Abstract
Self-medication, as a form of self-care, is a common practice worldwide, and often involves the use of both over-the-counter and prescription-only medicines, including antibiotics, anti-malarials and others. Increasing concerns over the global emergence and spread of antimicrobial resistance point to the need to reduce and optimise the use of antimicrobial medicines, both in human and animal health. Over the past few decades, numerous studies on self-medication with antibiotics have sought to determine the prevalence, risks and/or factors related to ‘inappropriate’ use in different parts of the world. Yet much of this literature tends to follow a rather normative approach, which regards such practices as problematic and often irrational, frequently overlooking structural aspects, situated circumstances and individuals’ own reasoning. Based on a mixed methods social science research project in Maputo, which included a household survey, observations in pharmacies and interviews with users and healthcare providers, this paper aims to discuss self-medication in light of local users’ everyday practical reasoning. While situating self-medication within local contextual contingencies, the analysis highlights the ways in which personal and socially shared experiences, articulated with forms of knowledge and information provided by different sources, shape and inform practices of and attitudes towards self-medication with antibiotics. By looking at self-medication beyond (non-)prescription use, and by examining individuals’ decisions within their socioeconomic and therapeutic landscapes in Maputo, this study sheds light on the structural and relational factors that contribute to certain consumption practices that do not always follow biomedical recommendations of ‘rational’ or ‘appropriate’ use, helping to deconstruct and further problematise the various legitimate meanings and understandings of ‘responsible’ use.
Similar content being viewed by others
Introduction
Practices of self-medication, as a form of self-care, have always triggered controversy. Yet they are common worldwide. Self-medication often involves a combination of therapeutic resources and the use of both over-the-counter (OTC) and prescription-only medicines, including antibiotics. Increasing concerns with the global emergence and spread of antimicrobial resistance (AMR) have pointed to the need to reduce and optimise the use of antimicrobial medicines (AMs), both in human and animal health (WHO, 2015a). This includes tackling the use of AMs without a prescription, which is considered a form of AM ‘misuse’ that can potentially accelerate the emergence of resistant microorganisms (WHO, 2015b). Over the last decades, numerous studies on self-medication with antibiotics, conducted in different parts of the world, have sought to determine the prevalence, risks and/or factors related to ‘inappropriate’ antibiotic use (e.g., Borg and Scicluna, 2002; Grigoryan et al., 2007; Elmasry et al., 2013; Albawani et al., 2017; Alghadeer et al., 2018). Although tracking OTC sales is challenging in most countries (WHO, 2015b), according to a review of Alhomoud et al. (2017, p. 4), “it has been estimated that more than 50% of antibiotics are purchased without a prescription and used over-the-counter in most parts of the world”.
Much of the literature on self-medication with antibiotics, however, tends to follow a rather normative approach, which regards such practices as problematic and often irrational, frequently overlooking structural aspects, situated circumstances and individuals’ own reasoning. Moreover, in framing antibiotic use and ultimately AMR as an ‘individual behaviour’ problem—which needs to be ‘corrected’ through regulatory restrictions and educational campaigns—such approaches neglect broader contextual and relational processes in which antibiotics and other medicines are embedded (see e.g., Tan, 1999; Rodrigues, 2016; Lambert et al., 2019; Willis and Chandler, 2019), which contrasts with the recognised ‘connectedness’ as promoted by the rhetoric of the ‘One Health’ approach (Chandler, 2019).
Adding to this broader discussion on AM use, and drawing on a social science research project on medicine use in Maputo, Mozambique, this paper aims to analyse and problematise antibiotic consumption practices beyond (non-)prescription use. I start by unpacking and discussing the very notion of self-medication, the rationales and ideologies behind it, as well as the processual backgrounds which have contributed to the spread and centrality of pharmaceuticals in individuals’ everyday lives and self-care practices. This will set the theoretical background and analytical framework, which will help to shed light on the situated rationales behind certain consumption practices and on the various meanings and understandings of ‘responsible’ use.
Theoretical background
Discussions of self-medication tend to revolve around its risks and benefits (WHO, 2000), and there are different approaches regarding its legitimacy. While the medical community tends to reject most self-medication practices, emphasising health risks and the need for expert diagnosis, public authorities tend to be more tolerant, highlighting the economic advantages for managing minor ailments (Fainzang, 2017). One way of overcoming such divergences has entailed reframing some of these practices as ‘responsible self-medication’ (WHO, 1998). Yet, what a ‘responsible’ practice is may have different meanings and implications according to situated circumstances.
While different definitions of self-medication can be found throughout the literature, they generally refer to “the selection and use of medicines by individuals to treat self-recognised illnesses or symptoms” (WHO, 1998, p. 3). Within social science literature, scholars have also taken different approaches to what they consider self-medication (see e.g., Fainzang, 2017, p. 2). Lopes (2003), for example, looked at multiple uses of pharmaceuticals without a medical indication. These included medicines bought without a prescription (regardless of possible orientations from pharmacists), as well as the use of medicines previously prescribed for perceived similar situations, which were not always seen by consumers as a form of self-medication. The variation in such interpretations highlights the importance of further deconstructing the multiple dynamics in and lay logics behind these practices. As Fainzang (2017, p. 44) highlights, the ‘intellectual operation’ of taking an anti-inflammatory for a pain medically diagnosed in the past is different from using a painkiller for an unknown situation while monitoring its developments. Such analysis thus entails moving the focus from ‘rational use’ to the ‘rationales for using’ medicines (Nichter and Vuckovic, 1994), or in this case, to the rationale(s) for self-medicating (Lopes, 2003).
To a certain extent, as Hardon (1991) and Van der Geest et al. (1996) have argued, all medicine use is a potential form of self-medication, since its administration is often conducted outside of health professionals’ control. This broader approach to self-medication allows us to take into consideration other more nuanced aspects of medicine use, including the management of prescribed medicines. This is particularly relevant for understanding different modalities of use around certain medicines, such as antimicrobials, whose prescription regimens normally imply strict compliance. Therefore, despite maintaining an analytical distinction between self-initiated consumption practices and lay adjustments to medical prescriptions, in this paper I will use this broader conception of self-medication. The aim here, however, is not to incorporate the study of compliance into self-medication practices. Compliance is a ‘value-laden term’ (Donovan and Blake, 1992) embedded in a normative and medical-centred perspective (Conrad, 1985), which tends to frame variations to medical prescriptions as a form of deviance (idem; see also Stevenson et al., 2002). Such an approach often fails to recognise and understand the ‘various legitimate rationalities’ (Cohen et al., 2001) in medicine use, as highlighted above. Acknowledging the legitimacy of multiple, and sometimes overlapping, modes of reasoning brings complexity and further enlightening insights to the otherwise dichotomised conception of rational/irrational use (see e.g., Britten, 2008; Craig, 2002; Etkin and Tan, 1994; Whyte et al., 2002). As these and other studies have shown, and as the empirical examples in this paper will also illustrate, it is important to study medicines as social, political and economic phenomena, in order to contextualise and understand the reasoning behind different forms of use, but also their significance in modern therapeutic consumption practices.
Processes of medicalisation (Zola, 1972; Conrad, 1992) and the commodification of health (Nichter, 1989) gave rise to the increasing use of pharmaceuticals as a privileged therapeutic solution for health problems—both for prescribers and users. Such a phenomenon, described in the sociological literature as the ‘pharmaceuticalisation of society’ (e.g., Abraham, 2010; Williams et al., 2011), has resulted in the widespread use of medicines to manage gradually more and more aspects of individuals’ everyday lives. Increased access to both biomedical healthcare, as well as to contact with health professionals or agents has contributed not only to the social dissemination of biomedical concepts of health, disease, well-being and care, but also to the dissemination of prescribed pharmaceutical solutions. This has resulted in a general increase in pharmaceutical consumption, and consequently a gradual increase in lay familiarity with such therapeutic technologies (Lopes, 2009). The expansion of pharmaceutically-driven solutions has furthermore characterised what Biehl (2007, p. 1100) has called the ‘pharmaceuticalisation of public health’; in other words, the “delivery of technology regardless of health care infrastructures”, otherwise known as so-called ‘magic bullet’ approaches (see also Cueto, 2013), which for decades have dominated international health interventions (Biehl and Petryna, 2013)Footnote 1.
These processual backgrounds, together with medicines’ pharmacological, social and symbolic efficacies, and their potentially ‘liberating’ effects (Whyte, 1988; Van der Geest and Whyte, 1989), are key to understanding the spread and centrality of pharmaceuticals in individuals’ everyday lives and, in particular, their presence in self-care practices. As different scholars have pointed out, self-medication can be seen as a source of individual empowerment, offering a certain autonomy in treatment decisions (Fainzang, 2017) and freedom from professional dominance (Van der Geest et al., 1996). It may, however, also contribute to a greater dependence on the pharmaceutical industry (Van der Geest, 1987; Nichter and Vuckovik, 1994) or on expert systems (Lopes, 2009), shifting the exclusive emphasis even further away from prescribers towards the substances and the multiplicity of other social, economic and political structures and relations surrounding medicine use, particularly in self-medication practices.
To understand self-medication practices, it is therefore important to take into consideration the multiple contextual aspects, reasoning and dynamics that may differentially influence how individuals relate to medicines (or medical technologies), as well as their therapeutic options and decisions in different situations. These include, as numerous studies have highlighted, contextual economic infrastructure, drug regulations, the functioning structure of health systems, and the role of both formal and informal sectors in pharmaceutical and healthcare provision (e.g., van der Geest, 1987; Van der Geest and Hardon 1990; Kamat and Nichter, 1998), but also local cultural (re)interpretations of medicines, individuals’ financial constraints, access to reliable information and lay practical experience (e.g., Nichter, 1980; Bledsoe and Goubaud, 1988; Hardon, 1991; Tan, 1999; Lopes, 2009).
In this paper, I aim to add to these contributions by examining self-medication practices in light of the everyday practical reasoning (cf. Horlick-Jones et al., 2007) of local users in Maputo. While situating self-medication within their contextual contingencies and wider therapeutic consumption practices and relationships, I analyse how individuals’ own and socially shared experiences, articulated with information provided by different sources, shape and inform their practices and attitudes towards self-medication, particularly with antibiotics. Combining different methodological approaches, including the collection of qualitative and quantitative data, and focusing on the management of common symptoms—thus not looking exclusively at antibiotic use—have provided richer insight into the place of antibiotics in individuals’ everyday lives.
In the following sections, I will briefly describe the study setting and present the methods used to collect and analyse the data. The main findings of this study will then be presented and discussed in the last sections of the paper.
Setting
Maputo is the capital and most populous city of Mozambique, with approximately 1.1 million people, and is situated on the east coast of southern Africa (INE, 2019). The city has a small central urbanised area with conventional buildings, paved roads, water, electricity and drainage systems, and is surrounded by a larger peripheral area, mainly characterised by shanty town neighbourhoods, where most of the city’s population lives (UN-HABITAT, 2010).
Extensive reforms and developments in the health and pharmaceutical sectors since the country’s independence in 1975 have improved the population’s access to public healthcare facilities, as well as the supply and distribution of essential medicines (Barker, 1983). Despite significant improvements in the last decades, however, Mozambique’s health sector still faces multiple challenges. The country’s health profile and disease burden are largely dominated by communicable diseases, especially HIV/AIDS and malaria (together responsible for over half of deaths in the general population), followed by diarrhoeal diseases, respiratory infections and tuberculosis (MISAU, 2013). Besides improvement needs in areas such as nutrition, access to safe water, sanitation and basic health services, the country’s epidemiological disease patterns are also determined by climate conditions and variations, not only regarding seasonal-related diseases (during both rainy and dry seasons), but also due to the country’s vulnerability to natural disasters such as floods and cyclones (idem).
Developments in the pharmaceutical sector in the last decades have also resulted in significant changes. The national formulary to regulate the use of medicines within health services, published in 1977 (and last updated in 2017), reduced the number of required medicines in order to achieve more cost-effectiveness, and was accompanied by legislation that allowed the prescription of generic drugs only (Barker, 1983)—which may be the reason why most individuals know most of their antibiotics by their active ingredient rather than by their brand name. The introduction of neoliberal policies in the 1980s and the Medicines Law—Lei do Medicamento (nr. 4/98)—of 1998 both expanded the private pharmaceutical sector in the country. The population’s access to pharmaceuticals increased from 10% in 1975 to 80% in 2007 (WHO, 2007), and in 2012 there were a total of 293 pharmacies in the country—60% of which were concentrated in Maputo (MISAU, 2012). Such a proliferation of pharmacies in the capital city made pharmaceutical products more easily accessible. Despite legislative restrictions to control the sale of certain medicines (such as antimicrobials), in many pharmacies some of these drugs are available without a prescription. Moreover, pharmaceuticals in Maputo circulate through multiple channels and, as in many other African countries (see e.g., van der Geest, 1987; Jaffre, 1999; Baxerres and Le Hesran, 2006; Sánchez, 2016), a variety of medicines, including different types of antibiotics, are widely available in local informal markets.
Methods
The quantitative and qualitative data supporting this paper were collected during a total of ten months of fieldwork in Maputo city, divided into two phases. The first phase of data collection (2013–2014) included observations of client–provider interactions in pharmacies, exploratory interviews and informal conversations with practitioners and representatives from different health-related organisations, the conducting of seven focus group discussions (FGDs, n = 42), and the application of a household survey (n = 265, one person per household) in fifteen randomly selected neighbourhoods in Maputo city. The questionnaires were applied by 8 undergraduates studying sociology at the Eduardo Mondlane University (UEM). These students were trained, supervised and accompanied to the neighbourhoods by the author. The survey respondents had multiple religious and ethnic backgrounds; their ages ranged from 18 to 87 years (mean 34); 68.7% were female and 31.3% were male; a slight majority was employed (37.7%) and/or students (27.9%). Besides their housing characteristics (and the neighbourhoods they lived in), respondents’ economic conditions were also measured based on the ownership of durable home assets and access to services. This was assessed on the basis of 11 items (adapted from the socioeconomic indicator used in MISAU, INE, and ICFI, 2011), ranging from the most common—such as electricity, piped water, TV and radio—to the scarcest— such as access to the Internet, a car, a motorcycle or a bicycle. While half of the respondents had access to the five most common items, only 9% possessed them all. Socioeconomic status differed significantly according to the district the respondents lived in (with a higher concentration of individuals with more possessions/access in the more affluent areas in the city centre), and it was positively related to their educational level (the higher the level of education, the higher their economic status). The quantitative data were analysed using IBM SPSS Statistics 20.
In the second phase of fieldwork (2016), more in-depth qualitative data were collected. Repeat follow-up interviews (2 to 3 encounters) were conducted with 17 participants (15 from the household survey and 2 from the FGDs) and 10 key informants (including practitioners from different health-related organisations) to explore further the main initial findings. The 17 in-depth interviewees were selected from 10 different neighbourhoods in Maputo city, ranging from more affluent and semi-affluent areas of the city centre to more peripheral neighbourhoods (where most study participants lived) as described above, with an attempted balance in terms of sex (nine men and eight women), age (from 21 to 59) and school level (from 10th [secondary] grade to university studies). All interviews were recorded and transcribed. After an initial thematic analysis (Green and Thorogood, 2014), a phenomenological approach (Schutz, 1972) was used to look at individuals’ experiences when managing common ailments, and their interactions with health professionals – both prescribers and dispensers. Particular emphasis was also given to their perceptions of risk and safety, and (un)certainties regarding antibiotic use and self-medication practices, based on various and multifaceted knowledge and information sources. As I will explore later in this paper, the lack of a shared understanding around the term ‘antibiotic’, as detected during the exploratory phase of the study, required some adjustments to be made to how the questions were framed, both in the questionnaires and in the follow-up interviews. In the household survey, when asked about the last antibiotic used, backup examples of common terms among the community, as well as the most common antibiotics in Maputo were provided. Despite the precautions taken, it is important to acknowledge that this vocabulary dissonance may have influenced some of the information shared by the study participants, as analysed in the following section.
In Maputo, the research project was hosted by the Department of Sociology (through the Health and Society Research Group), Faculty of Arts and Social Sciences, UEM. It received formal ethical approval from the Institutional Committee on Bioethics for Health of the Faculty of Medicine and Maputo Central Hospital (CIBS_FM&HCM), as well as all the required administrative permissions. Written informed consent was obtained from all individuals from the community who participated in the FGDs, the household survey and the individual interviews. All other informants gave oral consent. Apart from the face-to-face application of the household questionnaires, all data collection was undertaken by the author.
Findings
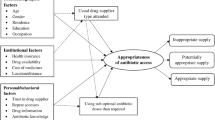
The empirical data on self-medication is structured around five main sub-sections, through which different dimensions of individuals’ everyday practical reasoning will be unfolded. A brief statistical overview of reported self-medication practices is followed by a thorough analysis of the more in-depth qualitative data, which explores how antibiotics are managed at home; the importance of the standardisation of medical prescriptions; the significance of experiential knowledge and the role of (and access to) different sources of information; and, finally, the contextual contingencies and realities of healthcare provision and therapeutic encounters, which also contribute to self-medication practices.
Self-medication practices: statistical overview
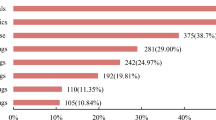
The household survey applied in fifteen neighbourhoods in Maputo city entailed two different approaches for capturing medicine use. The data analysed in this article refer to two sets of questions related to therapeutic consumption practices and itineraries. One focused on how individuals had managed the last time they felt each of three common symptoms—fever, cough and diarrhoea—as identified during the exploratory part of this researchFootnote 2. The other question focused on the last time they used specific therapeutic categories such as painkillers, antibiotics, vitamins and calming pillsFootnote 3.
With variations in terms of symptoms and therapeutic categories, overall 76.2%Footnote 4 of respondents reported having used medicines (pharmaceuticals or others) on their own initiative or following the advice of relatives or friends. Reported self-management with medicines was highest in cases of diarrhoea, followed by cough and finally fever. However, and similar to findings in other studies (e.g., Adome et al., 1996), while in most cases of fever (around 95%) a pharmaceutical (mostly paracetamol) was used, the reported self-management of diarrhoea, and especially cough, included the use of traditional medicines and home remedies. Only in very few cases, spread across all three symptoms, was the use of antibiotics reported.
Focusing on the second set of questions, 20.8%Footnote 5 of respondents mentioned the use of antibiotics within the month prior to the survey. Of those who reported having ever used antibiotics in the pastFootnote 6, 26% said that the last time they had done so was based on their own initiative (14.5%) or following advice from relatives (10.1%) or neighbours (1.4%). So, while antibiotics did not seem to be a first resort when self-managing the last appearance of common symptoms, as shown above, the high percentages of self-medication with antibiotics do indicate that they are available and are used when there is a perceived need.
When comparing the reported data on the reasons for both prescribed and non-prescribed antibiotic consumption, the differences do not seem to vary substantially. The use of antibiotics without a prescription was mainly for cough, pain in some part of the body, wounds and fever. By and large, these were also the main reported reasons (also described in terms of symptoms) for using prescribed antibiotics. Moreover, the most commonly used of the non-prescribed antibiotics was amoxicillin, followed by cotrimoxazole—which is also in line with the antibiotics most frequently bought in informal markets in Maputo (Maputo City Council, 2017); according to the study participants, including the interviewed clinicians and pharmacy workers, these were also amongst the most commonly prescribed antibioticsFootnote 7.
‘Home pharmacies’ and first aid medicines
The follow-up contacts with some of the survey respondents and FGD participants resulted in repeat encounters with a total of 17 individuals. One of the qualitative approaches I used to explore medicine use was to look at the medicines that individuals had in their households, here referred to as ‘home pharmaciesFootnote 8’. As Dew et al. (2014, p. 40) have argued, “households are a central site of health practices and decision-making”. Study participants were asked to show me whatever they considered to be a medicine. This included a variety of substances with perceived therapeutic properties: from pharmaceuticals stored in bedroom drawers, to therapeutic herbs grown in the backyard, to ‘holy water’ which had been blessed at the church or given by someone with ‘supernatural powers’. This was a useful strategy for redirecting some more general questions towards more concrete practices, and as a starting point to probe consumption practices that would otherwise have been left out of the study.
Stored pharmaceuticals included those being taken in current treatment, leftovers from previous treatments, medicines bought for possible future situationsFootnote 9, and prescriptions that had been bought and never used. The number of pharmaceuticals stored at home was substantially higher in more privileged households, and in some of the most resource-limited households only one or two pharmaceuticals were available. Figure 1 displays a ‘home pharmacy’ in the city centre and is illustrative of what I found in many other households: the predominance of a therapeutic pluralism (cf. Rodrigues, 2016; see also Clamote, 2008; Lopes, 2010) that, in this case, combined pharmaceuticals with Mozambican and other African traditional medicines and herbs, as well as Chinese teas. Among them, as we can see in the picture, was amoxicillin.
Around half (n = 8) of the houses I visited had antibiotics (bought with or without a prescription), none of which were being used at the time of the interview. The reasons for having leftovers of prescribed antibiotics at home varied. Some study participants had stopped taking the antibiotics once they felt better, or had forgotten one or two doses and had thus decided to stop the treatment altogether. In other cases, the number of pills in the boxes was reportedly higher than the dose prescribed. While in hospital pharmacies medicines were dispensed as a single dose (with the exact number of pills administered according to the prescription), in private pharmacies antibiotics were often sold in fixed-sized packages. In such cases, individuals tended to keep the extras at home for future use (for example, using the contents of capsules on wounds).
Not all antibiotics present in the visited households, however, had been bought with a prescription. In a few cases, they were bought and stocked as a preventive strategy for recurrent situations. This was the case for the home pharmacy illustrated in Fig. 1, which belonged to a highly educated 38-year-old woman, mother of three young children, who had three main pharmaceuticals as part of her home first aid kit: paracetamol, ibuprofen and amoxicillin.
These are the little things I have for first aid. Your head hurts, I give paracetamol. You have tonsillitis, or you are getting the flu, I give amoxicillin with paracetamol together. (…) I don’t expand myself to things I do not know. I don’t go to the Internet very often. I know people who are there, self-medicate, they look like doctors! (…) The pills in my house are three: paracetamol, amoxicillin and ibuprofen. (Woman, 38 years)
This woman described how she had learnt to treat these common symptoms from her mother, while growing up in a time of scarce access to healthcare following Mozambican independence. At that time, it was, according to her mother, safer to treat at home than to go to a hospital. This respondent’s reliance on such knowledge, which had been passed on from a previous generation and which had also been validated in her current practices with her own children, seems to suggest that there are variations in terms of legitimate self-medication practices. Her perceived cognitive control over a small number of medicines and health conditions seemed to be a way of distancing herself from other self-medication practices that have a widespread negative connotation.
The circulation of medicines, as well as of recommendations regarding their use in specific events, was a common practice among family members, friends and neighbours. Such recommendations were often based on medicines they had tried themselves in the past—whether recommended by a health professional or as part of community referral chains within the ‘lay referral system’ (Freidson, 1960). In this latter case, an expert referral, given to the first individual in the lay referral chain, would eventually get lost along the prescribed person’s social network. This was especially the case in situations perceived as non-severe or not serious enough to visit a doctor, where pharmaceuticals appeared as quick and effective fixes, not only in helping to alleviate certain symptoms (especially pain), but also in terms of enabling individuals to go on with their daily lives and routines. Painkillers (especially paracetamol) and anti-inflammatory medicines (ibuprofenFootnote 10, but also diclofenac) were among the most popular medicines in self-medication practices and were broadly considered to be ‘safe’. As a 42-year-old male interviewee said, smiling, while referring to the use of paracetamol to alleviate pain: “I can say it is already tradition”.
Despite the popularity of certain antibiotics, particularly amoxicillin, their recommendation and circulation within individuals’ social networks tended to be more restricted when compared to other pharmaceuticals. In most cases, antibiotics had been prescribed or recommended by a health professional (medical doctor, prescribing nurse or pharmacy worker) in the past, and their efficacy had been validated through an individual’s own embodied experience. Hence, one of the primary sources of knowledge, and of legitimacy, in self-medication patterns with antibiotics was a previous prescription for a similar situation.
Standardisation of prescriptions as a source of knowledge in self-medication practices
As explained in the introductory part of this paper, both the increased access to healthcare and contact with health professionals that followed independence also resulted in a gradual increase in lay familiarity with medical solutions, which tend to be primarily in the form of a prescription. The routinisation and standardisation of medical prescriptions (cf. Lopes, 2009) for the same perceived conditions thus constituted an important source of knowledge that enabled a more autonomous form of self-care. One common example of self-medication with antibiotics, reported by several study participants, was in the management of tonsillitis. As a 30-year-old mother of four children described:
We almost always went to the hospital in case of tonsillitis. And it was always the same medication, it was always the same thing. And I say, ‘No, I’m sorry, the mouth is smelling, he has fever, he doesn’t want to eat and everything. Ah, it’s tonsillitis, it can only be!’ So, it was also from experience. Then I began to realise the medication was that one [clavamoxFootnote 11]. Now, staying in line [at the hospital], prick the child [with a needle] and take [the sample] to a laboratory to make the malaria screening… (…) No, [we would go to the hospital] only in case of malaria, if I was missing one of the symptoms that could tell me it was tonsillitis. Otherwise we would medicate at home. (Woman, 30 years)
This highly educated woman described how the combination of symptoms normally led her to certain common diagnoses, such as tonsillitis. The frequency with which such symptoms occurred, both in her and her children, together with the repeat prescriptions of the same medicines and the efficacy of the prescribed treatments, informed her regarding how to manage perceived similar situations herself. As in most cases in this study, however, antibiotics were not immediately the first resource. When a sore throat appeared, she started with what she called a ‘home treatment’, using honey, ginger and lemon together with paracetamol or an anti-inflammatory drug. When fever came into the picture, she would then introduce clavamox. The same happened when her kids had a cough:
They leave [for school] early in the morning, catch lots of air draft and so on. But if they spend three days with cough, with home treatment [honey, carrot with sugar and/or onion], without any improvement, I introduce amoxicillin. (…) it depends on the [type of] cough.
(…) They also have asthma, which is very well controlled, they don’t even seem asthmatic. So, when it starts, I also give oral salbutamol, to combine with honey, instead of taking antibiotic, and soon it goes away. So, I’m controlling, seeing how they react and all that.
As elaborated in these excerpts, the use of antibiotics depended on how this woman’s children reacted to different treatments and how the symptoms evolved. This confidence in self-medication was also supported by her educational background: she considered herself to be very well-informed regarding health issues, since she had studied medicine (although she had not finished her studies) and had access to a diversity of expert sources of information through her personal network, but also through scientific papers that she occasionally consulted online.
As with many other interviewees, this woman considered the constraints of going to a healthcare facility for a situation she perceived as common and under her cognitive control; she claimed to know both the symptoms and the medical/pharmaceutical solutions for a variety of situations. Similar to other study participants, while in the case of perceived malaria she would go to a hospital, because she knew a laboratory test would be performed, in the case of cough or tonsillitis she opted for treatment at home since the clinical diagnosis was based on the observation of symptoms—and she knew what symptoms to look for. Hence self-medication, as illustrated in this case, involved using both the same medication from previous prescriptions and the same diagnostic strategy.
As cough and tonsillitis occurred frequently in this woman’s household, she also liked to have a stock of these antibiotics at home. As with many other upper middle class Mozambicans living in Maputo, she frequently drove to neighbouring South Africa to buy many kinds of products, including antibiotics (in this case, clavamox), syrups and other medicines, because they were cheaper there. Pharmaceuticals were thus part of the commodities that some Mozambicans would buy when crossing the border for their (sometimes monthly) grocery shopping.
The importance of the standardisation of medical prescriptions, as a source of individuals’ knowledge and confidence in managing perceived similar situations, was further emphasised by other reported situations where variations in prescriptions occurred. For example, a 29-year-old woman described two episodes of vaginal discharge which had occurred shortly before our first encounter. For each episode, she had been prescribed different treatments, which made her doubtful about what to take if the symptoms would recur.
The first time was injection plus eight tablets that I had to take all at once. The second time it was not injection, but it was also eight [tablets] plus amoxicillin. Because this happened twice and I got different medicines, [if it happened again] I’d have to go to the doctor. (Woman, 29 years)
The variation in the prescriptions together with the respondent’s unfamiliarity with the situation, the uncertainty around the severity of its cause, and the lack of access to a potentially useful and legitimate source of information (other than health professionals) resulted in an expressed reluctance to try to solve the problem in the future without medical assistance.
All of these examples are illustrative of the importance in self-medication practices of being familiar with recurrent situations that tend to receive standard prescriptions. Yet health professionals’ recommendations do not always fit with individuals’ experiences and conceptions of their (or their relatives’) health problems, and the perceived appropriate treatment and care in particular situations. As I explore next, individuals also evaluate their prescriptions and, not uncommonly, act on their evaluations.
Experiential knowledge and the role of other information sources
Although using previous prescriptions as a point of reference for self-medication is a well-known practice, as Lopes (2009) noticed in her study, individuals did not simply reproduce or mimic previous prescribed treatments. Likewise, as multiple conversations with study participants in Maputo have also shown, individuals did not passively follow the original prescriptions without making any considerations about and/or adjustments to them. Prescriptions were assessed based on multiple factors, including individuals’ accumulated knowledge and their interactions with prescribers, and were adapted according to other meaningful aspects of their everyday livesFootnote 12.
The articulation of individuals’ practical reasoning and their active engagement in such therapeutic processes is illustrated in the example below; a situation where a child was prescribed with six different medicines for her tonsillitis and her father decided to choose which to use from those in the prescription list:
I wondered [about] the prescription. I went out [of the consultation room] and started reading the medicines… And as I knew, because they always prescribed me the drugs for that, I just told the pharmacist: ‘I want this and this medicine, the rest I don’t need’. So then I bought those I knew, the others I didn’t. Why? Because when she complains about something, I already know what the problem is and what the solution is. Many times, I have that medicine at home. The fridge is full of syrups. I just take out the syrups, so they are not too cold. They take them, and it goes away! So, that’s what I did. (…) I bought those two I knew and the others I did not buy. (C: Do you remember which medicines you decided not to buy?) It was amoxicillin in syrup and clavamox. These two are antibiotics. I asked myself ‘Two antibiotics? What for? Why not amoxicillin OR clavamox?’ Then there was something else… I just forgot the names. But I know I did not buy it, I ended up opting for clavamox instead of amoxicillin. (Man, 36 years)
As described above, different factors guided this father’s decision to adjust his daughter’s medical prescription: the perceived lack of consistency with previous prescriptions (not accompanied by further explanations); his considerations about what is a reasonable number of medicines to prescribe a child (for a common situation); his understandings about antibiotic use (complemented by what he further learnt from the Internet); and his expertise as a father of four children with previous medication intake experience. The example highlights how lay knowledge is constructed (see also Baszanger, 1998) and shows how the rationales behind ‘responsible’ self-medication – or adjustments to medical prescriptions – are dynamic, and how they articulate different sources of information and forms of knowledge. Such reasoning and a ‘bricolage-like process’ (Horlick-Jones et al., 2007) of learning and making sense (and use) of multiple interpretative resources set up a more critical approach to medical prescriptions; the doctor’s prescription in this case did not follow the respondent’s perception of ‘reasonable’ prescription standards.
The role of the Internet as a source of information about antibiotic use seemed to have an important complementary place, especially when considering possible risks and associated side effects. One study participant, for example, showed how the Internet served as a confirmatory source following the recommendation he had heard on the television for the need for a cautious use of antibiotics:
[I decided to search online] by watching on television. Sometimes they talk about antibiotics, that it is not advisable to take them without medical prescription. I started searching, because I knew it was not recommendable. (Man, 42 years)
Antibiotics, in particular amoxicillin, used to be among the group of medicines that this man had consumed more frequently. He had used it every time he had flu symptoms or a cold, after having once been advised at a local pharmacy to take them when in a similar situation. Information about the potential health risks of antibiotic use, however, made him reconsider his previous consumption patterns, which had also included not taking the whole course of antibiotics: “When you feel better, you forget about intake times and then you stop for good”. Nevertheless, although perceptions of the potential risks regarding the use of antibiotics varied, risks were always considered at an individual level. While some study participants highlighted the side effects they had felt in their own bodies when using certain antibiotics, others were reluctant to use them without a recommendation by a professional, due to uncertainties regarding what they were actually meant for.
In addition to the uneven access to available information, individuals’ socioeconomic and educational background seemed to also play an important role regarding the kind of knowledge that they were able to mobilise, and their confidence in doing so, especially when managing antibiotics. A higher education and socioeconomic background not only enabled access to a wider range of information sources, such as the Internet—access to which was restricted for the majority of my study participants—but also seemed to influence the way in which such information was retrieved, interpreted and used in their own consumption practices. A clear example of this was related to the vocabulary used to identify the medicines themselves. Although there seemed to be a general awareness amongst most interviewees about the circulating recommendations regarding antibiotic use—as a specific medicinal category that should only be used when recommended by a health professional—some of the study participants did not associate antibiotics with the medicines that they or their family consumed. They knew the generic name of the medicines, but not always the therapeutic category to which they belonged, as shown in the excerpt below:
C: Do you remember the last time you took an antibiotic?
R: Antibiotic, no.
C: And amoxicillin?
R: Amoxicillin, yes. The two-colour pill, right?
(Woman, 29 years)
This mother of two young children, similar to many study participants, referred to antibiotics as ‘capsules’, the ‘two-colour pill’ or the ‘yellow and red pill’, while others called them by their active ingredient, as they were normally prescribed. As a finding during the exploratory phase of the research, this vocabulary dissonance was taken into consideration when designing the household questionnaires. In 17% of cases, respondents were not able to identify what antibiotics meant when asked about ‘the last time they used an antibiotic’. In such cases, examples like those above were given, as a way of making the survey more accurate.
While the uneven articulation of, and access to, different sources of information among the study participants seemed to play a role in terms of how antibiotic use was managed, the terminology used within individuals’ life-world vocabularies also shed light on some of the communication and therapeutic engagement gaps between users and providers (both prescribers and dispensers), which will be discussed in the following section.
Communication with prescribers and the role of dispensers in self-medication practices
The relationships between health professionals and patients, widely explored in the literature (e.g., Kamat and Nichter, 1998), certainly play an important role in self-medication practices. Although the thorough analysis of such multifaceted relationships is beyond the scope of this article, it is noteworthy to briefly articulate different accounts from prescribers, dispensers and users in Maputo to highlight a few points.
Even though, for most study participants, health professionals (medical doctors in particular) were seen as the main (potential) source of expert information about medications, in practice, interactions with health professionals were generally seen as too short and authoritarian. Besides the very limited consultation time in public healthcare services, due to the high number of patients and the insufficiencies in human (and technological) resources (similar to in other low-income and middle-income countries [LMICs]—see for example Pearson et al., 2018), many study participants shared the fact that they did not usually pose questions to medical doctors, as this could be perceived as disrespectful. This often resulted in individuals leaving the consultation room with doubts regarding their treatments, broadening the space for other information and reasonings to prevail when considering their prescription. As a 35-year-old man described,
When you come in [the consultation room] you say: ‘I’m feeling pain here’. And he’s already writing. Already writing, they are fast! So it brings doubts… ‘But is he actually writing what I really feel? In fact, are they working well, these guys?’ There’s that doubt. (Man, 35 years)
The promptness with which medical doctors made prescriptions was sometimes perceived as a lack of ‘good care’ and raised doubts about whether the prescriptions were in fact the most appropriate for their situation. This had implications not only regarding how these professionals were perceived by their patients, but also in terms of how individuals later managed the prescriptions they had received. As some explained, is was not rare in such situations for them to not follow the prescription (or to follow only part of it) and to try to find other solutions elsewhere.
While acknowledging the importance of establishing a good relationship and of improving their communication with patients, some of the prescribers I talked with described how challenging this was in the context of public healthcare services. The following excerpt from a medical doctor working in a health centre outside of the city centre illustrates her constraints when managing consultation times:
In a private system, you have a maximum of 10 patients. Here, no. Here, you have a line of 80 out there [points to the door]. How will you have time to explain all this? Because what happens here is that quality and quantity do not match. You may want to do everything you can, and talk, but time is never enough to talk [about] everything you can because the line is big outside. If you stay longer with a patient, there is another patient outside making noise, complaining: ‘They are not calling us’, ‘It is taking too long’, ‘They went for a walk…’. So, we have to balance things. (Medical doctor, healthcare centre)
The pressure to shorten consultation times led this medical doctor to provide what she considered “essential information” to her patients “whenever possible”. Indeed, as she later added, doctors in general did not tend to provide their patients with much explanation – something that went beyond a matter of time and rather depicted a broader medical attitude towards the role of patients in a consultation encounter. However, what some prescribers considered to be ‘essential information’ was not always in accordance with their patients’ perspectives, and the little information about the prescription provided during a medical appointment sometimes went with a lack of information about the diagnosis itself. In other words, patients were many times left without the information they may consider important to discuss, and thus ended up being excluded from their treatment decisions.
In many cases, pharmacy workers played an important role in filling some of the communication gaps between patients and medical doctors. They acted not only as dispensers (e.g., by sometimes helping clients to choose the most important medicines, when they could not afford to buy the whole prescription list), but were also sources of information (e.g., providing their clients with more information, not only about the medicines they were prescribed but also what they were meant forFootnote 13). Pharmacies were, furthermore, accessible points of healthcare, where many individuals would go for perceived minor ailments before consulting a medical doctor. Moreover, despite the low consultation fees and standardised costs for prescription medication in public healthcare facilities, the often-reported lack of medicines in hospital pharmacies pushed patients to buy their medications at a higher rate in private pharmacies. As a result, and combined with other reported constraints examined in this paper and elsewhere (Rodrigues, 2016, p. 397), some study participants sometimes opted to go directly to a private pharmacyFootnote 14. Therefore, and as is broadly recognised (WHO, 1998), pharmacists and pharmacy workers play an important role in self-medication practices.
According to most of the pharmacy workers I interviewed or talked with, amoxicillin was among the most requested medicines without a prescription for flu, tonsillitis, cough, infections and wounds, among others. Some of these pharmacy workers believed that the problem started with doctors prescribing often without running any tests, which led individuals to follow the same logic. Although this resonated with some of the study participants from the community, the first prescription or recommendation of antibiotics did not always come from medical doctors or prescribing nurses, but from staff working in local pharmacies.
Amoxicillin requests without a prescription increased considerably during the cold season. As one pharmacy technician, who had worked for more than 20 years in different pharmacies around Maputo Province, described:
When cold arrives, the medication is mainly ‘amoxicillins’. In the city centre pharmacies, it is a bit difficult [to sell without a prescription]. But in those pharmacies in the suburbs, amoxicillin is being very much ‘attacked’ without a prescription. The person already knows ‘I want amoxicillin’ or ‘those 2-colour capsules’. If you don’t have a force to stop it [and say no to the client]… But if you do have that force, this pharmacy tomorrow will not sell. (Pharmacy technician)
Although antibiotics cannot officially be sold without a prescription, as in many other settings—especially in LMICs (Morgan et al., 2011)—they were available OTC in many private pharmacies. Pharmacy workers talked about how the competition among pharmacies (also found in other studies, e.g., Adome et al., 1996; Kamat and Nichter, 1998) pressured them to keep their clients happy. While some pharmacies, especially in the city centre, seemed to be stricter in following official rules, as the technical director of one private pharmacy explained, there is no rigid control of their sales:
The Ministry of Health doesn’t have a strict control over private pharmacies. So antibiotics end up being sold. Under normal conditions, they should be justified. Each sale should be justified with a prescription. We do register antibiotic sales. But the number of sales exceeds the number of prescriptions. They exceed [by] a lot! They do have that information in the pharmacies of the National Health Service, because there’s no dispensing without a prescription. So, this control is possible over there. Here, in the private sector, it’s not. (Pharmacy technical director)
While the described lack of regulatory monitoring seemed to give private pharmacies room to make different adjustments to the official rules, the continuous proliferation of private pharmacies around the city increased individuals’ options regarding what to consume and where to buy it.
Discussion
This article has analysed self-medication with antibiotics in light of the everyday practical reasoning (cf. Horlick-Jones et al. 2007) of local users in Maputo, situating such practices within their contextual contingencies and wider therapeutic consumption practices and relationships. As the empirical data shows, antibiotics, whether prescribed or not, are part of individuals’ everyday lives. They were present in almost half of the households I visited and, according to the household survey, one fifth of the respondents had used antibiotics in the month prior to the survey. Although, in most cases, the antibiotics had reportedly been prescribed by a health professional, in around 26% of cases the most recent antibiotic use was based on individuals’ own initiative or following relatives’ or neighbours’ advice.
Despite the considerable prevalence of self-medication practices, antibiotics and other prescription-only pharmaceuticals were seldom used as a first resort. They were amongst the most commonly used medicines, but most individuals tended to start their therapeutic consumption itineraries with ‘home remedies’ such as honey, ginger, and lemon, sometimes together with paracetamol or anti-inflammatory medicines. Only when a certain combination of symptoms was identified, and especially when fever was present, were common antibiotics generally introduced. For suspected conditions where diagnoses are generally based on laboratory tests (such as malaria), individuals were more inclined to seek medical advice in healthcare settings. However, for recurring situations where diagnoses are based on a combination of symptoms (such as tonsillitis), and for problems perceived as minor and/or under their cognitive control, individuals tended to avoid the various constraints of healthcare settings and tried to solve the problem themselves.
The influential role of health professionals, both prescribers and dispensers, in self-medication practices in Maputo was clear at different levels. According to the study participants, the most commonly used antibiotics, particularly amoxicillin but also cotrimoxazole and clavamox, were also the most prescribed and recommended; and the main reported reasons for using prescribed antibiotics, generally described in terms of symptoms—such as cough, fever, wounds and specific pains—were consistent with the main conditions self-treated with antibiotics. Indeed, as many studies have long shown (e.g., Haak, 1988; Hardon, 1991; Nichter and Vuckovic, 1994), previous medical recommendations are not only a point of reference for self-medication, but are also often used as a way of legitimising such practices. As illustrated in Maputo, repeated medical prescriptions and recommendations for common conditions increased individuals’ familiarity with certain pharmaceutical solutions, as well as with the process of identifying the health problem. Yet although they constitute a main reference for self-medication practices, as this and other studies (e.g., Lopes, 2009) have shown, individuals do not simply follow or reproduce previous medical recommendations. Medical prescriptions are evaluated according to an ‘interpretative framework’ (Schutz, 1972), based on individuals’ life-worlds and experiential knowledge, which articulates information collected from a variety of sources, including from health professionals, their personal and socially shared experiences with the medication (Lopes, 2009; Rodrigues, 2016; Fainzang, 2017), experiences with prescribers and dispensers (Kamat and Nichter, 1998), and interpretations of perceived symptoms and medical solutions. Prescriptions are, moreover, adapted according to individuals’ financial conditions, as well as to other meaningful aspects of their everyday lives.
The constructed nature of individuals’ knowledge, which differently incorporates and mobilises appropriations of technical expertise (Giddens, 1990), results in modalities of medicine use that do not always conform to health professionals’ recommendations. In this context, socioeconomic and educational backgrounds also played a role in individuals’ perceived autonomy regarding the management of certain medicines, with highly educated individuals displaying more confidence in self-medicating with antibiotics than other interviewees. They tended to have access to a wider variety of information sources and the perceived literacy necessary to understand and apply technical information to both prescribed and non-prescribed medication use. Most study participants, however, stressed the overall lack of information about medications—including that provided by prescribers, as therapeutic encounters tended to be short, vertical and prescriptive, often preventing individuals from raising questions. This reflects a wider problem of a lack of good communication between prescribing health professionals and patients, something that is widely acknowledged in the literature (see e.g., Gregory et al., 2011).
The sociocultural distancing between medical doctors and patients, especially when the latter were from a lower socio-educational background, was also reflected in the medication vocabulary used. Many individuals in Maputo did not associate some of the medicines they used, such as amoxicillin, with antibiotics. Improving communication between prescribers and users, and adjusting health campaign messages to use more contextually-significant vocabulary, could help improve awareness. However, terminology is only one example of much deeper and structural gaps that shape communication between prescribers and users. The very idea that individuals need to be educated in order to improve both the ‘rational’ use of antibiotics and prescription compliance results from a normative and medical-centred approach which neglects individuals’ engagement in their own healthcare and the ‘social and economic realities’ (Nichter and Vuckovic, 1994) of medicine prescription and use. As previously discussed, compliance tends to emphasise the legitimacy of prescribers’ actions over those of patients (Stevenson et al., 2002). The assumption that individuals should recognise such legitimacy, and therefore follow whatever is prescribed for them (or their children), regards individuals as “passive and obedient recipients of medical instructions” (Stimson, 1974 cited in Conrad, 1985), and neglects other legitimate forms of reasoning which could lead to different actions. It also assumes that medical doctors’ prescriptions are always the most ‘rational’ and legitimate, disregarding issues around over-prescribing, and other prescribing errors, which are repeatedly highlighted in the literature on antibiotics and AMR (e.g., Llor and Bjerrum, 2014), as well as the context of the prescription itself (see also Pearson et al., 2018). Moreover, as Morgan et al. (2011, p. 697) found in their systematic review of non-prescription antimicrobial use worldwide, “[c]lear evidence that antimicrobials obtained without prescription are used less appropriately than prescription antimicrobials does not exist”.
Prescribing is a social exchange (Hall, 1980) and “cannot be easily disengaged from its larger social and cultural contexts” (Pellegrino, 1976). Its legitimacy is contextually assessed, by both patients and prescribers, based on social and medical factors (Stevenson et al., 2002) and thus the act of prescribing at the end of the therapeutic encounter often goes beyond strictly medical purposes. Hence, the repeated argument that the over-prescription of antibiotics is mainly driven by ‘patient demand’ needs to be further deconstructed and analysed in concrete contextual circumstances. As Britten (2008) has pointed out, doctors’ perceptions of patients’ expectations can have a greater influence on prescription patterns than patients’ actual expectations. As empirical examples from Maputo have illustrated, when individuals are not able to solve health-related problems through self-care (or community help) and they decide to navigate the challenges inherent to any public healthcare service in a resource-poor setting, they do expect medical solutions. However, if these solutions—often materialised in prescriptions—are not accompanied by other equally valued elements such as time, care and good communication, important in the construction of a trusting relationship (see Rodrigues, 2016, p. 397), then individuals may leave the consultation room with doubts. Doubts that will, eventually, influence how (if at all) they will use the prescribed solutions. Therefore, prescriptions need to be discussed between prescribers and users to ensure that the most adequate solution to individuals’ life-worlds (Schutz, 1972) and to their socioeconomic conditions is found (see also Zola, 1972).
Finally, as is widely recognised (WHO, 1998), pharmacy workers play an important role in self-medication practices, including in the management of prescribed medicines. They act not only as dispensers, but as sources of information and points of healthcare (see also Ferguson, 1981; Logan, 1988; Kamat and Nichter, 1998). Particularly in contexts where public health services are overloaded and often lack human and technological/material resources, such as Maputo and other LMICs, going directly to a pharmacy is often seen as the most cost-effective solution. The ongoing and growing competition in the pharmacy business in ‘loosely regulated’ contexts (Hardon and Sanabria, 2017), however, results in pharmacy workers feeling pressured to satisfy their clients, which may sometimes conflict with their role as health professionals. Hence, the involvement of pharmacy workers in programmes aimed at improving antibiotic use is important (Saradamma et al., 2000). Yet, while most recommendations to strengthen restrictions on self-medication with antibiotics emphasise the lack of policy enforcement to prohibit OTC sales (e.g., Mitema, 2010; Llor and Bjerrum, 2014), cautions on the balance between restriction and access and the need to consider geographical inequalities have also been raised (e.g., Bloom et al., 2015; Lambert, 2016; Laxminarayan et al., 2016; Khan et al., 2018). Indeed, regulatory measures need to be adjusted to local realities. In resource-limited settings, pharmacies may be the most reliable providers of both general healthcare and life-saving medicines. Moreover, the availability of antibiotics through illegal or informal channels may represent an even bigger challenge. The circulation of unsafe, substandard and/or counterfeit antimicrobials, often dispensed by untrained and uncredited sellers, is a challenge in many countries in the African region and, it has been argued, may accelerate and spread AMR (Ndihokubwayo et al., 2013). These realities need to be considered in regulatory measures and interventions.
Final remarks
Studies from different parts of the world have shown how self-medication is “the most common medical action” (van der Geest et al. 1996, p. 154) and how, in some settings, antibiotics are amongst the most commonly used therapeutic category. Likewise, in Maputo, I found that antibiotics were part of the ‘home pharmacies’ in almost half of the households I visited. By looking at self-medication with antibiotics beyond (non-)prescription use, and by situating individuals’ decisions and practical reasoning within their socioeconomic and therapeutic landscapes in Maputo, this study sought to shed light on the situated rationales of certain consumption practices that do not always follow biomedical recommendations of ‘rational/appropriate use’. Looking at some of the relational and structural factors behind such rationales helps us to deconstruct and further problematise the various legitimate meanings of responsible use. Individuals are actively engaged in therapeutic processes, whether regarding their own or those of their family and community. While this is in accordance with a predominant healthism ideology (Crawford, 1980) that emphasises self-reliance and individual responsibility for one’s own health (Declaration of Alma Ata, 1978), it contrasts with global public health efforts to control antibiotic useFootnote 15. Yet, as part of individuals’ home technologies, antibiotics are embedded in self-care practices. It is therefore important to examine the social, cultural, political and economic contingencies that may influence different antibiotic needs and modalities of use, in “one context at a time” (Lambert, 2016), and to engage with all of the different local actors to improve antibiotic use. In such an approach, individuals’ rationales should not be seen as part of the problem, but should rather be incorporated into the solution. While this study analysed self-medication practices in Mozambique’s capital city, where access to public healthcare services and pharmacies is significantly higher than in the rest of the country, further research is needed to understand self-medication practices and needs in different national settings.
Data availability
The original data generated and/or analysed during this study are not publicly available, as this was not included in the informed consent obtained from study participants.
Change history
06 February 2020
An amendment to this paper has been published and can be accessed via a link at the top of the paper.
Notes
The underlying rationale of such pharmaceutically-driven approaches, especially in Low-Income and Middle-Income Countries, seems now to contrast with current global health efforts to prevent and further regulate the overall use of antibiotics.
The questions were posed in both Portuguese and Changane, and the main questions included: The last time you felt fever/cough/diarrhoea; what did you do; why; did you take any medicine—if so: what did you take, who advised you, where did you get it, for how long did you take it, did it solve the problem?
The main questions included: When was the last time you took an antibiotic (examples provided, if needed); what was the purpose; what did you take; who advised you; where did you get it; for how long did you take it; how many pills per day; how do you evaluate the results?
Referring to data from both sets of questions.
Referring to data exclusively from the set of questions regarding antibiotics.
Of the respondents, 18.8% said they had never used antibiotics, even after the provision of examples of the most common antibiotics in Maputo, as well as other more commonly known terms/terminologies for antibiotics among the community.
According to GARP-Mozambique (2015, p. 2), the high rates of resistance to cotrimoxazole in the country is also a result of “[t]he widespread use of cotrimoxazole as a first-line treatment for acute respiratory infections, as well as to prevent opportunistic infections in people with HIV/AIDS.”
‘Home pharmacy’ is used in this paper as a translation of the Portuguese term farmácia caseira (see e.g., Diehl and Almeida, 2012).
This was the case for antibiotics only in two of the most privileged households.
Ibuprofen was often referred to as a ‘calming’ medicine, as it does not ‘cure the problem’, but calms down bodily pain.
Clavamox contains Amoxicillin and Clavulanic Acid, and was often mentioned by the study participants as prescribed for tonsillitis.
Including, for example, not having the financial means or not wanting to buy the whole prescription (as also reported in other studies, e.g., Kamat and Nichter, 1998).
According to some of the pharmacists interviewed, this information was only shared if the client buying the medicines was also the patient.
As a study conducted by the Maputo City Council (2017) has found, the lack of medicines in public health facilities and time constraints were also the main reasons why some individuals chose to buy medicines at informal markets in Maputo.
https://www.who.int/mediacentre/commentaries/stop-antibiotic-resistance/en/ (last consulted in May 2019).
References
Abraham J (2010) Pharmaceuticalization of society in context: theoretical, empirical and health dimensions. Sociology 44(4):603–622
Adome R, Whyte S, Hardon A (1996) Popular pills: community drug use in Uganda. (Vol. 1). Het Spinhuis, Amsterdam
Albawani SM, Hassan YB, Abd-Aziz N, Gnanasan S (2017) Self-medication with antibiotics in Sana’a City, Yemen. Trop J Pharm Res 16(5):1195–1199
Alghadeer A, Aljuaydi K, Babelghaith S, Alhammad A, Alarifi M (2018) Self-medication with antibiotics in Saudi Arabia. Saudi Pharm J 26(5):719–772
Alhomoud F, Aljamea Z, Almahasnah R et al. (2017) Self-medication and self-prescription with antibiotics in the Middle East – do they really happen? A systematic review of the prevalence, possible reasons, and outcomes. Int J Infect Dis 57:3–12
Barker C (1983) The Mozambique pharmaceutical policy. The Lancet
Baszanger I (1998) Aspects sociologiques–Gérer la migraine: experience, savoir et information des maladies. In: Guevara et al. (eds) La migraine: connaissances descriptives, traitement et prévention. [Rapport de recherche] Institut national de la santé et de la recherche médicale (INSERM), p 251–263
Baxerres C, Le Hesran JY (2006) Le marché parallèle du médicament en milieu rural au Sénégal, Les atouts d’une offre de soins populaire. Anthropologie et Sociétés 30(3):219–230
Biehl J (2007) Pharmaceuticalization: AIDS treatment and global health politics. Anthropological Q 80(4):1083–1126
Biehl J, Petryna A (2013) Critical Global Health. In: Biehl J, Petryna A (eds) When people come first: critical studies in Global Health. Princeton University Press, Princeton
Bledsoe C, Goubaud M (1988) The Reinterpretation and distribution of Western pharmaceuticals: an example from the Mende of Sierra Leone. In: van der Geest S, Whyte SR (eds) The context of medicines in developing countries: studies in pharmaceutical anthropology. Kluwer, Dordrecht, p 253–276
Bloom G, Wilkinson A, Tomson G et al. (2015) Addressing resistance to antibiotics in pluralistic health systems, STEPS Working Paper 84. STEPS Centre, Brighton
Borg MA, Scicluna EA (2002) Over-the-counter acquisition of antibiotics in the Maltese general population. Int J Antimicrobial Agents 20:253–257
Britten N (2008) Medicines and Society–patients, professionals and the dominance of pharmaceuticals. Palgrave MacMillan, Basingstoke
Chandler C (2019) Current accounts of antimicrobial resistance: stabilisation, individualisation and antibiotics as infrastructures. Pal Commun (5)1
Clamote T (2008) Entre pluralismo médico e pluralismo terapêutico: contributos para a revisão de uma narrativa sociológica. In: Full Papers of the 6th Conference of the Portuguese Sociological Association–Mundos Sociais: Saberes e Práticas, Lisboa, Associação Portuguesa de Sociologia
Cohen D, McCubbin M, Collin J, Pérodeau G (2001) Medications as social phenomena. Health 5(4):441–469
Conrad P (1985) The meaning of medications: another look at compliance. Soc Sci Med 20(1):29–37
Conrad P (1992) Medicalization and social control. Annu Rev Sociol 18:209–232
Craig D (2002) Familiar Medicine–everyday health knowledge and practice in today’s Vietnam. University of Hawai’i Press, Honolulu
Crawford R (1980) Healthism and the medicalization of everyday life. Int J Health Serv 10(3):365–388
Cueto M (2013) A return to the magic bullet? Malaria and global health in the twenty-first century. In: Biehl J, Petryna A (eds) When people come first: critical studies in global health. Princeton University Press, Princeton
Declaration of Alma Ata (1978) International conference on primary health care. USSR, Alma Ata. http://www.who.int/hpr/NPH/docs/declaration_almaata.pdf
Dew K, Chamberlain K, Hodgetts D et al. (2014) Home as a hybrid centre of medication practice. Sociol Health Illn 36(1):28–43
Diehl EE, Almeida LK (2012) Medicamentos em contexto local indígena: a “farmácia caseira” Xokleng, Santa Catarina. Rev de Antropologia Soc da UFSCar 4(1):189–206
Donovan J, Blake D (1992) Patient non-compliance: deviance or reasoned decision-making? Soc Sci Med 34(5):507–513
Elmasry A, Bakr A, Kolkailah D et al. (2013) Pattern of antibiotic abuse-a population based study in Cairo. Egypt J Chest Dis Tuberculosis 62:189–195
Etkin ML, Tan NL (eds) (1994) Medicines: meanings and contexts. Health Action Information Network, Quezon City, Philippines
Fainzang S (2017) Self-medication and society-Mirages of autonomy. Routledge, London, New York
Ferguson AE (1981) Commercial pharmaceutical medicine and medicalization: a case study from El Salvador. Cult Med Psychiatry 5:105–134
Freidson E (1960) Client control and medical practice. Am J Sociol 65(4):374–382
Giddens A (1990) Consequences of modernity. Polity Press, Cambridge
Global Antibiotic Resistance Partnership-Mozambique Working Group (2015) Situation Analysis and Recommendations: Antibiotic Use and Resistance in Mozambique. Center for Disease Dynamics, Economics and Policy (CDDEP), Washington, New Delhi
Green J, Thorogood N (2014) Qualitative methods for health research (3rd edn.). Sage, London
Gregory R, Peters E, Slovic P (2011) Making decisions about prescription drugs: a study of doctor-patient communication. Health Risk Soc 13(4):347–371
Grigoryan L, Burgerhof JGM, Haaijer-Ruskamp FM et al. (2007) Is self-medication with antibiotics in Europe driven by prescribed use? J Antimicrobial Chemother 59:152–156
Haak H (1988) Pharmaceuticals in two Brazilian villages: lay practices and perceptions. Soc Sci Med 27(12):1415–1427
Hall D (1980) Prescribing as social exchange. In: Mapes RE (ed) Prescribing practice and drug usage. Croom Helme, London, p 39–57
Hardon A (1991) Confronting Ill health: medicines, self-care and the poor in Manila. Health Action Information Network, Quezon City, Philippines
Hardon A, Sanabria E (2017) Fluid drugs: revisiting the anthropology of pharmaceuticals. Annu Rev Anthropol 46:117–132
Horlick-Jones T, Wall J, Kitzinger J (2007) Bricolage in action: learning about, making sense of, and discussing, issues about genetically modified crops and food. Health Risk Soc 9(1):83–103
INE, Instituto Nacional de Estatística (2019) IV Recenseamento Geral da População e Habitação 2017: Resultados Definitivos - Moçambique. Maputo, Abril 2019
Jaffre Y (1999) Farmacie cittadine, farmacie «per terra». Afr e Mediterr 1(99):31–36
Kamat V, Nichter M (1998) Pharmacies, self-medication and pharmaceutical marketing in Bombay, India. Soc Sci Med 47(6):779–794
Khan M, Rego S, Wu S et al. (2018) Health systems barriers to controlling infectious diseases in low and middle income Asian countries. In Legido-Quigley & Asgari-Jirhandeh (eds) Resilience and people-centred health systems: Progress, challenges and future directions in Asia. World Health Organization, Regional Office for South-East Asia, New Delhi
Lambert H (2016) Tackling drug resistance, one context at a time, Medical Research Council, available online: https://mrc.ukri.org/news/blog/tackling-drug-resistance/
Lambert H, Chen M, Cabral C (2019) Antimicrobial resistance, inflammatory responses: a comparative analysis of pathogenicities, knowledge hybrids and the semantics of antibiotic use. Pal Commun 5(85):1–13
Laxminarayan R, Matsoso P, Pant S et al. (2016) Access to effective antimicrobials: a worldwide challenge. Lancet 387:168–175
Llor C, Bjerrum L (2014) Antimicrobial resistance: risk associated with antibiotic overuse and initiatives to reduce the problem. Therapeutic Adv Drug Saf 5(6):229–241
Logan K (1988) ‘Casi como doctor’: pharmacists and their clients in a Mexican urban context. In: van der Geest, Whyte (eds) The context of medicines in developing countries: studies in pharmaceutical anthropology. Kluwer, Dordrecht
Lopes N (2003) Automedicação: práticas e racionalidades sociais. PhD Dissertation, ISCTE, Lisbon
Lopes N (2009) Changing self-medication practices, lay knowledge and rationales. RCCS Annu Rev [Online], 1:36–54. https://journals.openedition.org/rccsar/143
Lopes N (org.) (2010) Medicamentos e pluralismo terapêutico: práticas e lógicas sociais em mudança. Afrontamento, Porto
Conselho Municipal do Município de Maputo [Maputo City Council] (2017) Venda informal de medicamentos na Cidade de Maputo, Causas e Consequências para a Saúde Pública. Relatório de Pesquisa
Ministério da Saúde (MISAU), Instituto Nacional de Estatística (INE) e ICF International (ICFI) (2011) Moçambique: Inquérito Demográfico e de Saúde. MISAU, INE e ICFI, Calverton, Maryland
MISAU (2013) Plano Estratégico do Sector da Saúde–PESS 2014-2019 [Strategic plan for the health sector 2014–2019]. Governo de Moçambique, Maputo
MISAU (2012) Relatório da Revisão do Sector da Saúde. Governo de Moçambique, Maputo
Mitema ES (2010) The Role of Unregulated Sale and Dispensing of Antimicrobial Agents on the Development of Antimicrobial Resistance in Developing Countries. In: Sosa et al. (eds) Antimicrobial resistance in developing countries. Springer-Verlag, New York
Morgan D, Okeke I, Laxminarayan R et al. (2011) Non-prescription antimicrobial use worldwide: a systematic review. Lancet Infect Dis 11:692–701
Ndihokubwayo JB, Yahaya AA, Desta AT et al. (2013) Antimicrobial resistance in the African Region: issues, challenges and actions proposed. Afr Health Monit 16:27–30
Nichter M (1989) South Asian case studies. Kluwer Academic Publishers, Dordrecht
Nichter M (1980) The layperson’s perspective of medicine as perspective into the utilization of multiple therapy systems in the Indian context. Soc Sci Med 14B(4):225–233
Nichter M, Vuckovic N (1994) Agenda for an anthropology of pharmaceutical practice. Soc Sci Med 39(11):1509–1525
Pearson M, Doble A, Glogowski R et al. (2018) Antibiotic Prescribing and Resistance: views from LMIC prescribing and dispensing professionals. Report to World Health Organisation AMR Secretariat, available online at https://www.who.int/antimicrobial-resistance/LSHTM-Antibiotic-Prescribing-LMIC-Prescribing-and-Dispensing-2017.pdf
Pellegrino ED (1976) Prescribing and drug ingestion: symbols and substances. Drug Intell Clin Pharm 10:624–630
Rodrigues CF (2016) Medicines and Therapeutic Pluralism in Maputo: exploring modalities of trust and the (un)certainties of everyday users. Health Risk Soc 18(7–8):385–406
Sánchez AJ (2016) Marcos formales, recorridos informales: las lógicas del consumo terapéutico en Guinea Ecuatorial. PhD Thesis, Universidad de Castilla-La Mancha
Saradamma RD, Higginbotham N, Nichter M (2000) Social factors influencing the acquisition of antibiotics without prescription in Kerala State, south India. Soc Sci Med 50(6):891–903
Schutz A (1972) The phenomenology of the social world. Heinemann, London, [1932]
Stevenson F, Britten N, Barry C et al. (2002) Perceptions of legitimacy: the influence on medicine taking and prescribing. Health 6(1):85–104
Stimson GV (1974) Obeying doctor’s orders: A view from the other side. Soc Sci Med 8(2):97–104
Tan ML (1999) Good medicine: pharmaceuticals and the construction of power and knowledge in the Philippines. Het Spinhuis, Amsterdam
UN-HABITAT (2010) Mozambican cities profile: Maputo, Nacala and Manica. Retrieved from http://unhabitat.org/books/mozambique-cities-profile-maputo-nacala-and-manica/
Van der Geest S (1987) Self-care and the informal sale of drugs in South Cameroon. Soc Sci Med 25(3):293–305
Van der Geest S, Hardon A (1990) Self-medication in developing countries. J Soc Adm Pharm 7(4):199–204
Van der Geest S, Whyte S (1989) The charm of medicines: metaphors and metonyms. Med Anthropol Q 3(4):345–367
Van der Geest S, Whyte S, Hardon A (1996) The anthropology of pharmaceuticals-a biographical approach. Annu Rev Anthropol 25:153–178
WHO (1998) The role of the pharmacist in self-care and self-medication: report of the 4th WHO Consultative Group on the Role of the Pharmacist, The Hague, The Netherlands, 26–28 August. World Health Organization. https://apps.who.int/iris/handle/10665/65860
WHO (2000) The benefits and risks of self-medication. WHO Drug Information 14(1):1–2
WHO (2007) Access to essential medicines. WHO Drug Information 21(4):267–269
WHO (2015a) Global action plan on antimicrobial resistance. World Health Organization. http://www.who.int/iris/handle/10665/193736
WHO (2015b) Worldwide Country Situation Analysis: response to antimicrobial resistance. World Health Organization. https://apps.who.int/iris/handle/10665/163473
Whyte SR (1988) The power of medicines in East Africa. In: Whyte, Van der Geest (eds) The context of medicines in developing countries: studies in pharmaceutical anthropology. Kluwer Academic Publishers, Dordrecht
Whyte SR, van der Geest S, Hardon A (2002) Social lives of medicines. Cambridge University Press, Cambridge
Williams S, Martin P, Gabe J (2011) The pharmaceuticalisation of society? A framework for analysis. Sociol Health Illn 33(5):710–725
Willis LD, Chandler C (2019) Quick fix for care, productivity, hygiene and inequality: reframing the entrenched problem of antibiotic overuse. BMJ Global Health 4(4):e001590
Zola IK (1972) Medicine as an institution of social control. Sociological Rev 20(4):487–504
Acknowledgements
This research was supported by the Portuguese national funding agency for science, research and technology (FCT) under Grant SFRH/BD/78172/2011. I am grateful to all the study participants who shared their time and experiences with me; to the support provided by my colleagues and sociology students from Eduardo Mondlane University; and to the constructive inputs received from Noémia Lopes, Anita Hardon, Trudie Gerrits and other colleagues, from both the University of Amsterdam and the University of Bristol, on earlier versions of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The author declares no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rodrigues, C.F. Self-medication with antibiotics in Maputo, Mozambique: practices, rationales and relationships. Palgrave Commun 6, 6 (2020). https://doi.org/10.1057/s41599-019-0385-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1057/s41599-019-0385-8
This article is cited by
-
Susceptibility antibiotic screening reveals high rates of multidrug resistance of Salmonella, Shigella and Campylobacter in HIV infected and uninfected patients from Mozambique
BMC Infectious Diseases (2023)
-
Prevalence and antimicrobial resistance patterns of microbes isolated from individuals attending private diagnostic centre in Cape Coast Metropolis of Ghana
Scientific Reports (2022)
-
The potential impact of the COVID-19 pandemic on antimicrobial resistance and antibiotic stewardship
VirusDisease (2021)