.X. conducted literature search and determined studies for exclusion and inclusion. D.X., Q.L., Z.C.L. and Y.K. extracted data from the included studies, performed the meta-analysis and drafted the manuscript. J.H.L., D.X. and B.W. conceived the idea of the study, designed the study and critically revised the manuscript for important intellectual content. All authors reviewed the paper and approved the final manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Xing, D., Xu, Y., Liu, Q. et al. Osteoarthritis and all-cause mortality in worldwide populations: grading the evidence from a meta-analysis. Sci Rep 6, 24393 (2016). https://doi.org/10.1038/srep24393
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep24393
This article is cited by
-
Health-related quality of life in children with developmental coordination disorder: a systematic review
Health and Quality of Life Outcomes (2023)
-
Association between knee osteoarthritis and the risk of cardiovascular disease and the synergistic adverse effects of lack of exercise
Scientific Reports (2023)
-
Environmental and occupational exposure to cadmium associated with male reproductive health risk: a systematic review and meta-analysis based on epidemiological evidence
Environmental Geochemistry and Health (2023)
-
Comorbidity phenotypes and risk of mortality in patients with osteoarthritis in the UK: a latent class analysis
Arthritis Research & Therapy (2022)
-
Cost Effectiveness of Pharmacological Management for Osteoarthritis: A Systematic Review
Applied Health Economics and Health Policy (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.