Abstract
Chronic lymphocytic leukemia (CLL) has a complex pattern of driver mutations and much of its clinical diversity remains unexplained. We devised a method for simultaneous subgroup discovery across multiple data types and applied it to genomic, transcriptomic, DNA methylation and ex vivo drug response data from 217 patients with CLL. We uncovered a biological axis of heterogeneity strongly associated with clinical behavior and orthogonal to known biomarkers. We validated its presence and clinical relevance in four independent cohorts (n = 547 patients). We found that this axis captures the proliferative drive (PD) of CLL cells, as it associates with lymphocyte doubling rate, global hypomethylation, accumulation of driver aberrations and response to pro-proliferative stimuli. CLL–PD was linked to the activation of mTOR–MYC–oxidative phosphorylation through transcriptomic, proteomic and single-cell resolution analysis. CLL–PD is a key determinant of disease outcome in CLL. Our multi-table integration approach may be applicable to other tumors whose inter-individual differences are currently unexplained.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
For the samples from our study cohort, the sequencing read data from whole-exome sequencing, targeted sequencing, DNA methylation profiling and RNA-seq assay were deposited in the European Genome–phenome Archive under accession code EGAS00001001746. The native mass spectrometer output files (in .RAW format) for proteomic data are available at Proteomics Identifications Database (https://www.ebi.ac.uk/pride/, identifier: PXD025756). The CyTOF signal intensity data (in .fcs format) are available at BioStudies (https://www.ebi.ac.uk/biostudies/, identifier: S-BSST587). Source data for main and Extended Data Figs. have been provided as Source Data files. Processed omics data, including DNA-seq, RNA-seq, DNA methylation profiling, proteomic profiling, CyTOF and drug sensitivity data are available in the R package mofaCLL (https://github.com/Huber-group-EMBL/mofaCLL).
In our study, we used some public datasets: RNA-seq data from ICGC-CLL cohort via the ICGC data portal (https://dcc.icgc.org/) under accession code CLLE-ES; microarray expression data from the Munich CLL cohort, the UCSD CLL cohort and the Duke CLL cohort at ArrayExpress (https://www.ebi.ac.uk/arrayexpress/) under accession codes: E-GEOD-22762, E-GEOD-39671 and E-GEOD-10138, respectively. The public microarray expression data of CLL cells upon four pro-proliferative stimulations are available at ArrayExpress under accession codes E-GEOD-30105 (CpG ODN), E-GEOD-50572 (co-culturing with T cells and IL21 + CD40L treatment) and E-GEOD-39411 (cross-linked anti-IgM). The Hallmark gene set (v.6.2) was downloaded from MSigDB (http://www.gsea-msigdb.org/gsea/msigdb/index.jsp). The list of Solo-WCGW CpGs for human genome assembly GRCh37 (hg19) was downloaded from https://zwdzwd.github.io/pmd. Source data are provided with this paper.
Code availability
The computational codes, in the form of Rmarkdown documents, for reproducing all major figures and results reported in this article are provided in the mofaCLL R package on GitHub (https://github.com/Huber-group-EMBL/mofaCLL) under GNU General Public License v.3.0. The CLLPDestimate function in the mofaCLL R package can be used to compute CLL–PD from compatible gene expression data. Instructions are in the vignette of the package.
References
Guièze, R. & Wu, C. J. Genomic and epigenomic heterogeneity in chronic lymphocytic leukemia. Blood 126, 445–453 (2015).
Zenz, T., Mertens, D., Küppers, R., Döhner, H. & Stilgenbauer, S. From pathogenesis to treatment of chronic lymphocytic leukaemia. Nat. Rev. Cancer 10, 37–50 (2010).
Oakes, C. C. et al. DNA methylation dynamics during B cell maturation underlie a continuum of disease phenotypes in chronic lymphocytic leukemia. Nat. Genet. 48, 253–264 (2016).
Queirós, A. C. et al. A B-cell epigenetic signature defines three biologic subgroups of chronic lymphocytic leukemia with clinical impact. Leukemia 29, 598–605 (2015).
Damle, R. N. et al. Ig V gene mutation status and CD38 expression as novel prognostic indicators in chronic lymphocytic leukemia. Blood 94, 1840–1847 (1999).
Hamblin, T. J., Davis, Z., Gardiner, A., Oscier, D. G. & Stevenson, F. K. Unmutated Ig V(H) genes are associated with a more aggressive form of chronic lymphocytic leukemia. Blood 94, 1848–1854 (1999).
Giacopelli, B. et al. Developmental subtypes assessed by DNA methylation-iPLEX forecast the natural history of chronic lymphocytic leukemia. Blood 134, 688–698 (2019).
Stevenson, F. K., Krysov, S., Davies, A. J., Steele, A. J. & Packham, G. B-cell receptor signaling in chronic lymphocytic leukemia. Blood 118, 4313–4320 (2011).
Ferreira, P. G. et al. Transcriptome characterization by RNA sequencing identifies a major molecular and clinical subdivision in chronic lymphocytic leukemia. Genome Res. 24, 212–226 (2014).
Dietrich, S. et al. Drug-perturbation-based stratification of blood cancer. J. Clin. Invest. 128, 427–445 (2018).
Lu, J. et al. Energy metabolism is co-determined by genetic variants in chronic lymphocytic leukemia and influences drug sensitivity. Haematologica 104, 1830–1840 (2019).
Popp, H. D. et al. Accumulation of DNA damage and alteration of the DNA damage response in monoclonal B-cell lymphocytosis and chronic lymphocytic leukemia. Leuk. Lymphoma 60, 795–804 (2019).
Mallm, J.-P. et al. Linking aberrant chromatin features in chronic lymphocytic leukemia to transcription factor networks. Mol. Syst. Biol. 15, e8339 (2019).
Wan, Y. & Wu, C. J. SF3B1 mutations in chronic lymphocytic leukemia. Blood 121, 4627–4634 (2013).
Puente, X. S. et al. Whole-genome sequencing identifies recurrent mutations in chronic lymphocytic leukaemia. Nature 475, 101–105 (2011).
Landau, D. A. et al. Mutations driving CLL and their evolution in progression and relapse. Nature 526, 525–530 (2015).
Rossi, D. et al. Mutations of NOTCH1 are an independent predictor of survival in chronic lymphocytic leukemia. Blood 119, 521–529 (2012).
Argelaguet, R. et al. Multi-omics factor analysis: a framework for unsupervised integration of multi-omics data sets. Mol. Syst. Biol. 14, e8124 (2018).
Quesada, V. et al. The genomic landscape of chronic lymphocytic leukemia: clinical implications. BMC Med. 11, 124 (2013).
Herold, T. et al. An eight-gene expression signature for the prediction of survival and time to treatment in chronic lymphocytic leukemia. Leukemia 25, 1639–1645 (2011).
Chuang, H.-Y. et al. Subnetwork-based analysis of chronic lymphocytic leukemia identifies pathways that associate with disease progression. Blood 120, 2639–2649 (2012).
Friedman, D. R. et al. A genomic approach to improve prognosis and predict therapeutic response in chronic lymphocytic leukemia. Clin. Cancer Res. 15, 6947–6955 (2009).
Campo, E. et al. TP53 aberrations in chronic lymphocytic leukemia: an overview of the clinical implications of improved diagnostics. Haematologica 103, 1956–1968 (2018).
Wang, L. et al. SF3B1 and other novel cancer genes in chronic lymphocytic leukemia. N. Engl. J. Med. 365, 2497–2506 (2011).
Zenz, T. et al. TP53 mutation and survival in chronic lymphocytic leukemia. J. Clin. Oncol. 28, 4473–4479 (2010).
Fabris, S. et al. Biological and clinical relevance of quantitative global methylation of repetitive DNA sequences in chronic lymphocytic leukemia. Epigenetics 6, 188–194 (2011).
Kulis, M. et al. Epigenomic analysis detects widespread gene-body DNA hypomethylation in chronic lymphocytic leukemia. Nat. Genet. 44, 1236–1242 (2012).
Zhou, W. et al. DNA methylation loss in late-replicating domains is linked to mitotic cell division. Nat. Genet. 50, 591–602 (2018).
Duran-Ferrer, M. et al. The proliferative history shapes the DNA methylome of B-cell tumors and predicts clinical outcome. Nat. Cancer https://doi.org/10.1038/s43018-020-00131-2 (2020).
Feldmann, A. et al. Transcription factor occupancy can mediate active turnover of DNA methylation at regulatory regions. PLoS Genet. 9, e1003994 (2013).
Stadler, M. B. et al. DNA-binding factors shape the mouse methylome at distal regulatory regions. Nature 480, 490–495 (2011).
Heinz, S. et al. Simple combinations of lineage-determining transcription factors prime cis-regulatory elements required for macrophage and B cell identities. Mol. Cell 38, 576–589 (2010).
Krysov, S. et al. Surface IgM stimulation induces MEK1/2-dependent MYC expression in chronic lymphocytic leukemia cells. Blood 119, 170–179 (2012).
Ott, C. J. et al. Enhancer architecture and essential core regulatory circuitry of chronic lymphocytic leukemia. Cancer Cell 34, 982–995 (2018).
Decker, T. et al. Immunostimulatory CpG-oligonucleotides cause proliferation, cytokine production, and an immunogenic phenotype in chronic lymphocytic leukemia B cells. Blood 95, 999–1006 (2000).
Decker, T. et al. Cell cycle progression of chronic lymphocytic leukemia cells is controlled by cyclin D2, cyclin D3, cyclin-dependent kinase (cdk) 4 and the cdk inhibitor p27. Leukemia 16, 327–334 (2002).
Ozer, H. G. et al. BRD4 profiling identifies critical chronic lymphocytic leukemia oncogenic circuits and reveals sensitivity to PLX51107, a novel structurally distinct BET inhibitor. Cancer Discov. 8, 458–477 (2018).
Tarnani, M. et al. The proliferative response to CpG-ODN stimulation predicts PFS, TTT and OS in patients with chronic lymphocytic leukemia. Leuk. Res. 34, 1189–1194 (2010).
Liberzon, A. et al. The Molecular Signatures Database (MSigDB) hallmark gene set collection. Cell Syst. 1, 417–425 (2015).
Wu, D. & Smyth, G. K. CAMERA: a competitive gene set test accounting for inter-gene correlation. Nucleic Acids Res. 40, e133 (2012).
Pascutti, M. F. et al. IL-21 and CD40L signals from autologous T cells can induce antigen-independent proliferation of CLL cells. Blood 122, 3010–3019 (2013).
Vallat, L. et al. Reverse-engineering the genetic circuitry of a cancer cell with predicted intervention in chronic lymphocytic leukemia. Proc. Natl Acad. Sci. USA 110, 459–464 (2013).
Zeller, K. I. et al. Global mapping of c-Myc binding sites and target gene networks in human B cells. Proc. Natl Acad. Sci. USA 103, 17834–17839 (2006).
Attwood, P. V. & Muimo, R. The actions of NME1/NDPK-A and NME2/NDPK-B as protein kinases. Lab. Invest. 98, 283–290 (2018).
Swarnalatha, M., Singh, A. K. & Kumar, V. The epigenetic control of E-box and Myc-dependent chromatin modifications regulate the licensing of lamin B2 origin during cell cycle. Nucleic Acids Res. 40, 9021–9035 (2012).
Agarwal, S. et al. PAICS, a de novo purine biosynthetic enzyme, is overexpressed in pancreatic cancer and is involved in its progression. Transl. Oncol. 13, 100776 (2020).
Coudé, M.-M. et al. BET inhibitor OTX015 targets BRD2 and BRD4 and decreases c-MYC in acute leukemia cells. Oncotarget 6, 17698–17712 (2015).
Vázquez, R. et al. Promising in vivo efficacy of the BET bromodomain inhibitor OTX015/MK-8628 in malignant pleural mesothelioma xenografts. Int. J. Cancer 140, 197–207 (2017).
Waters, L. R., Ahsan, F. M., Wolf, D. M., Shirihai, O. & Teitell, M. A. Initial B cell activation induces metabolic reprogramming and mitochondrial remodeling. iScience 5, 99–109 (2018).
Rath, S. et al. MitoCarta3.0: an updated mitochondrial proteome now with sub-organelle localization and pathway annotations. Nucleic Acids Res. 49, D1541–D1547 (2021).
Morita, M. et al. mTORC1 controls mitochondrial activity and biogenesis through 4E-BP-dependent translational regulation. Cell Metab. 18, 698–711 (2013).
Morrish, F. & Hockenbery, D. MYC and mitochondrial biogenesis. Cold Spring Harb. Perspect. Med. 4, a014225 (2014).
Arif, T., Amsalem, Z. & Shoshan-Barmatz, V. Metabolic reprograming via silencing of mitochondrial VDAC1 expression encourages differentiation of cancer cells. Mol. Ther. Nucleic Acids 17, 24–37 (2019).
Tsai, Y.-P., Teng, S.-C. & Wu, K.-J. Direct regulation of HSP60 expression by c-MYC induces transformation. FEBS Lett. 582, 4083–4088 (2008).
Cheung, R. K. & Utz, P. J. Screening: CyTOF-the next generation of cell detection. Nat. Rev. Rheumatol. 7, 502–503 (2011).
Mognol, G. P., de Araujo-Souza, P. S., Robbs, B. K., Teixeira, L. K. & Viola, J. P. B. Transcriptional regulation of the c-Myc promoter by NFAT1 involves negative and positive NFAT-responsive elements. Cell Cycle 11, 1014–1028 (2012).
Wolf, C. et al. NFATC1 activation by DNA hypomethylation in chronic lymphocytic leukemia correlates with clinical staging and can be inhibited by ibrutinib. Int. J. Cancer 142, 322–333 (2018).
Messmer, B. T. et al. In vivo measurements document the dynamic cellular kinetics of chronic lymphocytic leukemia B cells. J. Clin. Invest. 115, 755–764 (2005).
Giné, E. et al. Expanded and highly active proliferation centers identify a histological subtype of chronic lymphocytic leukemia (‘accelerated’ chronic lymphocytic leukemia) with aggressive clinical behavior. Haematologica 95, 1526–1533 (2010).
Eastel, J. M. et al. Application of NanoString technologies in companion diagnostic development. Expert Rev. Mol. Diagn. 19, 591–598 (2019).
Amon, S. et al. Sensitive quantitative proteomics of human hematopoietic stem and progenitor cells by data-independent acquisition mass spectrometry. Mol. Cell Proteomics 18, 1454–1467 (2019).
Zhang, X. et al. Proteome-wide identification of ubiquitin interactions using UbIA-MS. Nat. Protoc. 13, 530–550 (2018).
Huber, W., von Heydebreck, A., Sültmann, H., Poustka, A. & Vingron, M. Variance stabilization applied to microarray data calibration and to the quantification of differential expression. Bioinformatics 18, S96–S104 (2002).
Love, M. I., Huber, W. & Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 15, 550 (2014).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. R. Stat. Soc. B 57, 289–300 (1995).
Ritchie, M. E. et al. limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 43, e47 (2015).
Korotkevich, G. et al. Fast gene set enrichment analysis. Preprint at bioRxiv https://doi.org/10.1101/060012 (2021).
Maksimovic, J., Phipson, B. & Oshlack, A. A cross-package Bioconductor workflow for analysing methylation array data. Version 3; peer review: 4 approved. F1000Res. 5, 1281 (2016).
Friedman, J., Hastie, T. & Tibshirani, R. Regularization paths for generalized linear models via coordinate descent. J. Stat. Softw. 33, 1–22 (2010).
Zunder, E. R., Lujan, E., Goltsev, Y., Wernig, M. & Nolan, G. P. A continuous molecular roadmap to iPSC reprogramming through progression analysis of single-cell mass cytometry. Cell Stem Cell 16, 323–337 (2015).
Zivanovic, N., Jacobs, A. & Bodenmiller, B. A practical guide to multiplexed mass cytometry. Curr. Top. Microbiol. Immunol. 377, 95–109 (2014).
Behbehani, G. K. et al. Transient partial permeabilization with saponin enables cellular barcoding prior to surface marker staining. Cytometry A 85, 1011–1019 (2014).
Catena, R., Özcan, A., Jacobs, A., Chevrier, S. & Bodenmiller, B. AirLab: a cloud-based platform to manage and share antibody-based single-cell research. Genome Biol. 17, 142 (2016).
Crowell, H. L. et al. An R-based reproducible and user-friendly preprocessing pipeline for CyTOF data. F1000Res. 9, 1263 (2020).
Chevrier, S. et al. Compensation of signal spillover in suspension and imaging mass cytometry. Cell Syst. 6, 612–620 (2018).
Finak, G. et al. OpenCyto: an open source infrastructure for scalable, robust, reproducible, and automated, end-to-end flow cytometry data analysis. PLoS Comput. Biol. 10, e1003806 (2014).
Van Gassen, S. et al. FlowSOM: Using self-organizing maps for visualization and interpretation of cytometry data. Cytometry A 87, 636–645 (2015).
Nowicka, M. et al. CyTOF workflow: differential discovery in high-throughput high-dimensional cytometry datasets. Version 3; peer review: 2 approved. F1000Res. 6, 748 (2017).
Weber, L. M., Nowicka, M., Soneson, C. & Robinson, M. D. diffcyt: differential discovery in high-dimensional cytometry via high-resolution clustering. Commun. Biol. 2, 183 (2019).
Acknowledgements
J. Lu and W. Huber were supported by the European Union (Horizon 2020 project SOUND under grant agreement no. 633974) and the German Federal Ministry of Education and Research (TRANSCAN project GCH-CLL 143 under grant agreement no. 01KT1610 and CompLS project MOFA under grant agreement no. 031L0171A). T. Zenz was supported by the CRPP ‘Next Generation Drug Response Profiling for Personalized Cancer Care’, the Swiss Cancer Research foundation (KFS-4439-02-2018) and the Monique-Dornonville-de-la-Cour Stiftung. D. Mougiakakos was supported by the Deutsche Forschungsgemeinschaft (German Research Foundation, project no. 404074532). F. Nadeu and E. Campo were supported by ‘la Caixa’ Foundation (CLLEvolution-LCF/PR/HR17/52150017, Health Research 2017 Program ‘HR17-00221’, to E.C.). For technical support and expertise, we thank the DKFZ Genomics and Proteomics Core Facility. We thank H. Glimm, S. Fröhling, D. Richter, C. von Kalle, R. Eils, P. Lichter, S. Wolf, K. Beck and J. Kirchhof for infrastructure and program development within DKFZ-HIPO and NCT POP.
Author information
Authors and Affiliations
Contributions
Conceptualization was carried out by W.H., T.Z. and J.L. Experimental design was conducted by T.Z. and E. Cannizzaro. Software, formal analysis and visualization was conducted by J.L. and W.H. Methodology and experimental investigation was conducted by E. Cannizzaro, S.S., P.B., L.W., B.G., S.D., C.O., M.B., D.M., F.M.-A., A.J., B.B., M.M. and I.R. J.L., E. Cannizzaro, W.H. and T.Z. were responsible for writing the manuscript. Data curation was performed by J.L., H.G., J.H., F.N., J.D., E. Campo and A.L. Resources were managed by J.L., J.H. and W.H.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information Nature Cancer thanks Dimitar Efremov and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Integration of multi-omics profiling datasets using multi-omics factor analysis (MOFA).
a, Datasets included in the MOFA training model and the overlap of patient samples among datasets. The number of features in each dataset is indicated by ‘d = ’ and the number of samples in each dataset is indicated by ‘n = ’. b, Stem plots showing the variance explained (R2) values for each view by each factor.
Extended Data Fig. 2 Characterization of the factors identified by MOFA.
a and b, Absolute loadings of the top features of F1 and F2 in the genomic dataset (n = 217 samples). c, Visualization of patient samples using F1 and F2 as coordinates. A dot represents a primary CLL with mutated IGHV status (M-CLL, n = 117 samples), and a circle represents a primary CLL with unmutated IGHV status (U-CLL, n = 89 samples). CLL with (n = 25 samples) and without trisomy 12 (n = 181 samples) are colored by blue and red, respectively. d, Association between F1 and three epigenetic subtypes of CLL: HP (high-programmed, n = 86 samples), IP (intermediate-programmed, n = 35 samples) and LP (low-programmed, n = 86 samples). F1 separated the three epigenetic subtypes in their proper order (HP-, IP- and LP-CLL). e, F3 values for CLL samples in different RNAseq batch (n = 103, 33, 43 and 23 samples for batch 1, 2, 3 and 4, respectively). Each dot represents a patient sample. The boxplot shows the interquartile range in the box with the median as a horizontal line. Whiskers extend to 1.5 times the interquartile range. P value was calculated by ANOVA test. f, Correlations between Factor 5 and the mRNA expression of T cell markers genes: CD4 and CD8A. P values are from two-sided Pearson’s correlation tests. g, Correlations between Factor 6 and the expression of two exemplary genes (SOD1 and GPX4) involved in the response to reactive oxygen species (ROS). P values are from two-sided Pearson’s correlation tests. h, Pathway enrichment results for Factor 6. Enrichment P values were adjusted by Benjamini-Hochberg method. i, Pathway enrichment results for Factor 7. Enrichment P values were adjusted by Benjamini-Hochberg method. Factor 5 and Factor 7 were characterized in detail, under the names of Factor 4 and Factor 5 respectively, in the article describing the implementation of MOFA18. All analysis results shown in panel f - i were performed on RNAseq data from 202 samples.
Extended Data Fig. 3 Associations between Factor 4 and demographic and clinical characteristics.
a, Association of F4 to age. P values are from two-sided Pearson’s correlation test. (n = 217 samples) b and c, Associations of F4 to sex and pretreatment status. P values are from two-sided t-tests. d and e, Kaplan-Meier plots for showing the associations between F4 and TTT or OS in patients without previous treatment. The P-values were assessed by Cox regression models with F4 as a continuous variable. For visualization purposes only, optimal cutoffs to separate patients into high and low CLL–PD groups were estimated by the maximally selected rank test implemented in the R/CRAN package maxstat (v0.7). f and g, Forest plots showing the hazard ratios with 95% confidence intervals and P values from multivariate Cox models that include known demographic and genomic risk factors, for TTT and OS in patients without previous treatment. F4 remained significantly associated with TTT in multivariate analysis. In multivariate analysis for OS, none of the risk factors except for age were significant, however, the hazard ratio showed the same trend for F4 as in the full dataset analysis, consistent with the reduced statistical power of the subset analysis. (n = 154 patients) h, Correlation between F4 and lymphocyte doubling time (LDT) in previously untreated patients. P values and coefficients are from two-sided Pearson’s correlation tests. i, Correlation between F4 and lymphocyte doubling time (LDT) in M/U-CLL separately. P values and coefficients are from two-sided Pearson’s correlation tests. (n = 43 and 40 samples for M-CLL and U-CLL, respectively).
Extended Data Fig. 4 Associations between CLL-PD score and outcomes (TTT or OS) in four external CLL cohorts with gene expression data.
The per-test P-values were calculated by two-sided log-rank tests on Cox regression models with CLL-PD score as a continuous variable. For visualization purposes only, optimal cutoffs to separate patients into high and low CLL-PD groups were estimated by the maximally selected rank test implemented in the R/CRAN package maxstat (v0.7).
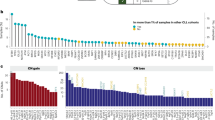
Extended Data Fig. 5 Associations of CLL-PD to genomic aberrations and DNA methylation.
a and b, Scatter plots showing the associations between CLL-PD and the total number of mutations detected by whole exome sequencing (a) or whole genome sequencing (b). Mutations on immunoglobulin genes were excluded when calculating the total number of mutations to avoid potential influence of somatic hypermutation. P values and coefficients were calculated by two-sided Pearson’s correlations tests. c, Associations of the CLL-PD score to genomic aberrations in the ICGC-CLL cohort (n = 249 samples). P values are from two-sided t-tests. d, Associations of the CLL-PD score to overall mutation load in the ICGC-CLL cohort. P value is from two-sided Pearson’s correlation test. e, top 10 enriched transcription factor binding motifs in the regions that show hypomethylation in samples with high CLL-PD values, P values were calculated by the Homer de novo algorithm32.
Extended Data Fig. 6 Gene expression signatures of CLL-PD.
a to c, Heatmap plots showing the z-score of the expression values of genes that are significantly correlated with CLL-PD (1% FDR, Benjamini-Hochberg’s method) and are in the Hallmark MYC targets v1 (a), Hallmark oxidative phosphorylation (OXPHOS) (b) and Hallmark mTORC1 signaling (c) gene sets from Molecular Signatures Database (MSigDB)39. Samples (columns) are ordered by their CLL-PD values. Symbols of the genes coding mitochondrial proteins are colored in red. d, Gene enrichment analysis of genes correlated with the CLL-PD scores in the four external cohorts shown in Fig. 2b, using Hallmark gene sets from MSigDB. The names of gene sets related to MYC targets, mTOR signaling and OXPHOS are colored in red. (n = 249, 107, 130 and 81 patients for the ICGC-CLL, Munich, UCSD and Duke cohorts, respectively) e, Gene set enrichment analysis of genes correlated with CLL-PD in U-CLL (n = 107 samples) and M-CLL (n = 93 samples) separately.
Extended Data Fig. 7 Comparison between the gene expression signatures of CLL-PD and the signatures of pro-proliferative stimuli.
a, GSEA plots showing the enrichment of CLL-PD correlated genes in the gene sets defined on the genes significantly up-regulated by the four indicated pro-proliferative stimuli (1% FDR and log2 fold change >1). b, Gene enrichment analysis of genes differentially regulated after four pro-proliferative microenvironment stimulations: including CpG ODN (ArrayExpress ID: E-GEOD-30105, n = 9 samples), co-culturing with T cells (ArrayExpress ID: E-GEOD-50572, n = 5 samples), IL21 + CD40L (ArrayExpress ID: E-GEOD-50572, n = 4 samples), and cross-linked anti-IgM (ArrayExpress ID: E-GEOD-39411, n = 11 samples). Gene sets that passed a threshold corresponding to an FDR of 5% are shown. The names of gene sets related to MYC targets, mTOR signaling and OXPHOS are colored in red.
Extended Data Fig. 8 Characterization of CLL-PD by proteomic, ex vivo drug response and bioenergetic profiling.
a, Correlations between CLL-PD to the protein levels of three MYC direct targets that are involved in cell proliferation: MCM4, NME1 and PAICS. Per-test P values and coefficients are from two-sided Pearson’s correlation tests (n = 46 samples). b, P values of associations between drug responses and F1 (IGHV), F2 (trisomy 12) and F4 (CLL-PD). P values are from ANOVA tests including F1, F2 and F4 as covariates. Dashed horizontal line indicates the threshold associated with a false discovery rate (FDR) of 5% (method of Benjamini and Hochberg). c, Scatter plots showing the correlations between cell viabilities after drug treatment (averaged over five concentrations tested) and the CLL-PD values. P values were from the same ANOVA test as shown in panel b. Only the drugs that showed significant correlations (5% FDR) are shown here. (panel b and c n = 190 samples): d, Scatter plots showing the associations of CLL-PD to the three bioenergetic features related to oxidative phosphorylation. Per-test P values and coefficients were from two-sided Pearson’s correlation tests (n = 136 samples). e, A heatmap plot showing the z-score of the expression values of proteins that are significantly correlated with CLL-PD (5% FDR, method of Benjamini and Hochberg). Samples (columns) are ordered by their CLL-PD values. The names of mitochondrial proteins are colored in red. f, The correlation between the CLL-PD values of 10 samples and their mitochondrial biomass, analyzed by MitoTracker staining. MitoTracker Green (ThermoFisher Scientific, M7514) was used according to the compound’s manual. P value and coefficient are from two-sided Pearson’s correlation tests. g, Correlations between CLL-PD and the expressions of two mitochondrial marker proteins, VDAC1 and HSPD1 (HSP60). Per-test P values and coefficients are from two-sided Pearson’s correlation tests (n = 46 samples).
Extended Data Fig. 9 Characterization of CLL-PD at single cell level using CyTOF.
a, The same t-SNE layout as shown in Fig. 5b, colored by the scaled intensity the other two proliferation markers, P-Rb and Cyclin B1. b, A volcano plot showing the differentially expressed markers between CLL-PD high and CLL-PD low samples upon CpG ODN treatment. Text label colors indicate pathway: orange—MYC, purple—mTOR, magenta—BCR, black—other. The y-axis shows the per-test P values, which were calculated by differential expression test (based on two-sided moderated t-test) implemented in the diffcyt R package. The dashed horizontal line indicates the threshold associated with a false discovery rate (FDR) of 10% (method of Benjamini and Hochberg) (n = 8 tumor samples for each of the CLL-PD high and low groups).
Extended Data Fig. 10 Illustrations of gating and cell type assignment strategies for flow cytometry and CyTOF analyses.
a, Gating strategy used in the assessment of proliferation by flow cytometry. Debris was excluded by gating the largest events based on the side and forward scatter of cells (SSC-A/FSC-A plot). Single cells were selected based on comparison of FSC-H and FSC-A parameters. Ki67 + /CD19 + double positive cells were gated among all events based on unstained and staining controls conditions (anti-IgG-PE/anti-IgG-PE-Cy5 isotype controls, anti-CD19-PE-Cy5 and anti-Ki67-PE single staining controls). b to g, An illustration of the gating and clustering strategy to annotate cell types in the CyTOF data. b, Intact cells and singlets were gated based on the two DNA channels and the event length channel. c, Intact cells and singlets were clustered using flowSOM, based on the cisplatin (dead) and cleaved PARP/Caspase3 (cl-PARP-Casp) channels. The number of clusters (k = 6) was chosen based on the elbow point of the relative change in area under CDF curve. d, Cells in the cluster that was negative for cisplatin and cl-PARP-Casp (Cluster3) were classified as live cells. Cells in other clusters were classified as dead/apoptotic cells. e, Live cells were clustered into 10 clusters using flowSOM based on the intensity of cell lineage and proliferation markers. f, Cluster 1, which was positive for CD45, MPO and CD14, was annotated as myeloid cell cluster. Cluster 6, 9 and 10, which were positive for CD45 and CD3 or CD7, were annotated as T cell clusters. Cluster 2, 5, 7 and 8, which were positive for CD45 and CD19, were annotated as CLL clusters. Cluster 3 and 4, which were negative for CD45, may represent non-lymphocytic cells or unhealthy cells and therefore were annotated as dead/apoptotic clusters. Among CLL clusters, Cluster 7 and 8, which are positive for all three proliferation markers, Ki-67, P-Rb and Cyclin B1, were annotated as proliferating CLL clusters, and other CLL clusters were annotated as non-proliferating CLL clusters. g, Visualization of cell types on a t-SNE map. Due to their low population size (0.14%), myeloid cells are not apparent.
Supplementary information
Supplementary Tables
Supplementary Tables 1–8
Source data
Source Data Fig. 1
Statistical Source Data for Fig. 1.
Source Data Fig. 2
Statistical Source Data for Fig. 2.
Source Data Fig. 3
Statistical Source Data for Fig. 3.
Source Data Fig. 4
Statistical Source Data for Fig. 4.
Source Data Fig. 5
Statistical Source Data for Fig. 5.
Source Data Extended Data Fig. 1
Statistical Source Data for Extended Data Fig. 1.
Source Data Extended Data Fig. 2
Statistical Source Data for Extended Data Fig. 2.
Source Data Extended Data Fig. 3
Statistical Source Data for Extended Data Fig. 3.
Source Data Extended Data Fig. 4
Statistical Source Data for Extended Data Fig. 4.
Source Data Extended Data Fig. 5
Statistical Source Data for Extended Data Fig. 5.
Source Data Extended Data Fig. 6
Statistical Source Data for Extended Data Fig. 6.
Source Data Extended Data Fig. 7
Statistical Source Data for Extended Data Fig. 7.
Source Data Extended Data Fig. 8
Statistical Source Data for Extended Data Fig. 8.
Source Data Extended Data Fig. 9
Statistical Source Data for Extended Data Fig. 9.
Source Data Extended Data Fig. 10
Statistical Source Data for Extended Data Fig. 10.
Rights and permissions
About this article
Cite this article
Lu, J., Cannizzaro, E., Meier-Abt, F. et al. Multi-omics reveals clinically relevant proliferative drive associated with mTOR-MYC-OXPHOS activity in chronic lymphocytic leukemia. Nat Cancer 2, 853–864 (2021). https://doi.org/10.1038/s43018-021-00216-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43018-021-00216-6
This article is cited by
-
Chronic lymphocytic leukemia patient-derived xenografts recapitulate clonal evolution to Richter transformation
Leukemia (2024)
-
Multimodal data fusion for cancer biomarker discovery with deep learning
Nature Machine Intelligence (2023)
-
SETD2 deficiency accelerates sphingomyelin accumulation and promotes the development of renal cancer
Nature Communications (2023)
-
In-vitro Modulation of mTOR-HIF-1α Axis by TLR7/8 Agonist (Resiquimod) in B-Chronic Lymphocytic Leukemia
Indian Journal of Hematology and Blood Transfusion (2023)
-
Transcriptomic profiles and 5-year results from the randomized CLL14 study of venetoclax plus obinutuzumab versus chlorambucil plus obinutuzumab in chronic lymphocytic leukemia
Nature Communications (2023)