Abstract
Phytochemicals are bioactive compounds found in plant-based foods. Consumption of phytochemical-rich foods has been associated with cardiovascular and metabolic diseases prevention in various populations. To quantify the phytochemical content of the diet, dietary phytochemical index (DPI) was established which is defined as the proportion of daily energy intake derived from foods rich in phytochemicals. The purpose of this study was to evaluate the association between the DPI and oxidative stress markers and cardiovascular risk factors in obese adults. In this cross-sectional study, a total of 140 adults aged 20–60 years and body mass index (BMI) of ≥ 30 kg/m2 were included. A validated food frequency questionnaire (FFQ) was used to collect information on dietary intakes. The DPI was calculated based on the following formula: DPI = [daily energy obtained from foods rich in phytochemicals (kcal)/total daily energy intake (kcal) × 100]. There was an inverse association between DPI and serum concentrations of Malondialdehyde (MDA) (P = 0.004), triglyceride (TG) (P-trend = 0.003), high-sensitive C-reactive protein (hs-CRP) (P = 0.017), and erythrocyte superoxide dismutase (SOD) activity (P = 0.024). Total antioxidant capacity (TAC) was positively associated with DPI score (P = 0.045). No significant relationship was found between the DPI score and fasting blood sugar (FBS), total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), total oxidant status (TOS), glutathione peroxidase (GPx), catalase (CAT), and anthropometric parameters as well as systolic and diastolic blood pressure. The current study found that there was a significant inverse association between DPI and oxidative stress, inflammation, and hypertriglyceridemia as cardiovascular disease (CVD) risk factors in obese population. However, further research is needed to confirm these findings.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) is the major cause of morbidity and death worldwide1. According to the recent studies, it has been shown that the disease has expanded to younger age groups as well2. This is partly attributed to the global epidemic of obesity, which has been demonstrated to be one of the most important predictors of CVD. Several risk factors related to CVD, such as hypertension, dyslipidemia, and insulin resistance are exacerbated by obesity3.
Oxidative stress and inflammation have been described in obesity and the pathogenesis of these CVD risk factors4. Oxidative stress is a state caused by the overproduction of reactive species, known as pro-oxidants, and the incapability of the antioxidant defense system to scavenge these species, which consequently causes cellular damage and destruction5. Several observational studies have supported the association between oxidative imbalance and cardio-metabolic conditions, which is associated with an increased risk of CVD. Thus, oxidative stress could be a potential target to manage cardiovascular complications in obese subjects.
Diet is considered as a key modifiable component of lifestyle in primary prevention of CVD and its consequences. Studies have shown that adherence to the plant-based diets and higher consumption of fruits and vegetables, whole grains, and dietary fiber may reduce the risk of developing CVD6,7. It is assumed that the protective effects of the plant-based diets may be attributed to dietary phytochemicals, in part8. Phytochemicals are natural bioactive compounds found in plants such as fresh fruits, vegetables, nuts, whole grains, and legumes9 with various known health benefits such as anti-inflammatory, antioxidant, antiangiogenic, and antihypercholesterolemic effects10.
Previous epidemiologic studies have demonstrated that the consumption of phytochemical-rich foods can help prevent cardiovascular and metabolic diseases in various populations. Evidence also suggest that phytochemicals can reduce the levels of inflammatory and oxidative stress markers and improve serum glycemic and lipid profiles11.
To quantify the phytochemical content of the diet, McCarty et al. established a simple and practical tool, known as dietary phytochemical index (DPI) which is defined as the proportion of daily energy intake derived from foods rich in phytochemicals12. Diet quality may be determined from this simple method for assessing phytochemical consumption13. It has been shown that higher DPI scores are associated with a lower risk of chronic diseases such as obesity, diabetes, metabolic syndrome, cancer, and CVD14. The available data regarding the association between DPI and oxidative stress biomarkers as well as other cardiometabolic risk factors in obese individuals are limited and the existing data are highly controversial. Thus, the purpose of this study was to investigate the relationship between DPI and oxidative stress status and cardiovascular risk factors in adults with obesity.
Materials and methods
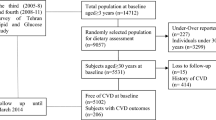
Study subjects
This cross-sectional study was conducted on 140 obese male and female subjects with a body mass index (BMI) of ≥ 30 kg/m2 and the age range of 20–60 years who attended the out-patient clinics affiliated to Zabol University of Medical Sciences. The sample size was determined based on the information obtained from the study by Golzarand et al.15 for serum triglyceride (TG) concentrations as the dependent variable employing the formula N = [(Z1-α/2)2S2]/d2. Considering SD = 7.0, d = 1.2, and α = 0.05, it was calculated that 130 subjects needed to be selected for the study. The sample size of the study was increased to 140 subjects for a possible dropout of 10%.
Pregnant and lactating women; those with recent inflammatory and infectious conditions, surgery or major trauma, a prior history of stroke, and renal or hepatic diseases; as well as those who were taking any antioxidant supplements three months before the study enrollment were not included. Subjects who were on a specific diet and subjects with obesity due to genetic causes or endocrine disorders were also not included.
Ethics approval and consent to participate
Prior to the study enrollment, participants were fully informed about the aims and the protocol of the study. Then, subjects were asked to sign a written informed consent. The study was performed in accordance with the Declaration of Helsinki and the protocol of the research was approved by the Ethics Committee of Zabol University of Medical Sciences (Ethics No: IR.ZBMU.REC.1400.118).
Demographic factors and anthropometric assessments
All participants enrolled in the study were interviewed by trained personnel. An interviewer-administered questionnaire was applied to gather the relevant demographic characteristics, detailed clinical information, and lifestyle habits of participants.
Weight was measured using a digital scale in the standing position with sensitivity of 100 g while subjects were light clothing, without shoes. Height was measured to the nearest of 0.5 cm in the normal standing position without shoes using a fixed wall scale. BMI was calculated as body weight (kg) divided by height in meters squared (m2). Waist circumference (WC) was measured using a flexible tape measure, without imposing any pressure to body surface.
Physical activity, and blood pressure assessment
The subject’s physical activity was assessed through the short form of the International Physical Activity Questionnaire (IPAQ)16, then divided into three categories of “high”, “moderate”, and “heavy” activity.
Blood pressure was measured after a 15-min sitting in a quiet environment using a mercury sphygmomanometer. The mean systolic blood pressure (SBP) and diastolic blood pressure (DBP) were recorded using two readings measured at 5-min intervals.
Dietary assessment and DPI calculation
Dietary intakes were evaluated using a validated semi-quantitative food frequency questionnaire (FFQ) with 168 food items17. A trained nutritionist recorded the subject’s frequency of food consumption in the previous year on a daily (e.g. bread), weekly (e.g. rice, meat) or monthly (e.g. fish) basis through face-to-face interviews. The assistants helped subjects estimate food quantities using calibrated household measurements (e.g. spoon, bowl, ladles). Portion sizes were then converted to grams. The intake of calorie and nutrients were calculated using Nutritionist IV software (First Databank; Hearst, San Bruno, CA, USA) based on the Iranian foods-modified US Department of Agriculture food composition. Nearly all foods in the participant list were coded and non-available foods were coded to a similar item.
The DPI was calculated based on the method developed by McCarty12 on the following formula: DPI = [daily energy obtained from foods rich in phytochemicals (kcal)/total daily energy intake (kcal)) × 100]. Fruits, vegetables, legumes, whole grains, nuts, soy products, seeds, and olive oil were considered as the phytochemical-rich foods to calculate DPI. Potatoes and pickled and powdered vegetables were not considered in the calculations because of their low phytochemical content. Furthermore, natural fruit juices were classified into the fruit group and vegetable juices and tomato sauces were classified into the vegetable group due to their high phytochemical content; therefore, they were included in the calculation of DPI. After calculating the DPI scores, they were categorized into tertiles, while subjects in the top tertile have the highest score of DPI.
Biochemical measurements
Fasting blood samples were taken after 10–12 h from all study subjects and centrifuged at 3500 rpm (~ 2000 g) to separate the sera. Fasting blood sugar (FBS), total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), and TG concentrations were assessed enzymatically on the day of sampling by commercial kits (Pars-Azmoon Co., Tehran, Iran) and the remaining sera were stored at − 80 °C until the assays were performed. Serum concentrations of high-sensitive C-reactive protein (hs-CRP) were measured based on the immunoturbidimetric method using the commercial kit (Pars Azmoon Co., Tehran, Iran) which is sensitive to 0.1 mg/L variations in serum concentrations of hs-CRP. The erythrocyte superoxide dismutase (SOD, EC 1.15.1.1) and glutathione peroxidase (GPx, EC 1.11.1.9) activities were determined using the Ransod (Randox Laboratories, Ltd., UK, cat. no. SD-125) and Ransel (Randox Laboratories, Ltd., UK, cat.no. RS-504) kits, respectively. Erythrocytes catalase (CAT, EC 1.11.1.6) activity was evaluated based on the method developed by Hygo Aebi18 by following the decomposition of H2O2 in phosphate buffer of pH 7.2 spectrophotometrically at 230 nm.
Serum concentrations of total antioxidant capacity (TAC) were determined colorimetrically in triplicate samples using 2, 2'-Azino-di-[3-ethylbenzthiazoline sulphonate] (ABTS)19. Malondialdehyde (MDA) concentrations in serum were also assessed by the measurement of thiobarbituric acid reactive substances (TBARS) according to Uchihara and Mihara method20. Serum total oxidant status (TOS) was determined according to Erel method21. The basis of this method depends on the oxidation of Fe2+ to Fe3+ in the presence of the oxidants contained in the sample. Fe+3 forms a colored complex with xylenol orange which the color intensity varies according to the amount of oxidant in the sample. The absorbance of this color spectrophotometrically is read at 530 nm. The assay is calibrated with hydrogen peroxide (H2O2) and the results are expressed in terms of micromolar H2O2 equivalent per liter (μmol H2O2 Equiv./L).
CVD risk factors
In this study, hyperglycemia and dyslipidemia were defined based on the diagnostic criteria proposed by the Adult Treatment Panel III guidelines of the National Cholesterol Education Program (NCEP ATP III)22. Hyperglycemia was considered as FBS ≥ 5.55 mmol/L or currently taking medication for impaired fasting glucose. Hypercholesterolemia was defined as TC ≥ 6.22 mmol/L or being on the treatment with lipid-lowering agents. Subjects who had serum TG ≥ 1.69 mmol/L or were on triglyceride-lowering medications were diagnosed with hypertriglyceridemia. Furthermore, “high LDL-C” and “low HDL-C” among subjects were diagnosed if they had serum LDL-C concentration of > 4.14 mmol/L and serum HDL-C concentration < 1.04 mmol/L, respectively. Based on the Eighth Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure23, subjects who had SBP ≥ 140 mmHg or DBP ≥ 90 mmHg or were on treatment with antihypertensive drugs were diagnosed with hypertension. According to the cutoff proposed by the American Heart Association and Centers for Disease Control, serum hs-CRP concentrations of ≥ 3.0 mg/l were considered as “high hs-CRP24”.
Statistical analyses
Statistical analyses were done using SPSS software (version 25; SPSS, Chicago, IL, USA). Data are illustrated as mean ± standard deviation (SD) for normally distributed continuous variables and median (interquartile range) for non-normally distributed variables. Categorical variables are displayed as absolute numbers and frequencies (%). The normality of data distribution was appraised using the Kolmogorov–Smirnov test. Subjects were classified based on cut-points of DPI in tertiles categories as follows: first tertile, < 27.3; second tertile, 27.3 to 33.9; third tertile, > 33.9. Differences in the characteristics of subjects across tertiles of DPI were evaluated by one-way analysis of variance (ANOVA) or chi-squared test, as appropriate. Sex-, age-, and energy-adjusted means for dietary intakes across DPI categories were compared by analysis of covariance (ANCOVA). Comparison of metabolic, inflammatory, and oxidative stress markers across DPI categories were also performed using ANOVA test for normally distributed data. To investigate and find the actual significant group differences, ANOVA was followed by Tukey’s test. Non-normally distributed data were compared by Kruskal–Wallis test across DPI categories and followed by Dunn’s post hoc test to investigate the actual significant group differences. The Jonckheere-Terpstra test was used to determine whether there is a significant trend between DPI and non-normally distributed variables. To find the association between DPI and metabolic, inflammatory, and oxidative stress biomarkers, the linear regression analysis was applied.
Logistic regression was used to investigate the relationship of DPI and CVD risk factors in two different models: the adjusted and unadjusted models. In the adjusted model, sex (male, female), age (years), BMI (kg/m2), smoking (yes, no), and physical activity level (categorical: light, moderate, and heavy) were adjusted. In both models, the first tertile of DPI was considered as the reference category. In all analyses, P < 0.05 was considered statistically significant.
Results
Subject’s characteristics
In this study, 140 obese subjects were included in the study. The mean age of participants was 41.0 ± 7.3 years and 55.0% of them were males. The DPI in this study ranged from 14.9 to 56.0 with the mean ± SD of 30.7 ± 7.1. The DPI in the first, second, and third tertiles was < 27.3, 27.3 to 33.9 and > 33.9, respectively. General characteristics of participants across tertile categories of DPI are shown in Table 1. There were no significant differences in the mean age, SBP, and DBP values as well as the distribution of participants regarding smoking, physical activity status, and education level among study groups.
Dietary intakes
Daily dietary intakes of study subjects across tertiles of DPI are presented in Table 2. Subjects in the upper tertile categories of DPI had higher energy intakes (P = 0.001) and higher daily energy intakes from carbohydrates (P = 0.004). Those in the highest tertile categories of DPI had higher intakes of fiber (P < 0.0001), vitamin C (P = 0.009), and folate (P = 0.006) compared with those in the lower tertiles. Compared to the subjects in the lowest tertile, those in the highest tertile of DPI consumed more grains (P < 0.0001), fruits (P < 0.0001), vegetables (P < 0.0001), and olive sources (P < 0.0001). No significant differences were found in daily energy intakes from protein, total fat, saturated fatty acids (SFA), monounsaturated fatty acids (MUFA), and polyunsaturated fatty acids (PUFA) across tertile categories of DPI. In addition, there were no significant differences across tertile categories of DPI for intakes of vitamin A, vitamin E, calcium, zinc, meats, nuts, and dairy products.
Association of DPI with metabolic, inflammatory, oxidative stress markers, and CVD risk factors
Table 3 indicates the anthropometric indices and metabolic, inflammatory, and oxidative stress markers of study subjects across tertiles of DPI. There were no significant differences in the mean weight, BMI, and WC across tertiles of DPI. The mean serum concentrations of TG (P-trend = 0.005) and hs-CRP (P-trend = 0.002) had decreasing trends across the increasing in DPI scores. The subjects in third tertile of DPI had lower serum concentrations of TG and hs-CRP compared to the counterparts in the first tertile (P < 0.05 for both). No significant regular trend was observed regarding FBS, TC, LDL-C, and HDL-C across DPI tertile categories. There was a trend towards decreasing serum concentrations of MDA (P-trend = 0.001) and TOS (P-trend = 0.013) as well as erythrocytes SOD activity (P-trend = 0.013) with increasing tertiles of DPI. Indeed, the subjects in the top tertile of DPI had lower serum concentrations of MDA and TOS as well as erythrocytes SOD activity compared to the subjects in the first tertile (P < 0.05 for all). Inversely, serum TAC concentration had increasing trend across the increasing in DPI categories (P-trend = 0.015) so that, subjects in the third tertile of DPI had higher serum TAC concentration compared to the counterparts in the first tertile (P < 0.05). Nonetheless, no significant associations was observed between DPI with GPx and CAT activities (Table 3).
The results obtained from the multiple linear regression analysis confirms aforementioned relationships (Table 4). DPI was inversely associated with serum concentrations of MDA (β = − 0.244, P = 0.004), TG (β = − 0.253, P = 0.003), and hs-CRP (β = − 0.202, P = 0.017) as well as erythrocytes SOD activity (β = − 0.189, P = 0.024) after controlling for potential confounders. In addition, DPI was positively associated with serum concentrations of TAC (β = 0.171, P = 0.045).
The odds ratios (OR) and 95% confidence interval (CI) for the incidence of CVD risk factors as the dependent variables across tertile categories of DPI as independent variables are illustrated in Table 5. After adjustment for potential confounding factors including age, sex, BMI, cigarette smoking, and physical activity, a noticeable inverse trend was found between DPI and the odds of having the hypertriglyceridemia (OR among tertiles, T1 to T3: 1.00, 0.58, and 0.32, respectively; P-trend = 0.023) and high hs-CRP (OR among tertiles, T1 to T3: 1.00, 0.49, and 0.23, respectively; P-trend = 0.004). However, no significant associations was found between DPI and the probability of having the hypercholesterolemia, high LDL-C, low HDL-C, hyperglycemia, and hypertension.
Discussion
Previous studies reported the risk of various chronic diseases and their inverse relationship with the DPI13; however, fewer studies evaluated this relationship in the obese population. This research is one of the first studies that investigated the relationship between DPI and oxidative stress markers and cardiovascular risk factors in the obese population. The results of the present study indicated a positive correlation between DPI and consuming olives, olive oils, grains, fruits, and vegetables. DPI was inversely associated with serum concentrations of TG, MDA, erythrocyte SOD activity, and hs-CRP levels. In addition, TAC was positively associated with DPI score. However, no significant relationship was found between the DPI score and FBS, TC, LDL-C, HDL-C, TOS, GPx, CAT, anthropometric parameters, as well as systolic and diastolic blood pressure.
DPI has been linked to the risk of some chronic diseases such as obesity, type 2 diabetes mellitus, metabolic syndrome, cancers, and cardiovascular and inflammatory diseases13,25,26,27,28. However, the exact mechanisms by which dietary phytochemicals protect against chronic diseases is not entirely understood. The potential beneficial effects of dietary phytochemicals seems to be mediated through down-regulating the inflammatory cytokines, as well as reducing oxidative stress because of their known anti-oxidative and anti-inflammatory properties29.
Numerous phytochemicals have been recognized as inducers of antioxidant enzymes in various studies30. Hermana et al. in a cross-sectional study on 246 healthy adults found a positive relationship between consumption of fruit and vegetables with TAC and GPx activity in plasma31. Another study on 205 prediabetes people also found a positive relationship between dietary intake of fruits and vegetables and TAC and SOD activity32. In the present study, DPI score was positively associated with serum TAC levels, but, inversely correlated with SOD activity. Since, SOD enzyme is part of the first line of defense against free radicals, it is expected that this inverse correlation may indicate the compensatory response to decreased oxidative stress by increasing phytochemical intakes through DPI tertiles. These findings support a role for dietary phytochemicals in the antioxidant defense system.
Higher amount of lycopene consumption, a kind of phytochemical, was associated with lower hs-CRP levels33. Kim et al. reported an inverse relationship between DPI scores and the likelihood of increasing hs-CRP levels in their study of 18,699 over-19 years Koreans from 2015 to 201834. Results from other studies match these current findings33,35,36. However, some other studies found no relationship between DPI and antioxidant or inflammatory biomarkers37,38,39,40. These contradictions could be due to the different biomarker evaluation methods, compound bioavailability, and the influence of other nutrients on the compound biological effects41,42.
Antioxidant properties of dietary phytochemicals have been determined by their capacity to scavenge and interact with reactive oxygen species (ROS) and inhibit enzymes involved in ROS generation43. It has been also found that dietary phytochemicals exert their antioxidant effects by activating specific genes involved in encoding antioxidant proteins through the key transcription factor, nuclear factor (erythroid-derived 2)-like 2 (Nrf2), which is known as an important regulator of the antioxidant response44.
The anti-inflammatory effects of phytochemicals is mediated through the regulation of various inflammatory cytokines such as interleukins and tumor necrosis factor alpha-α (TNF-α) as well as prostaglandin E2 as a non-cytokine mediator.
Current results indicate that phytochemicals have important antioxidant and anti-inflammatory effects, which reduce oxidative stress and inflammation. Regarding other cardiovascular risk factors including hypercholesterolemia, high LDL-C, low HDL-C, hypertriglyceridemia, hyperglycemia, and hypertension which investigated in the present study, higher scores of DPI was only associated with the lower risk of hypertriglyceridemia. Similar to this finding, in a cohort study on adult population, higher DPI was associated with a lower prevalence of hypertriglyceridemia45. Besides, a meta-analysis of 49 studies showed that plant-based diets are associated with improved plasma lipids46. Kim and Park also reported a significant association between higher DPI and a lower prevalence of hypertriglyceridemia, hyperglycemia, and high blood pressure25. Some evidence is also available regarding higher DPI and lower FBS levels in healthy people47,48. However, in one study on Iranian adults, no relation between DPI and serum lipid profile was found49. Besides, a cross-sectional study of 850 adults with metabolic syndrome reported no relationship between following a phytochemical-rich diet and the metabolic syndrome components49. Furthermore, few other cross-sectional studies found no significant relationship between higher intakes of flavonoids, polyphenols, and carotenoids and the metabolic syndrome components50,51,52.
These contradictions in the current evidence are probably because of heterogeneity in study designs, measured outcomes, sample sizes, specific food culture and habits, study population socio-demographic characteristics, and used assessment tools. Therefore, there were challenges in generalizing these results to other societies.
Population-based (obese people) design, data analysis after potential confounder modification, using valid questionnaires, and in-person interviews by trained nutritionists are the major strengths of this study. However, this study has some limitations, such as the impossibility of determining causality due to the cross-sectional nature of this study, the lack of native food databases for plant nutrients, and inherent DPI limitations, such as not considering some foods with high phytochemical values that have no energy (e.g., spices, green and black tea) and ignoring the phytochemical compound type and quality.
Conclusion
This study confirmed that there was a significant inverse association between DPI and oxidative stress, inflammation, and hypertriglyceridemia as CVD risk factors in obese population. Further randomized clinical trials and large-scale prospective cohorts are needed to validate these current findings using dietary data with low measurement errors.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Hosseini, J., Nematollahi, S., Shariatpanahi, S. & Sadegh-Zadeh, Z. The Prevalence of overweight and obesity in Iranian men: A systematic review and meta-analysis study. Men’s Health J. 5, e1–e1. https://doi.org/10.22037/mhj.v5i1.33612 (2021).
Piché, M.-E., Tchernof, A. & Després, J.-P. Obesity phenotypes, diabetes, and cardiovascular diseases. Circ. Res. 126, 1477–1500. https://doi.org/10.1161/CIRCRESAHA.120.316101 (2020).
Francula-Zaninovic, S. & Nola, I. A. Management of measurable variable cardiovascular disease’risk factors. Curr. Cardiol. Rev. 14, 153–163. https://doi.org/10.2174/1573403x14666180222102312 (2018).
Senoner, T. & Dichtl, W. Oxidative stress in cardiovascular diseases: Still a therapeutic target?. Nutrients 11, 2090. https://doi.org/10.3390/nu11092090 (2019).
Dubois-Deruy, E., Peugnet, V., Turkieh, A. & Pinet, F. Oxidative stress in cardiovascular diseases. Antioxidants 9, 864. https://doi.org/10.3390/antiox9090864 (2020).
Hemler, E. C. & Hu, F. B. Plant-based diets for cardiovascular disease prevention: All plant foods are not created equal. Curr. Atheroscler. Rep. 21, 1–8 (2019).
Patel, H., Chandra, S., Alexander, S., Soble, J. & Williams, K. A. Plant-based nutrition: An essential component of cardiovascular disease prevention and management. Curr. Cardiol. Rep. 19, 1–10. https://doi.org/10.1007/s11886-017-0909-z (2017).
Beura, S. K., Panigrahi, A. R., Yadav, P. & Singh, S. K. Phytochemicals as potential therapeutics for SARS-CoV-2–induced cardiovascular complications: Thrombosis and platelet perspective. Front. Pharmacol. 12, 658272. https://doi.org/10.3389/fphar.2021.658273 (2021).
Liu, R. H. Health-promoting components of fruits and vegetables in the diet. Adv. Nutr. 4, 384S-392S. https://doi.org/10.3945/an.112.003517 (2013).
Vasanthi, H. R., ShriShriMal, N. & Das, K. D. Phytochemicals from plants to combat cardiovascular disease. Curr. Med. Chem. 19, 2242–2251. https://doi.org/10.2174/092986712800229078 (2012).
Yuan, H. et al. The phytochemical epigallocatechin gallate prolongs the lifespan by improving lipid metabolism, reducing inflammation and oxidative stress in high-fat diet-fed obese rats. Aging Cell 19, e13199. https://doi.org/10.1111/acel.13199 (2020).
McCarty, M. F. Proposal for a dietary “phytochemical index”. Med. Hypotheses 63, 813–817. https://doi.org/10.1016/j.mehy.2002.11.004 (2004).
Eslami, O., Khoshgoo, M. & Shidfar, F. Dietary phytochemical index and overweight/obesity in children: A cross-sectional study. BMC. Res. Notes 13, 1–5. https://doi.org/10.1186/s13104-020-04979-6 (2020).
Kiebalo, T., Holotka, J., Habura, I. & Pawlaczyk, K. Nutritional status in peritoneal dialysis: Nutritional guidelines, adequacy and the management of malnutrition. Nutrients 12, 1715. https://doi.org/10.3390/nu12061715 (2020).
Golzarand, M., Mirmiran, P., Bahadoran, Z., Alamdari, S. & Azizi, F. Dietary phytochemical index and subsequent changes of lipid profile: A 3-year follow-up in Tehran lipid and glucose study in Iran. ARYA Atheroscler. 10, 203 (2014).
Hallal, P. C. & Victora, C. G. Reliability and validity of the international physical activity questionnaire (IPAQ). Med. Sci. Sports Exerc. 36, 556. https://doi.org/10.1249/01.MSS.0000117161.66394.07 (2004).
Mirmiran, P., Esfahani, F. H., Mehrabi, Y., Hedayati, M. & Azizi, F. Reliability and relative validity of an FFQ for nutrients in the Tehran lipid and glucose study. Public Health Nutr. 13, 654–662. https://doi.org/10.1017/S1368980009991698 (2010).
Aebi, H. In Methods in enzymology Vol. 105, pp. 121–126 (Elsevier, 1984).
Erel, O. A novel automated direct measurement method for total antioxidant capacity using a new generation, more stable ABTS radical cation. Clin. Biochem. 37, 277–285. https://doi.org/10.1016/j.clinbiochem.2003.11.015 (2004).
Uchiyama, M. & Mihara, M. Determination of malonaldehyde precursor in tissues by thiobarbituric acid test. Anal. Biochem. 86, 271–278. https://doi.org/10.1016/0003-2697(78)90342-1 (1978).
Erel, O. A new automated colorimetric method for measuring total oxidant status. Clin. Biochem. 38, 1103–1111. https://doi.org/10.1016/j.clinbiochem.2005.08.008 (2005).
Expert panel on detection, E. Executive summary of the third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). Jama 285, 2486–2497. https://doi.org/10.1001/jama.285.19.2486 (2001).
James, P. A. et al. 2014 evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the eighth joint national committee (JNC 8). JAMA 311, 507–520. https://doi.org/10.1001/jama.2013.284427 (2014).
Pearson, T. A. et al. Markers of inflammation and cardiovascular disease: Application to clinical and public health practice: A statement for healthcare professionals from the centers for disease control and prevention and the american heart association. Circulation 107, 499–511. https://doi.org/10.1161/01.CIR.0000052939.59093.45 (2003).
Kim, M. & Park, K. Association between phytochemical index and metabolic syndrome. Nurs. Res. Pract. 14, 252–261. https://doi.org/10.4162/nrp.2020.14.3.252 (2020).
Rigi, S. et al. Dietary phytochemical index in relation to risk of stroke: A case-control study. Nutr. Neurosci. 25, 1–8. https://doi.org/10.1080/1028415X.2021.1954291 (2021).
Ghoreishy, S. M., Aminianfar, A., Benisi-Kohansal, S., Azadbakht, L. & Esmaillzadeh, A. Association between dietary phytochemical index and breast cancer: A case–control study. Breast Cancer 28, 1–9. https://doi.org/10.1007/s12282-021-01265-6 (2021).
Amirkhizi, F., Ghoreishy, S. M., Hamedi-Shahraki, S. & Asghari, S. Higher dietary phytochemical index is associated with lower odds of knee osteoarthritis. Sci. Rep. 12, 1–8. https://doi.org/10.1038/s41598-022-13019-1 (2022).
Shen, C.-L. et al. Dietary polyphenols and mechanisms of osteoarthritis. J. Nutr. Biochem. 23, 1367–1377. https://doi.org/10.1016/j.jnutbio.2012.04.001 (2012).
Lee, S. E. & Park, Y. S. The emerging roles of antioxidant enzymes by dietary phytochemicals in vascular diseases. Life 11, 199 (2021).
Hermsdorff, H. H. M. et al. Vitamin C and fibre consumption from fruits and vegetables improves oxidative stress markers in healthy young adults. Br. J. Nutr. 107, 1119–1127. https://doi.org/10.1017/S0007114511004235 (2012).
Folchetti, L. D., Monfort-Pires, M., de Barros, C. R., Martini, L. A. & Ferreira, S. R. G. Association of fruits and vegetables consumption and related-vitamins with inflammatory and oxidative stress markers in prediabetic individuals. Diabetol. Metab. Syndr. 6, 1–8. https://doi.org/10.1186/1758-5996-6-22 (2014).
Mazidi, M., Katsiki, N., George, E. S. & Banach, M. Tomato and lycopene consumption is inversely associated with total and cause-specific mortality: A population-based cohort study, on behalf of the International lipid expert panel (ILEP). Br. J. Nutr. 124, 1303–1310. https://doi.org/10.1017/S0007114519002150 (2020).
Kim, C. & Park, K. Association between phytochemical index and Inflammation in Korean adults. Antioxidants 11, 348. https://doi.org/10.3390/antiox11020348 (2022).
Yu, Z. et al. Associations between nut consumption and inflammatory biomarkers. Am. J. Clin. Nutr. 104, 722–728. https://doi.org/10.3945/ajcn.116.134205 (2016).
Roager, H. M. et al. Whole grain-rich diet reduces body weight and systemic low-grade inflammation without inducing major changes of the gut microbiome: A randomised cross-over trial. Gut 68, 83–93. https://doi.org/10.1136/gutjnl-2017-314786 (2019).
Vincent, H. K., Bourguignon, C. M. & Taylor, A. G. Relationship of the dietary phytochemical index to weight gain, oxidative stress and inflammation in overweight young adults. J. Hum. Nutr. Diet. 23, 20–29. https://doi.org/10.1111/j.1365-277X.2009.00987.x (2010).
Edalati, S., Alipour, B. & Rashidkhani, B. Association between dietary intake of phytochemicals and hs-CRP in healthy women from tehran: A holistic approach using dietary phytochemical index. Nutr. Food Sci. Res. 5, 11–16 (2018).
Esmaeily, Z., Sotoudeh, G., Rafiee, M. & Koohdani, F. ApoA2–256T>C polymorphism interacts with healthy eating index, dietary quality index-international and dietary phytochemical index to affect biochemical markers among type 2 diabetic patients. Br. J. Nutr. 127, 1–9. https://doi.org/10.1017/S0007114521002348 (2021).
Delshad Aghdam, S. et al. Dietary phytochemical index associated with cardiovascular risk factor in patients with type 1 diabetes mellitus. BMC Cardiovasc. Disord. 21, 1–11. https://doi.org/10.1186/s12872-021-02106-2 (2021).
Sies, H. Total antioxidant capacity: appraisal of a concept. J. Nutr. 137, 1493–1495. https://doi.org/10.1093/jn/137.6.1493 (2007).
Lotito, S. B. & Frei, B. Consumption of flavonoid-rich foods and increased plasma antioxidant capacity in humans: Cause, consequence, or epiphenomenon?. Free Radic. Biol. Med. 41, 1727–1746. https://doi.org/10.1016/j.freeradbiomed.2006.04.033 (2006).
Komici, K. et al. Cardioprotective effects of dietary phytochemicals on oxidative stress in heart failure by a sex-gender-oriented point of view. Oxid. Med. Cell. Longev. 2020, 1–20. https://doi.org/10.1155/2020/2176728 (2020).
Krajka-Kuźniak, V. & Baer-Dubowska, W. Modulation of Nrf2 and NF-κB signaling pathways by naturally occurring compounds in relation to cancer prevention and therapy. Are combinations better than single compounds?. Int. J. Mol. Sci. 22, 8223. https://doi.org/10.3390/ijms22158223 (2021).
Bahadoran, Z., Golzarand, M., Mirmiran, P., Saadati, N. & Azizi, F. The association of dietary phytochemical index and cardiometabolic risk factors in adults: Tehran lipid and glucose study. J. Hum. Nutr. Diet. 26, 145–153. https://doi.org/10.1111/jhn.12048 (2013).
Yokoyama, Y., Levin, S. M. & Barnard, N. D. Association between plant-based diets and plasma lipids: A systematic review and meta-analysis. Nutr. Rev. 75, 683–698. https://doi.org/10.1093/nutrit/nux030 (2017).
Bahadoran, Z., Mirmiran, P., Tohidi, M. & Azizi, F. Dietary phytochemical index and the risk of insulin resistance and β-cell dysfunction: A prospective approach in Tehran lipid and glucose study. Int. J. Food Sci. Nutr. 66, 950–955. https://doi.org/10.3109/09637486.2015.1111867 (2015).
Urquiaga, I. et al. Wine grape pomace flour improves blood pressure, fasting glucose and protein damage in humans: A randomized controlled trial. Biol. Res. 48, 1–10. https://doi.org/10.1186/s40659-015-0040-9 (2015).
Firouzabadi, F. D. et al. The association of dietary phytochemical index with metabolic syndrome in adults. Clin. Nutr. Res. 10, 161. https://doi.org/10.7762/cnr.2021.10.2.161 (2021).
Kim, H., Lee, K., Rebholz, C. M. & Kim, J. Association between unhealthy plant-based diets and the metabolic syndrome in adult men and women: A population-based study in South Korea. Br. J. Nutr. 125, 577–590. https://doi.org/10.1017/S0007114520002895 (2021).
Zujko, M. E. et al. Dietary total antioxidant capacity and dietary polyphenol intake and prevalence of metabolic syndrome in Polish adults: A nationwide study. Oxid. Med. Cell. Longev. 2018, 1–10. https://doi.org/10.1155/2018/7487816 (2018).
Wei, J. et al. Associations between dietary antioxidant intake and metabolic syndrome. PLoS One 10, e0130876. https://doi.org/10.1371/journal.pone.0130876 (2015).
Acknowledgements
The authors appreciate the Research Vice-Chancellor of Zabol University of Medical Sciences for their support. The researchers also extend their sincerest appreciation to all subjects, who served as samples of this study.
Funding
This study was supported by Zabol University of Medical Sciences, Zabol, Iran.
Author information
Authors and Affiliations
Contributions
Conception and design: F.A., S.H., S.A., Acquisition of data: F.A., S.H. Analysis and interpretation of data: F.A., S.H. Drafting the manuscript: M.R.J., M.A.Z. Revising manuscript for intellectual content: S.A.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hamedi-Shahraki, S., Jowshan, MR., Zolghadrpour, MA. et al. Dietary phytochemical index is favorably associated with oxidative stress status and cardiovascular risk factors in adults with obesity. Sci Rep 13, 7035 (2023). https://doi.org/10.1038/s41598-023-34064-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-34064-4
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.