Abstract
Chronic inflammation induced by hypoxia during sleep is an important mechanism of microvascular damage in OSA patients. In this study, we investigated the role of the sphingosine rheostat, which has diverse inflammatory effects. Thirty-seven healthy subjects and 31 patients with OSA were recruited. We collected data on demographics and comorbidities. Plasma sphingosine-1-phosphate and ceramide antibody concentrations were measured by ELISA. The results were compared between the OSA and control groups, and the correlations between these measurements and markers of disease severity and comorbidities were explored. Ceramide antibody levels were significantly elevated in OSA patients (892.17 ng/ml) vs. controls (209.55 ng/ml). S1P levels were also significantly higher in patients with OSA (1760.0 pg/ml) than in controls (290.35 pg/ml, p < 0.001). The ceramide antibody concentration showed correlations with BMI (ρ = 0.25, p = 0.04), CRP (ρ = 0.36, p = 0.005), AHI (ρ = 0.43, p < 0.001), ODI (ρ = 0.43, p < 0.001), TST90% (ρ = 0.35, p = 0.004) and the lowest oxygen saturation (ρ = 0.37, p = 0.001) in the whole study population but not when patients with OSA were analyzed separately. The elevated ceramide antibody and sphingosine-1-phosphate concentrations in patients suffering from OSA suggests their involvement in the pathomechanism of OSA and its comorbidities.
Similar content being viewed by others
Introduction
Obstructive sleep apnea (OSA) is a disorder that is defined by the repeated collapse of the pharyngeal airways during sleep. It is a risk factor for the development of cardiovascular disease, with vascular inflammation induced by chronic intermittent hypoxemia playing a part1. However, despite extensive research, the elements of vascular inflammation in OSA are not fully defined. Identification of these processes may reveal potential treatable traits, as unfortunately, the current gold standard treatment for OSA, that is, continuous positive airway pressure (CPAP) therapy, has not been proven to reduce cardiovascular risk2.
Sphingolipids are lipid mediators that play a critical role in cellular membrane formation, cell proliferation, and apoptosis and have autocrine roles in regulating inflammation and coagulation3,4. In line with this, they are involved in various autoimmune, cardiovascular and metabolic diseases as well as malignancies5,6,7,8,9,10.
Ceramides have a central role in the metabolism of sphingolipids. Their production is induced by proinflammatory cytokines, such as tumor necrosis factor-α (TNF-α) or interleukin 1β3, which are both increased in OSA11. Once released, ceramides are bound to low-density lipoprotein (LDL) particles and are involved in the development of insulin resistance and the promotion of inflammation12. Ceramides might play a role in endothelial dysfunction by inducing apoptosis in endothelial cells in response to stress stimuli13. In radiation-induced inflammation, anti-ceramide antibodies have a protective role against inflammation14. There is also evidence that antibodies against gangliosides, another group of sphingolipids, play a role in nerve damage in a variety of neurological disorders (e.g., multiple sclerosis and peripheral nerve damage)15,16,17,18. Anti-ceramide antibodies can disrupt and alter the ceramide signaling pathway. Along these lines, monoclonal antibodies targeting sphingolipid signaling pathways have been intensively studied for the treatment of cancer19. Ceramides can further be metabolized to sphingosine 1-phosphate (S1P), which is another important molecule involved in inflammation3. Similar to ceramides, the production of S1P is induced by TNF-α in addition to thrombin and growth factors, such as vascular endothelial growth factor (VEGF)4. Both thrombin20 and VEGF21 are elevated in OSA, pointing toward the theoretically increased production of S1P. Following secretion, S1P is mainly bound to apolipoprotein M on high-density lipoprotein (HDL) particles22. S1P has a dual role in atherosclerosis. On the one hand, it contributes to vasodilation by activating endothelial nitric oxide synthase23. On the other hand, it induces the production of chemokine (C–C motif) ligand 20, which is a potent lymphokine24, and potentiates the release of procoagulant and adhesive molecules from platelets, such as P-selectin or von Willebrand factor4. The latter two molecules were shown to be increased in OSA25,26.
Despite the aforementioned evidence that ceramides and S1P may play a role in OSA, they have not been investigated before. Therefore, the aim of our study was to analyze these molecules in subjects with and without OSA. We also correlated their concentrations to markers of disease severity and associated comorbidities.
Materials and methods
Subjects and design
Sixty-eight participants were recruited from those patients who were referred to the Sleep Unit of the Department of Pulmonology, Semmelweis University, due to suspected OSA (i.e., snoring, witnessed apneas, daytime somnolence and/or comorbidities). None of the patients had previously been diagnosed with OSA, nor had they been treated with CPAP or mandibular advancement devices. Exclusion criteria included any uncontrolled chronic disease, history of any malignancy within 10 years, and infection within 2 months. Data for screen failures were not captured.
In the evening, after participants had filled out the Epworth Sleepiness Scale (ESS) and their medical history was recorded, venous blood was collected into EDTA tubes for biomarker measurement. This was followed by an attended full-night polysomnography or cardiorespiratory polygraphy.
The study was approved by the local Ethics Committee (Semmelweis University, TUKEB 30/2014 and RKEB 172/2018), and informed consent was obtained from all participating volunteers. All measurements were performed in accordance with the relevant guidelines and regulations.
ELISA measurements
EDTA-treated blood samples were centrifuged within 2 h at 1500 RPM for 10 min at 4 °C. Immediately following centrifugation, plasma was separated into 250-µL aliquots, which were stored at − 80 °C until analysis. Samples were thawed just before the ELISA measurements. The MBS3804520 Human Ceramide Antibody ELISA Kit and MBS2516132 Human S1P (sphingosine-1-phosphate) ELISA Kit were used to determine the plasma levels of ceramide antibody and sphingosine-1-phosphate, respectively (MyBioSource, San Diego, California, USA). We followed the manufacturer’s manual to measure these biomarkers; the samples were diluted eight-fold before measurements. Blood samples were measured in duplicate, and the intra-assay variation coefficients were 8.6% for the ceramide antibody assay and 4.2% for the sphingosine-1-phosphate assay.
Sleep studies
Inpatient overnight polysomnography (n = 41) and cardiorespiratory polygraphy (n = 27) were performed using Somnoscreen Plus Tele PSG and RC devices (Somnomedics GMBH Germany). Sleep stages, movements and cardiopulmonary events were scored manually according to the American Academy of Sleep Medicine (AASM) guidelines27. The total sleep time (TST), sleep period time (SPT) and minimum oxygen saturation (MinSatO2) were recorded. Apnea was defined as at least 90% nasal airflow reduction lasting for at least 10 s, while hypopnea was defined as at least 30% nasal airflow reduction lasting for at least 10 s that was associated with at least 3% desaturation (for both polysomnography and polygraphy) or arousal (for polysomnography). The apnea–hypopnea index (AHI), oxygen desaturation index (ODI), and percentage of total sleep time spent with oxygen saturation below 90% (TST90%) were calculated. An AHI ≥ 5/hour was diagnostic for OSA. The patient group was divided into the mild (AHI 5–14.9/hour), moderate (AHI 15–29.9/hour) and severe subgroups (AHI ≥ 30/hour).
Statistical analysis
The Shapiro‒Wilks test was used to test and assess normality, which showed a nonparametric distribution for ceramide antibody and S1P levels. The Mann‒Whitney U test and chi-square test were used to compare clinical and demographic characteristics as well as biomarker levels between the OSA and control groups. We applied a nonparametric analysis of covariance (ANCOVA) test adjusted for age, sex and body mass index (BMI) to investigate the differences in biomarker levels between patients and controls. Nonparametric ANCOVA, adjusted for age, sex and BMI, was also applied to investigate the relationship between biomarkers and disease severity stratified by the AHI followed by Tukey’s post hoc test. Plasma biomarker levels were correlated with clinical variables by using Spearman’s test and logistic regression analysis. Statistical analyses were carried out with JASP 0.14.1 (University of Amsterdam, Amsterdam, The Netherlands) and R v. 4.1.3 (R Statistical Foundation, Vienna, Austria). Graphs were plotted with the ggplot2 package for R. p values < 0.05 were considered significant. Data are presented as the mean ± SD or the median and range. The sample size was estimated to detect differences of at least 70% of the standard deviation (0.70 effect size) in either ceramide antibody or S1P levels between the two groups with a power of 0.80 and α error probability of 0.0528.
Results
Demographic characteristics
A summary of the descriptive statistics can be found in Table 1. The subjects with OSA were older and had a higher BMI. There were more subjects with hypertension among the patients. There was no significant difference in the distribution of diabetes mellitus type 2 or cardiovascular disease. Patients with OSA had significantly higher CRP, triglyceride, AHI, and oxygen desaturation index (ODI) levels and significantly lower HDL-C levels; however, there was no difference between the Epworth Sleepiness Scale scores.
Ceramide antibody levels
Ceramide antibody levels were 209.55 ng/ml (36.02–1725.29) vs. 892.17 ng/ml (4.02–1494.21) in controls and OSA patients, respectively (p < 0.001, Fig. 1). The difference remained significant following the adjustment for age, sex, and BMI (p < 0.001).
Correlation between clinical variables and ceramide antibody levels
We found a significant correlation between the ceramide antibody concentrations and clinical variables in the whole study population. There was a direct correlation with BMI (ρ = 0.25, p = 0.04), CRP (ρ = 0.36, p = 0.005), AHI (ρ = 0.43, p < 0.001), ODI (ρ = 0.43, p < 0.001) and TST90% (ρ = 0.35, p = 0.004). On the other hand, a significant inverse correlation was identified between ceramide antibody levels and the lowest levels of oxygen saturation (ρ = − 0.37, p = 0.001). Ceramide antibody concentrations proved to be independent of sex (p = 0.70) and the presence of hypertension (p = 0.36), diabetes mellitus (p = 0.79) and cardiovascular disease (p = 0.16). Ceramide antibody levels did not correlate with age, lipid values or the ESS (all p > 0.05).
When dividing patients into mild (n = 8), moderate (n = 14) and severe (n = 9) subgroups, ceramide antibody levels were in each OSA severity subgroup compared to controls (p = 0.02, p = 0.02, p = 0.008 for mild, moderate and severe subgroups, respectively, Fig. 2); however, there was no difference between any of the OSA subgroups. In line with this, analyzing patients with OSA separately, there was no correlation between ceramide antibody levels and markers of disease severity.
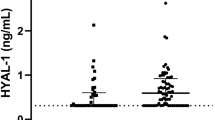
Sphingosine-1-phosphate levels
S1P levels were significantly higher in patients with OSA (1760.0 pg/ml, 99.13–1760.0) than in controls (290.35 pg/ml, 41.68–1760.0, p < 0.001). This difference was still significant following adjustment for age, sex, and BMI (p < 0.001). However, most patients had an S1P level above the upper limit of the ELISA kit. These values were treated as the upper limit value. Therefore, we did not proceed with further subgroup or correlation analyses. The graphical representation of S1P values can be seen in Fig. 3.
Discussion
We found that the levels of S1P and ceramide antibodies are elevated in patients with OSA, suggesting that sphingolipids are involved in the pathomechanism of OSA.
Ceramide antibodies are already upregulated in patients with mild OSA disease. Due to the cross-sectional nature of the study, the reasons for the increase can only be hypothesized. OSA is associated with systemic inflammation11, which can induce ceramide synthesis3. In line with this, C-reactive protein levels were increased in patients with OSA and correlated with ceramide antibody concentrations. Anti-sphingolipid antibodies were shown to exhibit a T-cell-independent inflammatory response15. In addition, ceramide production is directly augmented by hypoxemia29, which could be the reason for the direct correlation between ceramide antibody concentrations and markers of overnight hypoxemia. We also found a significant correlation between BMI and ceramide antibody levels. There is a strong relationship between obesity and ceramide metabolism, as white adipose tissue contains large amounts of sphingolipids30. However, the relationship between ceramide antibodies and the AHI was stronger than that with BMI. Moreover, differences between the OSA and control groups were present following adjustment for BMI. These results suggest that increased ceramide antibody levels in OSA were not due to obesity; however, this needs to be investigated in certain interventional experimental settings (i.e., changes in ceramide antibody levels either following weight loss or CPAP). Ceramides are also involved in the regulation of body weight and energy homeostasis31. It is therefore possible that the elevated ceramide antibody levels are the cause rather than the consequence of high body weight. Nevertheless, the relationship between BMI and ceramides could be essential in OSA, as it has recently been shown that OSA-associated cardiovascular risk is significantly driven by obesity32. Ceramides are proapoptotic molecules33 and could potentially contribute to the increased apoptotic potential in OSA34. In particular, they promote the downregulation of survivin33, which is consistent with the decreased survivin concentrations in OSA35. Interestingly, ceramides also increase the production of the anti-inflammatory clusterin36, which was reported to be elevated in OSA37. In addition, ceramides play a role in hypoxia-related vasoconstriction38. Elevated ceramide levels in plasma membranes will create rafts that have certain receptor configurations39,40. The binding of antibodies to these ceramide-rich rafts could change the configuration of plasma membrane rafts and counteract the effect of ceramide accumulation. Antibodies against ceramide might have a protective effect against hypoxia-induced inflammation, as these antibodies were described to be effective against radiation-induced gut inflammation and leprosy-associated nerve damage14,18. This is in accordance with our results, which suggest that ceramide antibody levels are elevated in OSA and are correlated with markers of disease severity. To counteract increased ceramide signaling, whether this elevation is a passive consequence of elevated ceramide production or a negative feedback mechanism needs to be investigated.
A potential consequence of increased ceramide levels is the increased production of S1P. Ceramides are metabolized into sphingosine and subsequently into S1P. This route is facilitated by ceramidase and sphingosine kinases4. Sphingosine kinases are activated by growth factors, insulin and TNF-α25, which could be involved in OSA11,21. Several cell types can release S1P into the circulation, including immune cells, endothelial cells, fibroblasts, and erythrocytes, but it seems that most of the plasma S1P is released during platelet activation4. Therefore, high S1P levels could be due to accelerated coagulation and platelet activation in OSA41. The fact that most of the S1P concentrations were above the upper limit of detection in OSA prevented us from performing further exploratory analyses. However, high S1P levels could potentially explain some OSA-related changes. For instance, S1P stimulates the secretion of cortisol42 and aldosterone43, both of which are elevated in OSA44,45 and thus contribute to hypertension and insulin resistance. In addition, sphingosine-1-phosphate has a diverse role in the inflammatory response, such as facilitating the extravasation of lymphocytes from lymphatic tissue46, inducing inflammation through CXCL-10 and CCL-547 and altering a cell’s gene expression by modulating histone-deacetylases48. Sphingosine-1-phosphate is associated with cardiovascular disease49 and inflammation caused by intermittent hypoxia50. However, our results warrant further investigation into these hypotheses, as S1P seems to be a promising protective biomarker in hypoxia-induced inflammation in OSA and cardiovascular comorbidities. Elevated S1P maintains endothelial barrier function and could be a mechanism to counteract inflammation of the microvessels, which is known to be associated with OSA7. However, the angiogenic effects of S1P are (at least partially) mediated through low-density lipoprotein receptor-related protein 151, which was found to be decreased in OSA52. Therefore, it is possible that the pathogenic roles of S1P overwhelm the protective functions.
Our study has some limitations. First, although it was powered to detect differences in either ceramide antibody or S1P levels between the two groups, the sample size might be too small to draw conclusions on correlations and subgroup differences. Even though the number of participants was determined based on the power calculation, the number of subjects is low, which adds to the limitations of the overall study. Therefore, our conclusions discussed above need to be tested by further studies. Second, the study had a cross-sectional design, and the causality between OSA and sphingolipid metabolism needs to be confirmed by interventional studies with CPAP. We believe our results will serve as the basis to design such studies. Third, previous evidence suggests that there are high ceramide levels in adipose tissues30. Although OSA was associated with high ceramide antibody concentrations independent of BMI, to better understand the effect of OSA on sphingolipid concentrations, comparisons should be performed in lean (BMI < 25 kg/m2) subjects. As only 3 patients with OSA fell into this category, we did not proceed with a further assessment. Finally, we used cardiorespiratory polygraphy instead of polysomnography as a diagnostic test in some individuals. Polygraphy is an accepted diagnostic test; however, it tends to underestimate disease severity, as it does not capture hypopneas associated with arousals and may overestimate the total sleep time32. This discrepancy could have potentially led to inaccuracies when investigating the correlations between biomarkers and markers of disease severity.
In conclusion, this study is the first to investigate the potential role of sphingolipid metabolism in OSA and its comorbidities. We have found that both sphingosine-1-phosphate and ceramide antibody levels are elevated in patients with OSA. Further investigation is needed to better understand these findings and to reveal the exact role of sphingolipid metabolism in the pathogenesis of OSA and its associated comorbidities.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Chiang, C. L. et al. Comorbidities and risk of mortality in patients with sleep apnea. Ann. Med. 49, 377–383. https://doi.org/10.1080/07853890.2017.1282167 (2017).
McEvoy, R. D. et al. CPAP for prevention of cardiovascular events in obstructive sleep apnea. N. Engl. J. Med. 375, 919–931. https://doi.org/10.1056/NEJMoa1606599 (2016).
Gomez-Muñoz, A. et al. Control of inflammatory responses by ceramide, sphingosine 1-phosphate and ceramide 1-phosphate. Prog. Lipid Res. 61, 51–62. https://doi.org/10.1016/j.plipres.2015.09.002 (2016).
Obinata, H. & Hla, T. Sphingosine 1-phosphate in coagulation and inflammation. Semin. Immunopathol. 34, 73–91. https://doi.org/10.1007/s00281-011-0287-3 (2012).
Berwick, M. L., Dudley, B. A., Maus, K. & Chalfant, C. E. The role of ceramide 1-phosphate in inflammation, cellular proliferation, and wound healing. Adv. Exp. Med. Biol. 1159, 65–77. https://doi.org/10.1007/978-3-030-21162-2_5 (2019).
Cremesti, A. et al. Ceramide enables fas to cap and kill. J. Biol. Chem. 276, 23954–23961. https://doi.org/10.1074/jbc.M101866200 (2001).
Hla, T. & Dannenberg, A. J. Sphingolipid signaling in metabolic disorders. Cell Metab. 16, 420–434. https://doi.org/10.1016/j.cmet.2012.06.017 (2012).
Stith, J. L., Velazquez, F. N. & Obeid, L. M. Advances in determining signaling mechanisms of ceramide and role in disease. J. Lipid Res. 60, 913–918. https://doi.org/10.1194/jlr.S092874 (2019).
Ruvolo, P. P. Intracellular signal transduction pathways activated by ceramide and its metabolites. Pharmacol. Res. 47, 383–392. https://doi.org/10.1016/s1043-6618(03)00050-1 (2003).
Maceyka, M. & Spiegel, S. Sphingolipid metabolites in inflammatory disease. Nature 510, 58–67. https://doi.org/10.1038/nature13475 (2014).
Unnikrishnan, D., Jun, J. & Polotsky, V. Inflammation in sleep apnea: An update. Rev. Endocr. Metab. Disord. 16, 25–34. https://doi.org/10.1007/s11154-014-9304-x (2015).
Boon, J. et al. Ceramides contained in LDL are elevated in type 2 diabetes and promote inflammation and skeletal muscle insulin resistance. Diabetes 62, 401–410. https://doi.org/10.2337/db12-0686 (2013).
Paris, F. et al. Endothelial apoptosis as the primary lesion initiating intestinal radiation damage in mice. Science 293, 293–297. https://doi.org/10.1126/science.1060191 (2001).
Rotolo, J. et al. Anti-ceramide antibody prevents the radiation gastrointestinal syndrome in mice. J. Clin. Invest. 122, 1786–1790. https://doi.org/10.1172/jci59920 (2012).
Freimer, M. L., McIntosh, K., Adams, R. A., Alving, C. R. & Drachman, D. B. Gangliosides elicit a T-cell independent antibody response. J. Autoimmun. 6, 281–289. https://doi.org/10.1006/jaut.1993.1024 (1993).
Kasai, N., Pachner, A. R. & Yu, R. K. Anti-glycolipid antibodies and their immune complexes in multiple sclerosis. J. Neurol. Sci. 75, 33–42. https://doi.org/10.1016/0022-510x(86)90048-1 (1986).
Podbielska, M., Ariga, T. & Pokryszko-Dragan, A. Sphingolipid players in multiple sclerosis: Their influence on the initiation and course of the disease. Int. J. Mol. Sci. 23, 258. https://doi.org/10.3390/ijms23105330 (2022).
Zaky, M., Obaid, Z., Khedr, M., El-Sokkary, H. & Elsaie, M. Implications of serum anti-ceramide antibodies and interleukin 4 on nerve damage and physical impairments among leprotic patients: A case-controlled study. J. Drugs Dermatol. 21, 284–291. https://doi.org/10.36849/jdd.5543 (2022).
Zhang, L. et al. Anti-S1P antibody as a novel therapeutic strategy for VEGFR TKI-resistant renal cancer. Clin. Cancer Res. 21, 1925–1934. https://doi.org/10.1158/1078-0432.Ccr-14-2031 (2015).
Fernández-Bello, I. et al. Procoagulant state of sleep apnea depends on systemic inflammation and endothelial damage. Arch. Bronconeumol. 58, 117–124. https://doi.org/10.1016/j.arbres.2020.11.017 (2022).
Briançon-Marjollet, A. et al. Altered in vitro endothelial repair and monocyte migration in obstructive sleep apnea: Implication of VEGF and CRP. Sleep 37, 1825–1832. https://doi.org/10.5665/sleep.4180 (2014).
Christoffersen, C. et al. Endothelium-protective sphingosine-1-phosphate provided by HDL-associated apolipoprotein M. Proc. Natl. Acad. Sci. U. S. A. 108, 9613–9618. https://doi.org/10.1073/pnas.1103187108 (2011).
Nofer, J. R. et al. HDL induces NO-dependent vasorelaxation via the lysophospholipid receptor S1P3. J. Clin. Invest. 113, 569–581. https://doi.org/10.1172/jci18004 (2004).
Kawa, Y. et al. Role of S1P/S1PR3 axis in release of CCL20 from human bronchial epithelial cells. PLoS ONE 13, e0203211. https://doi.org/10.1371/journal.pone.0203211 (2018).
Horváth, P. et al. Circulating P-selectin glycoprotein ligand 1 and P-selectin levels in obstructive sleep apnea patients. Lung 198, 173–179. https://doi.org/10.1007/s00408-019-00299-0 (2020).
Gao, S. et al. Complement promotes endothelial von Willebrand factor and angiopoietin-2 release in obstructive sleep apnea. Sleep 44, 4. https://doi.org/10.1093/sleep/zsaa286 (2021).
Berry, R. B. et al. Rules for scoring respiratory events in sleep: Update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J. Clin. Sleep 8, 597–619. https://doi.org/10.5664/jcsm.2172 (2012).
Faul, F., Erdfelder, E., Buchner, A. & Lang, A.-G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 41, 1149–1160. https://doi.org/10.3758/BRM.41.4.1149 (2009).
Xia, Q. S. et al. New role for ceramide in hypoxia and insulin resistance. World J. Gastroenterol. 26, 2177–2186. https://doi.org/10.3748/wjg.v26.i18.2177 (2020).
Juchnicka, I., Kuźmicki, M. & Szamatowicz, J. Ceramides and sphingosino-1-phosphate in obesity. Front. Endocrinol. (Lausanne) 12, 635995. https://doi.org/10.3389/fendo.2021.635995 (2021).
Nordström, V. et al. Neuronal expression of glucosylceramide synthase in central nervous system regulates body weight and energy homeostasis. PLoS Biol. 11, e1001506. https://doi.org/10.1371/journal.pbio.1001506 (2013).
Carratù, P. et al. Relationships between obstructive sleep apnea syndrome and cardiovascular risk in a naïve population of southern Italy. Int. J. Clin. Pract. 75, e14952. https://doi.org/10.1111/ijcp.14952 (2021).
Morad, S. A. F. & Cabot, M. C. Ceramide-orchestrated signalling in cancer cells. Nat. Rev. Cancer 13, 51–65. https://doi.org/10.1038/nrc3398 (2013).
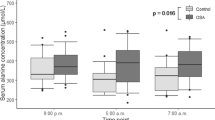
Bikov, A. et al. Diurnal variation of circulating microvesicles is associated with the severity of obstructive sleep apnoea. Sleep Breath 21, 595–600. https://doi.org/10.1007/s11325-017-1464-y (2017).
Kunos, L. et al. Circulating survivin levels in obstructive sleep apnoea. Lung 196, 417–424. https://doi.org/10.1007/s00408-018-0120-z (2018).
Calvo, E. L. et al. Clusterin overexpression in rat pancreas during the acute phase of pancreatitis and pancreatic development. Eur. J. Biochem. 254, 282–289. https://doi.org/10.1046/j.1432-1327.1998.2540282.x (1998).
Meszaros, M. et al. Circulating levels of clusterin and complement factor H in patients with obstructive sleep apnea. Biomark. Med. 15, 323–330. https://doi.org/10.2217/bmm-2020-0533 (2021).
Moreno, L. et al. Ceramide mediates acute oxygen sensing in vascular tissues. Antioxid. Redox Signal 20, 1–14. https://doi.org/10.1089/ars.2012.4752 (2014).
Albeituni, S. & Stiban, J. Roles of ceramides and other sphingolipids in immune cell function and inflammation. Adv. Exp. Med. Biol. 1161, 169–191. https://doi.org/10.1007/978-3-030-21735-8_15 (2019).
Elsherbini, A. et al. Extracellular vesicles containing ceramide-rich platforms: “Mobile Raft” isolation and analysis. Methods Mol. Biol. 2187, 87–98. https://doi.org/10.1007/978-1-0716-0814-2_5 (2021).
Bikov, A., Meszaros, M. & Schwarz, E. I. Coagulation and fibrinolysis in obstructive sleep apnoea. Int. J. Mol. Sci. 22, 2834. https://doi.org/10.3390/ijms22062834 (2021).
Rábano, M. et al. Sphingosine-1-phosphate stimulates cortisol secretion. FEBS Lett. 535, 101–105. https://doi.org/10.1016/S0014-5793(02)03882-6 (2003).
Brizuela, L. et al. Sphingosine 1-phosphate: A novel stimulator of aldosterone secretion. J. Lipid Res. 47, 1238–1249. https://doi.org/10.1194/jlr.M500510-JLR200 (2006).
Kritikou, I. et al. Sleep apnoea and the hypothalamic-pituitary-adrenal axis in men and women: Effects of continuous positive airway pressure. Eur. Respir. J. 47, 531–540. https://doi.org/10.1183/13993003.00319-2015 (2016).
Wang, Y. et al. The role of aldosterone in OSA and OSA-related hypertension. Front. Endocrinol. (Lausanne) 12, 801689. https://doi.org/10.3389/fendo.2021.801689 (2021).
Cyster, J. G. & Schwab, S. R. Sphingosine-1-phosphate and lymphocyte egress from lymphoid organs. Annu. Rev. Immunol. 30, 69–94. https://doi.org/10.1146/annurev-immunol-020711-075011 (2012).
Harikumar, K. B. et al. K63-linked polyubiquitination of transcription factor IRF1 is essential for IL-1-induced production of chemokines CXCL10 and CCL5. Nat. Immunol. 15, 231–238. https://doi.org/10.1038/ni.2810 (2014).
Hait, N. C. et al. Regulation of histone acetylation in the nucleus by sphingosine-1-phosphate. Science 325, 1254–1257. https://doi.org/10.1126/science.1176709 (2009).
McGranaghan, P. et al. Lipid metabolite biomarkers in cardiovascular disease: Discovery and biomechanism translation from human studies. Metabolites 11, 621. https://doi.org/10.3390/metabo11090621 (2021).
Yu, F. C. et al. Protective effect of sphingosine-1-phosphate for chronic intermittent hypoxia-induced endothelial cell injury. Biochem. Biophys. Res. Commun. 498, 1016–1021. https://doi.org/10.1016/j.bbrc.2018.03.106 (2018).
Nakajima, C. et al. The lipoprotein receptor LRP1 modulates sphingosine-1-phosphate signaling and is essential for vascular development. Development 141, 4513–4525. https://doi.org/10.1242/dev.109124 (2014).
Meszaros, M. et al. The role of soluble low-density lipoprotein receptor-related protein-1 in obstructive sleep apnoea. J. Clin. Med. 10, 1494. https://doi.org/10.3390/jcm10071494 (2021).
Acknowledgements
The authors thank Monika Banlaky and Laszlo Kunos for their assistance in the sleep studies. Andras Bikov is supported by the NIHR Manchester BRC. The research was funded by the Hungarian Pulmonology Foundation (awarded to Peter Horvath and David Laszlo Tarnoki). This research was supported by the Bólyai scholarship of the Hungarian Academy of Sciences; ÚNKP-20-5 and ÚNKP-21-5 New National Excellence Program of the Ministry for Innovation and Technology, from the National Research, Development, and Innovation Fund. The grammar and vocabulary of the article were checked by the Department of Languages for Specific Purposes of Semmelweis University.
Funding
Open access funding provided by Semmelweis University.
Author information
Authors and Affiliations
Contributions
P.H., A.B. and G.L. designed the study. A.B. and M.M. performed sample collection and sleep study analyses. D.L.T. and A.D.T. helped with the sample collection. D.H., R.V., L.B. and P.H. performed ELISA measurements. P.H. and A.B. performed statistical analyses. All authors contributed to the drafting and revision of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Horváth, P., Büdi, L., Hammer, D. et al. The link between the sphingolipid rheostat and obstructive sleep apnea. Sci Rep 13, 7675 (2023). https://doi.org/10.1038/s41598-023-34717-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-34717-4
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.