Abstract
Globally, air pollution is amongst the most significant causes of premature death. Nevertheless, studies on the relationship between fine particulate matter (PM2.5) exposure and blood lipids have typically not been population-based. In a large, community-based sample of residents in Yixing city, we assessed the relationship between short-term outdoor PM2.5 exposure and blood lipid concentrations. Participants who attended the physical examination were enrolled from Yixing People’s hospital from 2015 to 2020. We collected general characteristics of participants, including gender and age, as well as test results of indicators of blood lipids. Data on daily meteorological factors were collected from the National Meteorological Data Sharing Center (http://data.cma.cn/) and air pollutant concentrations were collected from the China Air Quality Online Monitoring and Analysis Platform (https://www.aqistudy.cn/) during this period. We applied generalized additive models to estimate short-term effects of ambient PM2.5 exposure on each measured blood lipid-related indicators and converted these indicators into dichotomous variables (non- hyperlipidemia and hyperlipidemia) to calculate risks of hyperlipidemia associated with PM2.5 exposure. A total of 197,957 participants were included in the analysis with mean age 47.90 years (± SD, 14.28). The increase in PM2.5 was significantly associated with hyperlipidemia (odds ratio (OR) 1.003, 95% CI 1.001–1.004), and it was still significant in subgroups of males and age < 60 years. For every 10 μg/m3 increase in PM2.5, triglyceride levels decreased by 0.5447% (95% CI − 0.7873, − 0.3015), the low-density lipoprotein cholesterol concentration increased by 0.0127 mmol/L (95% CI 0.0099, 0.0156), the total cholesterol concentration increased by 0.0095 mmol/L (95% CI 0.0053, 0.0136), and no significant association was observed between PM2.5 and the high-density lipoprotein cholesterol concentration. After excluding people with abnormal blood lipid concentrations, the associations remained significant except for the high-density lipoprotein cholesterol concentration. PM2.5 was positively correlated with low-density lipoprotein cholesterol and total cholesterol, and negatively correlated with triglyceride, indicating PM2.5 can potentially affect health through blood lipid levels.
Similar content being viewed by others
Introduction
Exposure to fine particulate matter (PM2.5) has been linked to a substantial disease burden globally1. Although some research has shown that short-term exposure to PM2.5 is positively correlated with mortality from respiratory diseases as well as an increased risk of cardiovascular disease2,3, the mechanisms and other impacts of PM2.5 exposure on health is still unclear.
Previous studies have reported that PM2.5 exposure may increase the incidence of non-alcoholic fatty liver disease4. A previous study among senior citizens found that individuals exposed to long-term PM2.5 exposure had an increased incidence of dementia5. Other studies found long-term PM2.5 exposure was associated with increased serum triglyceride and decreased high-density lipoprotein cholesterol concentration in elderly males6. Other research in children and adolescents suggests that long-term PM2.5 exposure was positively associated with the total cholesterol concentration and risk of hypercholesterolemia7. Whether PM2.5 exposure and blood lipids are epidemiologically related is debated and few large studies have investigated this relationship at the population-level.
Although there have been several studies on PM2.5 exposure and blood lipids, most of these studies are based on long-term PM2.5 exposure, and few studies have explored the association between short-term PM2.5 exposure and blood lipids. To further the understanding of the relationship between short-term PM2.5 exposure and blood lipids, we collected test results of blood lipid-related indicators through routine physical examinations from a community-based sample of 197,957 residents in Yixing city. We also assessed for a range of environmental factors during the same period.
Methods
Study population
This cross-sectional study was performed in Yixing city, located in eastern China, with a population of approximately 1.3 million. The study population was not selected based on disease status; participants who attended a routine physical examination at Yixing People’s Hospital from 2015 to 2020 were eligible and enrolled in the study. No subjects repeatedly took part in the study. Inclusion criteria: (1) participants who were tested for lipid-related indicators (2) participants were local residents Exclusion criteria: (1) participants who took lipid-lowering drugs (2) participants who were workers exposed to dust. We collected participant characteristics, blood lipid-related indicators, including total cholesterol, triglyceride, low-density lipoprotein cholesterol, and high-density lipoprotein cholesterol. Blood samples were obtained from individuals after at least 8 hours overnight fasting. High-density lipoprotein cholesterol and low-density lipoprotein cholesterol was analyzed by the direct assay method. Total cholesterol by cholesterol oxidase method and triglyceride by enzymatic method, using CobasC501, (Roche Diagnostics GmbH, Switzerland).
Binary and continuous outcomes
According to Chinese guidelines for the prevention and treatment of dyslipidemia in adults8, the normal range of these indicators are: (1) total cholesterol < 6.2 mmol/L; (2) triglyceride < 2.3 mmol/L; (3) low-density lipoprotein cholesterol < 4.1 mmol/L; and (4) high-density lipoprotein cholesterol > 1.0 mmol/L. We calculated the number of participants with normal blood lipid-related indicators separately. Participants with abnormalities in either indicator were defined as having hyperlipidemia.
Data on meteorological factors and air pollutants
The exposure data were obtained from a fixed monitoring station ((120.35′E, 31.62′N)) for the city. The quality control methods of the monitoring stations include climate limit value check, station extreme value check, time consistency check, space consistency check and manual check. We collected daily average meteorological factors, including atmospheric pressure (hPa), temperature (oC), wind speed (m/s), and relative humidity (%) during January 8, 2015 and December 31, 2020 from the National Meteorological Data Sharing Center (http://data.cma.cn/). Data on daily average air pollutant concentrations, including PM2.5, PM10 (particles of less than 10 μm diameter), sulphur dioxide (SO2), nitrogen dioxide (NO2), ozone (O3), and carbon monoxide (CO) were collected from the China Air Quality Online Monitoring and Analysis Platform (https://www.aqistudy.cn/). Except that the unit of CO concentration was mg/m3, the unit of other pollutants was μg/m3.
Statistical analysis
A generalized additive model (GAM) was applied to explore the relationship between short-term ambient PM2.5 exposure and blood lipid-related indicators similar to prior studies9,10. GAMs are useful for evaluating the impact of air pollution on human health11. Among the four indicators, triglyceride were not normally distributed. Total cholesterol, low-density lipoprotein cholesterol and high-density lipoprotein cholesterol were all normally distributed. We performed natural log conversions of triglyceride to achieve a approximate normal distribution. To account for potential confounders, adjusted covariates in the GAM model included day of the week, time, sex, age, and meteorological factors. To address multiple collinearities, Spearman rank correlation coefficients between environmental factors were calculated; the model only included variables with \(\left|\mathrm{r}\right|\)<0.712. We applied a thin plate spline function in order to control for nonlinear effects of meteorological factors13. Minimum Akaike information criterion (AIC) values corresponded to the optimal degree of freedom10. Considering lag effects of PM2.5 on blood lipids, we calculated 2- to 8-day moving averages (lag 0–1 day to lag 0–7 days) of the daily average concentration of PM2.5 to capture cumulative lag effects. For example, if a person attended the physical examination on January 9, we collected the daily average concentration of PM2.5 from January 2 to January 9, and then calculated the average concentration from January 8 to January 9 as the 2-day moving average. The n-day moving average concentration was applied to estimate personal short-term PM2.5 exposure level. Minimizing the AIC value was applied to identify the optimal lag time14,15,16. We expressed the effects as the estimated changes in blood lipid-related indicators and their 95% confidence intervals (CIs) for a 10 μg/m3 increase in ambient PM2.5 concentration15. We also converted lipid-related indicators into dichotomous variables (normal and abnormal) to calculate risks of hyperlipidemia associated with PM2.5 exposure, and expressed them as the odds ratio (OR) as well as their 95% CIs for 10 μg/m3 rise in outdoor PM2.5 concentration. In addition, we analyzed the relationship between other air pollutions (including PM10, SO2, NO2, O3, and CO) and blood lipids using similar approaches.
We performed two sensitivity analyses to examine the robustness of the associations between PM2.5 and blood lipid-related indicators. First, we constructed single- and multi-pollutant models for PM2.5, respectively. Second, individuals with abnormal indicators were excluded to estimate the effects of PM2.5 among the population with normal indicators. A subgroup analysis was also performed to explore if the effect was modified by sex or age. The heterogeneity effects between subgroups were evaluated using the formula: \(\left|{\beta }_{1}-{\beta }_{2}\right|/\sqrt{{{SE}_{1}}^{2}+{{SE}_{2}}^{2}}\), where \({\beta }_{1}\) and \({\beta }_{2}\) are the estimated effects, and \({SE}_{1}\) and \({SE}_{2}\) are their standard errors, respectively. When the value was larger than 1.96, the difference was considered statistically significant15.
All analyses were performed with the “mgcv” and “ggplot2” packages in R software version 4.1.2 (https://www.r-project.org/). The significance level was set at 0.05.
Ethics statement
This study was approved by ethics committee of Yixing people’s hospital.
Results
Characteristics of study participants
Of 206,452 participants eligible for the study, 205,945 attended a physical examination. In total, 7988 participants were excluded for various reasons; 1944 (0.90%) participants were excluded because they were not local residents while 4562 participants were not tested for lipid-related indicators. Lastly, 1482 participants were taking lipid-lowering drugs during the study period and were also excluded (Fig. 1). After exclusions, a total of 197,957 people were included in the analysis. Mean age was 47.90 years (± SD, 14.28) and 55.61% of participants were male. The mean values of total cholesterol, low-density lipoprotein cholesterol, and high-density lipoprotein cholesterol was 4.94 mmol/L (± 0.94), 2.73 mmol/L (± 0.67), and 1.31 mmol/L (± 0.31), respectively. The median triglyceride values were 1.35 mmol/L ((interquartile range [IQR], 0.92, 2.04) (Table 1). The number of participants with normal levels was 133,080 for triglyceride, 132,643 for low-density lipoprotein cholesterol, 132,308 for high-density lipoprotein cholesterol and 133,172 for total cholesterol.
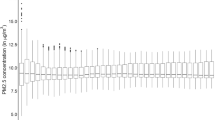
Characteristics of meteorological factors and air pollutants
The median daily average meteorological factors and air pollutant concentrations was 18.10 °C for temperature, 1016.30 hPa for atmospheric pressure, 2.10 m/s for wind speed, 74% for relative humidity, 38.00 μg/m3 for PM2.5, 67.00 μg/m3 for PM10, 11.00 μg/m3 for SO2, 38.00 μg/m3 for NO2, 0.90 mg/m3 for CO, and 95.00 μg/m3 for O3 (Table 1). PM2.5 was positively correlated with atmospheric pressure, PM10, SO2, NO2, and CO, and negatively correlated with temperature and wind speed (P < 0.05). Because Spearman rank correlation coefficients between PM2.5 and PM10 and CO were larger than 0.7, the above two air pollutants were excluded from the final model. The absolute value of the correlation coefficient between temperature and atmospheric pressure was larger than 0.7, atmospheric pressure was removed from the model (Supplementary Table 1). The df of meteorological factors in the analyze of effects of PM2.5 on blood lipids were shown in Supplementary Table 2.
PM2.5 and blood lipids in entire population
We applied lag 0–6 days, 0–7 days, 0–5 days and 0–7 days for triglyceride, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol and total cholesterol in the entire population respectively. For a 10 μg/m3 increase in PM2.5, the triglyceride decreased by 0.5447% (95% CI − 0.7873, − 0.3015), the low-density lipoprotein cholesterol concentration increased by 0.0127 mmol/L (95% CI 0.0099, 0.0156) and the total cholesterol concentration increased by 0.0095 mmol/L (95% CI 0.0053, 0.0136) and no significant association was observed between PM2.5 and the high-density lipoprotein cholesterol concentration(Table 2). The associations remained significant of low-density lipoprotein cholesterol and total cholesterol by the subgroups of males, females, age < 60 years and age ≥ 60 years. Of triglyceride, the associations remained significant in the subgroups of females, age < 60 years and age ≥ 60 years, and the effect of short-term PM2.5 exposure on the low-density lipoprotein cholesterol concentration and total cholesterol concentration could be modified by age, the effects was stronger for the subgroup of age ≥ 60 years (Fig. 2, Supplementary Table 3).
Estimated changes (95% confidence intervals) in the blood lipids for every 10 μg/m3 increase in PM2.5 among the entire population. We applied lag 0–6 days for triglyceride, lag 0–7 days for low-density lipoprotein cholesterol, lag 0–5 days for high-density lipoprotein cholesterol, and lag 0–7 days for total cholesterol.
PM2.5 and blood lipids in persons with normal blood lipid levels
In persons with normal test results, for a 10 μg/m3 increase in PM2.5, the triglyceride decreased by 0.5184% (95% CI − 0.7235, − 0.3128), the low-density lipoprotein cholesterol concentration increased by 0.0096 mmol/L (95% CI 0.0068, 0.0124) and the total cholesterol concentration increased by 0.0057 mmol/L (95% CI 0.0019, 0.0095). No significant association was observed between PM2.5 and the high-density lipoprotein cholesterol concentration (Table 2). The associations remained significant of low-density lipoprotein cholesterol and triglyceride in the subgroups of males, females, age < 60 years and age ≥ 60 years and remained significant of the total cholesterol concentration in the subgroups of males, age < 60 years and age < 60 years (Fig. 3). After excluding participants with abnormal test results, short-term PM2.5 exposure and its effect on triglyceride could be modified by age, the effects were stronger for the subgroup of age ≥ 60 years (Supplementary Table 3).
Estimated changes (95% confidence intervals) in the blood lipids for every 10 μg/m3 increase in PM2.5 among persons with normal blood lipid levels. We applied lag 0–6 days for triglyceride, lag 0–7 days for low-density lipoprotein cholesterol, lag 0–5 days for high-density lipoprotein cholesterol, and lag 0–7 days for total cholesterol.
The effects of PM2.5 on the blood lipid at different lag days
The associations between PM2.5 and triglyceride, low-density lipoprotein cholesterol concentration and total cholesterol concentration were robust at different lag days. And the effects of PM2.5 exposure on triglyceride, low-density lipoprotein cholesterol concentration, and total cholesterol concentration were strongest at lag 0–4 days, lag 0–7 days, lag 0–4 days and lag 0-7 days. However, no significant association was observed between PM2.5 and the high-density lipoprotein cholesterol concentration at different lag days. (Table 3).
The effects of PM2.5 on the blood lipids in multi-pollutant models
For a 10 μg/m3 increase in PM2.5, the low-density lipoprotein cholesterol concentration increased by 0.0194 mmol/L (95% CI 0.0152, 0.0237), the high-density lipoprotein cholesterol concentration decreased by 0.0022 mmol/L (95% CI − 0.0039, − 0.0005) and the total cholesterol concentration increased by 0.0284 mmol/L (95% CI 0.0224, 0.0345). No significant association was observed between PM2.5 and the triglyceride. In persons with normal test results, for a 10 μg/m3 increase in PM2.5, the low-density lipoprotein cholesterol concentration increased by 0.0134 mmol/L (95% CI 0.0093, 0.0175) and the total cholesterol concentration increased by 0.0209 mmol/L (95% CI 0.0153, 0.0265). No significant association was observed between PM2.5 and the triglyceride and high-density lipoprotein cholesterol concentration (Table 2).
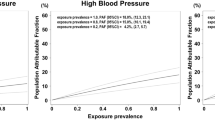
The effects of PM2.5 on hyperlipidemia
We converted lipid-related indicators into binary variables (non- hyperlipidemia and hyperlipidemia) to calculate risks of hyperlipidemia associated with PM2.5 exposure. As a result, when PM2.5 increased 10 μg/m3, the OR (95% CIs) was 1.003 (95% CI 1.001, 1.004), and it was still significant in the subgroups of males and age < 60 years (Supplementary Table 4). We also converted lipid-related indicators into binary variables (normal and abnormal) to calculate the OR and 95% CI of blood lipids for every 10 μg/m3 increase in PM2.5. We applied lag 0–6 days for triglyceride, lag 0–3 days for low-density lipoprotein cholesterol, lag 0–5 days for high-density lipoprotein cholesterol and lag 0–7 days for total cholesterol. When PM2.5 increased 10 μg/m3, the OR (95% CIs) for triglyceride, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol and total cholesterol was 0.998 (95% CI 0.996, 0.999), 1.001 (95% CI 1.000, 1.001), 1.002 (95% CI 1.001, 1.003) and 1.003 (95% CI 1.001, 1.004) (Supplementary Table 5).
The effects of other air pollutions (including PM10, SO2, NO2, O3, and CO) on the blood lipids are shown in the Supplementary Appendix (Supplementary Tables 6–15).
Discussion
In this study, we found that PM2.5 was positively correlated with low-density lipoprotein cholesterol concentration and total cholesterol concentration, while being negatively correlated with triglyceride. Findings from our study provide evidence of the potential harmful effects of PM2.5 exposure on blood lipids. To our knowledge, this is the largest population-based study to explore the association between short-term PM2.5 exposure and blood lipids, and will provide new empirical for the effect of short-term air pollutant exposure on health.
Previous studies have been heterogeneous with some showing similar results17,18 while others harmful. Study design and differential exposure may partially explain these differences. For example, long-term exposure to PM2.5 was positively associated with triglyceride concentration in a study in Perth6. Distinct durations of exposure may partially explain this inconsistency and our analysis specifically evaluated short-term effect of PM2.5 exposure while many studies concentrated on longer-term effect of PM2.56. Previous studies in rural areas have demonstrated that short-term PM2.5 exposure was positively associated with triglyceride concentration19 and negatively associated with total cholesterol concentration20, inconsistent with our results. Differences in lifestyle and air quality between rural and urban areas may influence outcomes17,18,21. For example, Omega-3 fatty acids may attenuate cardiovascular effects of short-term exposure to ambient air pollution22. In our study, PM2.5 was negatively correlated with triglyceride in the single pollutant model, and positively correlated with triglyceride in the multi-pollutant model, regardless of the overall population or the population with normal blood lipids. This suggested that other air pollutants may alter the associations between PM2.5 and triglyceride, which requires further research.
In our study, PM2.5 was positively associated with the low-density lipoprotein cholesterol concentration. Most previous studies investigated long-term, rather than short-term, exposure effects of PM2.5 to low-density lipoprotein cholesterol concentration23,24,25. Our study provides new evidence for the effect of short-term exposure. Long-term PM2.5 exposure was shown to be negatively associated with high-density lipoprotein cholesterol concentration18, inconsistent with our findings, indicating that differential exposure durations (short- versus long-term) may also have an impact on the results.
Previous studies have been heterogenous concerning the effect of PM2.5 on total cholesterol concentration. A study in Shanghai showed no significant association between total cholesterol and PM2.526. However, another study is consistent with our results27, showing PM2.5 exposure was associated with an elevated total cholesterol concentration. The difference of exposure durations may explain the inconsistency because we evaluated the short-term effect of PM2.5, while the study in shanghai explored the long-term exposure. A study among college students20 showed that short-term PM2.5 exposure was negatively associated with total cholesterol concentration, the inconsistency may be attributed to the difference of sample size and age. Recent research showed that long- term PM2.5 exposure was negatively correlated with the risk of hyperlipidemia28, however, in our study, the OR of every 10 μg/m3 increase in PM2.5 for hyperlipidemia population was 1.009, which suggested that short-term PM2.5 exposure was a risk factor for hyperlipidemia. Different life-styles and areas may explain the inconsistency. In our study, the effect of short-term PM2.5 exposure on the low-density lipoprotein cholesterol concentration and total cholesterol concentration could be modified by age and the older were more susceptible to PM2.5 exposure, which may be due to hypometabolism and/or hypoimmunity. Previous studies support these findings29,30,31.
Our study has several limitations. First, our study was a time-series study, limiting our ability to account for reverse causation or time-specific confounding. Second, the fixed environmental monitoring station was used to estimate personal PM2.5 exposure, which cannot be equated entirely with individual exposure. Lastly, although our dataset was large and community-based, we did not have available several other characteristics which may be associated with PM2.5 exposure and blood lipid-related indicators, such as exercise, smoking, and medical history. Therefore, unmeasured and residual confounding is possible.
Conclusions
PM2.5 was positively correlated with low-density lipoprotein cholesterol and total cholesterol, and negatively correlated with triglyceride, indicating PM2.5 can potentially affect health through blood lipid levels.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- 95%CI:
-
95% Confidence interval
- OR:
-
Odds ratio
- PM2.5 :
-
Particulate matter with an aerodynamic matter smaller than 2.5 μm
- PM10 :
-
Particulate matter with an aerodynamic matter smaller than 10 μm
- NO2 :
-
Nitrogen dioxide
- SO2 :
-
Sulphur dioxide
- O3 :
-
Ozone
- CO:
-
Carbon monoxide
- GAM:
-
Generalized additive model
- AIC:
-
Akaike information criterion
References
Zhang, D. et al. A machine learning model to estimate ambient PM(2.5) concentrations in industrialized highveld region of South Africa. Remote Sens. Environ. https://doi.org/10.1016/j.rse.2021.112713 (2021).
Xue, X., Chen, J., Sun, B., Zhou, B. & Li, X. Temporal trends in respiratory mortality and short-term effects of air pollutants in Shenyang, China. Environ. Sci. Pollut. Res. Int. 25, 11468–11479. https://doi.org/10.1007/s11356-018-1270-5 (2018).
Dominici, F. et al. Fine particulate air pollution and hospital admission for cardiovascular and respiratory diseases. JAMA 295, 1127–1134. https://doi.org/10.1001/jama.295.10.1127 (2006).
Chen, J. et al. The influence of PM2.5 exposure on non-alcoholic fatty liver disease. Life Sci. 270, 119135. https://doi.org/10.1016/j.lfs.2021.119135 (2021).
Mortamais, M. et al. Long-term exposure to ambient air pollution and risk of dementia: Results of the prospective Three-City Study. Environ. Int. 148, 106376. https://doi.org/10.1016/j.envint.2020.106376 (2021).
Vander Hoorn, S. et al. Long-term exposure to outdoor air pollution and risk factors for cardiovascular disease within a cohort of older men in Perth. PLoS ONE 16, e0248931. https://doi.org/10.1371/journal.pone.0248931 (2021).
Gui, Z. H. et al. Exposure to ambient air pollution and blood lipids in children and adolescents: A national population based study in China. Environ. Pollut. 266, 115422. https://doi.org/10.1016/j.envpol.2020.115422 (2020).
Committee, C. A. D. G. R. J. Guidelines for prevention and treatment of dyslipidemia in Chinese adults (update 2016) (in Chinese). Chin. Circ. J. 937–953, 7–28 (2017).
Sui, X. et al. The short-term effect of PM2.5/O3 on daily mortality from 2013 to 2018 in Hefei, China. Environ. Geochem. Health 43, 153–169. https://doi.org/10.1007/s10653-020-00689-x (2021).
Wang, S., Kaur, M., Li, T. & Pan, F. Effect of different pollution parameters and chemical components of PM2.5 on health of residents of Xinxiang City, China. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph18136821 (2021).
Hua, J. et al. Quantitative estimation of meteorological impacts and the COVID-19 lockdown reductions on NO2 and PM2.5 over the Beijing area using Generalized Additive Models (GAM). J. Environ. Manag. 291, 112676. https://doi.org/10.1016/j.jenvman.2021.112676 (2021).
Zhu, S. et al. Ambient air pollutants are associated with newly diagnosed tuberculosis: A time-series study in Chengdu. China. Sci Total Environ 631–632, 47–55. https://doi.org/10.1016/j.scitotenv.2018.03.017 (2018).
Tian, L. et al. Ambient carbon monoxide and the risk of hospitalization due to chronic obstructive pulmonary disease. Am. J. Epidemiol. 180, 1159–1167. https://doi.org/10.1093/aje/kwu248 (2014).
Bai, Y. L., Huang, D. S., Liu, J., Li, D. Q. & Guan, P. Effect of meteorological factors on influenza-like illness from 2012 to 2015 in Huludao, a northeastern city in China. PeerJ 7, e6919. https://doi.org/10.7717/peerj.6919 (2019).
Li, Z. Q. et al. Effects of short-term ambient PM2.5 exposure on the blood cell count and hemoglobin concentration among 82,431 people in eastern China. Sci. Total Environ. https://doi.org/10.1016/j.scitotenv.2021.146046 (2021).
Zheng, S. et al. The effect of diurnal temperature range on blood pressure among 46,609 people in Northwestern China. Sci. Total Environ. 730, 138987. https://doi.org/10.1016/j.scitotenv.2020.138987 (2020).
McGuinn, L. A. et al. Fine particulate matter exposure and lipid levels among children in Mexico city. Environ. Epidemiol. 4, e088. https://doi.org/10.1097/ee9.0000000000000088 (2020).
Mao, S. et al. Long-term effects of ambient air pollutants to blood lipids and dyslipidemias in a Chinese rural population. Environ. Pollut. 256, 113403. https://doi.org/10.1016/j.envpol.2019.113403 (2020).
Wu, Y. et al. Short-term exposure to air pollution and its interaction effects with two ABO SNPs on blood lipid levels in northern China: A family-based study. Chemosphere 249, 126120. https://doi.org/10.1016/j.chemosphere.2020.126120 (2020).
Sun, J. et al. Association of short-term exposure to PM(2.5) with blood lipids and the modification effects of insulin resistance: A panel study in Wuhan. Toxics https://doi.org/10.3390/toxics10110663 (2022).
Li, J. et al. Short term effect of PM(2.5) on cardiovascular mortality in residents in Changping district, Beijing. Zhonghua Liu Xing Bing Xue Za Zhi 40, 331–334. https://doi.org/10.3760/cma.j.issn.0254-6450.2019.03.014 (2019).
Chen, H. et al. Omega-3 fatty acids attenuate cardiovascular effects of short-term exposure to ambient air pollution. Part. Fibre Toxicol. 19, 12. https://doi.org/10.1186/s12989-022-00451-4 (2022).
Li, J. H. et al. Association of long-term exposure to PM2.5 with blood lipids in the Chinese population: Findings from a longitudinal quasi-experiment. Environ. Int. https://doi.org/10.1016/j.envint.2021.106454 (2021).
Zhang, H. H. & Zhao, Y. H. Long-term exposure to ambient air pollution is associated with elevated low-density lipoprotein cholesterol level. Atmos. Environ. https://doi.org/10.1016/j.atmosenv.2020.117970 (2021).
Bell, G. et al. Association of air pollution exposures with high-density lipoprotein cholesterol and particle number the multi-ethnic study of atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 37, 976. https://doi.org/10.1161/atvbaha.116.308193 (2017).
Jiang, S. et al. Traffic-related air pollution is associated with cardio-metabolic biomarkers in general residents. Int. Arch. Occup. Environ. Health 89, 911–921. https://doi.org/10.1007/s00420-016-1129-3 (2016).
Chen, Z. et al. Ambient air pollutants have adverse effects on insulin and glucose homeostasis in Mexican Americans. Diabetes Care 39, 547–554. https://doi.org/10.2337/dc15-1795 (2016).
Lin, J. et al. Long-term ambient PM(2.5) exposure associated with cardiovascular risk factors in Chinese less educated population. BMC Public Health 21, 2241. https://doi.org/10.1186/s12889-021-12163-z (2021).
Wang, M. et al. Association between short-term exposure to air pollution and dyslipidemias among type 2 diabetic patients in northwest China: A population-based study. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph15040631 (2018).
Tong, L., Li, K. & Zhou, Q. The association between air pollutants and morbidity for diabetes and liver diseases modified by sexes, ages, and seasons in Tianjin, China. Environ. Sci. Pollut. Res. Int. 22, 1215–1219. https://doi.org/10.1007/s11356-014-3432-4 (2015).
Bell, M. L., Dominici, F. & Samet, J. M. A meta-analysis of time-series studies of ozone and mortality with comparison to the national morbidity, mortality, and air pollution study. Epidemiology 16, 436–445. https://doi.org/10.1097/01.ede.0000165817.40152.85 (2005).
Funding
This study was supported by the National Nature Science Foundation of China (82003516, 81902148), Medical Scientific Research General Project of Jiangsu Health Commission (M2020020/ZD2021052/ZDA2020022) and Young Science Talents Promotion Project of Jiangsu Science and Technology Association. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. All the authors have reviewed and approved the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Q.L., Z.W. and Z.L. conceived the study, analyzed the data and drafted the manuscript; Q.L. and X.P. participated in the study design; X.M., J.L. and C.W. implemented the field investigation; B.T., L.M., L.Z., W.L. and B.Z. participated in the study design and helped draft the manuscript. All authors contributed to the study and have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, Q., Wang, Z., Lu, J. et al. Effects of short-term PM2.5 exposure on blood lipids among 197,957 people in eastern China. Sci Rep 13, 4505 (2023). https://doi.org/10.1038/s41598-023-31513-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-31513-y
This article is cited by
-
The impact of co-exposure to air and noise pollution on the incidence of metabolic syndrome from a health checkup cohort
Scientific Reports (2024)
-
Influence of Air Pollution Exposures on Cardiometabolic Risk Factors: a Review
Current Environmental Health Reports (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.