Abstract
Multiagent combination chemotherapy can be curative in acute lymphoblastic leukemia (ALL). Still, patients with primary refractory disease or with relapsed leukemia have a very poor prognosis. Here we integrate an in-depth dissection of the mutational landscape across diagnostic and relapsed pediatric and adult ALL samples with genome-wide CRISPR screen analysis of gene–drug interactions across seven ALL chemotherapy drugs. By combining these analyses, we uncover diagnostic and relapse-specific mutational mechanisms as well as genetic drivers of chemoresistance. Functionally, our data identify common and drug-specific pathways modulating chemotherapy response and underscore the effect of drug combinations in restricting the selection of resistance-driving genetic lesions. In addition, by identifying actionable targets for the reversal of chemotherapy resistance, these analyses open therapeutic opportunities for the treatment of relapse and refractory disease.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
Source data are provided with this paper. All other data supporting the findings of this study are available from the corresponding author on reasonable request. BTCGA data are available from the Broad Institute Firehose platform at http://gdac.broadinstitute.org/; AROMA for SNP6 data preprocessing is available at http://www.aroma-project.org/, raw TCGA data are available from the Cancer Genomics Hub at https://cghub.ucsc.edu/ and the TARGET data matrix is available at https://ocg.cancer.gov/programs/target/data-matrix. Whole-exome and whole-genome sequences have been deposited following the guidelines of the NIH Genomic Data Sharing Policy in the Genotypes and Phenotypes (dbGaP) database with accession numbers phs001072.v1.p1 and phs001951.v1.p1. In addition, all sequencing data are available from the authors. The RNA-seq Sequence Read Archive (SRA) access code is PRJNA534488.
Code availability
Code related to the main figures of the study is available at GitHub at: https://github.com/zjf19870628/Nature_Cancer_2020.
References
Malard, F. & Mohty, M. Acute lymphoblastic leukaemia. Lancet 395, 1146–1162 (2020).
Chan, K. W. Acute lymphoblastic leukemia. Curr. Probl. Pediatr. Adolesc. Health Care 32, 40–49 (2002).
El Fakih, R. et al. Current paradigms in the management of Philadelphia chromosome positive acute lymphoblastic leukemia in adults. Am. J. Hematol. 93, 286–295 (2018).
Pui, C. H. & Evans, W. E. Treatment of acute lymphoblastic leukemia. N. Engl. J. Med. 354, 166–178 (2006).
Bhojwani, D. & Pui, C. H. Relapsed childhood acute lymphoblastic leukaemia. Lancet Oncol. 14, e205–e217 (2013).
Tzoneva, G. et al. Activating mutations in the NT5C2 nucleotidase gene drive chemotherapy resistance in relapsed ALL. Nat. Med. 19, 368–371 (2013).
Meyer, J. A. et al. Relapse-specific mutations in NT5C2 in childhood acute lymphoblastic leukemia. Nat. Genet. 45, 290–294 (2013).
Li, B. et al. Negative feedback-defective PRPS1 mutants drive thiopurine resistance in relapsed childhood ALL. Nat. Med. 21, 563–571 (2015).
Mullighan, C. G. et al. CREBBP mutations in relapsed acute lymphoblastic leukaemia. Nature 471, 235–239 (2011).
Li, B. et al. Therapy-induced mutations drive the genomic landscape of relapsed acute lymphoblastic leukemia. Blood 135, 41–55 (2020).
Dobson, S. M. et al. Relapse-fated latent diagnosis subclones in acute B lineage leukemia are drug tolerant and possess distinct metabolic programs. Cancer Discov. 10, 568–587 (2020).
Oshima, K. et al. Mutational landscape, clonal evolution patterns, and role of RAS mutations in relapsed acute lymphoblastic leukemia. Proc. Natl Acad. Sci. USA 113, 11306–11311 (2016).
Ma, X. et al. Rise and fall of subclones from diagnosis to relapse in pediatric B-acute lymphoblastic leukaemia. Nat. Commun. 6, 6604 (2015).
Mullighan, C. G. Molecular genetics of B-precursor acute lymphoblastic leukemia. J. Clin. Invest. 122, 3407–3415 (2012).
Weng, A. P. et al. Activating mutations of NOTCH1 in human T cell acute lymphoblastic leukemia. Science 306, 269–271 (2004).
Thompson, B. J. et al. The SCFFBW7 ubiquitin ligase complex as a tumor suppressor in T cell leukemia. J. Exp. Med. 204, 1825–1835 (2007).
Van Vlierberghe, P. et al. PHF6 mutations in T-cell acute lymphoblastic leukemia. Nat. Genet. 42, 338–342 (2010).
Tosello, V. et al. WT1 mutations in T-ALL. Blood 114, 1038–1045 (2009).
Della Gatta, G. et al. Reverse engineering of TLX oncogenic transcriptional networks identifies RUNX1 as tumor suppressor in T-ALL. Nat. Med. 18, 436–440 (2012).
De Keersmaecker, K. et al. Exome sequencing identifies mutation in CNOT3 and ribosomal genes RPL5 and RPL10 in T-cell acute lymphoblastic leukemia. Nat. Genet. 45, 186–190 (2013).
Zhang, J. et al. The genetic basis of early T-cell precursor acute lymphoblastic leukaemia. Nature 481, 157–163 (2012).
Hsiao, M. H., Yu, A. L., Yeargin, J., Ku, D. & Haas, M. Nonhereditary p53 mutations in T-cell acute lymphoblastic leukemia are associated with the relapse phase. Blood 83, 2922–2930 (1994).
Kawamura, M. et al. Mutations of the p53 and ras genes in childhood t(1;19)-acute lymphoblastic leukemia. Blood 85, 2546–2552 (1995).
Brown, L. et al. Site-specific recombination of the tal-1 gene is a common occurrence in human T cell leukemia. EMBO J. 9, 3343–3351 (1990).
Mullighan, C. G. et al. Genomic analysis of the clonal origins of relapsed acute lymphoblastic leukemia. Science 322, 1377–1380 (2008).
Greaves, M. F., Maia, A. T., Wiemels, J. L. & Ford, A. M. Leukemia in twins: lessons in natural history. Blood 102, 2321–2333 (2003).
Alexandrov, L. B. et al. Signatures of mutational processes in human cancer. Nature 500, 415–421 (2013).
Mar, B. G. et al. SETD2 alterations impair DNA damage recognition and lead to resistance to chemotherapy in leukemia. Blood 130, 2631–2641 (2017).
Li, J. et al. A gain of function mutation in the NSD2 histone methyltransferase drives glucocorticoid resistance of acute lymphoblastic leukemia. Blood 132, 653–653 (2018).
Bordin, F. et al. WT1 loss attenuates the TP53-induced DNA damage response in T-cell acute lymphoblastic leukemia. Haematologica 103, 266–277 (2018).
Soverini, S. et al. Implications of BCR-ABL1 kinase domain-mediated resistance in chronic myeloid leukemia. Leuk. Res. 38, 10–20 (2014).
Inaba, H., Greaves, M. & Mullighan, C. G. Acute lymphoblastic leukaemia. Lancet 381, 1943–1955 (2013).
Mirski, S. E., Gerlach, J. H. & Cole, S. P. Multidrug resistance in a human small cell lung cancer cell line selected in adriamycin. Cancer Res. 47, 2594–2598 (1987).
Ruel, N. M., Nguyen, K. H., Vilas, G. & Hammond, J. R. Characterization of 6-mercaptopurine transport by the SLC43A3-encoded nucleobase transporter. Mol. Pharmacol. 95, 584–596 (2019).
Moriyama, T. et al. NUDT15 polymorphisms alter thiopurine metabolism and hematopoietic toxicity. Nat. Genet. 48, 367–373 (2016).
Nakamura, A. et al. Inhibition of GCN2 sensitizes ASNS-low cancer cells to asparaginase by disrupting the amino acid response. Proc. Natl Acad. Sci. USA 115, E7776–E7785 (2018).
Bunpo, P. et al. The eIF2 kinase GCN2 is essential for the murine immune system to adapt to amino acid deprivation by asparaginase. J. Nutr. 140, 2020–2027 (2010).
Griffiths, M. et al. Cloning of a human nucleoside transporter implicated in the cellular uptake of adenosine and chemotherapeutic drugs. Nat. Med. 3, 89–93 (1997).
Matherly, L. H. & Goldman, D. I. Membrane transport of folates. Vitam. Horm. 66, 403–456 (2003).
Burgess, D. J. et al. Topoisomerase levels determine chemotherapy response in vitro and in vivo. Proc. Natl Acad. Sci. USA 105, 9053–9058 (2008).
Riccio, A. A., Schellenberg, M. J. & Williams, R. S. Molecular mechanisms of topoisomerase 2 DNA–protein crosslink resolution. Cell. Mol. Life Sci. 77, 81–91 (2020).
Trumpp, A. & Wiestler, O. D. Mechanisms of disease: cancer stem cells—targeting the evil twin. Nat. Clin. Pract. Oncol. 5, 337–347 (2008).
Schroeder, M. P. et al. Integrated analysis of relapsed B-cell precursor acute lymphoblastic leukemia identifies subtype-specific cytokine and metabolic signatures. Sci. Rep. 9, 4188 (2019).
Kankanala, J. et al. Novel deazaflavin analogues potently inhibited tyrosyl DNA phosphodiesterase 2 (TDP2) and strongly sensitized cancer cells toward treatment with topoisomerase II (TOP2) poison etoposide. J. Med. Chem. 62, 4669–4682 (2019).
Numan, Y. et al. First report of clinical response to venetoclax in early T-cell precursor acute lymphoblastic leukemia. JCO Precis. Oncol. 2, PO.18.00127 (2018).
Rahmat, L. T. et al. Venetoclax in combination with decitabine for relapsed T-cell acute lymphoblastic leukemia after allogeneic hematopoietic cell transplant. Case Rep. Hematol. 2018, 6092646 (2018).
Farhadfar, N., Li, Y., May, W. S. & Adams, C. B. Venetoclax and decitabine for treatment of relapsed T-cell acute lymphoblastic leukemia: a case report and review of literature. Hematol. Oncol. Stem Cell Ther. https://doi.org/10.1016/j.hemonc.2019.10.002 (2020).
Guan, Y., Gerhard, B. & Hogge, D. E. Detection, isolation, and stimulation of quiescent primitive leukemic progenitor cells from patients with acute myeloid leukemia (AML). Blood 101, 3142–3149 (2003).
Iwamoto, S., Mihara, K., Downing, J. R., Pui, C. H. & Campana, D. Mesenchymal cells regulate the response of acute lymphoblastic leukemia cells to asparaginase. J. Clin. Invest. 117, 1049–1057 (2007).
Goker, E. et al. Amplification of the dihydrofolate reductase gene is a mechanism of acquired resistance to methotrexate in patients with acute lymphoblastic leukemia and is correlated with p53 gene mutations. Blood 86, 677–684 (1995).
Mar, B. G. et al. Mutations in epigenetic regulators including SETD2 are gained during relapse in paediatric acute lymphoblastic leukaemia. Nat. Commun. 5, 3469 (2014).
Kunz, J. B. et al. Pediatric T-cell lymphoblastic leukemia evolves into relapse by clonal selection, acquisition of mutations and promoter hypomethylation. Haematologica 100, 1442–1450 (2015).
Malinowska-Ozdowy, K. et al. KRAS and CREBBP mutations: a relapse-linked malicious liaison in childhood high hyperdiploid acute lymphoblastic leukemia. Leukemia 29, 1656–1667 (2015).
Waters, T. R. & Swann, P. F. Cytotoxic mechanism of 6-thioguanine: hMutSalpha, the human mismatch binding heterodimer, binds to DNA containing S6-methylthioguanine. Biochemistry 36, 2501–2506 (1997).
Evensen, N. A. et al. MSH6 haploinsufficiency at relapse contributes to the development of thiopurine resistance in pediatric B-lymphoblastic leukemia. Haematologica 103, 830–839 (2018).
Kucab, J. E. et al. A compendium of mutational signatures of environmental agents. Cell 177, 821–836.e816 (2019).
Roberts, K. G. Genetics and prognosis of ALL in children vs adults. Hematology Am. Soc. Hematol. Educ. Program 2018, 137–145 (2018).
Szymanska, B. et al. Pharmacokinetic modeling of an induction regimen for in vivo combined testing of novel drugs against pediatric acute lymphoblastic leukemia xenografts. PloS ONE 7, e33894 (2012).
Schroeter, E. H., Kisslinger, J. A. & Kopan, R. Notch-1 signalling requires ligand-induced proteolytic release of intracellular domain. Nature 393, 382–386 (1998).
Herranz, D. et al. Metabolic reprogramming induces resistance to anti-NOTCH1 therapies in T cell acute lymphoblastic leukemia. Nat. Med. 21, 1182–1189 (2015).
Joung, J. et al. Genome-scale CRISPR–Cas9 knockout and transcriptional activation screening. Nat. Protoc. 12, 828–863 (2017).
Wang, B. et al. Integrative analysis of pooled CRISPR genetic screens using MAGeCKFlute. Nat. Protoc. 14, 756–780 (2019).
Trifonov, V., Pasqualucci, L., Tiacci, E., Falini, B. & Rabadan, R. SAVI: a statistical algorithm for variant frequency identification. BMC Syst. Biol. 7, S2 (2013).
Koboldt, D. C. et al. VarScan 2: somatic mutation and copy number alteration discovery in cancer by exome sequencing. Genome Res. 22, 568–576 (2012).
Gu, Z., Gu, L., Eils, R., Schlesner, M. & Brors, B. circlize implements and enhances circular visualization in R. Bioinformatics 30, 2811–2812 (2014).
Xi, R., Lee, S., Xia, Y., Kim, T.-M. & Park, P. J. Copy number analysis of whole-genome data using BIC-seq2 and its application to detection of cancer susceptibility variants. Nucleic Acids Res. 44, 6274–6286 (2016).
Mermel, C. H. et al. GISTIC2.0 facilitates sensitive and confident localization of the targets of focal somatic copy-number alteration in human cancers. Genome Biol. 12, R41 (2011).
Zairis, S. et al. Moduli spaces of phylogenetic trees describing tumor evolutionary patterns. International Conference on Brain Informatics and Health 8609, 528–539 (Springer, 2014).
Blokzijl, F., Janssen, R., van Boxtel, R. & Cuppen, E. MutationalPatterns: comprehensive genome-wide analysis of mutational processes. Genome Med. 10, 33 (2018).
Haas, B. et al. STAR-Fusion: fast and accurate fusion transcript detection from RNA-Seq. Preprint at https://www.biorxiv.org/content/10.1101/120295v1, 120295 (2017).
Acknowledgements
This work was supported by the University of Minnesota Academic Health Center Faculty Research Development Grant (Z.W.); the Leukemia & Lymphoma Society Quest for Cures Award no. 8011-18 (A.F.); an Innovative Research Award and a Phillip A. Sharp Innovation in Collaboration Award by Stand Up to Cancer (A.F.); the St. Baldrick’s Foundation (A.F.); the Chemotherapy Foundation (A.F.); the Swim Across America Foundation (A.F.); a Crazy 8 Pilot Project Award from the Alex Lemonade Stand Foundation (A.F.); the NIH grants no. P30 CA013696 (Genomics and High Throughput Screen Shared Resource, Flow Cytometry Shared Resource, Oncology Precision Therapeutics Shared Resource), no. R35 CA210065 (A.F.), no. R01 CA206501 (A.F.), no. R01 CA185486 (R.R.), no. R01 CA179044 (R.R.), no. U54 CA121852 (R.R.), no. CA180827 (E.P.), no. CA196172 (E.P.), no. CA180820 (ECOG-ACRIN), no. CA189859 (ECOG-ACRIN), no. CA14958 (ECOG-ACRIN), no. CA180791 (ECOG-ACRIN), no. CA17145 (ECOG-ACRIN), no. U10 CA180827 (ECOG-ACRIN), no. CA233332 (ECOG-ACRIN), no. U10 CA180886 (M.L.L.), no. U10 CA98413 (M.L.L.), no. U10 CA180899 (M.L.L.), no. U24 CA114766 (M.L.L.), no. U24-CA196173 (M.L.L.), and no. U10 CA98543 (J.M.G.-F., M.L.L.); the Human Specimen Banking Grant no. U24 CA114766 (J.M.G.-F.); and the Stewart Foundation (R.R.). K.O. is a Rally Foundation fellow. J.A.B. is the Candy and William Raveis Fellow of the Damon Runyon-Sohn Foundation Pediatric Cancer Fellowship Award (grant no. DRSG-31-19).
Author information
Authors and Affiliations
Contributions
K.O. performed validation, recurrence mutation analysis, CRISPR screens and functional assays, and wrote the original manuscript. J.Z. analyzed Illumina sequence data, clonality and copy number variations. P.P.-D. performed CRISPR screen analyses and experimental therapeutics in vivo experiments. J.A.B. did functional experiments, and wrote, edited and revised the manuscript. J.A.P.-G. and T.C. performed molecular clock analyses. A.A.-I. and A.Q. performed bioinformatic analyses on exome and RNA-seq data. L.B. and T.G. did functional experiments. V.T. contributed to xenograft analyses. Z.W. developed and provided the ZW1231 TDP2 inhibitor. M.L.S., M.K., K.K., M.P., G.B., M.B., C.N., J.M.G.-F., M.D., M.L.L., E.P., M.S.T., J.M.R., M.L., M.D.M. and J.M. contributed clinical samples and correlative clinical and molecular data. R.R. directed and supervised the analysis of genomic sequencing data. A.F. designed the study, directed and supervised research, and wrote, edited and revised the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Genomic profiling of diagnostic and relapsed ALL samples.
Number of mutations identified in the diagnosis and relapse adult and pediatric ALL samples (n= 27 adult; 148 pediatric.). Transitions are indicated in blue bars. Transversions are indicated in black bars.
Extended Data Fig. 2 Mutational profiles of diagnosis and relapsed ALL.
Bar graphs indicate the relative contribution of mutational profiles in diagnosis and relapsed ALL patient samples (n=50).
Extended Data Fig. 3 Mutational signatures of diagnosis and relapsed ALL samples.
The percentage contribution of mutational signatures in diagnosis (blue, n=49 patients) and relapsed (red, n=49 patients) ALL samples represented as violin plots. Violin plots use median as the centre measure with the 1st quantile and 3rd quantile as the bottom and top boundary, respectively, of the plot.
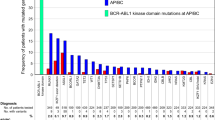
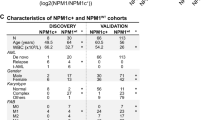
Extended Data Fig. 4 Schematics of the protein structures showing mutations recurrently identified in diagnostic and relapse ALL samples.
Proteins involved in chemotherapy resistance and signaling are represented. Black circles indicate amino acid substitutions. Red circles indicate truncating mutations. TAD, transactivation domain; HAD haloacid dehalogenase domain; SB, substrate binding; Zn, zinc finger domain; LBD, ligand binding domain; P, P loop domain; SWI, Switch I domain; SWII, Switch II domain; HVR, hypervariable region domain; FERM, 4.1 protein Ezrin Radixin Moesin domain; SH2 like, Src homology 2 like domain; FZ, Frizzled domain; GPCR, GPCR family 2-like; Ig, Immunoglobulin; PTPase, Tyrosine specific protein phosphatases domain; HEAT, Huntingtin, EF3A, ATM, TOR; FAT, Frap, ATM, TRRAP; FRB, FKBP-rapamycin complex binding; RD, regulatory domain; FATC, FAT C-terminal; B41, Band 4.1 homologues; PH-like, Pleckstrin homology-like; EGF like, epidermal growth factor like domain repeats; LNR, Lin12-Notch repeats; HD, heterodimerization domain; TM, transmembrane region; RAM, Rbp-associated molecule domain; ANK, ankyrin repeats; PEST, proline (P), glutamic acid (E), serine (S), and threonine (T) domain; FN3, Fibronectin type III; OD, oligomerization domain; SH3, Src homology 3 domain; FABD, F-actin binding domain.
Extended Data Fig. 5 Schematics of the protein structures showing mutations recurrently identified in diagnostic and relapse ALL samples.
Proteins involved in epigenetic regulation and other recurrently mutated factors are represented. Black circles indicate amino acid substitutions. Red circles indicate truncating mutations. TAZ, TAZ zinc finger; KIX, kinase-inducible domain interacting domain; Bromo, bromodomain; HAT, histone acetyl transferase domain; PWWP, proline (P) tryptophan (W) tryptophan (W) proline (P) domain; HMG, high mobility group domain; PHD, plant homeodomain; SET, Su(var)3-9 Enhancer of zeste and Trithorax domain; AWS, associated with SET; SRI, Set2 Rpb1 interacting; MED12, Mediator complex, subunit Med12; FYRN, FY-rich domain N-terminal; UBL, ubiquitin like domain; USP, ubiquitin specific protease domain; ITD, ion transport domain; PH, pleckstrin homology; GED, GTPase effector domain; PRD, proline/arginine-rich domain; Neur_chan_LBD, Neurotransmitter-gated ion-channel ligand binding domain; LIC, Cation transporter family protein; Neur_chan_memb, Neurotransmitter-gated ion-channel transmembrane region; TRAF, tumor necrosis factor-receptor associated factor; HUBL, HAUSP/USP7 ubiquitin-like domain; FN3_D, Fibronectin type III-like domain; SEFIR, SEF/IL-17R; Myc_N, Myc amino-terminal region; HLH, Helix-loop-helix; LZ, leucine zipper; Jmjc, Jumonji C.
Extended Data Fig. 6 Copy number alterations in diagnostic and relapse ALL samples.
Human chromosomal ideograms showing the areas of genetic gain and loss identified by whole exome sequencing, whole genome sequencing or Genome-Wide Human SNP Array 6.0 (Affymetrix) in 103 B-precursor ALL samples and 46 T-cell ALL samples at diagnosis and relapse (rel). Green bars represent areas of loss. Red bars represent areas of gain.
Extended Data Fig. 7 GISTIC analysis of recurrent Copy number alterations in diagnostic and relapse ALL samples.
GISTIC qplots of 149 diagnosis and relapse ALL samples. Copy number segmentation files were generated by EXCAVATOR base on Whole Exome Sequencing data, BIC-seq2 for whole genome sequencing or Genome-Wide Human SNP Array 6.0 (Affymetrix). The resulting seg files (genomic intervals), together with the union of whole exome probes from different platform were used in GISTIC version 2.0.22.
Extended Data Fig. 8 Clonal evolution profiles in relapsed ALL.
Evolutionary trees of 49 matched diagnosis and relapse samples evaluated by whole-genome sequencing. The lengths of the branches in the evolutionary tree graph indicate the number of shared (orange), diagnosis-specific (blue) and relapse-specific (red) genetic alterations in each sample. We used the variant allele frequency cutoff >= 20%.
Supplementary information
Supplementary Tables
Supplementary Tables 1–8
Supplementary Data
Gating strategy for flow cytometry experiments
Source data
Source Data Fig. 4
Unprocessed western blots for Fig. 4.
Source Data Fig. 4
Statistical source data for Fig. 4.
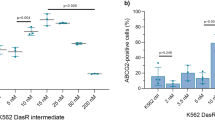
Source Data Fig. 5
Statistical source data for Fig. 5.
Source Data Fig. 5
Unprocessed western blots for Fig. 5.
Source Data Fig. 6
Statistical source data for Fig. 6.
Rights and permissions
About this article
Cite this article
Oshima, K., Zhao, J., Pérez-Durán, P. et al. Mutational and functional genetics mapping of chemotherapy resistance mechanisms in relapsed acute lymphoblastic leukemia. Nat Cancer 1, 1113–1127 (2020). https://doi.org/10.1038/s43018-020-00124-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43018-020-00124-1
This article is cited by
-
CRISPR screening in hematology research: from bulk to single-cell level
Journal of Hematology & Oncology (2023)
-
Knockout KHDRBS3 inhibits cell proliferation and glucocorticoid resistance in acute lymphoblastic leukemia
Molecular & Cellular Toxicology (2023)
-
Targeting pan-essential pathways in cancer with cytotoxic chemotherapy: challenges and opportunities
Cancer Chemotherapy and Pharmacology (2023)
-
Phosphoproteomic profiling of T cell acute lymphoblastic leukemia reveals targetable kinases and combination treatment strategies
Nature Communications (2022)
-
mTOR inhibition attenuates chemosensitivity through the induction of chemotherapy resistant persisters
Nature Communications (2022)