Abstract
The second iteration of the Autism Brain Imaging Data Exchange (ABIDE II) aims to enhance the scope of brain connectomics research in Autism Spectrum Disorder (ASD). Consistent with the initial ABIDE effort (ABIDE I), that released 1112 datasets in 2012, this new multisite open-data resource is an aggregate of resting state functional magnetic resonance imaging (MRI) and corresponding structural MRI and phenotypic datasets. ABIDE II includes datasets from an additional 487 individuals with ASD and 557 controls previously collected across 16 international institutions. The combination of ABIDE I and ABIDE II provides investigators with 2156 unique cross-sectional datasets allowing selection of samples for discovery and/or replication. This sample size can also facilitate the identification of neurobiological subgroups, as well as preliminary examinations of sex differences in ASD. Additionally, ABIDE II includes a range of psychiatric variables to inform our understanding of the neural correlates of co-occurring psychopathology; 284 diffusion imaging datasets are also included. It is anticipated that these enhancements will contribute to unraveling key sources of ASD heterogeneity.
Design Type(s) | data integration objective • observation design |
Measurement Type(s) | nuclear magnetic resonance assay |
Technology Type(s) | digital curation |
Factor Type(s) | research institute • study design • Autism |
Sample Characteristic(s) | Homo sapiens • brain |
Machine-accessible metadata file describing the reported data (ISA-Tab format)
Similar content being viewed by others
Background & Summary
Multiple sources of evidence have substantiated models of abnormal neural connectivity in autism spectrum disorder (ASD)1–5. At the macroscale, abnormal connections among brain regions have been revealed by functional and structural neuroimaging in children, adolescents and, adults with ASD1,6–9. Yet, both the complexity of the brain connectome10,11 and the striking heterogeneity of ASD12–16 have hampered efforts to specify the nature of putative dysconnections. In response, open-data sharing is increasingly being encouraged to rapidly amass the large-scale datasets needed to confront heterogeneity, engage a broader range of scientific disciplines, and facilitate independent replications17–21. To bring the open data sharing model to autism neuroimaging, the Autism Brain Imaging Data Exchange (ABIDE)22 was launched in 2012. The initial ABIDE initiative—now termed ABIDE I—was the first open-access brain imaging repository of resting state functional magnetic resonance imaging (R-fMRI) and corresponding structural data of individuals with ASD and typical controls (N=539 and 573, respectively) aggregated from multiple international institutions. Here, we introduce ABIDE II (Data Citation 1), a new multi-site open data resource containing 1,044 independent datasets (ASD N=487; Controls N=557) created to enhance the significance of the questions that can be addressed regarding the neural correlates of ASD and accelerate the pace of discovery.
The initial ABIDE I effort established the feasibility of aggregating multisite data without prior harmonization, leading to more than 55 peer-reviewed studies in the 48 months since inception. Despite its success, ABIDE I is limited in regard to sample characterization and sample size. Specifically, despite containing more than 1,000 datasets, ABIDE I was not sufficiently large to furnish optimally sized discovery and replication subsamples. By combining the ABIDE I and ABIDE II data resources, investigators can select larger samples for discovery and replication, depending on their investigative endeavors. Replication samples are needed to minimize false positives and avoid settling for ‘approximate replications’19—a practice that has plagued biological psychiatry19 and neuroscience more broadly17. Additionally, as recently demonstrated, the utility of datasets for prediction increases with sample size—even if heterogeneous data sources are used to amass large samples23.
Along with increased sample size, ABIDE II provides greater phenotypic characterization than was available across the ABIDE I data collections to better address two key sources of heterogeneity. The first is psychopathology co-occurring with ASD, which has been largely overlooked in the imaging literature15,16,24. Accordingly, ABIDE II actively encouraged investigators to provide phenotypic information regarding co-occurring illness, if assessed. The second source of heterogeneity is driven by sex-related differences. These have been generally ignored in the ASD imaging literature due to the markedly higher prevalence of males with ASD and the tendency of single sites to exclude or minimally represent females. The ABIDE II sample has increased the number of available datasets from females with ASD from 65 in ABIDE I to 138 when ABIDE I+II are combined. We believe these enhancements will allow investigators to more directly investigate pathophysiology specific to ASD, to potentially identify neurobiological subgroups and facilitate the identification of protective and risk factors.
Finally, beyond its focus on intrinsic functional connectivity and other indices of intrinsic brain function, ABIDE II now includes a subset of datasets (N=284) with diffusion-weighted images. In order to facilitate immediate access and use of ABIDE II, the methods utilized to generate this resource, the resulting currently available data and their technical validation are described below.
Methods
Criteria for data contributions
We solicited investigators willing and able to openly share their previously collected awake R-fMRI data of individuals with ASD and controls, along with corresponding high-resolution anatomical images and phenotypic information. Contributions have been sought from all charter ABIDE I members and invitations are extended to any other investigators involved in ASD neuroimaging. The present work includes information regarding all contributions received prior to June 24, 2016. Contributions will continue to be accepted up to December 2016.
Contributors are encouraged to share at least 20 unique datasets per diagnostic group (i.e., ASD and controls). Data collections of only individuals with ASD are also accepted as they can be utilized for data-driven explorations addressing heterogeneity e.g., refs 25,26. Consistent with prior FCP/INDI efforts27, investigators are also encouraged to contribute nearly all MRI datasets, without a priori quality criteria (see Technical Validation for quality assessment (QA) measures incorporated into ABIDE II).
The availability of minimal phenotypic information essential for data analyses and sample characterization (i.e., diagnostic classification, age, sex) is required for contribution. To enhance phenotypic characterization, sharing of additional measures commonly used in ASD research, information on psychiatric comorbidity, medication status, cognition and/or language are highly encouraged. Similarly, to enhance the breath of investigations about the ASD connectome, whenever available, contributions of corresponding diffusion images for each individual are welcome for aggregation.
Finally, prior to data contribution, sites are required to confirm that their local Institutional Review Board (IRB) or ethics committee have approved both the initial data collection and the retrospective sharing of a fully de-identified version of the datasets (i.e., after removal of the 18 protected health information identifiers including facial information from structural images as identified by the Health Insurance Portable and Accountability Act [HIPAA]).
Of note, two institutions provided longitudinal MRI scans from subsets of individuals’ datasets (n=23 ASD and n=15 controls) previously contributed to ABIDE I. Given the relevance of developmental changes28–32, these datasets are also included in the ABIDE II. To distinguish them from the cross-sectional aggregates, these datasets are organized into a separate set of collections focused on longitudinal data using the original ABIDE I IDs.
Data preparation and aggregation
Prior to contribution, each institution is asked to rename all data by replacing local subject identification numbers with FCP/INDI identifiers. They are also asked to remove personally identifying information (PHI) including those from images (e.g., NIFTI headers and face information from any high-resolution images) using the FCP/INDI anonymization script available in http://fcon_1000.projects.nitrc.org/. Once data are fully anonymized at each site, they are submitted to the coordinating centers (Nathan Kline Institute and New York University) for review and harmonization within and across sites. Specifically, MRI data are visually inspected and edited as needed to ensure complete removal of facial information. Additionally, to further protect personal privacy, images of ears are removed from high-resolution images. Regarding phenotypic datasets, each entry is also reviewed to identify and correct missing data, any impossible entry values (e.g., beyond published maxima and minima), and extreme outliers (relative to each sample). To ensure uniformity across sites, all entries are recorded as needed and organized in a common template along with a legend of code keys. As a final step in preparation for release, both donating and coordinating sites jointly prepare a narrative for each data collection, documenting information on the methods utilized, funding sources, the investigators involved, whether any link with other databases (e.g., National Database for Autism Research—NDAR33) exists, along with publications related to the contributed datasets. Before open release, each donating site reviews their reorganized phenotypic records, five random images per imaging modality and their collection-specific narrative for final approval.
Data Records
Overview
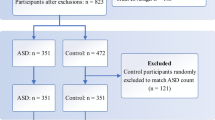
The current ABIDE II dataset encompasses 17 collections of unique independent datasets (i.e., from individuals whose data were not previously shared in ABIDE I) yielding 487 datasets classified as ASD and 557 as controls (Fig. 1a, Table 1). These represent previously collected datasets across 16 sites, including nine charter ABIDE I institutions and seven new members (See Supplementary Table 1 for information on each institution). A simple naming convention is used to label each data collection: <ABIDEII> -<institution acronym name>_<collection number>(e.g., ABIDEII-NYU_1). When a collection in ABIDE II is a continuation of one initiated in ABIDE I, we employ the same collection number used in ABIDE I (or 1 if none was used, e.g., SDSU_1, KKI_1). For new collections, a unique consecutive number is assigned (e.g., BNI_1, KUL_3). Accompanying the primary cross-sectional aggregate, two longitudinal collections are also aggregated in ABIDE II. These include MRI datasets collected as follow-ups to the MRI and phenotypic data released in ABIDE I (N total=38 unique IDs). These pilot longitudinal collections are identified as <ABIDEII> -<institution acronym name>_<Long> (Table 1).
(a) Total number of datasets per group (gray=controls; blue=autism spectrum disorder (ASD)) for the 17 cross-sectional ABIDE II data collections (i.e., collections from individuals not included in ABIDE I). Data are ordered as a function of sample size. (b) Number of males (light blue) and females (red) for each data collection, irrespective of diagnostic group. Data are ordered as a function of sample size. (c) Age at time of scan in years per collection (ordered by mean age per collection), irrespective of diagnostic group. The median age across collections (11.7 years) is depicted with a thick red dashed line; 25th, 75th, and 90th percentiles (9.3, 18.6, and 25.5 years, respectively) are represented by thin red dashed lines. (d) Distribution of full scale IQ (FIQ) standard scores per collection (ordered by lowest FIQ included per collection) for all datasets, irrespective of diagnostic group. The median FIQ across collections (112) is depicted with a thick red dashed line; 25th, 75th, and 90th percentiles (101, 122, and 130, respectively) are represented by thin red dashed lines. (e) Tukey’s box-whiskers plots depict the distribution of Autism Diagnostic Observation Schedule, Second Edition (ADOS-2) total calibrated severity scores (CSS) for ASD datasets in the nine collections sharing them (ordered by mean CSS per collection). The black plus sign depicts the mean CSS for each collection. (f) Distribution of Social Responsiveness Scale (SRS) total T scores (gray=controls; blue=ASD) in the 12 collections sharing them. For each collection, red dashed and solid lines indicate mean SRS total T scores of ASD and controls, respectively.
All ABIDE II datasets can be accessed, after establishing a login and user password, through FCP/INDI at the Neuroimaging Informatics Tools and Resources Clearinghouse (NITRC; http://fcon_1000.projects.nitrc.org/indi/abide/). The datasets are organized by data collection and stored in.tar files, each containing imaging and phenotypic data.
Phenotypic information
All phenotypic data are stored in comma separated value (.csv) files. A legend describing each phenotypic variable source is available at the website http://fcon_1000.projects.nitrc.org/indi/abide/abide_II.html. Phenotypic files are organized by data collection; a phenotypic composite file including all variables across all collections is also available. Counts of phenotypic variables available for each collection and distributions of selected key variables for each diagnostic group are provided in Supplementary Tables 2 and 3. Below, we briefly describe the main demographics and key phenotypic variables provided in the 17 cross-sectional ABIDE II data collections (Figs 1 and 2).
(a) Number of ASD datasets with and without psychiatric diagnoses for each of the nine data collections sharing information on categorical psychiatric diagnoses other than ASD. (b) Percentage of ASD datasets with one (black), two (dark gray) or more (light gray) comorbid diagnoses and those without any comorbidity (white) across the nine collections sharing comorbidity information. (c) Distribution of ASD datasets with comorbidity divided into those with comorbid Attention-Deficit/Hyperactivity Disorder (ADHD, green), anxiety (blue/white pattern) or others (cyan-white pattern) for each collection. Other comorbidities include enuresis, and/or mood, speech and language and/or disruptive behavior disorders. Here, given that multiple comorbid disorders can co-occur, the number of comorbid ASD datasets across categories exceeds the absolute number of comorbid ASD datasets.
Diagnostic classification
A dummy variable indicates diagnostic group (1 and 2 for ASD and controls, respectively). Given the retrospective nature of this data aggregate, assessment protocols used to identify ASD and controls varied across institutions. They are documented in each data collection narrative. Briefly, ASD classification was determined by either 1) combining clinical judgment with ‘gold standard’ diagnostic instruments—Autism Diagnostic Observation Scale34,35 and/or Autism Diagnostic Interview-Revised36 [ADOS, ADI-R]; (n=12 data collections; 368 ASD datasets) or 2) by using these ‘gold standard’ diagnostic instruments only (n=4 collections; 92 ASD datasets), with one exception. Specifically, in EMC_1 (n=27 datasets), which was selected from the longitudinal Generation R sample37, the ASD classification was based on prior medical records documenting ASD among those individuals meeting screening cutoffs in at least one of two distinct ASD questionnaires or for whom the mother reported a diagnosis of ASD. Regarding controls (N=557, available for 15 collections), all datasets are characterized by absence of ASD diagnosis and absence of history of any other major neurodevelopmental disorders for the vast majority of the datasets (N=546; 98%). This was determined using semi-structured/unstructured in-person interviews (N=7 data collections; 353 datasets), or parent/self- (if adults) reports/questionnaires (N=8; 193 datasets). The remaining 11 control datasets (OHSU_1 data collection) are from individuals assigned a ‘rule out’ psychiatric disorder, but without ASD or Attention-Deficit/Hyperactivity Disorder (ADHD) diagnoses.
Other specific inclusion/exclusion criteria used for selecting controls (e.g., IQ range, first degree relative with ASD) or ASD (e.g., absence of reported seizure and genetic syndromes) varied across collections. Each collection narrative on the ABIDE II website provides details regarding these criteria.
Demographics
Across collections, age at time of scanning ranges from 5 to 64 years; four of the collections focused specifically on adults—with one of these collections specifically enrolling on older adults (BNI_1)—and eight enrolling only children and/or adolescents. The remaining five data collections include children, teens and young adults, which allows for cross-sectional age-related explorations (Fig. 1c; Supplementary Table 3). All but four collections include data from both sexes (Fig. 1b). Reflecting the higher prevalence of males in ASD38, 15% of the ASD datasets consist of females versus 31% of the control datasets (Supplementary Table 3).
Intelligence
Full scale intelligence quotient (FIQ) and/or verbal and/or performance IQ standard scores are provided. Across collections, although variation exists with respect to the minimum FIQ, 97% of the datasets have FIQ above 80 (Fig. 1d). For both groups, mean FIQ is above average, albeit significantly higher in controls versus ASD (Mann Whitney U=86.5; P<0.0001; Supplementary Table 3).
Handedness
Categorical handedness codes for right, left or mixed handedness are available across all collections. Additionally, handedness strength scores are available for eight collections, enabling dimensional characterization of handedness (n=244 ASD and n=327 controls). Across collections, right-handedness is more frequent in both diagnostic groups (84 and 90% for ASD and controls, respectively), though a significantly higher prevalence of non-right-handedness (either left or mixed handedness) occurs in ASD relative to controls (χ12=10.6, P=0.01; Supplementary Table 3).
ASD core measures
Scores from the ADOS and ADI-R are available (Supplementary Table 3). Only nine collections share ADOS-2 calibrated severity scores34 (CSS; N=9 sites; 228 ASD datasets) recently designed to adjust for differences in age, intellectual abilities and language skills across ADOS modules39,40. As illustrated in Fig. 1f, CSS distribution are similar across most sites. ADOS-G41 scaled total scores are available for 15 collections (n=280 ASD datasets). Additionally, data from parent or self-report questionnaires commonly used in the field to quantify severity on multiple ASD domains collected across both diagnostic groups are also available. The Social Responsiveness Scale42 is the most common (n=378 ASD, n=407 controls; Fig. 1f) followed by the Repetitive Behavior Scale Revised43,44 (n=217 ASD, n=208 controls; Supplementary Table 3).
Comorbid psychopathology in ASD
Information on psychopathology accompanying ASD is provided either as 1) categorical diagnostic labels (or its absence, if assessed) with corresponding diagnostic code based on the International Classification of Diseases-9th edition45 (N=9 data collections; 281 ASD datasets) and/or as severity scores in one or multiple psychopathology dimensions across available for 11 collections (see Supplementary Table 3 for a list of measures used) (Fig. 2). Categorical comorbid psychiatric diagnoses were determined based on clinicians’ assessments in seven data collections, parent-questionnaires in one data collection (UCD_1) and self-report in another (KUL_3). Consistent with the clinical literature46–48, approximately 60% of the ASD data correspond to individuals with one or more co-occurring psychiatric diagnoses (Fig. 2b); the most frequent are ADHD and anxiety disorders.
MRI data
For each of the 17 ABIDE II cross-sectional collections, for each unique ID#, at least one structural MRI (sMRI), one corresponding R-fMRI dataset are available (except for one individual in the IP collection for which only MRI is available); corresponding diffusion MRI (dMRI) datasets are available for six collections. One data collection (SDSU) provided field map-corrected version of its R-fMRI and DTI data. The two pilot longitudinal collections include sMRI and R-fMRI datasets collected at two time points (1–2 years apart) for 23 individuals with ASD and 15 controls.
Consistent with its popularity in the imaging community and prior usage in FCP/INDI efforts, the NIFTI file format was selected for storage of the ABIDE II MRI datasets. With the exception of a single collection (IP_1, 1.5 Tesla), all MRI data were acquired using 3 Tesla scanners. Table 1 lists the specific MRI scanners and head coils utilized for each collection, along with the number of individuals available for each MRI modality within diagnostic groups (i.e., ASD and controls). Specific MRI sequence parameters for the various data collections are summarized in Tables 2, 3, 4 and detailed on the ABIDE II website. Across collections, R-fMRI acquisition durations varied from five to eight minutes (6:21±0.04 min) per individual; in all but four collections, individuals were verbally asked to keep their eyes open. For 12 collections, exposure to scan simulators prior to scanning was also used for habituation, as documented in the narratives.
Technical Validation
Consistent with the established FCP/INDI policy, all data contributed to ABIDE II was made available to users regardless of data quality27. The rationale of this decision includes the lack of consensus on optimal quality criteria in regards to specific measures or their combinations and cutoffs. Additionally, depending on the study goal, the availability of scans with a range of quality can facilitate the development of artifact correction techniques18. For initiatives focusing on clinical populations like ABIDE II, the inclusion of datasets with artifacts such as motion are valuable, as they enable investigators to determine impact of such real-world confounds on reliability and reproducibility.
To facilitate quality assessment of the ABIDE II collections and selection of datasets for analyses by individual users, we used the Preprocessed Connectome Project quality assurance protocol49 (http://preprocessed-connectomes-project.github.io). These encompass quantitative metrics commonly used in the imaging literature for assessing data quality, particularly for multisite projects, e.g., ref. 50. They include spatial metrics of scanner performance such as contrast to noise ratio50 artifactual voxel detection51 as well as temporal metrics including those quantifying head motion52; all metrics are summarized in Table 5 and all are available in the data release. As expected by design, within- and between-site variation exists across quality metrics (see Figs 3 and 4 and Supplementary Fig. 1 for examples of spatial and temporal metrics in sMRI, R-fMRI and DTI). It is important to note that the field remains without consensus standards for the usage of QA measures. Additionally, differences in some measures across collections may reflect purposeful tradeoffs in the design of an imaging protocol, which may not be readily obvious at times. As such, caution should be taken in over-interpretation of between-collection differences in QA measures. At a minimum, the various QA measures provided can be used to find outlier datasets for a given site; though, potentially they may be used to provide insights into the impact of differences in acquisition protocols on quality measures as well.
(a) Contrast-to-noise ratio (CNR)50, (b) smoothness of voxels indexed as full half-width maximum (FHWM)62, (c) signal-to-noise ratio (SNR)50, (d) artifactual voxel detection (Qi1)51- See Table 5 for details on this and the other quality metrics released. The colored scatterplots illustrate the quality metrics distribution for spatial MRI dataset within a given ADBIE II collection (17 cross-sectional and 2 longitudinal collections). The black and white violin plots represent a kernel density estimation of the distribution across all datasets for each quality metrics. The midline thick gray line represents the value that occurs most commonly in the distribution. For each plot the horizontal gray lines mark the 1st, 5th, 25th, 50th (solid gray line), 75th, 95th and 99th percentiles starting from the bottom.
Spatial metrics include: (a) Ghost to single ratio (GSR)50; (b) smoothness of voxels indexed as full-width half maximum (FWHM)62, (c) signal to noise ratio (SNR)50. Temporal metrics are: (d) mean framewise displacement52; (e) standardized DVARS63, and (f) global correlation (GCORR)64—See Table 5 for details on this and the other quality metrics released. The colored scatterplots illustrate the quality metrics distribution for spatial MRI dataset within a given ADBIE II collection (17 cross-sectional and 2 longitudinal collections). The black and white violin plots represent a kernel density estimation of the distribution across all datasets for each quality metrics with its midline thick gray line representing the value that occurs most commonly in the distribution. For each plot, the horizontal gray lines mark the 1st, 5th, 25th, 50th (solid gray line), 75th, 95th and 99th percentiles starting from the bottom.
Usage Notes
As data aggregation followed independent data collections across multiple sites, various sources of heterogeneity exist between collections. They can range from inclusion/exclusion criteria, recruitment/sampling strategies, MRI scanner types, data acquisition parameters and instructions (e.g., eyes open versus closed). Users must be aware of such factors when designing their research questions and selecting data for analyses accordingly. Care should be taken when attempting to draw comparisons across ABIDE I and ABIDE II, as they are independently created aggregate datasets, bringing with them both commonalities and differences. Nine institutions participated in both initiatives with either related collections in regard to both phenotypic and imaging protocols (e.g., NYU_1 in ABIDE II is a continuation of NYU in ABIDE I) or collections acquired through independent protocols (e.g., KUL_3 in ABIDE II). We suggest consideration of the commonalities and differences among contributions when attempting to combine datasets from the two ABIDE initiatives. The narratives included in the ABIDE II website should facilitate this process—see Supplementary Fig. 2 for the collections distributed among the ABIDE initiatives. As a general rule, for aggregate data analyses datasets should be selected to ensure that the number ASD and TDC data are balanced at each collection, unbalanced designs (e.g., all typical participants selected from one collection, all ASD selected from another) should be avoided.
The impact of known and unknown sources of heterogeneity between collections should also be taken in account at the analytical level. First, we encourage the use of standardization at individual- and group-level analyses e.g., refs 53–55. Second, we recommend to model data collection as a covariate at the group level when possible, to account for the variance related to the specific site protocol e.g., refs 53,56,57. Users can also employ meta-analytic approaches that have been shown to be fruitful for examination of cortical thickness or structural volumes e.g., ref. 58. Awareness of site-related variability should also be reflected in the presentation of findings. For example, effects within each data collection should be reported along with those obtained across collections e.g., refs 29,56,59. Inconsistencies that arise may be informative and provide insights into known or unknown differences in samples including and beyond data acquisition protocols. Finally, we note that along with the challenges related to its multisite post-hoc data aggregation, ABIDE II also offers a unique opportunity to develop analytical approaches to address these challenges. For example, a recent effort based on ABIDE I demonstrated the ability to optimize classifiers for the prediction of data from previously unseen imaging sites23.
The need for careful consideration of variation in acquisition parameters also applies to the use of the quality assurance (QA) metrics available for the ABIDE-II sample. Some QA measures may be more or less comparable across data collections. Mean FD is an example of a measure commonly used for QA in resting state fMRI studies, albeit without significant considerations on the impact of the specific acquisition protocol employed. Motion-induced fluctuations in the BOLD signal are primarily due to spin history effects and partial voluming, which are proportional to the amount of tissue displacement between subsequent excitations. From this perspective, one might expect that factors capable of impacting spin history effects or partial voluming, would in turn impact meanFD. Importantly, these relationships may not necessarily be linear or additive. As such, some caution is suggested when interpreting systematic differences in meanFD, or related motion metrics (e.g., DVARS), across collections. Users may also employ this and other shared multisite datasets e.g., refs 60,61 to explore the impact of possible differences related to acquisition parameters, such as TR and other, on motion metrics. MeanFD computed in DTI data should not be used for comparisons between different collections with different MRI protocols. Mean FD in DTI is the result of the combination of both eddy current effects and head motion. As a result, meanFD can be used to compare and select data within collections obtained with the same scanning protocols and equipment.
Finally, to facilitate replications among studies using ABIDE data, we encourage users to provide the ID list utilized for their published manuscripts in the manuscript section of the ABIDE website (http://fcon_1000.projects.nitrc.org/indi/abide/manuscripts.html). Users are also requested to acknowledge the primary funding source for ABIDE II (NIMH 5R21MH107045) in any manuscripts using the ABIDE II data.
Additional Information
How to cite this article: Di Martino, A. et al. Enhancing studies of the connectome in autism using the autism brain imaging data exchange II. Sci. Data 4:170010 doi: 10.1038/sdata.2017.10 (2017).
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
References
Minshew, N. J. & Williams, D. L. The new neurobiology of autism: cortex, connectivity, and neuronal organization. Archives of Neurology 64, 945–950 (2007).
Geschwind, D. H. & Levitt, P. Autism spectrum disorders: developmental disconnection syndromes. Current opinion in neurobiology 17, 103–111 (2007).
Frith, C. Is autism a disconnection disorder? Lancet Neurology 3, 577 (2004).
Hutsler, J. J. & Casanova, M. F. Review: Cortical construction in autism spectrum disorder: columns, connectivity and the subplate. Neuropathology and applied neurobiology 42, 115–134 (2016).
Bourgeron, T. From the genetic architecture to synaptic plasticity in autism spectrum disorder. Nature reviews Neuroscience 16, 551–563 (2015).
Minshew, N. J. & Keller, T. A. The nature of brain dysfunction in autism: functional brain imaging studies. Current Opinion in Neurology 23, 124–130 (2010).
Vissers, M. E., Cohen, M. X. & Geurts, H. M. Brain connectivity and high functioning autism: a promising path of research that needs refined models, methodological convergence, and stronger behavioral links. Neuroscience and biobehavioral reviews 36, 604–625 (2012).
Just, M. A., Cherkassky, V. L., Keller, T. A. & Minshew, N. J. Cortical activation and synchronization during sentence comprehension in high-functioning autism: evidence of underconnectivity. Brain: a journal of neurology 127, 1811–1821 (2004).
Picci, G., Gotts, S. J. & Scherf, K. S. A theoretical rut: revisiting and critically evaluating the generalized under/over-connectivity hypothesis of autism. Developmental science 19, 524–549 (2016).
Kelly, C., Biswal, B. B., Craddock, R. C., Castellanos, F. X. & Milham, M. P. Characterizing variation in the functional connectome: promise and pitfalls. Trends in cognitive sciences 16, 181–188 (2012).
Craddock, R. C. et al. Imaging human connectomes at the macroscale. Nat Med 10, 524–539 (2013).
Hughes, V. Epidemiology: Complex disorder. Nature 491, S2–S3 (2012).
Geschwind, D. H. Advances in autism. Annu Rev Med 60, 367–380 (2009).
Lenroot, R. K. & Yeung, P. K. Heterogeneity within Autism Spectrum Disorders: What have We Learned from Neuroimaging Studies? Front Hum Neurosci 7, 733 (2013).
Lai, M. C., Lombardo, M. V., Chakrabarti, B. & Baron-Cohen, S. Subgrouping the autism ‘spectrum’: reflections on DSM-5. PLoS Biol. 11, e1001544 (2013).
Grzadzinski, R., Huerta, M. & Lord, C. DSM-5 and autism spectrum disorders (ASDs): an opportunity for identifying ASD subtypes. Mol. Autism 4, 12 (2013).
Button, K. S. et al. Power failure: why small sample size undermines the reliability of neuroscience. Nature reviews Neuroscience 14, 365–376 (2013).
Milham, M. P. Open neuroscience solutions for the connectome-wide association era. Neuron 73, 214–218 (2012).
Kapur, S., Phillips, A. G. & Insel, T. R. Why has it taken so long for biological psychiatry to develop clinical tests and what to do about it? Molecular psychiatry 17, 1174–1179 (2012).
Castellanos, F. X., Di Martino, A., Craddock, R. C., Mehta, A. D. & Milham, M. P. Clinical applications of the functional connectome. NeuroImage 80, 527–540 (2013).
Gorgolewski, K. J., Margulies, D. S. & Milham, M. P. Making data sharing count: a publication-based solution. Frontiers in neuroscience 7, 9 (2013).
Di Martino, A. et al. The autism brain imaging data exchange: towards a large-scale evaluation of the intrinsic brain architecture in autism. Molecular psychiatry 19, 659–667 (2014).
Abraham, A. et al. Deriving reproducible biomarkers from multi-site resting-state data: An Autism-based example. NeuroImage 147, 736–745 (2016).
Solomon, M., Miller, M., Taylor, S. L., Hinshaw, S. P. & Carter, C. S. Autism symptoms and internalizing psychopathology in girls and boys with autism spectrum disorders. J Autism Dev Disord. 42, 48–59 (2012).
Karalunas, S. L. et al. Subtyping attention-deficit/hyperactivity disorder using temperament dimensions: toward biologically based nosologic criteria. JAMA psychiatry 71, 1015–1024 (2014).
Yang, Z. et al. Generalized RAICAR: discover homogeneous subject (sub)groups by reproducibility of their intrinsic connectivity networks. NeuroImage. 63, 403–414 (2012).
Mennes, M., Biswal, B., Castellanos, F. X. & Milham, M. P. Making data sharing work: The FCP/INDI experience. NeuroImage 82, 683–691 (2012).
Padmanabhan, A., Lynn, A., Foran, W., Luna, B. & O'Hearn, K. Age related changes in striatal resting state functional connectivity in autism. Frontiers in human neuroscience 7, 814 (2013).
Alaerts, K. et al. Age-related changes in intrinsic function of the superior temporal sulcus in autism spectrum disorders. Social cognitive and affective neuroscience 10, 1413–1423 (2015).
Di Martino, A. et al. Unraveling the miswired connectome: a developmental perspective. Neuron 83, 1335–1353 (2014).
Plitt, M., Barnes, K. A., Wallace, G. L., Kenworthy, L. & Martin, A. Resting-state functional connectivity predicts longitudinal change in autistic traits and adaptive functioning in autism. Proceedings of the National Academy of Sciences of the United States of America. 112, E6699–E6706 (2015).
Lynn, A. C. et al. Functional connectivity differences in autism during face and car recognition: underconnectivity and atypical age-related changes. Developmental science (2016).
Hall, D., Huerta, M. F., McAuliffe, M. J. & Farber, G. K. Sharing heterogeneous data: the national database for autism research. Neuroinformatics 10, 331–339 (2012).
Gotham, K., Risi, S., Pickles, A. & Lord, C. The Autism Diagnostic Observation Schedule: revised algorithms for improved diagnostic validity. Journal of autism and developmental disorders 37, 613–627 (2007).
Lord, C., Rutter, M., DiLavore, P. C. & Risi, S. Autism Diagnostic Observation Schedule (Western Psychological Service, 1999).
Rutter, M., LeCoutuer, A. & Lord, C. . Autism Diagnostic Interview-Revised (ADI-R) manual (Western Psychological Services, 2003).
Jaddoe, V. W. et al. The Generation R Study: design and cohort update 2012. European journal of epidemiology 27, 739–756 (2012).
Centers for Disease Control and Prevention. Prevalence of Autism Spectrum Disorders—Autism and Developmental Disabilities Monitoring Network, 14 Sites, United States, 2008. MMWR Surveill Summ 61, 1–19 (2012).
Gotham, K., Pickles, A. & Lord, C. Standardizing ADOS scores for a measure of severity in autism spectrum disorders. Journal of autism and developmental disorders 39, 693–705 (2009).
Jones, R. M. & Lord, C. Diagnosing autism in neurobiological research studies. Behavioural brain research 251, 113–124 (2012).
Lord, C. et al. The Autism Diagnostic Observation Schedule-Generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of autism and developmental disorders 30, 205–223 (2000).
Constantino, J. N. & Gruber, C. P. . Social Responsiveness Scale (SRS): Manual (Western Psychological Services, 2005).
Bodfish, J. W., Symons, F. J., Parker, D. E. & Lewis, M. H. Varieties of repetitive behavior in autism: comparisons to mental retardation. Journal of autism and developmental disorders 30, 237–243 (2000).
Lam, K. S. & Aman, M. G. The Repetitive Behavior Scale-Revised: independent validation in individuals with autism spectrum disorders. Journal of autism and developmental disorders 37, 855–866 (2007).
World Health Organization. ICD-9-CM: International classification of diseases, 9th revision, clinical modification (Medicode, 1996).
Simonoff, E. et al. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. Journal of the American Academy of Child and Adolescent Psychiatry 47, 921–929 (2008).
Simonoff, E. et al. The persistence and stability of psychiatric problems in adolescents with autism spectrum disorders. Journal of child psychology and psychiatry, and allied disciplines 54, 186–194 (2013).
Lai, M. C., Lombardo, M. V. & Baron-Cohen, S. Autism. Lancet 383, 896–910 (2014).
Shehzad, Z. et al. The Preprocessed Connectomes Project Quality Assessment Protocol—a resource for measuring the quality of MRI data. Frontiers in neuroscience (2015).
Magnotta, V. A., Friedman, L. & First, B. Measurement of Signal-to-Noise and Contrast-to-Noise in the fBIRN Multicenter Imaging Study. Journal of digital imaging 19, 140–147 (2006).
Mortamet, B. et al. Automatic quality assessment in structural brain magnetic resonance imaging. Magn Reson Med. 62, 365–372 (2009).
Jenkinson, M., Bannister, P., Brady, M. & Smith, S. Improved optimization for the robust and accurate linear registration and motion correction of brain images. NeuroImage 17, 825–841 (2002).
Yan, C. G., Craddock, R. C., Zuo, X. N., Zang, Y. F. & Milham, M. P. Standardizing the intrinsic brain: Towards robust measurement of inter-individual variation in 1000 functional connectomes. NeuroImage 80, 246–262 (2013).
Panta, S. R. et al. A Tool for Interactive Data Visualization: Application to Over 10,000 Brain Imaging and Phantom MRI Data Sets. Frontiers in neuroinformatics 10, 9 (2016).
Chen, S., Kang, J. & Wang, G. An empirical Bayes normalization method for connectivity metrics in resting state fMRI. Frontiers in neuroscience 9, 316 (2015).
Valk, S. L., Di Martino, A., Milham, M. P. & Bernhardt, B. C. Multicenter mapping of structural network alterations in autism. Human brain mapping 36, 2364–2373 (2015).
Fard, P. K., Matthis, C., Balsters, J. H., Maathuis, M. & Wenderoth, N. Promises, pitfalls, and basic guidelines for applying machine learning classifiers to psychiatric imaging data, with autism as an example. Front. Psychiatry 7, 177 (2015).
Schmaal, L., Hibar, D., Thompson, P., Veltman, D. & Grp, E.-M. W. Cortical brain alterations in major depressive disorder (MDD) from adolescence to adulthood: findings from the enigma-MDD working group. Bipolar disorders 18, 19–19 (2016).
Nielsen, J. A. et al. Multisite functional connectivity MRI classification of autism: ABIDE results. Frontiers in human neuroscience 7 (2013).
Zuo, X. N. et al. An open science resource for establishing reliability and reproducibility in functional connectomics. Sci. Data 1, 140049 (2014).
Fair, D. A. et al. Distinct neural signatures detected for ADHD subtypes after controlling for micro-movements in resting state functional connectivity MRI data. Frontiers in systems neuroscience 6, 80 (2012).
Friedman, L., Glover, G. H., Krenz, D. & Magnotta, V. Reducing inter-scanner variability of activation in a multicenter fMRI study: Role of smoothness equalization. NeuroImage. 32, 1656–1668 (2006).
Nichols, T. E. Standardizing DVARS. http://blogs.warwick.ac.uk/nichols/entry/standardizing_dvars. (2012).
Saad, Z. S. et al. Correcting brain-wide correlation differences in resting-state FMRI. Brain connectivity 3, 339–352 (2013).
Atkinson, D., Hill, D. L. G., Stoyle, P. N. R., Summers, P. E. & Keevil, S. F. Automatic correction of motion artifacts in magnetic resonance images using an entropy focus criterion. Ieee T Med Imaging 16, 903–910 (1997).
Giannelli, M., Diciotti, S., Tessa, C. & Mascalchi, M. Characterization of Nyquist ghost in EPI-fMRI acquisition sequences implemented on two clinical 1.5T MR scanner systems: effect of readout bandwidth and echo spacing. J Appl Clin Med Phys. 11, 170–180 (2010).
Cox, R. W. AFNI: Software for analysis and visualization of functional magnetic resonance neuroimages. Comput Biomed Res 29, 162–173 (1996).
Data Citations
Di Martino, A. Functional Connectomes Project International Neuroimaging Data-Sharing Initiative https://doi.org/10.15387/FCP_INDI.ABIDE2 (2016)
Acknowledgements
We would like to thank the numerous contributors at each donating institution (see Supplementary Table 1 and http://fcon_1000.projects.nitrc.org/indi/abide/) as well as the www.nitrc.org team for providing the data-sharing platform. We are particularly thankful to Tanmay Nath for support in aspects of website organization and assistance in some aspects of MRI data review along with Dorothea Floris, Yuta Aoki, Lindsay Alexander and Erica Ho. Support for ABIDE II coordination and data aggregation was provided by NIMH (521MH107045) to A.D.M. and gifts from Joseph P. Healey, Phyllis Green and Randolph Cowen to M.P.M. (M.P.M. is a Randolph Cowen and Phyllis Green Scholar). Support for data collection at each site was provided by NIH (MH084961-GU_1; MH094409-IU_1; NS048527, MH085328, MH078160-KKI_1; MH102660, MH087770, MH084126, MH081218, HD065282-NYU_1; MH102660-NYU_2; MH095888-ONRC_2; MH096773, MH091238, MH096773-03S1, MH086654-OHSU_1; MH081023, MH097972-SDSU_1; MH099250-01-UCD_1; HD055784-UCLA_1; MH092697, MH080826, MH60450, DC008553, NS34783-USM_1; HD065280-01-UCLA_Long; MH081191, MH67924, HD55748-UPSM_Long), Autism Speaks (KKI_1, 04593; UPSM_Long), the Simons Foundation (307280; EMC_1, OHSU_1), IDDRC (HD040677-07; GU_1), State of Arizona Alzheimer’s Consortium, BNI and Department of Defense (AR140105; BNI_1), Dutch ZonMw TOP grant (91211021; EMC_1), European Community’s 7th Framwork Programme (FP7/2008-2013, 212652; EMC_1), Physical Sciences Division, SURFsara, the Municipal Health Service Rotterdam area, the Rotterdam Homecare Foundation, and the Stichting Trombosedienst & Artsenlaboratorium Rijnmond STAR-MDC (EMC_1), Institut Pasteur, CNRS, INSERM, AP-HP, University Paris 7 Diderot, the BioPsy Labex, the DHU PROTECT, the Bettencourt-Schueller Foundation, the FondaMental Foundation, and the ANR SynDiv (IP_1), Branco Weiss fellowship of the Society in Science ETH Zürich, Marguerite-Marie Delacroix Foundation, Flanders Fund for Scientific Research (FWO project 1521313N, G.0401.12;1206013N; KUL_3), the Stavros Niarchos Foundation, The Leon Levy Foundation, an endowment provided by Phyllis Green and Randolph Cowen, and Goldman Sachs Gives on behalf of Ram Sundaram (NYU_1), DeStefano Family Foundation, Oregon Clinical and Translational Institute, and Medical Research Foundation (OHSU_1), National Children’s Research Centre Our Lady’s Children’s Hospital (TCD_1), University of Utah Multidisciplinary Research Seed Grant, NRSA Predoctoral Fellowship (F32 DC010143; USM_1), Ben B. and Iris M. Margolis Foundation (USM_1), and UCLA Autism Center for Excellence (UCLA_Long).
Author information
Authors and Affiliations
Contributions
Conception, design and implementation of the ABIDE II initiative, data analyses and preparation of the manuscript: A.D.M. & M.P.M. Data aggregation and analyses: D.O’C. & B.C. Development of the Quality Control Pipeline for MRI data analyses: R.C.C. Conceptualization on some aspects of study design: B.L., C.L. Data contribution: K.A., J.S.A., M.A., J.H.B., L.B.a., A.B., S.B., L.B.l., S.Y.B., B.B.B., L.B.y., F.X.C., M.D., R.D., A.D.M., D.A.F., I.F., J.F., L.G., R.J.J.K., D.P.K., J.E.L., B.L., S.H.M., R.A.M., M.B.N., J.T.N., K.O’H., M.S., R.T., C.J.V., N.W., & T.W. Editorial input in preparation of manuscript: F.X.C. All authors have provided critical review and final approval of the manuscript version submitted.
Corresponding authors
Ethics declarations
Competing interests
C.L. receives royalties from the publication of the Autism Diagnostic Interview-Revised and the Autism Diagnostic Observation Schedule. The remaining authors declare no competing financial interests.
ISA-Tab metadata
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0 Metadata associated with this Data Descriptor is available at http://www.nature.com/sdata/ and is released under the CC0 waiver to maximize reuse.
About this article
Cite this article
Di Martino, A., O’Connor, D., Chen, B. et al. Enhancing studies of the connectome in autism using the autism brain imaging data exchange II. Sci Data 4, 170010 (2017). https://doi.org/10.1038/sdata.2017.10
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/sdata.2017.10
This article is cited by
-
Differently different?: A commentary on the emerging social cognitive neuroscience of female autism
Biology of Sex Differences (2024)
-
Structural connectome alterations between individuals with autism and neurotypical controls using feature representation learning
Behavioral and Brain Functions (2024)
-
Deep learning based joint fusion approach to exploit anatomical and functional brain information in autism spectrum disorders
Brain Informatics (2024)
-
Predicting high-level visual areas in the absence of task fMRI
Scientific Reports (2024)
-
Efficacy of MRI data harmonization in the age of machine learning: a multicenter study across 36 datasets
Scientific Data (2024)