Abstract
We used US nationwide commercial insurance claims data (2011–2015) to study the effect of social deprivation on clinical and demographic risk factors for suicidal ideation (SI) and suicide attempts (SA) among US youth and adults < 65 years, after having a mental health or substance use disorder-related outpatient encounter. Neighborhood social deprivation level was summarized by the quintile of social deprivation index (SDI) at individuals’ zip code level. Cox proportional hazard models were used to evaluate the effect of social deprivation on demographic and clinical risk factors for SI and SA. The study cohort consisted of 317,383 individuals < 65 years, with 124,424 aged < 25 (youth) and 192,959 aged between 25 and 64 (adults). Neighborhood social deprivation impacted risk factors for SI and SA differently for youth and adults. Among youth, SDI interacted with multiple risk factors for both SI and SA. The effects of the risk factors were larger on youth from middle socioeconomic neighborhoods. Among adults, risk of SI was the strongest in the most deprived neighborhoods, but risk of SA did not vary by neighborhood deprivation level. Our findings suggest community-based suicide prevention initiatives should be tailored according to neighborhood deprivation level and the targeted individual’s age to maximize the impact.
Similar content being viewed by others
Introduction
Suicide remains an important public health concern in the US1. Despite significant resources allocated towards suicide prevention, the rates of suicidal ideation (SI) and suicide attempts (SA) have increased over the last several years1,2. Numerous models have been developed to predict the risk of suicide and suicidal behaviors in clinical settings3,4,5, focusing on demographic and clinical risk factors associated with SI or SA. A recent study used electronic health records (EHR) data from multiple health systems across the US to identify important clinical risk factors for SA and suicide from over 300 potential predictors, including prior history, diagnoses, medications, healthcare service utilization, and routinely collected depression questionnaires, through developing and validating predictive models4. The most important risk factors identified were long-, mid-, and short-term (past 5 years, past 1 year, and past 3 months) mental health and substance use disorder (MH/SUD) related diagnosis, healthcare services utilization, and prescription medications. Using EHR data of almost 20 million visits of individuals aged 13 years or older with an outpatient mental health diagnosis, this study’s models achieved overall accuracy of prediction (c-statistic) over 80%, which significantly outperformed other published models, and thus can be considered as benchmark models for risk prediction.
As many health care systems are moving towards routinely collecting individual-level data on social determinants of health (SDoH) during a clinical encounter and integrating such information within EHRs6,7, it has become possible to study the effects of SDoH on health outcomes. Several studies have found associations between SDoH and suicide, including unemployment, poverty, and divorce rates8,9,10,11. In addition, the independent effects of SDoH on SI or SA persisted even after controlling for the demographic and clinical risk factors of individual participants. In a recent study using the EHR data from the Veterans Health Administration (VHA), adverse SDoH factors, such as housing instability, unemployment, and financial problems, were strongly associated with SI and SA even after adjusting for the presence of major depressive, alcohol use, drug use, anxiety, posttraumatic stress, schizophrenia, and bipolar disorders12. Further, SDoH are associated with risk factors for SI and SA. Living in disadvantaged neighborhoods has also been linked to depression13,14, substance use disorders in adolescents15, and higher utilization of health services16,17, all of which are risk factors for suicide and suicidal behaviors4. Therefore, it is important to investigate if SDoH modifies the effects of demographic and clinical risk factors for SI or SA.
Few studies have investigated the modifying effect of SDoH on demographic and clinical risk factors for SI or SA. A study based on the Canadian National Longitudinal Survey of Children and Youth data found that youth living in poor neighborhoods were at greater risk of SI and SA, and the effects of psychosocial risk factors were higher in poor neighborhoods, suggesting the need of tailoring community-based youth suicide prevention initiatives to the poverty level of the neighborhoods in order to increase their impact18. However, this study only considered one dimension of SDoH, neighborhood poverty, which was dichotomized and used as a binary measure. SDoH contains intangible factors from multiple dimensions, including but not limited to economics, food, education, healthcare, social supports, and environment19. Using poverty alone will not be able to effectively identify neighborhoods that require more health care resources. In addition, polarizing neighborhoods into “poor” and “non-poor” oversimplifies reality20; the majority are in the middle of the distribution21. To avoid false dichotomies22, more granular levels of SDoH should be considered in analysis.
This study utilized data on commercially insured individuals in the US. Commercial health insurance plans cover over 60% of the US population under age 65, and individuals with commercial insurance coverage tend to have higher income compared to those who have public health plan coverage or are uninsured23. The primary objective was to evaluate whether the risks for SI or SA vary across a wide range of neighborhood-level SDoH factors, measured by the social deprivation index (SDI) at each zip code tabulation area (ZCTA). SDI is a population-level composite measure which captures multiple dimensions of SDoH, including income, education, employment, housing, household characteristics, and transportation24. The independent effects of neighborhood social deprivation on SI or SA in addition to individual-level demographic and clinical risk factors were also evaluated. The second objective was to evaluate whether neighborhood social deprivation modifies the effects of clinical and demographic risk factors for SI and SA. Because youth and adults exhibit different patterns for suicidal thoughts and behaviors1, data on youth and on adults were analyzed separately.
Methods
Data source and cohorts description
This nationwide retrospective cohort study was conducted using health insurance claims data from the Health Care Cost Institute (HCCI), a non-profit, nonpartisan, independent research entity. The HCCI holds nationwide deidentified insurance claims data on beneficiaries covered by commercial or Medicare Advantage plans from four major health insurance companies in the US (i.e., Aetna, Humana, Kaiser Permanente, and UnitedHealthcare) in a manner that is compliant with the Health Insurance Portability and Accountability Act (HIPAA)25,26. A detailed description of the HCCI database can be found elsewhere27.
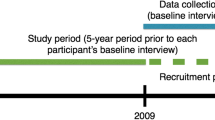
We used the HCCI data from 2011 to 2015 to build the youth and adult study cohorts. Specifically, we restricted the cohorts to individuals who were (1) < 65 years of age; (2) subscribed to a commercial insurance plan with mental health coverage; (3) had an MH/SUD related outpatient visit between 1/1/2014 and 6/30/2015 (index event); and (4) at least 3 years of continuous enrollment before the index event. MH/SUD diagnoses were defined by the ICD-9-CM codes lists for mental health, alcohol use, and substance use summarized elsewhere28. For individuals with multiple index events in the study window, the first encounter was used as the index event. The three-year continuous enrollment criterion was imposed to fully capture individuals’ recent prior healthcare encounters. Figure 1 summarizes the design of the study. The data were, then, split into two cohorts: the youth and very young adults cohort included individuals younger than 25 years at the time of the index event (hereafter referred to as youth), and the other adults cohort included individuals aged 25–64 years at the time of the index event (hereafter referred to as adults).
Independent variables
Demographic variables sex (male vs. female), age group (< 18, 18–24, 25–34, 35–44, 45–54, 55–64 years), and region (rural vs. urban) were directly extracted from the membership enrollment file in the month of the index event. Individuals’ five-digit residential zip codes were also extracted. The region (rural vs. urban) variable was derived from metropolitan statistical areas defined by the US Census core-based statistical areas (CBSAs). Individuals living in a CBSA with a population fewer than 50,000 residents were classified as living in a non-metropolitan setting.
Individuals’ neighborhood deprivation level was defined by the quintile of the social deprivation index (SDI) at individuals’ residential zip codes. SDI is a composite measure ranging from 0 to 100 developed to quantify the socio-economic variation at different area levels, i.e., counties, census tracts, Zip Code Tabulation Areas (ZCTA), and Primary Care Service Areas (PCSA). SDI combines seven socio-demographic characteristics from the American Community Survey (ACS) in a particular geographical area: percent living in poverty, percent with less than 12 years of education, percent single-parent household, percent living in rented housing unit, percent living in overcrowded housing unit, percent of households without a car, and percent non-employed adults under 65 years of age. SDI was originally developed using 2005–2009 ACS 5-year estimates and calculated at the PCSA level24, whereas the SDI version used in this study was updated using the 2011–2015 ACS 5-year estimates and calculated at the ZCTA level. We selected the SDI instead of other measures for two reasons: (1) social deprivation assessed with the SDI is associated with the individuals’ health and health quality29, as well as hospitalization and mortality risks30; and (2) SDI has a version developed at the ZCTA level, making it easier to map to the zip codes recorded in our claims data. Quintiles of SDI were used to allow for deprivation patterns to vary across different characteristics and to preserve the complexity of the effects of disadvantaged neighborhoods. Higher SDI quintile indicates a higher level of social deprivation.
Clinical risk factors for SI/SA included in our analysis were selected through predictive modeling in prior research4, which consisted of a combination of long-, mid-, and short-term diagnoses (i.e., anxiety disorders, depression, alcohol use disorders, drug use disorders, eating disorders, personality disorders, suicide attempts with schizophrenia, and suicide attempts in the past 3 years; suicide attempts in the past year; and suicide attempts in the past 3 months), medication prescriptions (i.e., antidepressant prescription filled in the past 3 months, benzodiazepine prescription filled in the past 3 months), and healthcare services (i.e., mental health inpatient stay in the past year, mental health emergency department visit in the past year, and mental health emergency department visit in the 3 months). Hospitalizations were defined by having claims in the inpatient files. ED visits were identified via claims reporting Revenue Center Codes values for emergency room services: 0450-0459 (emergency room) or 0981 (professional fees-emergency room). Diagnoses were defined by ICD-9-CM codes (details provided in Supplementary Information Table S1) and medication prescriptions were defined by national drug code (NDC) codes (The 6111 NDC codes for antidepressants and 7570 NDC codes for benzodiazepine are available upon request).
Outcome variables
For each cohort, two outcomes were considered for survival analyses: time to SI (in days) and time to SA (in days) from the time of the index event. Survival outcomes were chosen because a binary outcome for logistic regression requires insurance beneficiaries to have continuous enrollment of the commercial health insurance plan throughout the entire period of the study, including the follow-up period post index date, which will selectively remove beneficiaries who might have changed or lost employment due to their mental health status and introduce selection bias. SI was defined by ICD-9-CM diagnosis code V62.84 and SA was defined by ICD-9-CM diagnosis codes E950-E958 and E980-E988 (undetermined intent). ICD-9-CM codes E980-E988 were included because using only E95X.X had low sensitivity in identifying a suicide attempt31, and including E980-E988 codes increased the sensitivity and positive predictive value of identifying a suicide attempt4,32. Since the US transitioned from using ICD-9-CM to ICD-10-CM codes on 10/1/2015 and our data ended on 12/31/2015, individuals were censored if they did not have an SI or SA diagnosis before 9/30/2015. We did not include SI or SA diagnoses after 9/30/2015 to avoid the potential artifacts caused by coding changes33. The censoring date was defined by either the last day of the month of individuals’ insurance plan enrollment or 9/30/2015, whichever came first.
Statistical analysis
The distributions of outcome variables (time to SI and SA post index event), demographic characteristics, and risk factors were summarized for the entire cohort, each age-stratified cohort, and each age-stratified cohort by SDI quintile. Chi-square tests were used to compare the distributions of variables between the youth and the adult cohorts, as well as across SDI quintiles within each cohort.
For each outcome variable in each cohort, a sequence of Cox proportional hazards models were fit for various purposes: (1) Model 1 was fit to validate the clinical risk factors identified by others4, which contained all the clinical risk factors described in Section "Independent variables", (2) Model 2 was fit to evaluate the main effects of demographic variables beyond clinical risk factors, which contained clinical risk factors and demographic variables, (3) Model 3 was fit to evaluate the main effects of neighborhood-level SDI beyond clinical risk factors and demographic variables, which contained clinical risk factors, demographic variables, and SDI, and (4) Model 4 was fit to evaluate if SDI modified the effects of clinical risk factors and demographic variables, which contained clinical risk factors, demographic variables, SDI, and the interactions between SDI and clinical risk factors and demographic variables. The partial-likelihood-ratio test was used to compare the latter model with the former one, with the exception of Model 4, which was directly compared with Model 2 if the main effects of SDI were not significant (i.e., if Model 3 vs. Model 2 was not significant, then Model 4 was compared with Model 2 instead of Model 3). The latter model was selected if the partial-likelihood-ratio test was significant at 0.05 level.
All data management and analyses were performed using R statistical software (version 3.6.3; R Foundation for Statistical Computing, Vienna, Austria). All methods were carried out in accordance with the HIPAA compliance. This study was reviewed, approved, and informed consent was waived by the Institutional Review Board at Weill Cornell Medicine.
Results
Between 1/1/2014 and 6/30/2015, we identified 317,383 individuals younger than 65 years with an index outpatient mental health visit. Among them, 124,424 aged < 25 (defined as youth) and 192,959 were aged 25–64 years (defined as adults). Youth had higher post index event prevalence rates of SI and SA than adults: The post 7-, 30-, 90-, 180-, and 365-day SI rates were 2.98%, 3.76%, 4.76%, 5.65%, and 6.66% among youth, respectively, and 1.16%, 1.50%, 1.91%, 2.36%, and 2.80% among adults, respectively. The post 7-, 30-, 90-, 180-, and 365-day SA rates were 0.40%, 0.61%, 0.92%, 1.25%, and 1.67% among youth, respectively, and 0.16%, 0.24%, 0.38%, 0.53%, and 0.69% among adults, respectively. The SI and SA rates for youths were significantly higher than those of adults at each time period of the outcome (e.g., 7, 30, 90, 180, and 365 days after the index event). Details of the distributions of the outcome variables (i.e., SI and SA rates 7-, 30-, 90-, 180-, and 365-day post index event), demographic variables, and clinical risk factors for each cohort are summarized in Table 1. Distributions of the above-mentioned variables by SDI for each cohort are summarized in Supplementary Information Table S2.
Suicidal ideation in youth
Additional main effects of demographic variables to Model 1 significantly improved prediction accuracy (\({\chi }^{2}(3)\)=535.5, p < 0.01 for Model 2 vs. Model 1). Further addition of neighborhood level SDI to Model 2 improved prediction accuracy significantly (\({\chi }^{2}(4)\)=16.90, p < 0.01 for Model 3 vs. Model 2). Furthermore, Model 4, which included interactions between SDI and clinical and demographic risk factors, significantly improved the prediction accuracy of Model 3, which did not include interactions. This observation suggests that SDI significantly modified the effects of clinical risk factors and demographic variables on youth SI (\({\chi }^{2}(72)\)=98.55, p = 0.02 for Model 4 vs. Model 3).
The following interactions were significant in the final model (i.e., Model 4): interactions between SDI and age, SDI and alcohol use disorder diagnosis in the past 3 years, SDI and SA in the past 1 year, and SDI and MH emergency department (ED) visits in the past 3 months (Fig. 2). Overall, the largest effect of SDI on risk factors was usually observed among middle SDI quintiles.
Specifically, youth under 18 years had higher hazard rates of SI than youth aged between 18 and 24 years; the magnitude of the elevated risk of SI decreased as the neighborhood deprivation level increased (higher SDI quintiles), with the exception of the first two quintiles, where the risks were comparable (HR = 1.62, 95% CI [1.48, 1.78]; HR = 1.73, 95% CI [1.57, 1.90]; HR = 1.59, 95% CI [1.44, 1.77]; HR = 1.43, 95% CI [1.28, 1.59]; and HR = 1.31, 95% CI [1.17, 1.46] for the 1st, 2nd, 3rd, 4th, and 5th SDI quintile, respectively). Having an alcohol use disorder diagnosis in the past 3 years was associated with an increased risk of SI for individuals from neighborhoods that belonged to the 2nd SDI quintile (HR = 1.25, 95% CI [1.07, 1.46]), but this relationship was not significant for individuals from neighborhoods of other SDI quintiles. Having mental health-related ED visits in the past 3 months was associated with an increased risk of SI for individuals from neighborhoods that belonged to the 2nd (HR = 1.30, 95% CI [1.04, 1.63]) and 4th (HR = 1.63, 95% CI [1.28, 2.09]) SDI quintiles. However, this relationship was not significant for individuals from neighborhoods of other SDI quintiles.
Suicide attempts in youth
Additional main effects of demographic variables to Model 1 were significant (\({\chi }^{2}(3)\)=187.3, p < 0.01 for Model 2 vs. Model 1), but additional main effects of SDI were not significant (\({\chi }^{2}(4)\)=2.96, p = 0.56 for Model 3 vs. Model 2). Nevertheless, SDI still modified the effects of clinical risk factors and demographic risk factors for youth SA (\({\chi }^{2}(76)\)=103.8, p = 0.02 for Model 4 vs. Model 2).
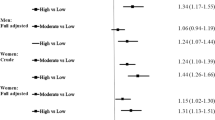
The following interactions were significant in the final model (i.e., Model 4): interactions between SDI and SA and schizophrenia in the past 3 years, SDI and SA in the past 3 years, SDI and Benzodiazepine prescription in the past 3 months, and SDI and mental health-related ED visits in the past 1 year. Hazard ratios (HR) of SA by SDI for each risk factor are summarized in Fig. 3. Similar to SI, the impact of SDI on risk factors for SA was usually the largest among middle SDI quintiles.
Specifically, having SA in the past 3 years was associated with an increased risk of SA for individuals from neighborhoods that belonged to the 2nd (HR = 1.94, 95% CI [1.27, 2.98]), 3rd (HR = 2.73, 95% CI [1.81, 4.12]), 4th (HR = 2.52, 95% CI [1.58, 4.01]), and 5th (HR = 3.82, 95% CI [2.47, 5.92]) SDI quintiles, but the association was not significant for individuals from neighborhoods that belonged to the first SDI quintile. Taken together, the effect of having SA in the past 3 years increased with neighborhood deprivation level (higher SDI quintiles). Having SA and schizophrenia in the past 3 years was associated with an increased risk of SA for individuals from neighborhoods that belonged to the 2nd SDI quintile (HR = 3.10, 95% CI [1.40, 6.87]), but this relationship was not significant for individuals from neighborhoods of other SDI quintiles. Having benzodiazepine prescriptions in the past 3 months was associated with an increased risk of SA for individuals from neighborhoods that belonged to the 2nd SDI quintile (HR = 1.93, 95% CI [1.40, 2.65]), but this relationship was not significant for individuals from neighborhoods of other SDI quintiles. Having mental health-related ED visits in the past year was associated with an increased risk of SA for individuals from neighborhoods that belonged to the 1st SDI quintile (HR = 1.59, 95% CI [1.22, 2.09]), but this relationship was not significant for individuals from neighborhoods of other SDI quintiles.
Suicidal ideation in adults
Additional main effects of demographic variables and SDI were significant (\({\chi }^{2}(5)\)=154.45, p < 0.01 for Model 2 vs. Model 1; \({\chi }^{2}(4)\)=31.30, p < 0.01 for Model 3 vs. Model 2). However, SDI did not modify the effects of clinical risk factors and demographic variables on adult SI (\({\chi }^{2}(80)\)=83.76, p = 0.36 for Model 4 vs. Model 3).
The results of the final Cox model for adult SI (i.e., Model 3) are summarized in Table 2. Specifically, SDI was positively associated with adult SI: Individuals from more disadvantaged neighborhoods had higher risk of having SI (HRs = 1.13, 1.19, and 1.25 for SDI quintiles 3rd, 4th, 5th vs. 1st; p < 0.05 for all 3 HRs).
Suicide attempts in adults
Additional main effects of demographic variables to Model 1 were significant (\({\chi }^{2}(5)\)=16.38, p = 0.01 for Model 2 vs. Model 1). However, additional main effects of SDI were not significant (\({\chi }^{2}(4)\)=6.66, p = 0.16 for Model 3 vs. Model 2). SDI did not modify the effects of clinical risk factors and demographic variables on adult SA (\({\chi }^{2}(84)\)=101.83, p = 0.09 for Model 4 vs. Model 2). Therefore, the final model for adult SA included clinical risk factors and demographic variables (i.e., Model 2).
The results of the final Cox model for adult SA (i.e., Model 2) are summarized in Table 2. For the adult cohort, having SA was not affected by the SDI level of individuals’ neighborhoods, after controlling for demographics and clinical risk factors. However, belonging to a younger age group, having anxiety disorders, depression, alcohol use disorders, drug use disorders, eating disorders, personality disorders, and suicide attempts in the past 3 years, having benzodiazepine prescriptions in the past 3 months, having mental health inpatient stay and mental health ED visits in the past year were all associated with an increased risk of SA in adults.
Discussion
The main finding of this study is that neighborhood level social deprivation impacts the demographic and clinical risk factors of SI and SA differently among commercially insured youth and adults. Among youth, SDI interacted with many risk factors for both SI and SA. The modified effects were usually larger in individuals from less extreme SDI neighborhoods. In adults, SDI was positively associated with SI but not with SA.
Among those who had an outpatient mental health or substance use related encounter, SI and SA rates were consistently more prevalent among youth than adults. This finding aligns with a multi-center study of individuals with outpatient mental health conditions conducted during the same study period34. The post 90-day SA rate among youth and adults was 0.92% and 0.38%, respectively. The post 90-day SA rate among adults was within the range of post 90-day SA rates reported by Simon et al., which were 0.26% among primary care outpatient visits and 0.62% among mental health specialty visits4.
We found that, among youth, the impact of social deprivation on the effects of risk factors for SI and SA was usually not the largest in the most deprived or the least deprived neighborhoods. For example, having an alcohol use disorder diagnosis in the past 3 years only impacted youth’s SI among those living in neighborhoods that belonged to the 2nd SDI quintile. A potential explanation would be that parents or educators from other neighborhoods pay more attention to youth’s mental health once they are diagnosed with alcohol use disorder, so that their risk of future SI was more effectively reduced. However, more in-depth studies are needed to understand these magnified effects. Our findings on the youth cohort were consistent with an earlier study on Canadian youth where risk factors for SI and SA varied by neighborhood poverty level18. However, with more granular information on neighborhood disadvantage level (i.e., quintiles vs. binary), we were able to uncover that social deprivation had stronger impact on middle neighborhoods50, which was not apparent in the previous analysis in which a dichotomized measure of neighborhood poverty level was used.
Among adults, neighborhood social deprivation level did not modify the effects of clinical and demographic risk factors on SI or SA. However, the main effects of SDI were still significantly associated with adult SI; individuals from more deprived neighborhoods had a higher risk of having SI. The main effects of SDI were not associated with adult SA, after controlling for demographics and clinical risk factors. Several studies also reported a positive association between low income and SI35,36. However, one study found a positive association between relative deprivation in income and SA35,36, and another study observed a positive association between area deprivation and SA37. Among severely depressed adults, one study reported no association between area-level social deprivation and SI or SA38.
There are several limitations of our study. First, the deprivation level we investigated was at the individuals’ neighborhood level, which may or may not reflect the individuals’ actual socio-economic status. Second, the HCCI dataset does not provide more detailed brackets for beneficiaries under the age of 18 years. Therefore, we were unable to define the youth cohort as “aged between 12 and 25 years,” which is more commonly reported in the literature39,40,41. However, mental health problems and substance usage such as depression and exposure to drugs and alcohol are rare in very young children42. Therefore, we did not expect a significant portion of children under 12 in our youth cohort. Third, although fitting survival models relaxed the continuous enrollment criterion, we still imposed a three-year before index event continuous enrollment criterion in order to fully capture individuals’ prior healthcare utilization encounters. Individuals with and without continuous insurance plan enrollment might have very different socioeconomic status27. Fourth, since we used claims data for analysis, any encounters that were not billed to the beneficiaries' insurance plan could not be captured. Fifth, analysis in this study was conducted on the commercially insured population. Over 50% of the US population was covered by employer-sponsored health insurance plans43, making commercial insurance the largest insurance coverage type in the US. In our study, the average neighborhood-level percentage of population under 100% Federal Poverty Level (FPL) varied by SDI quintile, from 0.04 to 0.24 in the adults cohort and from 0.04 to 0.23 in the youth cohort (Supplementary Information Figs. S1 and S2). During the same period (2011–2015), the total US population below 100% FPL was between 14.7 and 15.9%44. Therefore, although the commercially insured population underrepresents people with lower incomes, in our cohorts, there was still enough variability in income to not compromise our findings. Evaluating the impact of social deprivation on risk factors for SI or SA among Medicaid enrollees will be a future direction of our study. Finally, our analysis did not include patients’ race/ethnicity information. It is well documented that suicidality, as well as risk and protective factors for suicidality vary by race and ethnicity45,46,47. A recent study also found racial/ethnic disparities in the performance of suicide predictive models48. Racial/ethnic minorities are disproportionately represented in deprived neighborhoods49, therefore, social deprivation might partially explain the racial/ethnic disparities in suicidality. Further studies are needed to evaluate whether SDI mediates the effect of race/ethnicity on suicidality.
In conclusion, our study provides information on the effects of neighborhood-level social deprivation on suicidal behaviors in youth and in adults. Community-based suicide prevention initiatives may take into considerations the targeted individuals’ age. Our findings suggest that community-based suicide prevention initiatives for adults should target severely deprived neighborhoods. Interventions for youth should focus on those residing in neighborhoods with middle social deprivation level50, which is the demographic group sometimes being overlooked by researchers, policy makers, and health professionals planning suicide prevention51.
Data availability
The data that support the findings of this study are available from Health Care Cost Institute (HCCI) but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Readers should contact HCCI for raw data.
References
Steele, I. H., Thrower, N., Noroian, P. & Saleh, F. M. Understanding suicide across the lifespan: A United States perspective of suicide risk factors. Assess. Manag. J. Forensic Sci. 63(1), 162–171 (2018).
Walsh, C. G. et al. Prospective validation of an electronic health record-based, real-time suicide risk model. JAMA Netw. Open. 4(3), e211428–e211428 (2021).
Brown, G. K., Beck, A. T., Steer, R. A. & Grisham, J. R. Risk factors for suicide in psychiatric outpatients: A 20-year prospective study. J. Consult. Clin. Psychol. 68(3), 371–377 (2000).
Simon, G. E. et al. Predicting suicide attempts and suicide deaths following outpatient visits using electronic health records. Am. J. Psychiatry. 175(10), 951–960 (2018).
García de la Garza, Á., Blanco, C., Olfson, M. & Wall, M. M. Identification of suicide attempt risk factors in a national US survey using machine learning. JAMA Psychiat. 78(4), 398–406 (2021).
Cantor, M. N. & Thorpe, L. Integrating data on social determinants of health into electronic health records. Health Aff. 37(4), 585–590 (2018).
Gold, R. et al. Adoption of social determinants of health EHR tools by community health centers. Ann. Fam. Med. 16(5), 399–407 (2018).
Rehkopf, D. H. & Buka, S. L. The association between suicide and the socio-economic characteristics of geographical areas: A systematic review. Psychol. Med. 36(2), 145–157 (2006).
Milner, A., Page, A. & LaMontagne, A. D. Cause and effect in studies on unemployment, mental health and suicide: A meta-analytic and conceptual review. Psychol. Med. 44(5), 909–917 (2014).
Chen, J., Choi, Y. J., Mori, K., Sawada, Y. & Sugano, S. Socio-economic studies on suicide: A survey. J. Econ. Surv. 26(2), 271–306 (2012).
Middleton, N., Sterne, J. A. C. & Gunnell, D. The geography of despair among 15–44-year-old men in England and Wales: Putting suicide on the map. J. Epidemiol. Community Health 60(12), 1040–1047 (2006).
Blosnich, J. R. et al. Social determinants and military veterans’ suicide ideation and attempt: A cross-sectional analysis of electronic health record data. J. Gen. Intern. Med. 35(6), 1759–1767 (2020).
Choi, J. K., Teshome, T. & Smith, J. Neighborhood disadvantage, childhood adversity, bullying victimization, and adolescent depression: A multiple mediational analysis. J. Affect. Disord. 279, 554–562 (2021).
Richardson, R., Westley, T., Gariépy, G., Austin, N. & Nandi, A. Neighborhood socioeconomic conditions and depression: A systematic review and meta-analysis. Soc. Psychiatry Psychiatr. Epidemiol. 50(11), 1641–1656 (2015).
Handley, E. D., Rogosch, F. A., Guild, D. J. & Cicchetti, D. Neighborhood disadvantage and adolescent substance use disorder: The moderating role of maltreatment. Child Maltreat. 20(3), 193–202 (2015).
Hu, J., Kind, A. J. H. & Nerenz, D. Area deprivation index predicts readmission risk at an urban teaching hospital. Am. J. Med. Qual. 33(5), 493–501 (2018).
Kind, A. J. H. et al. Neighborhood socioeconomic disadvantage and 30-Day rehospitalization. Ann. Intern. Med. 161(11), 765. https://doi.org/10.7326/m13-2946 (2014).
Dupéré, V., Leventhal, T. & Lacourse, E. Neighborhood poverty and suicidal thoughts and attempts in late adolescence. Psychol. Med. 39(8), 1295–1306 (2009).
Catalyst. Social determinants of health (SDOH). NEJM Catal. https://doi.org/10.1056/cat.17.0312.
Aassve, A., Mazzuco, S. & Mencarini, L. Childbearing and well-being: A comparative analysis of European welfare regimes. J. Eur. Soc. Policy. 15(4), 283–299 (2005).
Institute of Medicine, Board on Health Promotion and Disease Prevention, Committee on Assuring the Health of the Public in the 21st Century. The Future of the Public’s Health in the 21st Century. National Academies Press (2003).
Escandón, K. et al. COVID-19 false dichotomies and a comprehensive review of the evidence regarding public health, COVID-19 symptomatology, SARS-CoV-2 transmission, mask wearing, and reinfection. BMC Infect. Dis. 21(1), 710 (2021).
Cohen, R. A., Terlizzi, E. P., Cha, A. E., & Martinez, M.E. Health insurance coverage: early release of estimates from the national health interview survey, January–June 2020. Published online 2021. https://stacks.cdc.gov/view/cdc/100469/cdc_100469_DS1.pdf.
Butler, D. C., Petterson, S., Phillips, R. L. & Bazemore, A. W. Measures of social deprivation that predict health care access and need within a rational area of primary care service delivery. Health Serv. Res. 48(2 Pt 1), 539–559 (2013).
HCCI. Accessed March 9, 2020. https://healthcostinstitute.org/about-hcci.
Newman, D., Herrera, C. N., & Parente, S. T. Overcoming barriers to a research-ready national commercial claims database. Am. J. Manag. Care. 20(11 Spec17), eSP25–eSP30 (2014).
Xi, W. et al. Healthcare utilization among patients with psychiatric hospitalization admitted through the emergency department (ED): A claims-based study. Gen. Hosp. Psychiatry. 67, 92–99 (2020).
Johnston, K. J., Allen, L., Melanson, T. A. & Pitts, S. R. A “Patch” to the NYU emergency department visit algorithm. Health Serv Res. 52(4), 1264–1276 (2017).
Liaw, W. et al. Living in “cold spot” communities is associated with poor health and health quality. J. Am. Board Fam. Med. 31(3), 342–350 (2018).
Zhang, Y. et al. Socioeconomic variation in characteristics, outcomes, and healthcare utilization of COVID-19 patients in New York City. PLoS ONE 16(7), e0255171 (2021).
Swain, R. S. et al. A systematic review of validated suicide outcome classification in observational studies. Int. J. Epidemiol. 48(5), 1636–1649 (2019).
Simon, G. E. et al. Self-reported suicidal ideation as a predictor of suicidal behavior among outpatients with diagnoses of psychotic disorders. Psychiatr. Serv. 70(3), 176–183 (2019).
Stewart, C., Crawford, P. M. & Simon, G. E. Changes in coding of suicide attempts or self-harm with transition from ICD-9 to ICD-10. Psychiatr. Serv. 68(3), 215 (2017).
Rossom, R. C. et al. Suicidal ideation reported on the PHQ9 and risk of suicidal behavior across age groups. J. Affect. Disord. 215, 77–84 (2017).
Pak, T. Y. & Choung, Y. Relative deprivation and suicide risk in South Korea. Soc. Sci. Med. 247, 112815 (2020).
Cabello, M. et al. Cross-national prevalence and factors associated with suicide ideation and attempts in older and young-and-middle age people. Aging Ment. Health. 24(9), 1533–1542 (2020).
Lemstra, M., Neudorf, C. & Opondo, J. Health disparity by neighbourhood income. Can. J. Public Health. 97(6), 435–439 (2006).
Werbeloff, N., Markou, M., Hayes, J. F., Pitman, A. L. & Osborn, D. P. J. Individual and area-level risk factors for suicidal ideation and attempt in people with severe depression. J. Affect. Disord. 205, 387–392 (2016).
Malla, A. et al. Youth mental health should be a top priority for health care in Canada. Can. J. Psychiatry. 63(4), 216–222 (2018).
Clarke, A. M., Kuosmanen, T. & Barry, M. M. A systematic review of online youth mental health promotion and prevention interventions. J. Youth Adolesc. 44(1), 90–113 (2015).
Purcell, R. et al. Demographic and clinical characteristics of young people seeking help at youth mental health services: Baseline findings of the Transitions Study. Early Interv. Psychiatry. 9(6), 487–497 (2015).
Gould, M. S., Greenberg, T., Velting, D. M. & Shaffer, D. Youth suicide risk and preventive interventions: A review of the past 10 years. J. Am. Acad. Child. Adolesc. Psychiatry. 42(4), 386–405 (2003).
Health Insurance Coverage of the Total Population (CPS). KFF. Published September 21, 2021. Accessed August 2, 2022. https://www.kff.org/other/state-indicator/health-insurance-coverage-of-the-total-population-cps/?currentTimeframe=2&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D.
Distribution of the Total Population by Federal Poverty Level (above and below 100% FPL). KFF. Published October 23, 2020. Accessed August 2, 2022. https://www.kff.org/other/state-indicator/population-above-and-below-100-fpl/?currentTimeframe=4&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D.
Davidson, C. L. & Wingate, L. R. Racial disparities in risk and protective factors for suicide. J. Black Psychol. 37(4), 499–516 (2011).
Lee, C. S. & Wong, Y. J. Racial/ethnic and gender differences in the antecedents of youth suicide. Cultur. Divers. Ethnic Minor. Psychol. 26(4), 532–543 (2020).
Assari, S. et al. Higher educational attainment is associated with lower risk of a future suicide attempt among non-hispanic whites but not non-hispanic blacks. J. Racial Ethn. Health Disparities. 6(5), 1001–1010 (2019).
Coley, R. Y., Johnson, E., Simon, G. E., Cruz, M. & Shortreed, S. M. Racial/ethnic disparities in the performance of prediction models for death by suicide after mental health visits. JAMA Psychiat. 78(7), 726–734 (2021).
Chauhan, P., Reppucci, N. D. & Turkheimer, E. N. Racial differences in the associations of neighborhood disadvantage, exposure to violence, and criminal recidivism among female juvenile offenders. Behav. Sci. Law. 27(4), 531–552 (2009).
Mallach, A. America’s Middle Neighborhoods: Setting the Stage for Revival. Lincoln Institute of Land Policy (2018).
Zandy, M. et al. Area-based socioeconomic disparities in mortality due to unintentional injury and youth suicide in British Columbia, 2009–2013. Health Promot. Chronic. Dis. Prev. Can. 39(2), 35–44 (2019).
Acknowledgements
This research has been funded in part by R01MH119177, U19MH121738, and P50MH113838.
Author information
Authors and Affiliations
Contributions
W.X., S.B., and J.P. designed the study. W.X. carried out the statistical analysis. W.X. wrote the initial draft of the manuscript. S.B., M.O., G.S.A., Y.X., and J.P. critically assessed and edited the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
Dr. Pathak is the Cofounder of Iris OB Health Inc., New York and has equity ownership. The other authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xi, W., Banerjee, S., Olfson, M. et al. Effects of social deprivation on risk factors for suicidal ideation and suicide attempts in commercially insured US youth and adults. Sci Rep 13, 4151 (2023). https://doi.org/10.1038/s41598-023-31387-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-31387-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.