Abstract
Plants, animals and humans metabolically produce volatile isoprene (C5H8). Humans continuously exhale isoprene and exhaled concentrations differ under various physio-metabolic and pathophysiological conditions. Yet unknown metabolic origin hinders isoprene to reach clinical practice as a biomarker. Screening 2000 individuals from consecutive mass-spectrometric studies, we herein identify five healthy German adults without exhaled isoprene. Whole exome sequencing in these adults reveals only one shared homozygous (European prevalence: <1%) IDI2 stop-gain mutation, which causes losses of enzyme active site and Mg2+–cofactor binding sites. Consequently, the conversion of isopentenyl diphosphate to dimethylallyl diphosphate (DMAPP) as part of the cholesterol metabolism is prevented in these adults. Targeted sequencing depicts that the IDI2 rs1044261 variant (p.Trp144Stop) is heterozygous in isoprene deficient blood-relatives and absent in unrelated isoprene normal adults. Wild-type IDI1 and cholesterol metabolism related serological parameters are normal in all adults. IDI2 determines isoprene production as only DMAPP sources isoprene and unlike plants, humans lack isoprene synthase and its enzyme homologue. Human IDI2 is expressed only in skeletal-myocellular peroxisomes and instant spikes in isoprene exhalation during muscle activity underpins its origin from muscular lipolytic cholesterol metabolism. Our findings translate isoprene as a clinically interpretable breath biomarker towards potential applications in human medicine.
Similar content being viewed by others
Introduction
Isoprene (2-methyl 1,3-butadiene; C5H8) is an omnipresent and the most abundant hemiterpene in our planet’s atmosphere1,2, Isoprene is globally produced by vegetation and along with its chiral monoterpenes (e.g., alpha pinene) acts as predictor for ecosystem fluxes3, forest emissions and drought response4, environmental pollution5, cloud chemistry6, and climate change7. Besides being abundantly emitted via the de novo emission pathway in plants8, isoprene is also endogenously produced by animals and humans.
The C5 isoprene unit is the basic building block for terpenoid including steroid hormones biosynthesis that has been biologically essential for ubiquitous terrestrial life forms since billions of years in the course of evolution9. It is the second most abundant and endogenous volatile organic compound (VOC) in our exhaled breath10. Exhaled concentrations range between 80 and 300 ppbV in healthy adults. In 1960, mass-spectrometric techniques had detected the presence of exhaled isoprene, which was later quantified by Jansson et al.11,12 Though the evolutionary significance of isoprene production and biological function are not well understood in humans. differences/dynamics in its exhaled alveolar concentrations are well reported as potential markers for various physiological, metabolic, and pathophysiological effects. While any kind of muscle activity/exercise immediately spikes its expression13,14, studies have reported differential breath profiles and significant concentration changes under conditions such as cardio-respiratory diseases15,16,17, hypercholesteremia18, oxidative stress19, cancers20,21, sexual arousal22, and ageing23,24,25. Despite such interesting observations, the clinical translation of isoprene as a routine biomarker is hindered due to the uncertainty upon its exact metabolic origin.
Surprisingly, while significant deficiency or absence of non-sterol C5H8 is reported in cases with inherited diseases like mevalonic aciduria, hyper immunoglobulinemia D syndrome, autoinflammatory periodic fever26,27,28 and Duchenne muscle dystrophy29, there are rare (<0.3% population prevalence) adults living healthy lives without (absence) exhaling any traceable isoprene and exhaling very low (deficiency) concentrations of isoprene30. Existence of an isoprene absent adult was first reported by Gelmont et al.31 Since then, only a few pilot studies have randomly reported the presence of breath isoprene absent healthy subjects and in 2021, we have first approximated the actual rare genetic occurrence of this character by screening in a large cohort of 1026 humans30. Such breath isoprene aberrated healthy adults may hold the fundamental key to its true origin in human breath30.
While looking at the physio-metabolic aspects, the increase in isoprene exhalation at the beginning of exercise was first reported by Jordan et al.32 Miekisch et al. first postulated the peripheral source of isoprene by measuring blood isoprene from vascular compartments of mechanically ventilated pigs33. Turner et al. found one isoprene deficient healthy adult34. While compared to isoprene normal adults, no correlations were seen between isoprene exhalation and fasting blood cholesterol profiles. King et al. also predicted its extrahepatic endogenous production via physiological modeling of exhaled isoprene dynamics35. The model reasonably explained the exercise driven immediate increase in breath isoprene. King et al. observed reduced (by a factor ≧8, while compared to healthy adults) levels of blood and breath isoprene in five late state muscle dystrophy patients and thereby, postulated its possible production in muscle29. Unterkofler et al. applied a two compartmental model to establish connection between endogenous production and metabolism of systemic VOCs and demonstrated that inhaled deuterated isoprene-D5 does not exhibit a peak at the beginning of exercise36. Although, we have reported pronounced effects of peripheral vasoconstrictions (in muscular compartments) during standing37, while wearing medical face-masks38 and also effects of natural menstrual cycle and daily oral contraceptive pills39 on exhaled isoprene profiles, actual down-stream analysis to confirm the true origin in human and metabolic source of breath isoprene was completely missing. Recently, we executed breathomics, lipid profiling and gene expression analyses in an isoprene absent rare German adult and her isoprene deficient parents and sibling sister. Outcomes depicted no aberration in cholesterol levels and/or in gene expression of the mevalonate pathway enzymes and indicated a recessive inheritance of this healthy character30. Therefore, we questioned the putative human origin (hepatic cholesterogenesis) of exhaled isoprene that was proposed by Deneris et al. based on in vitro experiments in rat liver cells40. Nevertheless, a single rare case was insufficient for detailed down-stream multi-omic analysis to determine the exact source. In a recent case study on one isoprene deficient American adult male and his blood-relatives by Harshman et al.41 and in another study on an isoprene deficient Italian adult female and her blood-relatives by Biagini et al.42 also demonstrated no relation of exhaled isoprene profiles to plasma cholesterol levels. They neither find any isoprene absent rare adult nor investigated the human cholesterol metabolism related gene expressions.
As a continuation of our precedent down-stream observations in the isoprene aberrated family30, we conducted untargeted breathomics in clinical screening scenarios and discovered four more isoprene absent healthy German adults. Thus, to determine the exact metabolic origin, we have now performed multi-omic investigations involving, whole exome sequencing, breathomics and relevant serological analyses in these five rare adults (amongst 2000 recruited subjects) along with targeted sequencing of lead variants in blood-related isoprene deficient and unrelated isoprene normal healthy German adults. Our findings revealed only one shared homozygous (<1% prevalent in Europeans) IDI2 stop-gain mutation (at c.431 position) causing loss of enzyme active site and magnesium ion–cofactor binding sites in the isoprene absent adults. This prevented the conversion of isopentenyl diphosphate to dimethylallyl diphosphate (DMAPP) in cholesterol metabolism pathway. The IDI2 variant turned out to be heterozygous in isoprene deficient blood-relatives and absent in unrelated isoprene normal adults. Wild-type IDI1 and cholesterol metabolism related serological parameters were normal in all adults. Unlike other mammals, naturally IDI2 knocked-out pigs and bottlenose dolphins do not exhale isoprene. In humans, IDI1 is expressed highly in liver but the hepatocellular cytochrome-P450 enzymes immediately oxidizes isoprene. Skeletal muscles metabolize lipids (oxidize fatty acids, cholesterol) to produce energy, regulate intramyocellular signaling and integrity. Peroxisomes are metabolic organelle—mainly responsible for lipolysis. Peroxisomal beta-oxidation produces acetyl-CoA, i.e., channelled towards DMAPP production. Thus, human IDI2 determines isoprene production as DMAPP is the only source of isoprene and unlike plants, humans do not have isoprene synthase and its enzyme homologue. In humans, IDI2 is only expressed in skeletal-myocellular peroxisomes and instant spikes in isoprene exhalation during any muscle activity confirm the origin from muscular lipolytic cholesterol metabolism. We discovered the genetic origin of human isoprene production and related biochemical routes. We translated isoprene as the first breath VOC biomarker with well-defined endogenous origins and metabolic pathways. This knowledge will redefine clinical interpretations and applications of this non-invasive metabolic biomarker for various physio-metabolic and pathophysiological conditions.
Results
Distribution of exhaled alveolar and inhaled isoprene concentrations
Out of 2000 recruitments from clinical screenings, we obtained only five (3 females and 2 males) isoprene absent healthy adults (i.e., rare with <0.03% prevalence), 64 (39 females and 25 males) isoprene deficient (with low exhaled concentrations <50 ppbV) adults and 1318 (687 females and 631 males) isoprene normal (i.e., exhaled concentrations >50 ppbV) adults aged between 20 and 60 years. Besides, we obtained 345 (158 females and 187 males) subjects aged between 01 and 19 years and 268 (196 females and 72 males) subjects aged between 61 and 90 years. Correlations between biological age (year) and exhaled isoprene concentrations (ppbV) are presented in Supplementary Table 1.
Figure 1 represents the distribution of exhaled alveolar and inhaled room air concentrations (ppbV) of isoprene measured via real-time PTR-ToF-MS from 2000 recruited subjects. Exhaled isoprene concentrations are also presented within different age groups and subgroups. Statistically significant (p-value ≤ 0.005) differences between groups with respect to isoprene normal adults are indicated via green colored ‘*’ and corresponding p-values are presented in Supplementary Table 2. Numerical source data on exhaled alveolar (room-air deducted) isoprene concentrations are presented in Supplementary Data 1.
Y-axis represents isoprene concentrations (ppbV). X-axis represents the total number of recruitments (n = 2000) along with different age groups/subgroups (with corresponding number of screened subjects) and total number of inspiratory samples (n = 2000). The adult group (aged 20–60 years) is sub-grouped into three colored boxes viz. isoprene normal (n = 1320; exhaled isoprene concentrations >50 ppbV), isoprene deficient (n = 64; concentrations <50 ppbV) and isoprene absent healthy (n = 5), respectively. Statistical significances of differences in isoprene concentrations between different age groups/subgroups were tested by means of one-way ANOVA on ranks (p-value ≤ 0.005). From all pairwise-multiple comparisons, statistically significant differences with respect to ‘isoprene normal adults’ are marked with green-colored ‘*’. The group containing the ‘total recruited subjects’ was not compared statistically to avoid overlaps of exhaled isoprene concentrations from different age groups and subgroups.
Exhaled alveolar (corresponding room air deducted) isoprene concentrations (mean ± SD) in subjects aged <20 years, isoprene normal adults, isoprene deficient adults, isoprene absent adults and subjects aged >60 years were 86.51 ± 59.80 ppbV, 150.24 ± 65.13 ppbV, 35.27 ± 10.33 ppbV, −12.23 ± 0.91 ppbV (corresponds to 0.00 ppbV in breath, i.e., below LLOD and LLOQ) and 105.03 ± 49.70 ppbV, respectively. Room air concentrations were 3.80 ± 3.74 ppbV. The group of young subjects (aged <20 years) had significantly (p-value < 0.001) lower isoprene levels than the group of seniors (aged >60 years).
Exhaled alveolar isoprene concentrations (corresponding room air subtracted) in rare adult-1’s father (aged 60 years, German), mother (aged 60 years, German) and sibling sister (aged 30 years, German) were 15.86 ppbV, 17.54 ppbV and 27.24 ppbV, respectively. These three adults were isoprene deficient and healthy. Previous serological investigations showed normal lipid profiles in them30.
Demographic, serological, and breathomic parameters from rare adults
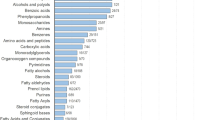
Demographic data (age, gender, ethnic origin, health status and lifestyle habits), relevant serological parameters (viz. plasma lipid profile, bile metabolites and sex hormones) and exhaled concentrations of prime endogenous and exogenous VOCs from the five isoprene absent adults are presented in Table 1.
No considerable serological aberration was found in the rare adults. Exhaled endogenous VOCs (except isoprene) were also within the expected normal ranges. Exhaled exogenous VOCs were mainly related to lifestyle habits.
Filtering strategies for the identification of candidate mutations
Figure 2 represents the filtering strategies for the identification of candidate mutations following whole exome sequencing of isoprene-absent healthy German adults (n = 5) identifying heterozygous and homozygous variants across all known gene and protein coding regions. The filtering strategy for the detection of rare homozygous deleterious variants shared by all individuals are presented in 2a. Throughout the exome, over 63,000 variants passed the upstream bioinformatics pipeline to secure sufficient data quality and were present in at least one of the five isoprene-absent adults. As a recessive mode of inheritance was suspected, we next filtered for homozygous variants, resulting in roughly 25,000 remaining candidate variants. To justify biological significance, we only included mutations that resulted in changes on amino acid level, including frameshift, missense, nonsense or in-del variants, lowering the number of potential candidates to around 9000. Knowing roughly the frequency of the investigated character (5 homozygotes out of 2000), we aimed to exclude variants with a reported population frequency of 15% or higher, being tantamount to roughly 1% homozygotes. Finally, out of those 556 rare homozygous variants, only one (IDI2, c.431 G > A) was shared by all five isoprene-absent adults. The detected mutation is listed in dbSNP (rs1044261) but no association towards isoprene metabolism was mentioned so far.
a Filtering strategy for the detection of rare homozygous deleterious variants shared by all individuals. b Filtering strategy for the characterization of variants located within the mevalonate arm of cholesterol biosynthesis and steroid hormone metabolism. including ACAT2, HMGCS1, HMGCR, MVK, PMVK, MVD, IDI1, IDI2, FDPS1, GGPS1, FDFT1, SQLE, LSS, and DHCR7.
We further investigated if there are any heterozygous variants located within the mevalonate arm of cholesterol biosynthesis and steroid hormone metabolism pathway that might be related to the character (Fig. 2b). Again, out of the roughly 63,000 variants that passed upstream quality assessment, over 25,000 mutations resulted in frameshift, in-del, nonsense or missense mutations. We then analyzed the pathway genes ACAT2, HMGCS1, HMGCR, MVK, PMVK, MVD, IDI1, IDI2, FDPS1, GGPS1, FDFT1, SQLE, LSS and DHCR7, resulting in 12 variants that are present in at least one of the isoprene-absent adults. The above-listed genes are step-wise converting acetyl-CoA to cholesterol. However, no additional mutation was shared by all cases, except for an FDFT1 variant that is very common in the European population and can therefore be excluded. Corresponding amino acids, variants, impact, variant allele frequencies and prevalence (%) of homozygous and heterozygous variants in the European population (based on gnomAD) are presented in Table 1.
Bidirectional targeted sequencing of the IDI2 mutational site
We next aimed to investigate the inheritance pattern of the IDI2 c.431 G > A variant. Therefore, confirmatory targeted bidirectional Sanger sequencing was performed for all isoprene absent adults (Fig. 3). As expected, the results demonstrated a homozygous mutation in the respective position in all isoprene-absent specimens, confirming the previous whole exome sequencing findings. Family members of isoprene absent adult-1, who demonstrated <30 ppbV of isoprene in exhaled breath, were also checked, revealing a heterozygous IDI2 genotype in her mother, father and sibling sister. Two unrelated healthy adults with normal isoprene profiles were sequenced as controls. Those control participants did not show the IDI2 c.431 G > A variant, neither homozygous nor heterozygous.
Sanger sequencing chromatograms using forward (left) and reverse (right) primers to analyze the IDI2 c.431 position. DNA nucleotide bases are assigned as A, T, G and C and are presented with green, red, black and blue colored peaks. respectively. Isoprene absent rare adults (1–5) demonstrate homozygosity while blood-related family members (isoprene deficient) of rare adult 1 were confirmed heterozygous. The mutation is absent in unrelated adult controls. Red boxes indicate the variant genomic site c.431.
IDI2 gene and protein structure
We finally interrogated the UCSC Genome Browser and UniProt databases to elucidate the biological significance of the detected IDI2 c.431 G > A variant. The IDI2 gene is located on the short arm of chromosome 10 and consists of five exons, with coding sequences in exons two to five (Fig. 4a). The mutation of interest is located at the beginning of exon five and results in a stop gain at p.W144*, accounting for a truncated mRNA (Fig. 4a). This genomic area is highly conserved, indicating a crucial and ubiquitous role of the transcriptional site.
a, b The gene structure was retrieved from the UCSC Genome Browser website (http://genome.ucsc.edu) using the GRCh38/hg38 assembly. a The full gene structure of IDI2 with the site of the c.431 G > A point mutation marked in orange. b Enlargement of the IDI2 exon 5 coding regions. c, d The IDI2 protein structure was retrieved from the UniProt database (http://uniprot.org) and the area of the hydrolase domain was added in blue. The deleted protein region following the p.W144* mutation is marked in red. Enzyme active sites and binding sites are depicted as black boxes and green circles. respectively. c Full protein structure. d Enlargement of amino acids 118–164. including the mutation site marked with a red box.
The wild-type IDI2 protein spans 227 amino acids (aa), with a large hydrolase domain spanning aa 49 to 199 (Fig. 4c). There are two active sites of the enzyme, one at the N-terminus of the hydrolase domain and the other one at aa 148, only four aa downstream from the detected p.W144* variant (Fig. 4d). Due to the truncated mRNA transcript, the second enzyme active site is deleted in the five individuals sharing the c.431 G > A mutation, likely resulting in impaired or absent protein function. In addition, the loss of the C-terminal part of IDI2 exon 5 also results in the deletion of two out of four magnesium binding sites, which is a required cofactor for the enzyme’s function.
Discussion
For the last 39 years, many have erroneously regarded hepatic cholesterogenesis (producing >90% of human cholesterol) as the prime origin of human exhaled isoprene. This believe was based on in vitro synthesis of isoprene from DL-mevalonate by utilizing a rat liver cytosolic fraction40. Consequently, various physio-metabolic and clinical conditions driven interesting differences (cross-sectional) and/or changes (longitudinal) in isoprene exhalation could not be explained via the well-known/established effects of those conditions on hepatic cholesterogenesis. As a result, breath isoprene could not step into routine clinical practice as a noninvasive biomarker. However, articles by Miekisch et al.33, Turner et al.34, and King et al.35 indicated extrahepatic production of this VOC and physiological modeling approaches under exercise hinted toward a probable muscular origin29,36. Despite a few studies reported the rare presence of isoprene absent adults25,31,34,40,41,42,43, until 2021, there was no down-stream evidence available to completely disregard the convention. In 2021, we finally disqualified the putative origin of breath isoprene30 and here, we have discovered the actual origin of human exhaled C5H8 by multi-omic analysis of genes and metabolites.
Distribution of exhaled isoprene concentrations from 2000 screened subjects reconfirmed previously reported age dependency23,24,25,30 of its exhalation. Complete absence of exhaled isoprene in the rare adults is caused by the shared homozygous IDI2 variant (stop-gain mutation at c.431 position). This mutation was the only variant in whole exome sequencing that was present in all specimens and met inclusion criteria. Functional aberrations of the enzyme active site and metal–cofactor binding sites likely arise through this mutation. Looking at the isoprene exhalation in our previous study30, we assumed that the inheritance of the character (isoprene absence) has a recessive trait. Here, the heterozygous presence of the IDI2 c.431 G > A variant in the isoprene deficient healthy parents and sibling sister of rare adult-1 and absence of this IDI2 mutation in unrelated healthy adults (isoprene normal) genetically confirmed our previous assumptions. It is possible, that a certain number of subjects from our clinical studies were first- or second-degree relatives. As per ethical obligations, we were not allowed to use/disclose such non-anonymous/identifiable information and/or to look for relationships between participants during their recruitments in clinical screening studies. Therefore, we did not consider such information during data analysis in our present study. Within this study, we were allowed to contact (only via formal letters of invitation) the adult family members of the isoprene absent adults. At the best of our knowledge, the five isoprene absent adults were unrelated to each other. Except the presented family members of the isoprene absent adult-1, no other blood relatives of the remaining rare adults were involved within this study.
In this study, the prevalence (<0.25%) of isoprene absent adults closely mirrored the actual homozygous prevalence (0.23%) of the IDI2 rs1044261 variant (p.Trp144Stop) in the EU population. A broader approach of parallel IDI2 sequencing in combination with breath analysis, however, is necessary to definitely confirm the relation between the amount of exhaled isoprene and IDI2 genotype. Nevertheless, such approach is considerably resource demanding in a large scale and remained beyond our immediate aim and present resource capacity. The overall expression (homozygous and heterozygous) of the mutated IDI2 is different in other ethnic origins (Supplementary Table 3) and therefore, the observed age distributions of isoprene, deficiency and/or absence may differ amongst another ethnicity/population. Besides, the cut-off limit of isoprene deficiency in adults was set by us to < 50 ppbV to define a clear cut-off beyond the inter-individual and physiological variations (normal range of exhaled isoprene 80–350 ppbV). Exhaled isoprene concentrations may vary by 5–25 ppbV in an individual simply due to his/her normal physiological variations in respiratory and hemodynamic parameters, natural menstrual rhythms and/or oral contraception and menopause23,37,39,44 etc. Therefore, the cut-off <50 ppbV allowed us to determine the clearly isoprene deficient adults—beyond his/her physio-metabolic fluctuations.
While the expression of human IDI1 is conserved in various tissues and high within the mitochondria and proteasome of the hepatocytes, its divergent isoform IDI2 is highly expressed only within the peroxisome of the skeletal myocytes45,46. Human IDI1 is poorly expressed in skeletal muscle. IDI1 and/or IDI2 catalyze the isomerization of isopentenyl diphosphate [(C14)IPP] to the highly nucleophilic dimethylallyl diphosphate [(C14)DMAPP]. In humans, the conversion of IPP to DMAPP takes place in two metabolic paths— during cholesterol biosynthesis in the endoplasmic reticulum of hepatocytes and during lipid catabolism (involving cholesterol metabolism) in the peroxisome of skeletal myocytes47,48. Only DMAPP (not IPP) is converted to C5H8 via isoprene synthase (IspS) enzyme in plants49,50,51. As humans do not have isoprene synthase and bioinformatic sequence alignment (whole exome/functional domain based) via BLAST search tool52 did not locate human enzyme homologs of isoprene synthase, the wild-type IDI1 and IDI2 genes (and related proteins) should serve as the determinant for human isoprene production from those two aforementioned metabolic paths.
Besides humans, while looking at other terrestrial and marine mammals, we observed interesting facts upon breath isoprene. In a recent pre-clinical study, mass-spectrometry based untargeted profiling of exhaled VOCs in spontaneously breathing awake healthy and/or influenza A virus infected pigs, we could not detect breath isoprene53. On the other hand, in pre-clinical breathomic studies on goats and on cattle, we observed significant concentrations of breath isoprene from both ruminants54,55. Via mass-spectrometry based comprehensive screening of exhaled metabolites from bottlenose dolphins, Aksenoy et al. did not detect any trace of isoprene56. Our present search in the Ensembl genome database57 and EMBL-EBI resource58 showed that IDI2 is not at all expressed in pigs and in bottlenose dolphins but is well expressed in goats and cattle, underlining functional IDI2 as discriminator between isoprene presence and absence. IDI1 is ubiquitously expressed in many tissues in all these animals.
Previously, via microextraction-coupled mass-spectrometric measurements of headspace of arterial and venous blood samples collected from mechanically ventilated humans and pigs, we observed extremely low (up to 10-fold lower than in human) isoprene concentrations within the portal and mixed venous blood of pigs33. Such tiny fraction may be washed-out (i.e., stored previously) and/or produced via minimal IDI1 activity in the peripheral compartments. Nevertheless, as soon as the blood crossed the hepatic circulation, isoprene concentrations were diminished in hepatic venous samples – most likely due to a high rate of isoprene metabolism in pig liver. Similar to pigs and dolphins, only the IDI1 is expressed in rats and mainly within the liver. Most likely, due to a low (compared to higher mammals) isoprene oxidation rate in rat liver59, Deneris et al. had detected a certain fraction of isoprene in rat liver cytosol in vitro. They suggested that isoprene could be produced in rat liver via non-enzymatic degradation of IPP and/or DMAPP and postulated in general that breath isoprene is linked to hepatic cholesterogenesis40. While the pre-clinical finding of Deneris et al. was correct, the general inference drawn on the origin of human breath isoprene based on those outcomes from rats was wrong. In human hepatocellular microsomes, the complex cytochrome P450 enzyme system immediately oxidizes isoprene and isoprene monoepoxides to avoid hemiterpene toxicity60. The oxidation rate in human liver microsomes is magnitudes higher compared to rats59. Due to such high isoprene oxidation rate, hepatic cholesterogenesis is insufficient to contribute any considerable concentration of isoprene to human exhalation.
In the present study, despite normal plasma lipid profiles, bile substrates, sex-hormones, and wild-type IDI1 in rare adults and blood-related family members, significant aberrations in their isoprene exhalations confirmed our previously suggested30 independence of human exhaled isoprene from hepatic cholesterogenesis and related principal pathways. Therefore, due to the absence of functional IDI2 expressions in these isoprene aberrated adults, the source of human breath isoprene should mainly be directly attributed to muscular metabolic activity and not to hepatic cholesterol biosynthesis. The isoprene absent adults constantly inhaled low concentrations of ambient isoprene from the inspired air but they never exhaled any tracible fraction of this VOC. This indicates an uptake/partial storage and/or metabolism of ambient isoprene in these individuals.
Skeletal muscles represent around 40% of adult human body mass and predominantly utilize glucose and lipids to produce energy, regulate intramyocellular signaling and integrity61,62. Insulin governs the balance between glucose and fatty acid metabolism in muscle63 and peroxisomal beta-oxidation senses intracellular fatty acids and regulates lipolysis64. Besides mitochondrial oxidation, peroxisomal beta-oxidation of very long-chain fatty acids, long-chain fatty acids and dicarboxylic acids produces acetyl-CoA. Acetyl-CoA is channeled towards farnesyl diphosphate (farnesyl-PP) production inside the peroxisomes48. All enzymes (except 3-hydroxy-3-methylglutaryl-CoA reductase/HMGCR) step-wise converting acetyl-CoA to farnesyl-PP contain functional peroxisomal targeting signals and at the second last step of this pathway, IPP is converted to DMAPP via the IDI2 enzyme as only IDI2 is highly expressed here. Farnesyl-PP exits the peroxisomes to execute various metabolic processes in other cellular organelles (Fig. 5).
The pathway is based on the results of this study. The pathway depicts the potential contributions of myocellular organelles, e.g., sarcoplasm, sarcoplasmic reticulum (SR), mitochondria and most importantly the peroxisomes. Human IDI2 is only and highly expressed within the myocellular peroxisomes. Peroxisomes are metabolic organelle—mainly responsible for lipolysis. Here, acetyl-CoA is produced via beta-oxidation of fatty acids within peroxisomes. Acetyl-CoA is then channeled towards farnesyl-PP (FPP) production. One step before the FPP generation, isopentyl-PP (IPP) is converted into its active isoform dimethylallyl-PP (DMAPP) by the IDI2 activity. IDI2 does not convert DMAPP back to IPP. In human, DMAPP is the only source of isoprene. Unlike plants, humans lack isoprene synthase and its enzyme homologue. Thus, IDI2 determines human isoprene production in skeletal-myocytes. Farnesyl-PP exits peroxisomes and enters other organelles to execute in other metabolic pathways, e.g., cholesterol metabolism in the SR.
Any kind of muscle movement/activity immediately gives rise to breath isoprene13,65. Due to its low aqueous solubility and high volatility, isoprene is positively related to cardiac output and negatively related to minute ventilation66,67. Both low-intensity and exhaustive exercise demonstrated an instant and profound increase in exhaled alveolar isoprene concentrations at the initial warm-up phase (that increases muscle perfusion) followed by gradual decrease with increasing work-load, which indicates its possible production and washout from the active muscle compartments14,65,68. Exercise immediately increases skeletal muscular lipolysis, fatty acid transport from plasma to sarcoplasm and triglyceride hydrolysis to compensate energy demand. Thus, our present findings ascertain that isoprene is potentially originating from lipolysis in the skeletal muscle and wild-type IDI2 denominates the presence of isoprene in exhaled human breath and also acts as the rate limiting factor for endogenous isoprene production.
Although we were able to detect the IDI2 mutation in PBMC, IDI2 gene and protein expression are skeletal muscle specific. Previously we observed IDI1 but not IDI2 gene expression in PBMC of healthy adults with absence, deficiency, and normal breath isoprene30. To assess the biological consequences of the IDI2 variant, gene, and protein expression studies would require the collection of muscle biopsies of the affected adults. Those investigations are, however, behind the scope of the present study and limited by ethical considerations. In vitro experiments using muscle tissue or cell lines might shed light on the metabolic and functional background of isoprene synthesis, metabolism, and downstream function. Investigation of relationship between IDI2 gene and protein expressions and isoprene exhalation under exercise was beyond the scope of the present study design but may reveal interesting insights in future studies.
We discovered the genetic origin of human breath isoprene production and related biochemical routes (Fig. 5). The rare character of isoprene absence/deficiency in healthy human adults is autosomal (10th chromosome, locus: 10p15.3) recessive. We translated isoprene as the first breath VOC biomarker with well-defined down-stream endogenous origin and metabolic pathways. This knowledge will redefine the clinical interpretations of this noninvasive biomarker for various physio-metabolic, pathophysiological, and inherited conditions. We assume that the presence of DMAPP may not be essential for healthy human life as all principal pathways converting acetyl-CoA to farnesyl-PP are associated with lipid and cholesterol metabolism can utilize IPP to execute them normally. Already reported endocrine regulation39 and age dependency23,24,30 of isoprene exhalation indicates new research scopes of IDI2 activity in human aging (Supplementary Table 1), muscle mass development and related conditions. Similarly, further investigation of IDI2 gene and protein expressions in skeletal muscle tissue along with breath isoprene expressions under various exercise trainings and in individuals with muscle dystrophy and risk of rhabdomyolysis, e.g., under statin interventions or injury may reveal unexplored frontiers in sports/fitness and musculoskeletal medicine and inter-organ metabolic cross-talk.
In order to understand the evolutionary significance of human IDI2 gene and the presence/rationales of isoprene production pathway in human, we need further multi-omic based system-wide evaluation from the genome to up-stream cascades. Tissue specific gene and protein expression followed by transcriptomics and proteomics may lead us to the actual enzymatic and metabolic significances (DMAPP to isoprene) that are linked to the last IDI2 exaptation taken place ~70 million years ago for an unknown function. Inducible IDI2 deficiency in animal models could also shed light on the kinetics and physiological background of isoprene metabolism. Further investigations should screen a large number of isoprene deficient subjects for IDI2 allele frequencies to realize its exact genetic correlation(/predisposition) factor with breath isoprene expressions. In order to apply isoprene or any other endogenous biomarker to routine clinical practice, well-defined down-stream origins and pathways should be addressed.
Methods
Study design
Based on our previously observed rare character of exhaled isoprene aberrations (absence and deficiency) in healthy adults30, we aimed to further investigate the actual reason(s) at the very down-stream level and thereby, to discover the principal human origin of this endogenous hemiterpene.
In adults, exhaled alveolar isoprene concentrations of 100–300 ppbV is regarded as the normal range and ±50 ppbV is regarded as the limit of normal physio-metabolic fluctuations. Exhaled alveolar concentration of 00 ppbV is regarded as isoprene absence and <50 ppbV is considered as significant isoprene deficiency. In adults, exhaled isoprene concentrations between.
In order to find adults with isoprene aberrations, we re-evaluated the isoprene exhalations in 2000 human subjects (aged between <1 and 100 years) from 15 consecutive clinical breath screening studies by applying real-time mass-spectrometry (proton transfer reaction—time of flight—mass spectrometry/PTR-ToF-MS). All studies were conducted at the University Medicine Rostock, 18057 Rostock, Germany in accordance with the amended Declaration of Helsinki guidelines. Ethical approvals from the Institutional Ethics Committee (IEC, University Medicine Rostock, Rostock, Germany) and signed informed consents from all participants were obtained prior to participation. In case of infants, both parents provided signed consents. Within these studies, healthy volunteers were recruited during physiological, metabolic, exercise and dietary/nutritional monitoring (Ethical approval numbers: A2011-67, A2012-0103, A2014-0037, A2015-0008, A2015-0076, A2018-0025, and A2020-0300) and both healthy and sick subjects were recruited during pathophysiological and/or therapeutic monitoring (Ethical approval numbers: A2012-0103, A2012-0071, A2015-0043, A2017-0106, A2018-0097, A2019-0040, A2020-0085, and A2021-0012). In the present study, ethical approval no. A2021-0012 is assigned to the investigations involving venous blood collection, peripheral blood mononuclear cells isolation, DNA isolation, multi-omics (breathomics, untargeted and targeted genomics) and serological metabolites analysis in healthy isoprene aberrated and isoprene normal adults.
After finding the isoprene absent rare adults, we executed multi-omic investigations of shared down-stream aberrations in genes and relevant metabolites among such adults, in blood-relatives and in unrelated healthy controls. Therefore, at first, we conducted whole exome sequencing to identify unknown homozygous variants shared by the rare adults. Then the shared mutations were checked via bidirectional Sanger sequencing in blood-related (isoprene deficient) and unrelated (isoprene normal) healthy adults. Plasma lipids, metabolites and hormones related to cholesterol metabolism were also checked serologically in all these subjects.
Due to ethical reasons, we were allowed to conduct genomics only in adults. Amongst the isoprene absent rare adults, we could only access the blood-related adult family members (parents and sibling sister) of the rare adult-1.
Breath sampling, VOC data analysis, and quantification
All spontaneously breathing subjects maintained a defined posture37 and performed oral breathing44 via customized mouthpiece69 or mask by following our state-of-the-are sampling protocol67. Continuous side-stream sampling (flow: 20–100 ml/min) from the mouthpiece or mask were performed via the heated (75–100 °C) transfer-line of a PTR-ToF-MS-8000 or a PTR-ToF-MS-1000 (Ionicon Analytik GmbH, Innsbruck, Austria) under pre-optimized experimental conditions70,71. Most importantly, PTR time-resolution of 200 ms, drift-tube temperature of 75 °C, voltage of 610 V and pressure of 2.3 mbar were used to reach the optimal E/N ratio of 139 Td23,30,72. After automatic recording of a data file/min the mass scale was recalibrated based on masses namely, 21.0226 (H3O+-isotope), 29.998 (NO+) and 59.049 (protonated C3H6O).
We used a PTR-MS viewer software (version 3.228) to process raw data. VOC data were measured continuously in counts per second (cps). Measured VOC counts were normalized to primary ion (H3O+) counts. Breath-resolved assignment of expiratory (alveolar/end-tidal) and inspiratory (room air) phases were executed via custom-made ‘breath tracker’ algorithm73,74. Here, we used an endogenous VOC (e.g., acetone) with orders of magnitudes higher concentration in exhalation than in room air as the tracker mass.
Measured VOCs were quantified either via reaction rate coefficients (k-rates) between VOC and primary ion (at the E/N ratio of 140 Th) or via multi-component VOC standard mixture under matrix adapted conditions (breath humidity) by using a liquid calibration unit (LCU, Ionicon Analytik GmbH, Innsbruck, Austria)72,75. Isoprene was quantified via LCU based calibrations.
Venous blood sampling
A total of 50 ml of antecubital venous blood was collected from each subject by a skilled and licensed physician for serological and genetic analysis.
Plasma metabolite analysis
Plasma lipids (total cholesterol, lipoproteins a, high density lipoproteins (HDL), low density lipoproteins (LDL) and triglycerides), bile substrates (total-, direct- and indirect bilirubin) and sex-hormones (estrogen, progesterone and testosterone) were analyzed at the central laboratory (Institute of Clinical Chemistry and Laboratory Medicine, University Medicine Rostock) via conventional methods (listed in Table 1).
Isolation of peripheral blood mononuclear cells
A total of 45 ml of venous blood was collected from all participants and mixed 1:1 with pre-warmed PBS (PAN-biotech, Aidenbach, Germany). Density gradient centrifugation (1200 × g, 12 min, 4 °C, brake 0) using PAN-coll separation solution (PAN-biotech) was carried out to separate peripheral blood mononuclear cells (PBMC). Isolated PBMC populations were washed twice (180 × g, 10 min) in PBS and cell numbers were determined. Cell pellets were stored at −80 °C for subsequent analyses.
Exome sequencing
Cell pellets were thawed and genomic DNA was isolated using the NucleoSpin® Tissue kit (Macherey-Nagel, Düren, Germany) according to the manufacturer’s instructions. Samples were sequenced via INVIEW Human Exome sequencing service (Eurofins Genomics, Ebersberg, Germany). The QIAGEN Clinical Insight Interpret platform (Qiagen, Hilden, Germany) was used to identify rare and unknown variants, using the following filtering criteria: only variants in exonic regions or variants that are ±20 bp flanking those regions; variants pass upstream pipeline filtering; variants with call quality ≥20; variants with allele fraction ≥90; variants that result in frameshift or in-frame indel or start/stop codon change or missense or nullizygous; variants with homozygous population frequency <1% in Europeans or no population data available.
Bidirectional Sanger sequencing
The PCR was carried out in a final volume of 25 µl containing 100 ng of genomic DNA, 0.4 µM of each primer (Eurofins Genomics), 250 µM of each dNTP (Agilent Technologies, Santa Clara, USA), 5 µl 5x Hi-Fi Reaction buffer (Meridian Bioscience, Cincinnati, OH, USA) and 0.5 µl VELOCITY™ DNA polymerase (Meridian Bioscience) using the following primers: F, AATTCTGTGTTTTACATTAGCGTTG; R, CTGGGACAGGTAGAGGATGCT. The PCR conditions were 2 min at 98 °C followed by 35 cycles of 30 s at 98 °C, 30 s at 57 °C and 15 s at 72 °C with a final step of 5 min at 72 °C. The products were further processed via QIAquick PCR Purification Kit (Qiagen) according to the manufacturer’s instructions. Purified PCR products were sequenced using the Mix2Seq sequencing service (Eurofins Genomics).
Statistics and reproducibility
Exhaled alveolar and inspired room air isoprene concentrations from a minute of steady spontaneous breathing (with normal respiratory rate of 10–14 breaths/min) were considered for quantification. Measurement was repeated three times in each subject. Due to non-parametric distributions, median values were used for statistical analysis.
Statistical significances of differences in isoprene concentrations between different age groups/subgroups were tested by means of Kruskal-Wallis one-way ANOVA on ranks (Kolmogorov-Smirnov test for normality followed by the multiple comparisons via post-hoc Dunn’s method at p-value ≤ 0.005) in SigmaPlot version 14. Here, groups with young subjects (aged <20 years, n = 345), isoprene normal adults (aged 20–60 years, n = 1318), isoprene deficient adults (aged 20–60 years, n = 64), isoprene absent adults (aged 20–60 years, n = 5), seniors (aged >60 years, n = 268) and total inspiratory samples (n = 2000) were compared. From all pairwise-multiple comparisons, statistically significant differences with respect to ‘isoprene normal adults’ were of study importance (Fig. 1). Detailed data on each group size (N), group median, difference in ranks and corresponding p-values are presented in Supplementary Table 1. In order to avoid overlaps of exhaled isoprene concentrations from different age groups and/or subgroups, the ‘total recruited subjects’ was not compared statistically (Fig. 1). Comparison of differences (with corresponding p-value) between the young subjects (aged <20 years) and seniors (aged >60 years) are also presented in the results.
Overall and group-wise correlations between subject’s biological age (year) and exhaled isoprene concentrations (ppbV) were assed via Spearman correlation test (due to non-parametric distribution of data).
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
All disclosable data are available in the main text or the supplementary materials. Raw and processed experimental data (i.e., not under ethical restrictions) is available from the corresponding author upon reasonable request. However, exome sequencing raw data cannot be made publicly available due to the General Data Protection Regulation (GDPR) of the European Union. Due to the small number of rare individuals, this potentially identifying and sensitive patient information could compromise the privacy of research participants.
References
Palmer, P. I., Marvin, M. R., Siddans, R., Kerridge, B. J. & Moore, D. P. Nocturnal survival of isoprene linked to formation of upper tropospheric organic aerosol. Science 375, 562–566 (2022).
Atmospheric chemistry: Isoprene’s fate. Nature 460, 782–782 (2009).
Byron, J. et al. Chiral monoterpenes reveal forest emission mechanisms and drought responses. Nature 609, 307–312 (2022).
Werner, C. et al. Ecosystem fluxes during drought and recovery in an experimental forest. Science. 374, 1514–1518 (2021).
Liu, Y. et al. Isoprene photo-oxidation products quantify the effect of pollution on hydroxyl radicals over Amazonia. Sci Adv. 4, eaar2547 (2018).
Lamkaddam, H. et al. Large contribution to secondary organic aerosol from isoprene cloud chemistry. Sci. Adv. 7, eabe2952 (2021).
Armstrong, A. Isoprene and agriculture. Nat. Geosci. 6, 513–513 (2013).
Sharkey, T. D. & Yeh, S. Isoprene emission from plants. Annu. Rev. Plant Physiol. Plant Mol. Biol. 52, 407–436 (2001).
Hillier, S. G. & Lathe, R. Terpenes, hormones and life: isoprene rule revisited. J. Endocrinol. 242, R9–R22 (2019).
Mochalski, P., King, J., Mayhew, C. A. & Unterkofler, K. A review on isoprene in human breath. J. Breath. Res. https://doi.org/10.1088/1752-7163/acc964 (2023).
SwRI Pegs Trace Compounds in Body Fluids. Chem. Eng. News Archive 38, 36–37 (1960).
Jansson, B. O. & Larsson, B. T. Analysis of organic compounds in human breath by gas chromatography-mass spectrometry. J. Lab Clin. Med. 74, 961–966 (1969).
King, J. et al. Measurement of endogenous acetone and isoprene in exhaled breath during sleep. Physiol. Meas. 33, 413–428 (2012).
Pugliese, G. et al. Real-time metabolic monitoring under exhaustive exercise and evaluation of ventilatory threshold by breathomics: Independent validation of evidence and advances. Front. Physiol. 13, 946401 (2022).
Visualization of exhaled breath metabolites reveals distinct diagnostic signatures for acute cardiorespiratory breathlessness. Sci. Transl. Med. https://www.science.org/doi/10.1126/scitranslmed.abl5849 (2022).
McGrath, L. T. et al. Breath isoprene during acute respiratory exacerbation in cystic fibrosis. Eur. Respiratory J. 16, 1065–1069 (2000).
T, M. L., Robin, P. & Bernard, S. Breath isoprene in patients with heart failure. Eur. J. Heart Fail. 3, 423–427 (2001).
Karl, T. et al. Human breath isoprene and its relation to blood cholesterol levels: new measurements and modeling. J. Appl. Physiol. 91, 762–770 (2001).
Pabst, F., Miekisch, W., Fuchs, P., Kischkel, S. & Schubert, J. K. Monitoring of oxidative and metabolic stress during cardiac surgery by means of breath biomarkers: an observational study. J. Cardiothorac. Surg. 2, 37 (2007).
Fuchs, D. et al. Decline of exhaled isoprene in lung cancer patients correlates with immune activation. J. Breath. Res. 6, 027101 (2012).
Poli, D. et al. Exhaled volatile organic compounds in patients with non-small cell lung cancer: cross sectional and nested short-term follow-up study. Respiratory Res. 6, 71 (2005).
Wang, N. et al. Breath chemical markers of sexual arousal in humans. Sci. Rep. 12, 6267 (2022).
Sukul, P. et al. Physiological and metabolic effects of healthy female aging on exhaled breath biomarkers. iScience 25, 103739 (2022).
Smith, D. et al. Isoprene levels in the exhaled breath of 200 healthy pupils within the age range 7–18 years studied using SIFT-MS. J. Breath. Res. 4, 017101 (2009).
Kushch, I. et al. Breath isoprene-aspects of normal physiology related to age, gender and cholesterol profile as determined in a proton transfer reaction mass spectrometry study. Clin. Chem. Lab. Med. 46, 1011–1018 (2008).
Hoffmann, G. et al. Mevalonic Aciduria — an inborn error of cholesterol and nonsterol isoprene biosynthesis. N. Engl. J. Med. 314, 1610–1614 (1986).
Haas, D. & Hoffmann, G. F. Mevalonate kinase deficiency and autoinflammatory disorders. https://www.nejm.org/doi/10.1056/NEJMp078083 (2009).
Neven, B. et al. Allogeneic Bone Marrow Transplantation in Mevalonic Aciduria. N. Engl. J. Med. 356, 2700–2703 (2007).
King, J. et al. Breath isoprene: Muscle dystrophy patients support the concept of a pool of isoprene in the periphery of the human body. Biochem. Biophys. Res. Commun. 423, 526–530 (2012).
Sukul, P., Richter, A., Schubert, J. K. & Miekisch, W. Deficiency and absence of endogenous isoprene in adults, disqualified its putative origin. Heliyon 7, e05922 (2021).
Gelmont, D., Stein, R. A. & Mead, J. F. Isoprene — The main hydrocarbon in human breath. Biochem. Biophys. Res. Commun. 99, 1456–1460 (1981).
Jordan, A. et al. On-line trace gas analysis at ppt-levels: medical applications. Food Res. Air Qual. 84, 7–17 (1997).
Miekisch, W., Schubert, J. K., Vagts, D. A. & Geiger, K. Analysis of volatile disease markers in blood. Clin. Chem. 47, 1053–1060 (2001).
Turner, C., Spanel, P. & Smith, D. A longitudinal study of breath isoprene in healthy volunteers using selected ion flow tube mass spectrometry (SIFT-MS). Physiol. Meas. 27, 13–22 (2006).
King, J. et al. Physiological modeling of isoprene dynamics in exhaled breath. J. Theor. Biol. 267, 626–637 (2010).
Unterkofler, K. et al. Modeling-based determination of physiological parameters of systemic VOCs by breath gas analysis: a pilot study. J. Breath. Res. 9, 036002 (2015).
Sukul, P., Trefz, P., Kamysek, S., Schubert, J. K. & Miekisch, W. Instant effects of changing body positions on compositions of exhaled breath. J. Breath. Res. 9, 047105 (2015).
Sukul, P. et al. Effects of COVID-19 protective face-masks and wearing durations onto respiratory-haemodynamic physiology and exhaled breath constituents. Eur. Respiratory J. 60, 2200009 (2022).
Sukul, P., Schubert, J. K., Trefz, P. & Miekisch, W. Natural menstrual rhythm and oral contraception diversely affect exhaled breath compositions. Sci. Rep. 8, 10838 (2018).
Deneris, E. S., Stein, R. A. & Mead, J. F. Invitro biosynthesis of isoprene from mevalonate utilizing a rat liver cytosolic fraction. Biochem. Biophys. Res. Commun. 123, 691–696 (1984).
Harshman, S. W. et al. Investigation of an individual with background levels of exhaled isoprene: a case study. J. Breath. Res. 17, 027101 (2023).
Biagini, D. et al. Effects of long-term vegan diet on breath composition. J. Breath Res. 16, 026004 (2022).
Taucher, J. et al. Detection of isoprene in expired air from human subjects using proton-transfer-reaction mass spectrometry. Rapid Commun. Mass Spectrom. 11, 1230–1234 (1997).
Sukul, P., Oertel, P., Kamysek, S. & Trefz, P. Oral or nasal breathing? Real-time effects of switching sampling route onto exhaled VOC concentrations. J. Breath. Res. 11, 027101 (2017).
Isopentenyl-diphosphate isomerases in human and mouse: evolutionary analysis of a mammalian gene duplication. https://link.springer.com/article/10.1007/s00239-003-2476-8 (2003).
Clizbe, D. B., Owens, M. L., Masuda, K. R., Shackelford, J. E. & Krisans, S. K. IDI2, a second isopentenyl diphosphate isomerase in mammals. J. Biol. Chem. 282, 6668–6676 (2007).
Morales, P. E., Bucarey, J. L. & Espinosa, A. Muscle lipid metabolism: role of lipid droplets and perilipins. J. Diabetes Res. 2017, 1789395 (2017).
Charles, K. N. et al. Functional peroxisomes are essential for efficient cholesterol sensing and synthesis. Front. Cell Dev. Biol. 8, 560266 (2020).
Bongers, M. et al. Adaptation of hydroxymethylbutenyl diphosphate reductase enables volatile isoprenoid production. eLife 9, e48685 (2020).
Sharkey, T. D. et al. Evolution of the isoprene biosynthetic pathway in Kudzu. Plant Physiol. 137, 700–712 (2005).
Sharkey, T. D. Isoprene synthesis by plants and animals. Endeavour 20, 74–78 (1996).
BLAST: Basic Local Alignment Search Tool. https://blast.ncbi.nlm.nih.gov/Blast.cgi (2023).
Traxler, S. et al. VOC breath profile in spontaneously breathing awake swine during Influenza A infection. Sci. Rep. 8, 14857 (2018).
Fischer, S. et al. Impact of food intake on in vivo VOC concentrations in exhaled breath assessed in a caprine animal model. J. Breath. Res. 9, 047113 (2015).
Oertel, P. et al. Continuous real-time breath analysis in ruminants: effect of eructation on exhaled VOC profiles. J. Breath. Res. 12, 036014 (2018).
Aksenov, A. A. et al. Metabolite content profiling of bottlenose dolphin exhaled breath. Anal. Chem. 86, 10616–10624 (2014).
Ensembl Genomes - an overview | ScienceDirect Topics. https://www.sciencedirect.com/topics/medicine-and-dentistry/ensembl-genomes (2023).
Institute, E. B. EMBL-EBI homepage. https://www.ebi.ac.uk/ (2023).
Duescher, R. J. & Elfarra, A. A. Human liver microsomes are efficient catalysts of 1,3-butadiene oxidation: evidence for major roles by cytochromes P450 2A6 and 2E1. Arch. Biochem. Biophys. 311, 342–349 (1994).
Bogaards, J. J. P., Venekamp, J. C. & van Bladeren, P. J. The biotransformation of isoprene and the two isoprene monoepoxides by human cytochrome P450 enzymes, compared to mouse and rat liver microsomes. Chem.-Biol. Interact. 102, 169–182 (1996).
Lipid metabolism in skeletal muscle: generation of adaptive and maladaptive intracellular signals for cellular function. Am. J. Physiol.-Endocrinol. Metab. https://journals.physiology.org/doi/full/10.1152/ajpendo.00561.2011 (2012).
Hagström-Toft, E. et al. Evidence for a major role of skeletal muscle lipolysis in the regulation of lipid oxidation during caloric restriction in vivo. Diabetes 50, 1604–1611 (2001).
Muscat, G. E. O. et al. Regulation of cholesterol homeostasis and lipid metabolism in skeletal muscle by liver X receptors. J. Biol. Chem. 277, 40722–40728 (2002).
Ding, L. et al. Peroxisomal β-oxidation acts as a sensor for intracellular fatty acids and regulates lipolysis. Nat. Metab. 3, 1648–1661 (2021).
Schubert, R. et al. Metabolic monitoring and assessment of anaerobic threshold by means of breath biomarkers. Metabolomics 8, 1069–1080 (2012).
Sukul, P. et al. FEV manoeuvre induced changes in breath VOC compositions: an unconventional view on lung function tests. Sci. Rep. 6, 28029 (2016).
Sukul, P. et al. Exhaled breath compositions under varying respiratory rhythms reflects ventilatory variations: translating breathomics towards respiratory medicine. Sci. Rep. 10, 14109 (2020).
King, J. et al. Isoprene and acetone concentration profiles during exercise on an ergometer. J. Breath. Res. 3, 027006 (2009).
Sukul, P., Schubert, J. K., Kamysek, S., Trefz, P. & Miekisch, W. Applied upper-airway resistance instantly affects breath components: a unique insight into pulmonary medicine. J. Breath. Res. 11, 047108 (2017).
Sukul, P., Trefz, P., Schubert, J. K. & Miekisch, W. Advanced setup for safe breath sampling and patient monitoring under highly infectious conditions in the clinical environment. Sci. Rep. 12, 17926 (2022).
Trefz, P. et al. Continuous real time breath gas monitoring in the clinical environment by proton-transfer-reaction-time-of-flight-mass spectrometry. Anal. Chem. 85, 10321–10329 (2013).
Remy, R. et al. Profiling of exhaled volatile organics in the screening scenario of a COVID-19 test center. iScience https://doi.org/10.1016/j.isci.2022.105195 (2022).
Schwoebel, H. et al. Phase-resolved real-time breath analysis during exercise by means of smart processing of PTR-MS data. Anal. Bioanal. Chem. 401, 2079–2091 (2011).
Sukul, P., Trefz, P., Schubert, J. K. & Miekisch, W. Immediate effects of breath holding maneuvers onto composition of exhaled breath. J. Breath. Res. 8, 037102 (2014).
Trefz, P., Schubert, J. K. & Miekisch, W. Effects of humidity, CO2 and O2 on real-time quantitation of breath biomarkers by means of PTR-ToF-MS. J. Breath. Res. 12, 026016 (2018).
Acknowledgements
We thank all participants for their voluntary participation in this study. We thank Dr. Fuchs (ROMBAT Group) for supporting us with the timely arrangements of consumables and materials ordering process. We thank Dr. Brock for collection of blood samples and for supporting the PBMC analysis. We thank our colleagues (Clinical chemists: Dr. Holdt, Dr. Bastian and Dr. Schubert) from the central laboratory (Institute of Clinical Chemistry and Laboratory Medicine) for timely serological analysis of all blood samples. The study was partly supported by the following research grants: European Union fund for regional development EFRE (JKS, WM). EU Horizon-2020 grant H2020-PCH-HEARTEN project 643694 (W.M., J.K.S., P.S.). European Union’s Horizon 2020 Marie Skłodowska-Curie research and innovation programme 674911-IMPACT (J.K.S., W.M., P.S.). University Medicine Rostock’s FORUN programme (2018) 889003 (P.S.).
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
P.S. conceived the idea and with J.K.S. and W.M. conceptualized the study. P.S., A.R., W.M., and J.K.S. designed the study. P.S., A.R., C.J., W.M., and J.K.S. developed the analytical methods. P.S. and A.R. recruited volunteers and performed experiments. P.S. and A.R. analyzed data. prepared and visualized results. P.S., A.R., C.J., W.M., and J.K.S. interpreted outcomes. W.M. and J.K.S. provided all resources. W.M., C.J., and J.K.S. supervised the entire project. P.S. and A.R. wrote the original draft. W.M., C.J., and J.K.S. reviewed and edited the original draft. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Communications Biology thanks Karl Unterkofler, Amane Hori, and Chiea Chuen Khor for their contribution to the peer review of this work. Primary Handling Editors: Tobias Goris. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sukul, P., Richter, A., Junghanss, C. et al. Origin of breath isoprene in humans is revealed via multi-omic investigations. Commun Biol 6, 999 (2023). https://doi.org/10.1038/s42003-023-05384-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s42003-023-05384-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.