Key Points
-
Suggests the phenomenon of root resorption is not well understood, especially in general practice, and as a result many lesions are diagnosed and treated incorrectly.
-
Highlights that previous articles in this field are either not systematic or lack current evidence-based background.
-
Presents a simple classification and systematic discussion that will not only help GDPs manage these defects effectively, but also provide students, specialist trainees, teachers and specialists with a concise account.
Abstract
Root resorption is a poorly understood phenomenon and is often misdiagnosed and, as a result, inappropriately treated. The aim of this paper is to provide a practical guide for diagnosis of root resorption lesions using a simple classification, and to describe the principles of management of these resorptive defects in everyday practice.
Similar content being viewed by others
Introduction
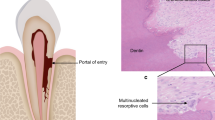
Root resorption is the non-bacterial destruction of the mineralised cementum or dentine due to the interaction of clastic cells and dental hard and soft tissues.1,2,3
In the adult dentition root resorption is caused by osteoclast-like multi or occasionally mononucleated cells called odontoclasts. Roots are usually protected against external and internal root resorption by unmineralised organic cementoid and predentin, respectively, and therefore do not undergo resorption in normal circumstances.2,4 This is due to the inability of the clastic cells to adhere to unmineralised surfaces.2,4
Resorption of permanent teeth is pathologic in nature and therefore undesirable.5 However, in the primary dentition it is desirable as this physiologic root resorption aids exfoliation of the deciduous tooth and thus facilitates eruption of the permanent successor.
Root resorption occurs in three stages; initiation, resorption and repair.6 The process of resorption may be self-limiting and go undetected clinically. Once initiated, if the initial surface resorptive process is sustained, for example by infection and/or pressure, dental hard tissue destruction will continue and tooth tissue loss may occur. This may result in the tooth becoming unsalvageable.
Detailed accounts of the pathogenesis of the dental resorptive lesions have not been discussed here as they would be beyond the scope of this paper.7
There are many different classifications of the dental resorptive lesions based on histology, aetiology or origin in the literature.1,2,3,8,9 Root resorption is a poorly understood phenomenon, it is often misdiagnosed and is inappropriately treated.
The aim of this paper is firstly, to provide a practical guide for diagnosis of root resorption lesions using a simple classification (Fig. 1), and secondly to describe the principles of management of these resorptive defects in everyday practice (Table 1).
Internal root resorption:
Internal inflammatory resorption (IIR)
This type of resorption may occur as a result of damage to the predentine either by trauma due to physical or chemical irritation or by bacterial infection in chronic pulpal inflammation. In active progressive IIR lesions, the root canal coronal to the resorptive lesion will typically be necrotic, while apically the pulp is vital providing nutrients to the odontoclasts allowing the resorptive lesion to progress. However, if the tooth loses vitality, resorption will cease to progress.1,5,8
Clinical signs and symptoms are normally diagnosed in advanced lesions. Teeth with IIR are usually asymptomatic but because these teeth are partially vital during resorptive lesion expansion, they may exhibit signs of reversible or irreversible pulpitis. In advanced cases, that is, with infected necrotic root canal systems, there may be symptoms and/or signs of periapical periodontitis (for example, discolouration, sinus, tenderness to palpation and/or percussion).
Diagnosis is usually made radiographically. Historically, the radiographic appearance of these lesions has been described as a radiolucent symmetrical round or oval ballooning out of the root canal wall. However, in reality the radiographic appearance of these lesions may deviate from the above descriptions and in many cases, does not follow these rigid portrayals commonly described in review papers (Fig. 2).7,10 Although parallax technique may be used to confirm the position and nature of the lesion, IIR may still be misdiagnosed as external cervical resorption in multi-rooted teeth as the root canal of an unaffected tooth may be superimposed over the affected root, thus giving the appearance of external cervical resorption.10
(a) A periapical radiograph of mandibular right and left central incisors with radiographic signs of IIR (red arrows); note the ballooning out of the root canal and relatively symmetrical nature of the defect. The margins are well-defined. (b) The sagittal CBCT slice through the mandibular right central incisor reveals the intact canal walls (yellow arrows) and the true dimension of the defect and root canal (red dashed line) that cannot be appreciated on the periapical radiograph. (c, d) Axial and (e) coronal CBCT slices through the same teeth reveal that the defects are in fact asymmetrical in nature (red arrows). (f) The root canals have been obturated using thermoplasticised gutta percha and temporised for bleaching (courtesy of Dr Alan Knight, King's College London)
Where management of IIR is being considered, a small field of view, high resolution cone beam computed tomography (CBCT) is recommended to appreciate the exact nature, location and extent of the IIR and the presence of a perforation.8,11 These factors may have an impact on the restorability and/or the management of the case.
Due to the granulomatous nature of the lesion, profuse bleeding from the root canal is frequently observed upon accessing the canal system. This will cease as soon as the pulp and granulation tissue have been completely removed. Due to the complex nature of the resorptive defect, energised irrigation and inter-appointment medication have been recommended.11,12
Due to the irregular nature of IIR and the root canal space, it is desirable to obturate the root canal with a thermoplasticised root filling to ensure optimum adaptation and compaction. In cases where IIR has perforated the root it may be necessary to seal the affected portion of root canal space with a bioactive root filling material, for example MTA or Biodentine.11
Internal replacement resorption (IRR)
This type of resorption is relatively uncommon with an unknown aetiology. However, it is usually associated with a history of dental trauma, caries or periodontal infections affecting the pulp as the main contributing factors.7,8
Histological appearance of IRR defects reveals the presence of metaplastic hard tissue replacing the resorbed dentine at the periphery of the defect, which is suggestive of active and simultaneous resorption and replacement. This metaplastic hard tissue resembles cementum or osteoid-like tissues. However, detailed pathogenesis is not fully understood.8 It has been suggested that IRR is an attempt of IIR to replace the damaged (resorbed) dentine.7
Clinical signs and symptoms of IRR are indistinguishable from IIR, and is usually diagnosed in advanced lesions. Teeth may be asymptomatic, however, as the active lesions are partially vital during the resorption phase, they may exhibit signs of reversible or irreversible pulpitis. In infected necrotic cases, signs and symptoms of apical periodontitis (for example, discolouration, sinus, tenderness to palpation and/or percussion) may be observed.
Diagnosis is made radiographically. The resorptive defect and the adjacent root wall usually have a cloudy and/or mottled appearance due to the radiopaque inclusions of hard tissue. The outline of the canal appears distorted and expanded. The true nature, position and extent of the defect can only be accurately detected with a CBCT (Fig. 3).
(a, b) Periapical radiographs of a maxillary left central incisor with radiographic signs of IRR; note the symmetrical nature of the defect, which remains centred with the parallax view, and the radioopaque nature of its coronal aspect (c) CBCT slices through the same tooth reveals a calcified tissue in the coronal part of the lesion. (d, e) Obturated tooth and a 2-year review radiograph demonstrating the irregular borders of the defect that have been obturated with thermoplastiicised gutta percha. Reproduced from Patel S, Ricucci D, Durak C, Tay F. Internal root resorption: a review. J Endod 2010; 36: 1107–1121, Elsevier
The management of IRR is similar to IIR and involves root canal treatment with energised irrigation and obturation with thermoplasticised gutta-percha. Endodontic ultrasonic tips may be required in order to navigate through the osteoid-like hard tissue. In restorable but perforated lesions, a subsequent surgical approach may also be required.11
External root resorption
External inflammatory resorption (EIR)
EIR occurs in teeth with infected necrotic root canals as a result of caries and microleakage and is a common finding in almost all teeth with periapical periodontitis.1,5,7,9 These resorptive lesions are frequently observed following severe traumatic dental injuries (for example, avulsion and luxation injuries). In these cases, the initial external resorption is triggered by injury to the root surface and the associated periodontium. However, the progression of the lesion is largely dictated by pulpal vitality.1,2,7,9 Consequently, if the affected tooth does not lose its blood supply, the osteoclastic activity will only focus on the repair of the damaged outer root surface and the resorption will be self-limiting, similar to what is seen in transient apical breakdown (which will be discussed in more detail later in the paper). However, if the root canal space becomes infected, bacterial toxins may advance via dentinal tubules to the resorption area, resulting in the progression of EIR.
Clinical signs and symptoms will be similar to those of periapical periodontitis, for example, the tooth will be non-responsive to sensibility testing and tender to percussion and/or palpation.
The roots may appear shorter than normally expected and/or have ragged root ends, and will have apical radiolucencies adjacent to the root-end. EIR associated with dental trauma will usually appear as radiolucent crater shaped indentations on the root surface with adjacent periradicular radiolucencies. The root canal outline will be visible indicating the resorption lesion is external to the root canal. Due to the two-dimensional nature of conventional radiographs EIR will only be detected if it is located on the proximal aspects of the root; resorptive defects on, or extending to the buccal/palatal aspect of the root will not be detected (Fig. 4).
(a) A periapical radiograph of a maxillary left central incisor tooth showing a well-circumscribed and round periapical radiolucency. The tooth has been root treated with what appears to be gutta-percha. However, the root filling lacks adequate length, width and density. During non-surgical root canal retreatment, the working length could not be reliably established with the electronic apex locator. (b) Sagittal CBCT reconstructed image through the same tooth revealed substantial loss of buccal root structure from the coronal third to the apex (yellow arrow). In addition, there was significant periapical and buccal cortical bone loss. This loss of root structure could lead to major complications as a result of a hypochlorite accident if the defect had not been detected. (c) The extracted tooth and associated defect
In some instances, a CBCT examination of the tooth may be indicated to confirm the nature of the resorptive lesion, that is, the true extent and dimension of the lesion, the number of sites affected along the root and whether there is a root wall perforation. This information is essential when considering endodontic treatment of these cases (Fig. 5).
(a, b, c) A series of periapical radiographs revealing a classic saucer-shaped excavation on the distal aspect of the maxillary left central incisor associated with EIR (red arrow) and the ballooning out of the root canal and a symmetrical defect in the maxillary left lateral incisor affected by IIR (yellow arrows). (d, e, f) Sagittal CBCT slices of the same teeth reveal the extent of EIR and the degree of external root wall destruction on the central incisor (red arrows). CBCT slices also reveal the destruction caused by IIR on the lateral incisor (yellow arrow). (g, h, i) Axial and (j, k, l) coronal slices reveal and confirm the true nature of the EIR (red arrows) and IIR (yellow arrows) and confirm the diagnosis
Root canal treatment is indicated in restorable teeth and will arrest the resorptive process and therefore prevent further damage.
External replacement resorption (ERR)
These types of resorptive lesions appear as a result of severe luxation and avulsion injuries.5,13,14 Depending on the nature of the injury, the periodontal ligament may tear, become crushed and/or degenerate due to desiccation resulting in the periodontal ligament cells undergoing necrosis and, together with cementum and dentine, become resorbed via osteoclastic action and replaced with alveolar bone laid down by osteoblasts as part of the repair process. The osteoblastic activity may then gradually replace the entire radicular dentine with bone in the process of remodelling.1,5,15 ERR may be self-limiting and/or localised.
It has been reported that when ERR covers more than 20% of root surface the tooth will lose its physiologic mobility which may result in a high-pitched metallic sound to percussion.5,16
The tooth may appear infra-occluded in developing dentition. As ERR is external in nature, the tooth should respond to sensibility testing albeit with delay if there is tertiary dentine formation. However, lack of response to sensibility testing in the absence of other clinical signs and symptoms of endodontic infection, is not an indication for endodontic treatment.
Conventional radiographic examination will reveal the lack of periodontal ligament space only in proximal areas as the affected root surface in the buccal and labial aspects cannot be assessed using conventional radiographs. A CBCT may be indicated to confirm the extent of labial and palatal ERR lesion, and therefore the prognosis of the tooth, especially in cases where follow up radiographs are showing a gradual increase in the size of ERR (Fig. 6).
(a) A periapical radiograph of the maxillary central incisors with late presentation following severe luxation injury and complicated crown root fracture of the maxillary left central incisor. Note periapical radiolucency and blunting of the root-ends (yellow arrows). (b) A 5-year review radiograph following root canal treatment of both teeth reveals direct bone replacement of the root dentine on the maxillary left central incisor (red brackets). Note the left central incisor has been decoronated and restored with a temporary resin bonded bridge. Note the periapical radiolucency on both teeth have healed. (c,d,e) Sagittal, axial and coronal CBCT slices through the same tooth confirm an almost complete bony replacement of root dentine associated with ERR (green arrows)
There is no effective management for ERR apart from periodic reviewing of these cases. The affected teeth may survive for years, or even decades before they become decoronated following total replacement of the root with bone.
In children and adolescents, the identification and management of ERR before or during the growth spurt is of paramount importance. Teeth that undergo ERR fail to erupt, preventing further development of the adjacent alveolar bone. This will lead to the affected tooth becoming infra-occluded.17,18,19 The underdeveloped alveolar ridge associated with the ankylosed tooth in these circumstances may have a negative impact on aesthetics, phonetics and function and will complicate any future restorative treatment.17,18,19 Therefore, to preserve the alveolar ridge height and promote its normal development, the ankylosed tooth may be electively decoronated to below the amelocemental junction and the root covered with attached mucosa to ensure alveolar bone maintenance and, in favourable cases, formation above the decoronated root and subsequent ridge preservation until the patient is old-enough for the definitive restorative plan.17,18,19
External cervical resorption (ECR)
These resorptive defects manifest mainly in the cervical region of the tooth and develop as a result of damage to, and/or deficiency of the subepithelial cementum.20 The aetiology of ECR is not known, however, several potential predisposing factors have been suggested.20 A three-stage mechanism; initiation, resorption (destructive) and repair, has been proposed for the development and progression of ECR.6 Osteoclastic cells from the adjacent periodontium are thought to invade the exposed root surface, via gaps in the cementum, and form a fibrovascular lesion (resorption phase), which may ultimately become calcified and develop into a fibro-osseous tissue (reparative phase).21,22,23 A small portion of these lesions may arrest. However, most cervical resorption lesions are not self-limiting and usually exhibit a prolonged resorption phase.1,9
Hithersay22 suggested that ECR lesions are aseptic and only become secondarily invaded with bacteria. However, Tronstad1 stated that ECR lesions were stimulated and sustained by microorganisms in the dentinal tubules and gingival sulcus and therefore were inflammatory in nature. A molecular study on the expression of bacteria-induced toll-like receptors in ECR lesions appears to support a bacterial aetiology.24
The aetiology of ECR remains unclear.5,20,25 However, several aetiological factors have been reported to contribute towards the initiation of ECR. These include trauma,2,20,25 orthodontic treatment,20,25 periodontal treatment,2,25 dentoalveolar surgery,25 intracoronal bleaching,25,26 playing wind instruments,27 bisphosphonate therapy,28 Varicella Zoster virus infection29 and idiopathic causes.20,30,31In addition, the possibility of a familial pattern and possible genetic predisposition to ECR has been reported.32 Furthermore, a possible relationship between ECR in humans and feline odontoclastic resorptive lesions in cats has also been suggested.33
However, there has been no strong evidence to show a 'cause and effect' with these suggested aetiological factors. These reported aetiological factors may be associated, rather than predisposing factors. ECR have also been observed in unerupted teeth suggesting that ECR may, in some cases be idiopathic in nature.7,34,35,36,37
ECR lesions can be challenging to diagnose, as individuals with ECR are usually asymptomatic in the early stages, therefore pulpal and/or periodontal involvement may only appear at the later stage of disease progression.3,20,38 In addition, ECR may be misdiagnosed as caries.
A pink spot in the cervical aspect of the tooth is reported as a pathognomic clinical sign, however, in reality a pink spot is a relatively rare finding.1,21,22,39
ECR is typically detected clinically when the tip of a dental probe, or a periodontal scaler, engages the defect and catches the resorptive lesion's edges. ECR defects will feel hard and scratchy when probed and should be differentiated from subgingival caries, which will give a tactile feedback of being sticky on probing. In addition, ECR lesions often bleed profusely when probed due to their vascularity.3 However, not all ECR lesions can be probed and investigated in the above manner, especially if they are in the early stages of progression and/or positioned in inaccessible areas of the tooth or the mouth, which will be completely missed. As a result, radiological examination is of utmost importance in the diagnosis of ECR.3,5,22,23
In early cases, ECR may be asymptomatic and just detected as a chance radiographic finding, however, in more advanced cases when there is pulpal involvement there may be symptoms of (ir) reversible pulpitis and/or apical periodontitis.
There is no 'classic' radiographic appearance; lesion may have well-defined, or irregular margins in the cervical aspect of the tooth (Fig. 7).3 While early lesions are radiolucent due to resorption of hard dental tissue, advanced (fibro-osseous) ECR lesions may exhibit a mottled appearance reflecting the attempted repair of the resorbed root structure.3,21 The outline of the root canal will be visible through the lesion thus indicating that the lesion is 'external' to the root canal. This is a pathognomonic sign of ECR.
(a and b) Parallax right bitewing radiographs with ten degree shift revealing the presence of an irregularly shaped radiolucency at the distal and cervical aspects of the maxillary right first premolar (green ovals). (c and d) Reconstructed sagittal CBCT slices confirm the presence of and the true extent and dimension of the ECR lesion (yellow arrows)
Even with parallax radiographs, early ECR lesions may not be easily detected. Furthermore, the true extent of these lesions may not be revealed. It has been well documented that the use of CBCT assists the clinician to determine the position, depth, and more importantly, the restorability of the affected teeth before the start of treatment. The additional information provided by CBCT may change the original treatment plan and lead to a more effective and pragmatic management (Fig. 8).23,40,41,42,43
(a) Periapical radiograph of the maxillary right first molar. The patient's chief complaint was tenderness to biting. However, there was no sign of endodontic or periodontal disease. (b) Reconstructed axial, (c) sagittal and (d) coronal CBCT slices through the same tooth reveal the presence of ECR and the true extent and nature of the defect (red arrows), which involved the furcation (yellow arrow) and penetrated into the coronal third of radicular dentine (blue arrow)
Hithersay25 classified ECR into four classes/stages in order of severity. This classification aims to assist the clinician in treatment planning. Class I and II are fibro-vascular in nature and do not extend below the attachment level and are easier to treat. Class I lesions manifest as shallow defects in the dentine but class II defects penetrate well into the coronal dentine and are close to the pulp.22 Class III and IV infiltrate the radicular dentine in complex channels and are very complicated to treat.2,9,22 Class III defects invade the coronal third of the root and class IV lesions extent beyond the coronal third of the root. However, as this classification is only two-dimensional, it is only valid if ECR is solely confined to the proximal aspects of the tooth. In reality, this is not common as external cervical resorptive lesions often affect the palatal and buccal aspects of teeth and therefore are underestimated. To overcome these limitations, Patel and co workers proposed a three-dimensional classification to accurately document the true nature of ECR (Fig. 9).44
The management of ECR largely depends on the location, extent, severity, whether the lesion has perforated the root canal system and the restorability of the tooth. The management options of ECR include external repair of the resorptive defect +/- endodontic treatment, internal repair and root canal treatment, intentional replantation, periodic review (untreatable teeth), extraction (untreatable teeth)3,45. The management of ECR lesions has been described at length by Patel etal.3 and Hithersay45.
External surface resorption (ESR)
This is a non-infective, transient, pressure-induced resorption. This resorptive process will stop progressing once the source of the pressure has been removed, resulting in repair of the resorbed root-face with cementum.5,46 Orthodontic tooth movement, impacted teeth, tumours and cysts have been reported to cause surface resorption.2,5,47
Clinical examination is usually unremarkable.
ESR can only be confirmed with radiographs. The root apices are blunted and/or the roots appear shorter in orthodontically treated teeth, where perhaps excessive pressure had been applied (Fig. 10). Alternatively, the roots may appear saucer-shaped or irregularly-shaped in teeth adjacent to an expanding tumour, cyst or impacted tooth.1,2,9,10,48
(a, b, c) A series of periapical radiographs revealing extensive ESR of the maxillary right and left central incisors (green arrows), and to a lesser extent of the maxillary right lateral incisor. (d and e) The reconstructed sagittal CBCT slices through the maxillary right (d) and left (e) central incisors reveal the intact lamina dura and periodontal ligament space in the palatal aspect (yellow arrows)
CBCT examination can reveal the full extent and position of the defect and allow the clinician to assess the true extent of root destruction (Fig. 11). Typically, a CBCT would be taken for the management of the tumour, cyst or impacted teeth rather than specifically for assessing the nature of the resorptive defect.
(a) Periapical radiograph of the maxillary right incisor tooth immediately following extrusive luxation. (b) The nonvital and traumatised teeth were repositioned and subsequently endodontically treated. (c and d) 4-year review radiographs reveal signs of ESR on the mesial and distal aspects of the maxillary right incisor (yellow arrows). (e) The axial and (f) coronal CBCT slices confirm surface resorption and the presence of intact lamina dura (red arrows)
Transient apical breakdown (TAB)
Transient apical breakdown (TAB) was first described by Andreasen & Andreasen49 and is a non-infected transient resorption of the apical portion of the root and the adjacent bone. It has been reported that TAB resolves within 12 months and is associated with moderate luxation injuries. It has been suggested that it could be linked to the repair process and removal of necrotic and injured tissue.5,50
Clinical examination may reveal transient tooth discolouration and delayed or no response to sensibility testing. Delayed or no response to sensibility testing may remain especially if the tooth undergoes root canal obliteration (tertiary dentine formation).
Radiographically, there is initial widening of the periodontal ligament space and blurry appearance or loss of apical lamina dura may be observed. The radiographic appearance of the periodontal ligament and lamina dura returns to a normal state within a year.
This phenomenon is essentially an external inflammatory resorption (EIR) with a short resorption phase followed by repair. It is well established that even with a beam aiming device it is not always possible to replicate the anatomy being assessed, and it is not possible to obtain exactly the same view with repeat radiographs taken over a period of time. This inadvertent geometric distortion resulting in elongation or foreshortening may contribute to the appearance of the presence and then disappearance of a widened periodontal ligament (TAB) over a period of time (Fig. 12).50
The PDL and lamina dura on the maxillary right central incisor appear intact (b) 6-months follow-up radiograph demonstrates the resolution of TAB on the maxillary left central incisor (green arrow). However, the maxillary right central incisor is associated with a loss of apical lamina dura. (c, d, e) Coronal and sagittal CBCT slices of the same teeth reveal well defined periapical radiolucencies associated with the maxillary right and left central incisors (red arrows). The diagnosis of chronic periapical periodontitis associated with infected necrotic pulp was reached
The important clinical consideration for teeth that undergo mild to moderate luxation injuries is regular monitoring including sensibility testing and radiographic assessment of the periapical tissues. The prevalence of TAB may have been under-reported as a result of endodontic treatment being commenced. Many asymptomatic teeth with small widening of the periodontal ligament space, lack of immediate response to sensibility testing immediately after mild or moderate luxation injuries or with slight discolouration may have received root canal treatment, even though further review and assessment might have demonstrated the transient nature of the signs and symptoms. On the other hand, the disappearance of the initial radiographic signs must not be regarded as the confirmation for TAB diagnosis either, as even a slight change in beam angulation may obscure the presence of the apical radiolucency and defect.
CBCT considerations
It is well established that CBCT has an important role in the diagnosis and management of complex endodontic problems.41,51,52,53,54
Only high-resolution small field of view scans can be justified for the diagnosis and management of resorptive lesions. It is essential to optimise the radiation dose, thus minimise patient exposure to radiation.55 This will ensure compliance with the ALARA 'as low as reasonably achievable' principle and achieve the lowest effective dose based on the number of teeth affected and sites involved.
The risks and benefits of a CBCT scan must be fully discussed with patients and an informed consent obtained before any exposure. In addition, clinicians should undergo appropriate training to gain knowledge of CBCT radiography before prescribing CBCT scans.56,57
CBCT should be seen as an adjunct and not a replacement for conventional radiography. A CBCT should only be considered after thorough clinical and conventional radiographic examination and assessment has been carried out.
The referrers and interpreters of CBCT images are strongly advised to follow the European Society of Endodontology's position statement55 on the use of CBCT in endodontics.
Management considerations
The overall decision-making process regarding the management of resorptive defects must be based on the nature and cause of the resorption, the prognosis and restorability. Furthermore, to obtain informed consent, the benefits and risks of any intervention must be fully discussed with the patient.7,58 The management must focus on the removal of the source of resorption and its repair.7,58
Unrestorable (symptomatic) teeth may be extracted in medically fit and healthy patients.
In restorable teeth with signs and symptoms of irreversible pulpitis or apical periodontitis, root canal treatment should be carried out. Ideally, the resorptive lesion should be assessed using a small FOV CBCT as described previously to assess its nature and rule out perforations/root canal communications and risk of causing hypochlorite accidents.7,58
If the uninfected defect is inaccessible or requires extensive alveolar bone and tooth structure removal to be repaired, a decision may be made to leave and monitor the lesion as the lesion may cease to progress and move into repair stage.
The management of resorptive defects have been comprehensively addressed by Patel etal. (2016)7 and Darcey and Qualtrough (2013).58
Conclusion
The aim of this paper was to provide a practical guide to diagnosis and treatment of dental resorption lesions using a systematic classification.
Accurate diagnosis is required for sound clinical decision making, treatment planning and execution of the treatment. A CBCT may be indicated to confirm the diagnosis and/or aid management. When appropriate, the clinician may wish to consider referring the patient for a specialist opinion.
Patients must be fully informed of the treatment options, the prognosis of the lesions and the success of the treatment. Treatment planning must be realistic and take into account the type and stage of the resorptive condition.
References
Tronstad L . Root resorptionaetiology, terminology and clinical manifestations. Endod Dent Traumatol 1988; 4: 241–252.
Trope M . Root resorption due to dental trauma. Endod Topics 2002; 1: 79–100.
Patel S, Kanagasingam S, Pitt Ford T . External cervical resorption: a review. J Endod 2009; 35: 616–625.
Wedenberg C, Lindskog S . Evidence for a resorption inhibitor in dentine. Scand J Dent Res 1987; 95: 205–211.
Patel S, Pitt Ford T . Is the resorption external or internal? Dent Update 2007; 34: 218–229.
Mavridou A M, Hauben E, Wevers M, Schepers E, Bergmans L, Lambrechts P . Understanding external cervical resorption in vital teeth. J Endod 2016; 42: 1737–1751.
Patel S, Durack C, Ricucci D . Root resorption. In Hargreaves K. M, Berman L H (eds) Pathways of the pulp. 11th edition. pp 660–683. St Louis: Elsevier, 2016.
Patel S, Ricucci D, Durak C, Tay F . Internal root resorption: a review. J Endod 2010; 36: 1107–1121.
Heithersay G S . Management of tooth resorption. Aust Dent J 2007; 52(Suppl 1): 105–121.
Durack C, Patel S . Root resorption. In Patel S, Harvey S, Shemesh H, Durack C (eds) Cone beam computed tomography in endodontics. 1st edition. pp 119–131. Berlin: Quintessence Publishing Co. Ltd, 2016.
Bhuva B, Barnes J J, Patel S . The use of limited cone beam computed tomography in the diagnosis and management of a case of perforating internal root resorption. Int Endod J 2011; 44: 777–786.
Burleson A, Nusstein J, Reader A, Beck M . The in vivo evaluation of hand/rotary/ultrasound instrumentation in necrotic, human mandibular molars. J Endod 2007; 33: 782–787.
Hammarstöm L, Pierce A M, Blomlöf L, Feiglin B, Lindskog S . Tooth avulsion and replantation – a review. Endod Dent Traumatol 1986; 2: 1–8.
Barrett E J, Kenny D J . Avulsed permanent teeth: a review of the literature and treatment guidelines. Endodont Dent Traumatol 1997; 13: 153–163.
Lindskog S, Pierce A M, Blomlöf L, Hammarström L . The role of the necrotic periodontal membrane in cementum resorption and ankylosis. Endod Dent Traumatol 1985; 1: 96–101.
Anderson L, Blomlöf L, Lindskog S, Feiglin B, Hammarström L . Tooth ankylosis. Clinical, radiographic and histological assessments. Int J Oral Surg 1984; 13: 423–431.
Malmgren B, Malmgren O, Andreasen J O . Alveolar bone development after decoronation of ankylosed teeth. Endod Topics 2006; 14: 35–40.
Cohenca N, Stabholz A . Decoronation – a conservative method to treat ankylosed teeth for preservation of alveolar ridge before permanent prosthetic reconstruction: literature review and case presentation. Dent Traumatol 2007; 23: 87–94.
Malmgren B . Ridge preservation/decoronation. J Endod 2013; 39: S67–S72.
Mavridou A M, Bergmans L, Barendregt D, Lambrechts P . Descriptive analysis of factors associated with external cervical resorption. J Endod 2017; 43: 1602–1610.
Hithersay G S . Clinical, radiologic and histopathologic features of invasive cervical resorption. Quintessence Int 1999; 30: 27–37.
Heithersay G S . Invasive cervical resorption. Endod Topics 2004; 7: 73–92.
Gunst V, Mavridou A, Huybrechts B, Van Gorp G, Bergmans L, Lamberchts P . External cervical resorption: an analysis using cone beam and microfocus computed tomography and scanning electron microscopy. Int Endod J 2013; 46: 877–887.
Lin Y P, Love R M, Friedlander L T, Shang H F, Pai M H . Expression of toll-like receptors 2 and 4 and the OPGRANKLRANK system in inflammatory external root resorption and external cervical resorption. Int Endod J 2013; 46: 971–981.
Heithersay G S . Invasive cervical resorption: an analysis of potential predisposing factors. Quintessence Int 1999; 30: 83–95.
Harrington G W, Natkin E . External resorption associated with the bleaching of pulpless teeth. J Endod 1979; 5: 344–338.
Gunst V, Huybrechts B, De Almeida Neves A, Bergmans L, Van Meerbeek B, Lambrechts P . Playing wind instruments as a potential aetiologic cofactor in external cervical resorption: two case reports. Int Endod J 2011; 44: 268–282.
Patel S, Saberi N . External cervical resorption associated with the use of bisphosphonates: a case series. J Endod 2015; 41: 472–478.
Patel K, Schirru E, Niazi S, Mitchell P, Mannocci F . Multiple apical radiolucencies and external cervical resorption associated with varicella zoster virus: a case report. J Endod 2016; 42: 978–983.
Liang H, Burkes E J, Frederiksen N L . Multiple idiopathic cervical root resorption: systematic review and report of four cases. Dentomaxillofac Radiol 2003; 32: 150–155.
Iwamatsu-Kobayashi Y, Satoh-Kuriwada S, Yamamoto T et al. A case of multiple idiopathic external root resorption: a 6year follow-up study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005; 100: 772–779.
Neely A L, Gordon S C . A familial pattern of multiple idiopathic cervical root resorption in a father and son: a 22-year follow-up. J Periodontol 2007; 78: 367–371.
von Arx T, Schawalder P, Ackermann M, Bosshardt D D . Human and feline invasive cervical resorptions: the missing link? Presentation of four cases. J Endod 2009; 35: 904–913.
Becker A . Orthodontic treatment of impacted teeth. 3rd edition. Chichester: Wiley-Blackwell, 2012.
Holan G, Eidelman E, Mass E . Pre-eruptive coronal resorption of permanent teeth: report of three cases and their treatments. Paediatr Dent 1994; 16: 373–377.
Seow W K, Hackley D . Pre-eruptive resorption of dentin in the primary and permanent dentitions: case reports and literature review. Paediatr Dent 1996; 18: 67–71.
Davidovich E, Kreiner B, Peretz B . Treatment of severe pre-eruptive intracoronal resorption of a permanent second molar. Paediatr Dent 2005; 27: 74–77.
Mavridou A M, Hauben E, Wevers M, Schepers E, Bergmans L, Lambrechts P . Understanding external cervical resorption patterns in endodontically treated teeth. Int Endod J 2017; 50: 1116–1133.
Trope M, Barnett F, Sigurdsson A, Chivian N . The role of endodontics after dental traumatic injuries. In Hargreaves K. M, Berman L H (eds) Pathways of the pulp. 11th edition. pp. 758–792. St Louis: Elsevier, 2016.
Patel S, Dawood A . The use of cone beam computed tomography in the management of external cervical resorption lesions. Int Endod J 2007; 40: 818–830.
Patel S, Dawood A, Wilson R, Horner K, Mannocci F . The detection and management of root resorption lesions using intraoral radiography and cone beam computed tomography – an in vivo investigation. Int Endod J 2009; 42: 831–838.
Patel K, Mannocci F, Patel S . The assessment and management of external cervical resorption with periapical radiographs and cone-beam computed tomography: a clinical study. J Endod 2016; 42: 1435–1440.
Vaz de Souza D, Schirru E, Mannocci F, Foschi F, Patel S . External cervical resorption: a comparison of the diagnostic efficacy using 2 different cone-beam computed tomographic units and periapical radiographs. J Endod 2017; 43: 121–125.
Patel S, Foschi F, Mannocci F, Patel K . External cervical resorption: a three-dimensional classification. Int Endod J 2017; 51: 206–214.
Heithersay G S . Treatment of invasive cervical resorption: an analysis of results using topical application of trichloroacetic acid, curettage and restoration. Quintessence Int 1999; 30: 96–110.
Andreasen J O . External root resorption: its implications in dental traumatology, paedodontics, periodontics, orthodontics and endodontics. Int Endod J 1985; 18: 109–118.
Gunraj M N . Dental root resorption. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999; 88: 647–653.
Brezniak N, Wasserstein A . Orthodontically induced inflammatory root resorption. Part I: the basic science aspects. Angle Orthod 2002; 72: 175–179.
Andreasen F M, Andreasen J O . Diagnosis of luxation injuries: The importance of standardized clinical, radiographic and photographic techniques in clinical investigations. Endod Dent Traumatol 1985; 1: 160–169.
Andreasen F M . Transient apical breakdown and its relation to colour and sensibility changes after luxation injuries to teeth. Endod Dent Traumatol 1986; 2: 9–19.
Abella F, Patel S, Durán-Sindreu F, Mercadé M, Bueno R, Roig M . An evaluation of the periapical status of teeth with necrotic pulps using periapical radiography and cone-beam computed tomography. Int Endod J 2014; 47: 387–396.
Brady E, Mannocci F, Brown J, Wilson J, Wilson R, Patel S . A comparison of cone beam computed tomography and periapical radiography for the detection of vertical root fractures in endodontically treated teeth. Int Endod J 2014; 47: 735–746.
Ee J, Fayad M I, Johnson B R . Comparison of endodontic diagnosis and treatment planning decisions using cone-beam volumetric tomography versus periapical radiography. J Endod 2014; 40: 910–916.
Rodriguez G, Abella F, Durán-Sindreu F, Patel S, Roig M . Influence of cone-beam computed tomography in clinical decision making among specialists. J Endod 2017; 43: 194–199.
Patel S, Durack C, Abella F, Roig M, Shemesh H, Lambrechts P, Lemberg K . European society of endodontology position statement: the use of CBCT in endodontics. Int Endod J 2014; 47: 502–504.
Horner K, Islam M, Flygare L, Tsiklakis K, Whaites E . Basic principles for use of dental cone beam computed tomography: consensus guidelines of the European Academy of Dental and Maxillofacial Radiology. Dentomaxillofac Radiol 2009; 38: 187–195.
Brown J, Jacobs R, Levring Jäghagen E et al. Basic training requirements for the use of dental CBCT by dentists: a position paper prepared by the European academy of dentomaxillofacial radiology. Dentomaxillofac Radiol 2014; 43: 20130, 291.
Darcey J, Qualtrough A . Resorption: part 2. Diagnosis and management. Br Dent J 2013; 214: 493–509.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Patel, S., Saberi, N. The ins and outs of root resorption. Br Dent J 224, 691–699 (2018). https://doi.org/10.1038/sj.bdj.2018.352
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2018.352