Abstract
Quantitatively determining physiological parameters at a microscopic level in the retina furthers the understanding of the molecular pathways of blinding diseases, such as diabetic retinopathy and glaucoma. An essential parameter, which has yet to be quantified noninvasively, is the retinal oxygen metabolic rate (rMRO2). Quantifying rMRO2 is challenging because two parameters, the blood flow rate and hemoglobin oxygen saturation (sO2), must be measured together. We combined photoacoustic ophthalmoscopy (PAOM) with spectral domain-optical coherence tomography (SD-OCT) to tackle this challenge, in which PAOM measured the sO2 and SD-OCT mapped the blood flow rate. We tested the integrated system on normal wild-type rats, in which the measured rMRO2 was 297.86 ± 70.23 nl/minute. This quantitative method may shed new light on both fundamental research and clinical care in ophthalmology in the future.
Similar content being viewed by others
Introduction
The demand for treating blindness and low vision continue to escalate as human longevity increases worldwide. By 20041, for example, blindness and low vision had affected more than three million Americans aged 40 years and older; by 20102, 285 million people globally were affected. More than 80% of such visual impairments were caused by eye diseases1, which include glaucoma, diabetic retinopathy (DR), age-related macular degeneration (AMD) and cataracts1,2. Alterations in oxygen metabolism are believed to be involved in most of these diseases3,4. For instance, hypoxia in the glaucomatous retina can damage the optic nerve head, partially due to insufficient vascular perfusion5. In DR, the loss of pericytes is often associated with poorly regulated blood flow6, which can further lead to retinal vascular occlusion and retinal hypoxia7. In AMD, abnormalities in retinal perfusion have also been reported8. Perturbations in retinal oxygenation can prompt, for example, degeneration of retinal neurons, loss of photoreceptors and onset of neovascularization, eventually causing visual impairment. Therefore, the precise measurement of retinal oxygen metabolic rate (rMRO2) can be critical in investigating these blinding diseases.
Non-invasive rMRO2 quantification has been proposed for decades9,10 without being successfully demonstrated. Obtaining rMRO2 measurements is challenging because it requires measuring retinal blood flow and oxygen saturation (sO2) together. Advances in Doppler spectral domain optical coherence tomography (SD-OCT) makes it possible to precisely detect retinal blood flow11. The main obstacle is accurately measuring retinal sO2. To measure retinal sO2, researchers have used oxygen-sensitive electrodes and magnetic resonance imaging12,13,14,15, but these efforts are usually restricted to terminal experiments and/or limited by low spatial resolution.
To resolve retinal sO2 noninvasively and with a high spatial resolution, researchers have mainly focused on multi-spectral fundus photography based oximetry16. Owing to the distinct light absorption spectrum between oxygenated and deoxygenated hemoglobins16,17, multi-wavelength fundus photography can assess the sO2 in retinal vessels. Specifically, optical density of a retinal blood vessel, which is the logarithm of the ratio between detected backscattered light intensities from the vessel and its adjacent retinal tissues16, is obtained at several selected illumination wavelengths. Hickham etal. first applied two-wavelengths fundus photography to map retinal sO218, yet two-wavelength fundus photography is sensitive to light scattering and is easily affected by retinal local parameters such as vessel size, melanin concentration in retinal pigment epithelium16. To improve the stability and accuracy in sO2 measurement, researchers employed additional wavelengths in fundus photography in later studies to compensate for the effect of optical scattering, as well as the vessel size19,20,21,22. In addition, researchers chose wavelengths 548 nm and 610 nm to correct the influence of melanin based on the approximate linearly decreased extinction coefficient of melanin within this wavelength range23. Building on such modifications, the performance of retinal oximetry was much improved. However, adding more wavelengths cannot completely eliminate the influence from optical scattering and variations of retinal local parameters16. Our recent numerical simulation study demonstrated that the absolute measured sO2 error could be up to be 20% when the vessel size is as large as 160 µm or the melanin concentration in the retinal pigment epithelium is as high as 8 mmol/L24.
Optical coherence tomography (OCT) has the potential to measure retinal sO2 measurement25,26 noninvasively. We recently explored the feasibility of using visible-light OCT (Vis-OCT) to quantify retinal sO2in vivo27; yet there is still a long way before OCT can be verified to precisely measure sO2 at various anatomical sites. The capability of photoacoustic (PA) imaging to quantify sO2, however, has been well-studied and well-documented in various anatomical sites, including the ears28, esophagus, colon29 and brain30.
Building on the proven strength of PA imaging31, we developed photoacoustic ophthalmoscopy (PAOM) to address the aforementioned need in retinal metabolic imaging using rats as an animal model. We further optimized a multi-wavelength methodology in PAOM to quantify retinal sO2.
Results
Imaging schematic for both sO2 and flow quantification
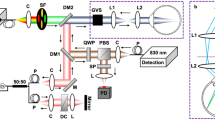
We accessed rMRO2 by integrating PAOM with Doppler SD-OCT. Figure 1a illustrates the combined functional imaging system (see Online Methods for more details.). The aligned and collimated probing beams for both PAOM and SD-OCT were scanned by the same optics on the retina for imaging. We employed a circular scanning pattern centered at the optic disc to image all the retinal vessels within single B-scans as shown in Figure 1b. The molar extinction coefficients of oxy-hemoglobin (HbO2) and deoxy-hemoglobin (HbR) can be found in Figure 1c, based on which sO2 can be measured by multi-wavelength PAOM. The accuracy of PAOM was validated by measuring a series of ex vivo bovine blood (Quad Five Inc, Ryegate, MO) phantom samples with different preset sO2 levels (see Supplementary Figure S1 and Supplementary Table S1 for more details). A typical anatomical fundus image acquired by PAOM is shown in Figure 1d (see Supplementary Figure S2 for 3D visualization). In Figure 1d, the white circle and arc were scanning trajectories, from where PA signals were extracted for sO2 measurement. To obtain retinal blood flow, we employed dual-beam scanning in SD-OCT. Corresponding SD-OCT fundus image is shown in Figure 1e; where the two white circles highlight the scanning trajectories used to measure Doppler angle and phase.
Illustration of integrated PAOM and SD-OCT to measure rMRO2.
(a) Schematic of the experimental setup. (b) Circular scanning pattern on the retina. (c) Molar extinction coefficient spectrum of oxy- and deoxy-hemoglobin. (d) A maximum-amplitude-projection PAOM fundus image showing 12 major retinal vessels. The circle (radius: 0.45 mm) and the concentric arc (radius: 0.56 mm) are scanning trajectories from which PAOM B-scan images were acquired for assessing sO2. Bar: 200 µm. (e) An OCT fundus image of the same rat showed in the panel d. The circles (radii of 0.45 and 0.56 mm) highlight the scanning trajectories for measuring Doppler angle and blood flow. Bar: 200 µm.
Quantification of retinal sO2 by muti-wavelength PAOM
The steps to measure sO2 using multi-wavelength PAOM are illustrated in Figure 2. We scanned along the highlighted circular trajectory around the optic disk at three wavelengths (570, 578 and 588 nm). Scanning around the optic disk enabled us to measure the complete hemodynamic properties of the eye from a fast one-dimensional scan. The B-scan images along the circular trajectory at the three-wavelengths are shown in the top part of Figure 2a. Fluctuations of the vessels' position along the vertical direction reflect the distances from the vessels to the ultrasonic detection. The PA amplitudes of the 12 major vessels were extracted and are shown below their corresponding B-scan images. We then used the multi-wavelength PA amplitudes of the vessels to estimate sO2 in every vessel based on the molecular extinction coefficients of HbO2 and HbR at corresponding optical wavelengths (Figure 1c). The steps to extract vessel PA amplitude from B-scan images are detailed in Supplementary Figure S3. After inverse calculation, the sO2 values of all the highlighted vessels scanned along the circular trajectory are given in Figure 2b and Figure 2c. On average, our results show the sO2 values in arterial and venous blood to be 93.0 ± 3.5% and 77.3 ± 9.1%, respectively. Shonat et al. pioneered the measuring of retinal oxygen partial pressure (PO2) based on phosphorescence quenching techniques in cats32. They reported that the cat's venous PO2 was 30 Torr, which corresponded to a 42% sO2 based on the oxygen-hemoglobin dissociation curve in cat33. Their measurements were consistent with other reported results in cats33. Different animal models are shown to have different retinal oxygenations34,35; the rodent's venous sO2 was reported to be around 70%36,37, which agrees with our PAOM measurements.
Steps to quantify retinal sO2 using multi-wavelength PAOM.
(a) Cross-sectional retina image acquired at 578 nm, 580 nm and 588 nm illuminating wavelengths. Top: raw PAOM B-scan images in pseudo-colors. In the 588-nm image, the yellow arrow highlights retinal blood vessels and the white arrow highlights choroidal vessels. Bottom: PA amplitudes of the 12 vessels. (b) pseudo-colored vessels as imaged in the circular PAOM B-scan based on their measured sO2 values; (c) comparison of sO2 values in all major vessels. (d) Measured sO2 in selected vessels from different radii as shown in Figure 1b, where spatial consistency is demonstrated.
Spatial consistency in sO2 measurements along the same vessels is essential, but it was not successfully demonstrated in existing retinal oximetry due to influences from retinal vessel diameter and retinal pigmentation variation16,24. We tested our spatial consistency by comparing sO2 measurements from four selected vessels scanned at different positions from the optic disk, as highlighted in Figure 1d. The radii of the two circles were 0.45 mm and 0.56 mm, a separation that is small enough where sO2 values at the two locations should be the same in each vessel. Results shown in Figure 2d confirm such consistencies, with the largest absolute variation found to be 3.9%.
Quantification of retinal flow by Doppler SD-OCT
Figure 3 shows the steps to quantify retinal blood flow velocity and vessel diameter using Doppler SD-OCT38,39. Because Doppler SD-OCT can only access the projected blood flow velocity along the probing beam, the Doppler angle (defined as the angle between the vessel and the probing beam) is required to estimate the absolute velocity. We adopted the dual-ring scanning method38,39 used by several groups to determine the Doppler angle (see Supplementary Figure S4). The two circular trajectories overlapping with those in PAOM are highlighted in the OCT fundus image (Figure 1e). The OCT B-scan amplitude and phase images (before bulk motion correction) from the inner scanning trajectory are shown in Figure 3a and Figure 3b, respectively. We obtained the blood flow velocity in each vessel based on the calculated OCT phase variations and their corresponding Doppler angles.
Steps to measure retinal blood flow using SD-OCT.
(a) OCT B-scan amplitude image acquired from the inner circle as shown in Figure 1c. (b) OCT B-scan phase image from the inner circle. (c) Blood velocity distribution within the vessel highlighted by the black arrow in panel b. Top: two-dimensional distribution along the vessel cross-section; Bottom: experimental and fitted transverse velocity profiles along the horizontal position highlighted by the dashed line. (d) Average blood flow velocity in all the major retinal vessels. The positive velocity of arterial blood shows flow coming from the optic disk to peripheral areas; the negative velocity of venous blood indicates flow coming from peripheral areas to the optic disk. (e) Calculated vessel diameters of all the major retinal vessels. (f) Comparison of the measured total arterial and venous blood flows.
Figure 3c shows a magnified view of the imaged blood flow velocity distribution in a typical vessel (highlighted by the arrow in Figure 3b). The laminar flow profile along the vessel's horizontal centerline clearly shows a quadratic dependence on radii within the vessel. Figure 3d provides the overall measurements of blood flow velocities in this particular retina, from which we can observe higher velocities in arteries than veins. We also extracted the vessel diameter from SD-OCT phase images using a recently developed automatic segmentation algorithm40, with results given in Figure 3e. The vessel diameters are shown in Figure 3e, where the veins have larger diameters than the arteries. By multiplying blood velocity with vessel cross-sessional size, we can calculate total retinal blood flow as 7.43 ± 0.51 µl/minute and 7.38 ± 0.78 µl/minute within the venous and arterial systems, respectively (Figure 3f). The results are consistent with previously reported results41 and the venous and arterial blood flows match each other well.
Quantification of rMRO2
With sO2 and blood flow acquired, the rMRO2 can be, therefore, calculated. For the particular retina whose sO2 and flow we present in Figure 2 and Figure 3, the measured rMRO2 of the complete inner retina is 373.41 ± 88.04 ng/minute, or 297.86 ± 70.23 nl/minute. This is lower than the 499 nl/minute measured by Shahidi et al42. As they pointed out, their rMRO2 result was higher than other reported values42, which was suggested to be caused by measurement variations in some important parameters, such as the retinal mass. In their results, the venous sO2 was around 50% (after converting the oxygen partial pressure into sO2 value based on the dissociation curve), which was lower than the reported normal rodent venous sO2 value of around 70%36. Also, their measured total retinal blood flow in the inner retina was 10.06 µl/min, which was higher than other reported values43. We think that different anesthesia conditions may also contributed to the discrepancy between our and Shahidi's measurements.
Discussion
Compared with other reported retinal functional imaging modalities, our integrated PAOM and Doppler SD-OCT approach to measure rMRO2 is advantageous in several aspects. First, our method completely interrogates rMRO2 noninvasively. Most of the currently reported retinal functional imaging methods13,16,39,41 can measure only one functional parameter, either retinal sO2 or blood flow, which is insufficient for rMRO2 quantification; other proposed imaging modalities that can quantify rMRO2 are invasive42, which is not suitable for in vivo applications. Secondly, PAOM is expected to assess retinal sO2 much more accurately than the multi-wavelength fundus photography24.
Our simulation studies suggested that such an improvement originates from the better quantification of blood optical absorption by PAOM than the multi-wavelength fundus photography24. Fundus photography estimates light absorption within blood from the collected retinal light reflectance16. Several factors deteriorated the accuracy of the indirect light absorption measurement. First, the acquired reflected light from the vessel is a superposition of photons, which may have no interaction, partial, or full interaction (travelled through the entire vessel) with the retinal blood. Among these photons, only fully interacted photons can provide accurate measurement of the optical absorption by blood24. Secondly, photons backscattered from the vessel's neighboring areas interact more (scattering/absorption) with the melanin in the retinal pigment epithelium (RPE) layer than photons reflected from vessels, because high absorption or scattering by blood allows only a few photons to enter into the RPE. Additional details on how scattering affects fundus photography measurements can be found in our previous Monte Carlo simulation studies24.
For multispectral PAOM, the imaging contrast is based on optical absorption from blood or RPE melanin within the visible light spectral range31. The absorbed photons can be either ballistic or scattered photons. In the current study, the time-resolved light induced acoustic signals can provide axial resolution of up to 23 µm, which enables us to separate the signals of retinal blood vascular from the RPE melanin given the retina thickness is around 200 µm44. As a result, PAOM signals generated from major vessels can be considered to be mainly generated from hemoglobin. Optical scattering, however, does affect the resolution of PAOM. It's reported that the lateral resolution can be degraded by 14% in turbid media compared with the case of no scattering when the imaging depth is close to the transport mean free path45. In PAOM, the theoretical lateral resolution is estimated to be 20 µm. Considering a 14% degradation, the lateral resolution will be reduced to 22.8 µm. Since the degradation in lateral resolution is merely 10% of the theoretical lateral resolution, it may not influence our experimental results much. In addition, the rat eye is notable for its stronger chromatic aberration46,47, we analyzed the chromatic aberration effects on the PAOM image within a bandwidth as short as 18 nm and it turned out the chromatic effects on imaging is small and should not affected the accuracy of PAOM results (see Supplemental Figure S5 for more details.)
Although versatile and unique, the combined PAOM and SD-OCT imaging system has the following limitations. One major concern comes from ultrasonic signal detection. First, ultrasonic signal detection requires physical contact, as in the experiment, where we coupled a needle ultrasonic transducer to the rodent eyelid with ultrasonic gel48. This ultrasonic signal detection scheme is not preferred in clinical settings. Second, the large size and opacity of the needle ultrasonic piezoelectric detector requires a long working distance, which forces a small NA for OCT and thus limits its imaging quality48. To overcome this, we recently developed a transparent micro-ring resonator for ultrasonic signals detection, which has a physical dimension of a few millimeters and a much lower noise equivalent pressure49. We plan to fabricate this micro-ring resonator onto a contact lens serving as the ultrasonic detector, which requires no ultrasonic gel coupling and allows for a flexible working distance. Thirdly, visual stimulus is reported to increase the retinal vessel diameter and blood flow, as well as affect the retinal sO2 through the process of retinal neurovascular coupling43,50. These may affect the accuracy of the PAOM. It has been demonstrated that the neurovascular coupling depends on visual stimulus frequency and stimulus duration51, where the examined flickering frequency, within our understanding, ranged from 10 to 60 Hz with a typical stimulation time last more than 10 s. Such a condition does not exist in PAOM, where we used 25-kHz A-line rate and 2.5 s total illumination time at each illuminating wavelength. Whether each PAOM illumination will introduce effective neurovascular coupling and lead to an observable hemodynamic response within each acquisition needs further investigation in the future. Lastly, despite the good match between measured sO2 by PAOM and the preset sO2 in blood phantom experiments (Supplemental Figure S1), we also understand that the phantom experimental conditions are different from those in in vivo rodent experiments. For example, there are eye movements during imaging, aberration from the eyeball, etc. Whether such differences will affect the sO2 quantification or not also require more future validation.
Another concern is that the performance of dual-ring scanning SD-OCT may be influenced by eye movement due to the consecutive and non-simultaneous scanning sequence of the small and big ring. In our present study, we averaged the vessels' central positions across eight pairs of small-big scanning patterns to prevent motion-induced variation. A motion-insensitive alternative is to scan a pair of small and big rings simultaneously38, which, further complicates the imaging system. Also, we measured the vessel diameter axially because OCT offers higher axial resolution than lateral resolution and we calculated the vessel cross-sectional area using the axial diameter by assuming a cylindrical vessel profile as other researchers did52.
Dysfunctions in the oxygen metabolic rate (MRO2) are not merely limited to the retina, as MRO2 also has been found to be involved in other diseases, such as cancer53, Alzheimer's disease54 and heart failure55. Owing to its capability to accurately assess MRO2, our multimodal imaging technology can help better understand a wider spectrum of disease mechanisms beyond blinding diseases.
Methods
Experimental setup
A schematic of the experimental setup is shown in Figure 1a. We used a tunable dye laser (Cobra, Sirah Laser and Plasmatchnik GmbH) pumped by a pulsed Nd:YLF laser (IS8II-E, Edge-Wave GmbH; pulse duration: 5 ns) as the illumination source for PAOM. The tunable laser output was collimated into 2 mm in diameter, then merged with the light of SD-OCT (center wavelength: 840 nm; bandwidth: 50 nm; SLED IPSDD0804, InPhenix). A two-dimensional galvanometer scanned the combined light beams (QS-7, Nutfield Technology) and relayed them to the eye through a telescopic lenses system. In PAOM, acoustic waves induced by light absorption were detected by an unfocused small-footprint ultrasonic transducer (central frequency: 40-MHz; bandwidth: 30-MHz; active element size: 0.5 × 0.5 mm2) attached to the rat's eyelid through ultrasonic gel. The detected photoacoustic signals were amplified by two amplifiers (ZFL-500LN+, Mini-circuits and 5073PR, Olympus, total gain: 60 dB) and digitalized by a data acquisition card (CS14200, Gage Applied Technology) at a sampling rate of 200 MS/s. In SD-OCT, backscattered light from the retina first interfered with the reference arm light, then sampled by a home-made spectrometer at an A-line rate of 25-kHz. The lateral resolutions of both PAOM and SD-OCT were around 20 µm in the retina with a slight difference caused by the different spectral ranges. The axial resolutions of PAOM and OCT were 23 µm and 5.6 µm, respectively56.
During imaging, a 256 × 256 A-lines scanning pattern was employed to acquire fundus images in both SD-OCT and PAOM. The circular B-scanning (each B-scan contains 4096 A-lines, A-line rate 25-kHz) was used for flow and sO2 measurement. In Doppler OCT, we performed eight pairs of big-small circular scans. We confirmed that 25-kHz A-line rate is able to precisely assess retinal blood flow by comparing the measurement at 25-kHz with results acquired by a 70-kHz A-line rate OCT, which is considered sufficiently high to acquire the entire pulsatile flow profile57.(see Supplementary Figure S6 for more details). In PAOM, the illuminating laser energy was 40 nJ/pulse, which is considered eye-safe as detailed in Supplementary Materials. For sO2 detection, at each wavelength, we scanned 16 consecutive circles centered on optical disc with 4096 A-lines in each circle. The time-resolved photoacoustic signals were collected in each A-line. After data collection, we first reconstructed the 16 B-scan images at each wavelength and then sequentially estimated the sO2 from the 1st B-scan to the 16th B-scan. Finally, all the sO2 measurements for each vessel were averaged across the 16 B-scan results.
Animal Preparation
We used wild-type rats (Sprague Dawley, 300 g, Harlan Laboratories, Indianapolis, IN) in our studies. During experiments, a mixture of isoflurane and normal air was supplied to the rats through a commercial non-rebreathing ventilating system (Vaporizer Inc, Rockmart, GA). We first placed the rat into an induction chamber and adjusted the vaporizer to 2% isoflurane vapor output percentage, setting the attached gas flowmeter at 3 L/min. The vaporizer and flowmeter setting corresponded to 12 mL/hour anesthetic agent gas consumption and were maintained for 10 minutes; then changed to 1.5% isoflurane and 2 L/min air flow for additional five minutes, corresponding to 6.6 mL/hour anesthetic agent gas consumption. At this point, the rat was under deep anesthesia. We then placed the rat on a homemade adjustable holder for imaging. The homemade holder was connected to the ventilation system, which kept the rat ventilated at the rate corresponding to 6.6 mL/hour isoflurane gas consumption. We dilated the rats' pupils with a 1% Tropicamide ophthalmic solution and paralyzed the iris sphincter muscle with a 0.5% Tetracaine hydrochloride ophthalmic solution. Meanwhile, artificial teardrops (Systane, Alcon Laboratories, Inc.) were applied every other minute to prevent corneal dehydration. During the experiment, the rats' electrocardiogram was monitored (ETH-256 Amplifier, Iworx). Their blood oxygen saturation levels were measured to be around 90% and the heart rate was measured to be around 223 bpm (Pulse oximetry, Model 8500AV, Nonin Medical, Inc).
All experimental procedures were in compliance with ARVO Statement for the Use of Animals in Ophthalmic and Vision Research and laboratory animal protocol approved by the Institutional Animal Care and Use Committee at Northwestern University.
sO2 quantification
We selected three wavelengths (570, 578 and 588 nm) for sO2 imaging in PAOM. The sO2 value of each vessel was estimated as follows:

where [HbR] and [HbO2] are the concentrations of oxy- and deoxy-hemoglobin [g/L]. [HbR] and [HbO2] were quantified through optical absorption by retinal blood. The blood absorption coefficient can be expressed as

where  and
and  are the known molar extinction coefficients [cm−1M−1] of HbR and HbO2 at wavelength λi [nm], respectively. In PAOM, the detected PA amplitude pa(x, y, z, λi) is considered to be proportional to the local optical energy deposition ϕ(x, y, z, λi), which is a product of local μa(x, y, z, λi) and local optical fluence F(x, y, z, λi). Thus, Eq. 2 can be rewritten as:
are the known molar extinction coefficients [cm−1M−1] of HbR and HbO2 at wavelength λi [nm], respectively. In PAOM, the detected PA amplitude pa(x, y, z, λi) is considered to be proportional to the local optical energy deposition ϕ(x, y, z, λi), which is a product of local μa(x, y, z, λi) and local optical fluence F(x, y, z, λi). Thus, Eq. 2 can be rewritten as:

where K1 is the proportionality coefficient. By assuming consistent optical illumination and ignoring optical attenuation in the retina, we can consider F(x, y, z, λi) to be constant and simplify K1·F(x, y, z, λi) as K2. For multiple wavelength PA measurements, Eq. 3 becomes

where  ,
,  and
and  . Although [HbR] and [HbO2] can only be estimated as relative values, the final sO2 in Eq. 1 is an absolute value58.
. Although [HbR] and [HbO2] can only be estimated as relative values, the final sO2 in Eq. 1 is an absolute value58.
In order to minimize the influence of the spatial sensitivity distribution of the unfocused transducer, the PA signals of each vessel at the 578 nm and 588 nm optical illuminations were normalized by the PA amplitude of the same vessel acquired at the isosbestic wavelength of 570 nm.
Vessel diameter and cross section area measurements
We measured the vessel diameter axially in the OCT B-scan amplitude image, because of the high axial resolution of OCT. If we denote the vessel diameter in the B-scan as Dia [m], the actual vessel diameter Dia_r [m] is

where θ [radians] is the Doppler angle. The vessel cross-sectional area A [m2] is calculated by

Blood velocity and flow rate
In Doppler OCT, the probing light passes through the pupil lens and is focused onto retinal vessels. The blood velocity v [m/s] can be calculated as

where fsample [kHz] is the SD-OCT A-line rate; λ0 [nm] is the center wavelength of the SD-OCT light source; ΔΦ is the phase shift [degree] between adjacent OCT A-lines after bulk motion correction59; n [dimensionless] is the refractive index of the sample (n = 1.4); and θ [radians] is the Doppler angle (estimation of the Doppler angle can be found in Supplementary Figure S4). To reduce the influence of eye motion on Doppler angle estimation, we averaged the estimated vessel depth across eight consecutive OCT B-scans. In our current work, the largest error in vessel depth is 2.9 μm across eight B-scans. Considering the scanning radii difference between the outer- and inner-scanning rings is 110 μm, the largest 2.9 μm depth error results in an angle estimation error of 1.5 degrees. Since the mean value of the measured Doppler angle is around 82 degrees, the influence of the 1.5-degree angle error is small.
We observed the phase-wrap in retinal flow measurement. Phase-wrap can be corrected once we know the axial blood flow direction, which can be obtained from the phase value close to the vessel border since flow velocity near vessel wall is small enough to prevent phase-wrapping60. With the known blood flow direction and assuming the actual phase Δφ< 0, we have

after phase wrapping correction. If the actual phase is Δϕ> 0, we have

after phase wrapping correction. After the blood velocity and vessel size are obtained, the blood flow in the ith vessel is

where vi is the average velocity and Ai is the vessel cross-sectional area.
Retinal metabolic rate of oxygen (rMRO2)
The rMRO2 [g/min] is quantified as

where WO2 and WHbO2 are the molecular weights of O2 and oxyhemoglobin, which are 32 and 68000 [g/mol], respectively; [HbT] is the total concentration of hemoglobin in the rat, which is 150 [g/L] in current studies; sO2ai and sO2vi are sO2 values in the ith artery and vein, respectively; dai and dvi are the vessel diameter of ith artery and vein, respectively; vai and vvi are the blood flow velocity within the ith artery and vein, respectively; M and N are the number of arteries and veins, respectively. The standard deviation of rMRO2 [g/min] (rMRO2_std) is derived through the principle of error propagation as follows.

where std(·) denotes the standard deviation operator and sqrt(·) denotes the square root operator. The unit of rMRO2 in Eq. 11 and Eq. 12 is ng/min and we can convert ng/min to L/min by

where V is the volume of gas; ng is the number of moles of gas; R is 8.3145 [J·mole−1·K−1]; T is the blood temperature (311.15 K); and P is the standard atmospheric pressure (101,325 Pa). All measured data, including vessel size, sO2 and flow velocity, are given in Supplemental Table S2.
References
Congdon, N. et al. Causes and prevalence of visual impairment among adults in the United States. Arch. Ophthalmol. 122, 477–485 (2004).
Pascolini, D. & Mariotti, S. P. Global estimates of visual impairment: 2010. Br. J. Ophthalmol. 96, 614–618 (2012).
Yu, D. Y. & Cringle, S. J. Oxygen distribution and consumption within the retina in vascularised and avascular retinas and in animal models of retinal disease. Prog. Retin. Eye Res. 20, 175–208 (2001).
Yu, D. Y. & Cringle, S. J. Retinal degeneration and local oxygen metabolism. Exp. Eye Res. 80, 745–751 (2005).
Tezel, G. & Wax, M. B. Hypoxia-inducible factor 1α in the glaucomatous retina and optic nerve head. Arch. Ophthalmol. 122, 1348–1356 (2004).
Kohner, E. M., Patel, V. & Rassam, S. M. Role of blood flow and impaired autoregulation in the pathogenesis of diabetic retinopathy. Diabetes 44, 603–607 (1995).
Antonetti, D. A., Klein, R. & Gardner, T. W. Diabetic retinopathy. N. Engl. J. Med. 366, 1227–1239 (2012).
Ciulla, T. A. et al. Color Doppler imaging discloses reduced ocular blood flow velocities in nonexudative age-related macular degeneration. Am. J. Ophthalmol. 128, 75–80 (1999).
Riva, C. E., Grunwald, J. E. & Sinclair, S. H. Laser Doppler Velocimetry study of the effect of pure oxygen breathing on retinal blood flow. Invest. Ophthalmol. Vis. Sci. 24, 47–51 (1983).
Hickam, J. B., Sieker, H. O. & Frayser, R. Studies of retinal circulation and A-V oxygen difference in man. Trans. Am. Clin. Climatol. Assoc. 77, 34–44 (1960).
An, L. & Wang, R. K. In vivo volumetric imaging of vascular perfusion within human retina and choroids with optical micro-angiography. Opt. Express 16, 11438–11452 (2008).
Wangsa-Wirawan, N. D. & Linsenmeier, R. A. Retinal oxygen: fundamental and clinical aspects. Arch. Ophthalmol. 121, 547–557 (2003).
Berkowitz, B. A. & Wilson, C. A. Quantitative mapping of ocular oxygenation using magnetic resonance imaging. Magn. Reson. Med. 33, 579–581 (1995).
De La Garza, B. H., Muir, E. R., Li, G., Shih, Y. Y. & Duong, T. Q. Blood oxygenation level-dependent (BOLD) functional MRI of visual stimulation in the rat retina at 11.7 T. NMR Biomed. 24, 188–193 (2011).
Duong, T. Q. Magnetic resonance imaging of the retina: A brief historical and future perspective. Saudi J Ophthalmol. 25, 137–143 (2011).
Harris, A., Dinn, R. B., Kagemann, L. & Rechtman, E. A review of methods for human retinal oximetry. Ophthalmic. Surg. Lasers Imaging 34, 152–164 (2003).
Prahl, S. Optical absorption of Hemoglobin. <http://omlc.org/spectra/hemoglobin/>, (1999) Date of access: 04/05/2013.
Hickam, J. B., Frayser, R. & Ross, J. C. A study of retinal venous blood oxygen saturation in human subjects by photographic means. Circulation 27, 375–386 (1963).
Delori, F. C. Noninvasive technique for oximetry of blood in retinal vessels. Appl. Opt. 27, 1113–1125 (1988).
Vucea, V., Bernard, P. J., Sauvageau, P. & Diaconu, V. Blood oxygenation measurements by multichannel reflectometry on the venous and arterial structures of the retina. Appl. Opt. 50, 5185–5191 (2011).
Hardarson, S. H. et al. Automatic retinal oximetry. Invest. Ophthalmol. Vis. Sci. 47, 5011–5016 (2006).
Traustason, S. et al. Spectrophotometric retinal oximetry in pigs. Invest. Ophthalmol. Vis. Sci. 54, 2746–2751 (2013).
Hammer, M., Vilser, W., Riemer, T. & Schweitzer, D. Retinal vessel oximetry-calibration, compensation for vessel diameter and fundus pigmentation and reproducibility. J. Biomed. Opt. 13, 054015 (2008).
Liu, W., Jiao, S. & Zhang, H. F. Accuracy of retinal oximetry: a Monte Carlo investigation. J. Biomed. Opt. 18, 066003 (2013).
Yi, J. & Li, X. Estimation of oxygen saturation from erythrocytes by high-resolution spectroscopic optical coherence tomography. Opt. Lett. 35, 2094–2096 (2010).
Faber, D. J., Mik, E. G., Aalders, M. C. & van Leeuwen, T. G. Toward assessment of blood oxygen saturation by spectroscopic optical coherence tomography. Opt. Lett. 30, 1015–1017 (2005).
Yi, J., Wei, Q., Liu, W., Backman, V. & Zhang, H. F. Visible-light optical coherence tomography for retinal oximetry. Opt. Lett. 38, 1796–1798 (2013).
Yao, J., Maslov, K. I., Zhang, Y., Xia, Y. & Wang, L. V. Label-free oxygen-metabolic photoacoustic microscopy in vivo. J. Biomed. Opt. 16, 076003 (2011).
Yang, J. M. et al. Simultaneous functional photoacoustic and ultrasonic endoscopy of internal organs in vivo. Nat. Med. 18, 1297–1302 (2012).
Hu, S., Maslov, K., Tsytsarev, V. & Wang, L. V. Functional transcranial brain imaging by optical-resolution photoacoustic microscopy. J. Biomed. Opt. 14, 040503 (2009).
Zhang, H. F., Maslov, K., Stoica, G. & Wang, L. V. Functional photoacoustic microscopy for high-resolution and noninvasive in vivo imaging. Nat. Biotechnol. 24, 848–851 (2006).
Shonat, R. D., Wilson, D. F., Riva, C. E. & Pawlowski, M. Oxygen distribution in the retinal and choroidal vessels of the cat as measured by a new phosphorescence imaging method. Appl. Opt. 31, 3711–3718 (1992).
Herbert, D. A. & Mitchell, R. A. Blood gas tensions and acid-base balance in awake cats. J. Appl. Physiol. 30, 434–436 (1971).
Lau, J. C. & Linsenmeier, R. A. Oxygen consumption and distribution in the Long-Evans rat retina. Exp. Eye Res. 102, 50–58 (2012).
Linsenmeier, R. A. & Braun, R. D. Oxygen distribution and consumption in the cat retina during normoxia and hypoxemia. J. Gen. Physiol. 99, 177–197 (1992).
Wilson, D. F. et al. Oxygen distribution and vascular injury in the mouse eye measured by phosphorescence-lifetime imaging. Appl. Opt. 44, 5239–5248 (2005).
Gray, L. H. & Steadman, J. M. Determination of the oxyhaemoglobin dissociation curves for mouse and rat blood. J. Physiol 175, 161–171 (1964).
Dai, C., Liu, X., Zhang, H. F., Puliafito, C. A. & Jiao, S. Absolute retinal blood flow measurement with a dual-beam Doppler optical coherence tomography. Invest. Ophthalmol. Vis. Sci. 54, 7998–8003 (2013).
Wehbe, H. et al. Automatic retinal blood flow calculation using spectral domain optical coherence tomography. Opt. Express 15, 15193–15206 (2007).
Liu, W., Liu, T., Song, W., Yi, J. & Zhang, H. F. Automatic retinal vessel segmentation based on active contours method in Doppler spectral-domain optical coherence tomography. J. Biomed. Opt. 18, 16002 (2013).
Choi, W. et al. Measurement of pulsatile total blood flow in the human and rat retina with ultrahigh speed spectral/Fourier domain OCT. Biomed. Opt. Express 3, 1047–1061 (2012).
Wanek, J., Teng, P. Y., Albers, J., Blair, N. P. & Shahidi, M. Inner retinal metabolic rate of oxygen by oxygen tension and blood flow imaging in rat. Biomed. Opt. Express 2, 2562–2568 (2011).
Radhakrishnan, H. & Srinivasan, V. J. Multiparametric optical coherence tomography imaging of the inner retinal hemodynamic response to visual stimulation. J. Biomed. Opt. 18, 86010 (2013).
Hammer, M., Leistritz, S., Leistritz, L. & Schweitzer, D. Light paths in retinal vessel oximetry. Biomedical Engineering, IEEE Transactions on. 48, 592–598 (2001).
Liu, Y., Zhang, C. & Wang, L. V. Effects of light scattering on optical-resolution photoacoustic microscopy. J. Biomed. Opt. 17, 126014 (2012).
Remtulla, S. & Hallett, P. E. A schematic eye for the mouse and comparisons with the rat. Vision Res 25, 21–31 (1985).
Harmening, W. M., Tiruveedhula, P., Roorda, A. & Sincich, L. C. Measurement and correction of transverse chromatic offsets for multi-wavelength retinal microscopy in the living eye. Biomed. Opt. Express 3, 2066–2077 (2012).
Song, W. et al. Multimodal photoacoustic ophthalmoscopy in mouse. J. Biophotonics 6, 505–512 (2013).
Li, H., Dong, B. Q., Zhang, Z., Zhang, H. F., & Sun, C. A transparent broadband ultrasonic detector based on an optical micro-ring resonator for photoacoustic microscopy. Sci. Rep. 4, 4496; 10.1038/srep04496 (2014).
Hammer, M. et al. Retinal venous oxygen saturation increases by flicker light stimulation. Invest. Ophthalmol. Vis. Sci. 52, 274–277 (2011).
Polak, K., Schmetterer, L. & Riva, C. E. Influence of flicker frequency on flicker-induced changes of retinal vessel diameter. Invest. Ophthalmol. Vis. Sci. 43, 2721–2726 (2002).
Leitgeb, R. A., Werkmeister, R. M., Blatter, C. & Schmetterer, L. Doppler Optical Coherence Tomography. Prog. Retin. Eye Res. 41c, 26–43 (2014).
Harris, A. L. Hypoxia--a key regulatory factor in tumour growth. Nat. Rev.Cancer 2, 38–47 (2002).
Minoshima, S. et al. Metabolic reduction in the posterior cingulate cortex in very early Alzheimer's disease. Ann. Neurol. 42, 85–94 (1997).
Poehlman, E. T., Scheffers, J., Gottlieb, S. S., Fisher, M. L. & Vaitekevicius, P. Increased resting metabolic rate in patients with congestive heart failure. Ann. Intern. Med. 121, 860–862 (1994).
Song, W. et al. Integrating photoacoustic ophthalmoscopy with scanning laser ophthalmoscopy, optical coherence tomography and fluorescein angiography for a multimodal retinal imaging platform. J. Biomed. Opt. 17, 061206 (2012).
Radhakrishnan, H. & Srinivasan, V. J. Multiparametric optical coherence tomography imaging of the inner retinal hemodynamic response to visual stimulation. J. Biomed. Opt. 18, 86010 (2013).
Zhang, H. F., Maslov, K., Sivaramakrishnan, M., Stoica, G., & Wang, L. V. Imaging of hemoglobin oxygen saturation variations in single vessels in vivo using photoacoustic microscopy. Appl. Phys. Lett. 90, 053901 (2007).
Makita, S., Hong, Y., Yamanari, M., Yatagai, T. & Yasuno, Y. Optical coherence angiography. Opt. Express 14, 7821–7840 (2006).
Singh, A. S., Kolbitsch, C., Schmoll, T. & Leitgeb, R. A. Stable absolute flow estimation with Doppler OCT based on virtual circumpapillary scans. Biomed. Opt. Express 1, 1047–1058 (2010).
Acknowledgements
This work is supported in part by the NIH grants 1R01EY019951 and 1R24EY022883. It is also supported in part by the NSF grants CBET-1055379, DBI-1353952 and CBET-1066776. W. Song was partially supported by the China Scholarship Council. W. Liu is supported by the Howard Hughes Medical Institute International Student Research Fellowship.
Author information
Authors and Affiliations
Contributions
H.F.Z. and S.L.J. initiated the project. H.F.Z. supervised the project. W.S., Q.W., W.Z.L. and T.L. performed the experiments and analyzed the results. W.S., Q.W., W.Z.L., T.L., J.Y., N.S., A.A.F., R.A.L., S.L.J. and H.F.Z. discussed the results and contributed to the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Supplementary Information
Supplementary information
Supplementary Information
Supplemental Figure S2
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Song, W., Wei, Q., Liu, W. et al. A combined method to quantify the retinal metabolic rate of oxygen using photoacoustic ophthalmoscopy and optical coherence tomography. Sci Rep 4, 6525 (2014). https://doi.org/10.1038/srep06525
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep06525
This article is cited by
-
Functional photoacoustic imaging: from nano- and micro- to macro-scale
Nano Convergence (2023)
-
In-vivo functional and structural retinal imaging using multiwavelength photoacoustic remote sensing microscopy
Scientific Reports (2022)
-
Functional and structural ophthalmic imaging using noncontact multimodal photoacoustic remote sensing microscopy and optical coherence tomography
Scientific Reports (2021)
-
Pumpless, modular, microphysiological systems enabling tunable perfusion for long-term cultivation of endothelialized lumens
Biomedical Microdevices (2021)
-
Measurement of blood-oxygen saturation using a photoacoustic technique in the rabbit hypoxemia model
Journal of Clinical Monitoring and Computing (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.