Abstract
We investigated the association between cataract and allergic diseases, including atopic dermatitis (AD), allergic rhinitis (AR), and asthma using 2,631,015 subjects’ data from the 2009 National Health Insurance Service-Health Screening Cohort in Korea. Each allergic disease was defined as three or more occasions of diagnosis within 1 year with dedicated ICD-10 codes. The primary endpoint was newly received cataract surgery during the follow-up period. In total, 447,883 subjects had at least one allergic disease. During the mean follow-up of 7.8 ± 1.7 years, newly developed cataract surgery was observed in 301,693 subjects (allergic group, n = 69,321; non-allergic group, n = 232,372). After adjusting for demographic characteristics (age, sex), systemic and ocular comorbidities, socioeconomic status, and lifestyle factors (smoking, drinking, regular exercise), the allergic group had a higher hazard ratio (HR) for cataract development compared with the non-allergic group. We further performed a subgroup analysis for patients regarding sex and age. In the subgroup analysis of subjects with AD, men aged < 50 years had a higher HR compared to women of the same age group. In conclusion, subjects with allergic diseases had a higher risk of cataract surgery than their counterparts, and the combination of AD and AR resulted in the highest risk. Particularly, the association was more evident in male than female patients with AD aged < 50 years.
Similar content being viewed by others
Introduction
Allergic diseases are common in adults and children, and their prevalence has consistently increased over the last few decades1. Atopic dermatitis (AD), allergic rhinitis (AR), and asthma, which comprise the atopic triad, are the most common chronic allergic diseases. They have a common etiology, involving type II immune responses secondary to genetic and allergic factors. Each condition is distinct, with its own phenotype and pathogenesis1.
Approximately 25–40% of adults with AD also have ophthalmic problems, including blepharitis, conjunctivitis, tear film disturbances, keratoconus, uveitis, cataract, and retinal detachment2. Among these, the risk of developing cataract remains controversial; eye rubbing, inflammation, serum immunoglobulin E level, and glucocorticoid use may or may not be related to cataract. Previous studies have suggested that among the allergic diseases, AD is most frequently associated with an increased incidence of cataract3. In particular, shield-shaped anterior and posterior subcapsular cataracts are characteristic ocular comorbidities associated with AD4.
Most of the available studies that explored the association between cataracts and asthma, or AR have been limited because of the repetitive use of systemic corticosteroids and long-term intranasal corticosteroids among the study populations. Furthermore, reports that investigated cataracts of all severities, including mild to moderate disease, are scarce5,6,7. Interestingly, even in the same cohort population, studies that investigated the association between allergic diseases and the incidence of cataracts have shown different results. Lee et al. studied a cohort of adults with allergic diseases and concluded that the incidences of cataracts and glaucoma were significantly associated with AD8. However, another study of the same cohort reported that the incidence of cataracts was significantly associated with asthma and AR, but not with AD9. These differences may be because of variations in the disease definitions and study methods. The present study aimed to evaluate the association between allergic diseases and the risk of cataract in Koreans using the National Health Insurance Service-National Sample Cohort (NHIS-NSC) as the database. To eliminate selection bias, the study population was restricted to only visually affected patients with cataract who underwent cataract surgery. Additionally, the study population was categorized into women and men aged < 50 years and ≥ 50 years to further adjust the sex and age effect. The effect of pre-existing allergic disease on the incidence of cataracts was investigated.
Results
Baseline characteristics of the study population
Table 1 shows the baseline characteristics according to the presence of cataracts and allergic diseases, such as any allergy, AD, asthma, and AR. Of the total 2,631,015 study subjects, 301,693 (11.4%) underwent cataract surgery at least in one eye. Furthermore, 447,883 (17.0%), 10,631 (0.40%), 91,673 (3.5%), and 400,037 (16.7%) subjects had allergy, AD, asthma, and AR, respectively. The subjects in the cataract and allergic disease groups were older than those in the control group, and the former group had a significantly lower proportion of men than the latter group. The proportions of heavy alcohol consumers, current smokers, and individuals who did not exercise regularly were significantly lower in the cataract and allergic disease groups, excluding the asthma group, than in the control group. Cardiovascular risk factors, such as hypertension, diabetes mellitus (DM), and dyslipidemia, and obesity parameters, including body mass index (BMI) and waist circumference, were higher in the cataract and allergic disease groups than in the control group.
Incidence and risk of cataract in patients with allergic diseases
During a mean follow-up of 7.8 ± 1.7 years, newly developed cataract was observed in 301,693 subjects. Of these, 69,321 (19.74/1000 person-years) and 232,372 (13.64/1000 person-years) subjects were from the allergic and non-allergic groups, respectively. After adjusting for confounding factors (age, sex, smoking, drinking, regular exercise, low income, DM, hypertension, dyslipidemia, chronic kidney disease [CKD], BMI, glaucoma, and retinal vascular occlusion [RVO]), the allergic group had a higher hazard ratio (HR) of cataract development than the non-allergic group (HR = 1.241; 95% confidence interval [CI], 1.230–1.252) (Table 2). Among one, two, or three allergic diseases, three allergic diseases had shown the highest HR of cataract development (HR = 1.409; 95% CI, 1.213–1.637). Figure 1 shows a comparison of the cumulative incidence probabilities of cataracts according to any allergy, asthma, AD, and rhinitis. The incidence probability of cataract was higher over time in the allergic group than in the non-allergic group for all types of allergic diseases.
Comparison of cumulative incidence probability of cataract according to the allergic disease (a), asthma (b), atopic dermatitis (c), and allergic rhinitis (d). The incidence probability of cataract increases more over time in the allergic group than in non-allergic group for all different kinds of allergic disease.
Subgroup analysis of the association between cataract and atopic dermatitis
In all subgroups, subjects with any allergy, AD, AR, and asthma had an increased risk for cataract development (Tables S1–3, Table 3). In the subjects with allergy, there were significant differences in the risk of cataract development in the subgroups, except for hypertension, CKD, and regular exercise (Table S1). Interestingly, in subjects with AD, there were sex differences in the age and sex subgroups. After adjusting for confounding factors (age, sex, smoking, drinking, regular exercise, low income, DM, hypertension, dyslipidemia, CKD, and BMI), the male group aged < 50 years showed higher HR (1.713) (95% CI, 1.338–2.194) than the female group aged ≥ 50 years (HR, 1.193; 95% CI, 1.119–1.273) (Table 3). These trends were not observed in the subgroup analyses of other allergic diseases, such as any allergy, asthma, and AR (Tables S1–3).
Discussion
The current study was a nationwide, population-based cohort study investigating the risk of cataract surgery in patients with allergic diseases. We found that the subjects with allergic diseases were at an increased risk of visually affected cataracts, which would lead to cataract surgery. Among these, young male subjects were more sensitive to the association between allergic diseases and cataract surgery incidence than their counterparts. In addition, the combination of AD and AR resulted in the highest risk.
The association between AD and cataract has been suggested as a case report of dermatology study before the 1950s10,11,12,13. However, whether allergic diseases increase the risk of cataract development remains unclear, or the mechanism between allergic diseases and cataracts remains unknown. Previous population-based studies have reported conflicting results4,8,9. A longitudinal cohort study included pediatric subjects aged between 12 and 20 years using claims data and compared the incidence probabilities of cataract development and cataract surgery between AD and propensity score-matched controls4. Definitions of AD, cataract development, and cataract surgery were identified using diagnostic codes. The incidence of cataract development and cataract surgery was rare in the AD and control groups (0.12% vs. 0.14% and 0.04% vs. 0.02%, respectively). The results showed that the development of cataracts was not different between the AD and control groups, but cataract surgery was performed more frequently in the AD cohort than in the control group (0.075% vs. 0.041%; 95% CI, 0.017%–0.050%; P = 0.02). The limitation of the study was the possibility of underestimation of cataracts because the subjects were defined based on diagnostic codes. To reduce selection bias, the incidence of cataract surgery was evaluated; however, childhood cataract tends to be neglected because of lower awareness of vision discomfort, and the decision to perform cataract surgery is postponed because of the need for general anesthesia. We enrolled a different age group of over 20 years and found that subjects aged < 50 years tended to have an increased risk of cataract surgery when diagnosed and treated with AD, AR, and asthma in the subgroup analysis. We classified the subjects based on age because aging has been shown to be the strongest risk factor for the development of cataract14. Thus, the analysis of other factors that contribute to an increased prevalence of cataracts might have been masked by the age of the subjects in the current study.
The following two cross-sectional population-based studies using the same database obtained from the Fifth Korean National Health and Nutrition Examination Survey (KNHANES-V, 2010–2012) showed different results8,9. Lee et al.9 investigated the association between cataract development and allergic diseases in a population aged > 19 years. Cataract was defined as a history of ophthalmology or cataract surgery, and allergic diseases were defined as “yes” responses to the questions of diagnostic history. After adjusting the confounding factors, the odds ratio (OR) for cataract according to the presence of allergic diseases revealed that AR and asthma were significantly associated with cataracts (OR = 1.511, 95% CI = 1.120–2.039 and OR = 1.565, 95% CI = 1.192–2.054, respectively), whereas AD was not associated with cataract development. However, another nationwide study using the same database of over the age of 20 years reported different results8. Cataract was defined according to the standard Lens Opacities Classification System III. Through comparison with standard photographs, cataracts were categorized as cortical, nuclear, posterior subcapsular, or mixed. Subjects with AD were defined as those who answered “yes” to the question of a history of AD diagnosis by physicians. After adjusting the confounding factors, cataract was significantly associated with AD (OR, 1.85; 90% CI, 1.06–3.22; P = 0.031), and the patients with AD had a higher prevalence of ophthalmic surgery compared to those without AD (OR, 2.22; 95% CI, 1.07–4.61; P = 0.032).
A possible explanation for these conflicting results may be the misclassification of patients with cataract. Several clinical classifications and measurements have been used to evaluate cataracts15. However, these examinations have a common limitation of the subjective nature of grading and are influenced by observers with various slit lamp settings and training levels16,17. This could lead to inconsistencies of cataract diagnosis and interobserver bias. Moreover, recall bias in which the AD subjects were classified as the AD group by survey is a common limitation of studies using the KHANES database. In this study, we identified all subjects with AD, AR, and asthma using the relevant diagnostic code with repeated hospital visits more than three times a year and included only those subjects who underwent cataract surgery with a wash-up period of 1 year of cataract diagnosis or surgery prior to enrollment of cohort observation to reduce selection bias.
Although the pathogenesis of cataract in allergic diseases has been elucidated, several mechanisms have been postulated to explain this association. First, allergic diseases and cataracts share similar risk factors. Allergic diseases are related to individual components of metabolic risk, such as elevated blood pressure, blood glucose, and high cholesterol levels18,19, which may partly explain the increased incidence of cataract formation20,21. Other factors, including inflammation, clinical severity of AD, oxidative stress, and corticosteroid use, may contribute to cataract formation. A previous study showed that higher levels of aqueous flare were reported in atopic cataract and suggested the possible role of the blood-aqueous barrier in cataract formation in patients with AD22. In addition, tissue-destroying major basic protein derived from eosinophils was found in atopic cataracts, but not in any of the senile cataracts23. However, a previous study failed to reveal an increased risk of cataract development based on the severity of allergic diseases or systemic skin lesions. Instead, cataract development was observed in some patients with only facial involvement24. Similarly, we found that subjects with AD showed higher HR for cataract surgery compared to those with AR and asthma, indicating that eye rubbing or facial skin involvement may be an additive risk factor in cataract development. A previous prospective study of patients with AD showed that subjects with facial AD, contact lenses, or both may rub their eyes more frequently than those with lesions on other body parts, increasing their risk of cataract progression25.
In the subgroup analyses, this study found that AD, AR, and asthma were significantly associated with an increased incidence of cataracts, with a higher HR in men aged < 50 years. This result is unexpected, as previous studies have found that AD and respiratory allergy predominantly affect women after adolescence, following the start of menarche26,27. It was hypothesized that estrogen was responsible for the higher incidence and severity of allergic diseases in women after menarche27. Factors other than typical allergic inflammatory responses may contribute to the pathogenesis and underlying mechanism related to the higher incidence of cataracts in patients aged < 50 years. In a previous prospective study of presenile nuclear cataracts in individuals aged 30–49 years, 74 of the 266 patients had presenile nuclear cataracts. Of these, 63.5% were male. Current smoking habits, non-exercise or high amount of physical exercise, asthma, tuberculosis, and iron deficiency status were significantly associated with disease incidence28. Our results concurred with the finding that respiratory allergy was associated with an early incidence of cataracts in men. Another explanation for sex differences in the association between allergic diseases and cataract surgery is smoking. Various studies have shown that smoking is a risk factor for early-onset cataract due to oxidative stress and triggers the worsening of symptoms by increasing the number of inflammatory cytokines in allergic diseases27,29,30. Alternatively, other studies have hypothesized that the higher incidence of cataracts in men aged < 50 years may be associated with the disease control status of young men. We used the National Health Insurance Database and analyzed the medical service utilization of patients with AD, AR, and asthma over 5 years. We found that inpatient admissions and outpatient visits were predominant in women in all three disease groups. In contrast, there was a male predominance in emergency visits in all three disease groups31. This result suggests that failure to control the disease and acute exacerbations occurred more commonly in men than in women. The higher incidence of cataracts in men aged < 50 years may be associated with indifference and/or poor adherence to allergic disease management among young men. Another explanation may be that men aged < 50 years may have a greater tendency to undergo early surgical intervention than women because men are more socially active than women in Korea32.
This study has several strengths, including a large cohort of men and women, stable multiple-year follow-up, and high participation rate. However, this study has some limitations that should be discussed. First, the nature of the study design, using a claims database, could lead to Berkson’s bias. As the operation definition using the ICD-10 diagnostic code was included in the claims data, misclassification bias and the possibility of underreporting or overreporting cannot be excluded. To increase diagnostic accuracy, we defined AD, AR, and asthma as having at least three records of diagnoses per year in the current study33. Frequent visits to hospitals could help to enroll a higher number of subjects with active disease conditions. Second, because this was a nationwide study conducted in a single country with single race, the results may not be generalizable to all populations. This may be the strength of the study to some extent because it prevents the confounding effect of racial, cultural, environmental, and climate differences. As Koreans have relatively uniform genetic and environmental influences, the results may be more consistent than those of other large, population-based studies. Third, the history of steroid treatment for ocular allergy was not considered in this claims data analysis. Thus, it is difficult to evaluate the effect of topical and systemic steroid therapy on the development of cataracts using our claims data. The route (oral, skin, eye, and inhaled), dosage, and strength of steroid medications are highly variable, which hinders accurate measurement of the total amount of systemic steroids. We cautiously assumed that patients with the allergic triad tend to be treated with systemic and local steroids. Future prospective clinical trials comparing the incidence of cataract between patients receiving steroid and non-steroid therapy for allergy may be needed, although ethical issues should be solved. Otherwise, concurrent use of claims data and individual chart review may suggest a possible relationship between steroid therapy and cataract in patients with allergy, because certain types of cataract (i.e., posterior subcapular cataract) are known to be induced by drugs. Finally, observational studies using claims data limit causal inference with the possibility of residual confounding.
In conclusion, long-term follow-up data in the national claims database revealed that the allergic diseases increased the incidence of visually threatening cataracts (cataract surgery) in adults. Patients with AD and AR had the highest risk of cataract surgery among all allergic disease combinations. Adult patients with AD, especially middle-aged men, require screening for a combination of other allergic conditions and regular ophthalmologic examination for the future risk of cataract.
Methods
Study design and database
This was a population-based cohort study that used data from the NHIS in Korea. The NHIS provides comprehensive medical care coverage to 97% of the Korean population, including a standardized national health screening program for registrants aged 20 years or older every 2 years. It also provides data on demographics, socioeconomic status, medical treatments, procedures, and disease diagnoses according to the International Classification of Disease, Tenth Revision (ICD-10).
All subjects in the NHIS database are recommended to undergo national health checkups every 2 years. The health checkups include anthropometric data, blood pressure, and laboratory data, such as fasting glucose, cholesterol, and serum creatinine levels. Information on the previous medical history and lifestyle factors, including smoking, alcohol consumption, and regular physical activity, was collected using self-reported questionnaires. All methods were performed in accordance with relevant guidelines and regulations. This study complies with the principles of the Declaration of Helsinki. The Institutional Review Board of the Catholic University of Korea approved this study, and the need for informed consent for study was waived as part of the study approval.
Establishment of study cohort
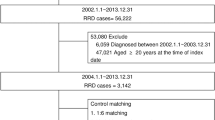
We initially selected 4,234,339 subjects aged older than 20 years who had undergone the NHIS health checkup from January 1, 2009, to December 31, 2009. In total, 1,338,019 subjects aged younger than 40 years and 114, 292 subjects with missing data were excluded. Moreover, 115,094 subjects with previous cataract surgery and 35,919 subjects diagnosed with cataract within 1 year from January 1, 2009, were also excluded. A total of 2,631,015 subjects were finally selected and observed through December 31, 2018. Considering the practice pattern for allergic diseases in Korea, prevalent allergic disease was defined as three or more occasions of diagnosis within 1 year with dedicated ICD-10 codes registered by physicians at the outpatient clinic.
Primary outcome and follow-up
The primary endpoint of this study was newly received cataract surgery at least once during the follow-up period. The cataract surgery group consisted of all subjects with a Korean Electronic Data Interchange (KEDI) code for cataract surgery. For each patient, cataract surgery was defined as the simultaneous claim of either “extracapsular or intracapsular” extraction (KEDI code S5111) or “phacoemulsification” (KEDI code S5119) and “primary intraocular lens implantation” (KEDI code S5117) on the same day. Procedures combined with vitrectomy or glaucoma surgery were excluded. The cohort was observed until the occurrence of the primary endpoint, cataract surgery, emigration, or until the end of the study period, whichever came first.
Definition of allergic diseases and comorbidities
The records of the ICD-10 Clinical Modification codes were used to define allergic diseases. The atopic triad, including asthma (J45-46), AR (J301-304), and AD (L20), was used to define allergic diseases. Subjects with at least one atopic disease were classified into the allergic disease group. The non-allergic group consisted of subjects without the atopic triad. To improve accuracy, data on allergic diseases were refined by dividing subjects according to the atopic triad diagnosis and number of clinic visits (three or more times per year) to diagnose each disease, which was validated in a previous epidemiological study in Korea33. Comorbidities, including hypertension (I10–I15), diabetes mellitus (E11–E14), and dyslipidemia (E78) were also defined on the basis of ICD-10 codes, as described in previous studies33.
Statistical analyses
Categorical variables are presented as numbers and relative frequencies (percentages) and were compared using the χ2 test. Normally distributed continuous variables are expressed as mean ± standard deviation and were analyzed using the independent t-test or analysis of variance test. The incidence rate of cataracts was calculated by dividing the number of incident cases by the total follow-up duration, which is presented as events per 1000 person-years. The HR and 95% CI for cataract development were analyzed using the Cox proportional hazards model. The following multivariate adjusted Cox proportional hazards models were applied: model 1 was non-adjusted; model 2 was adjusted for age (continuous variables) and sex; model 3 was adjusted for smoking, drinking, exercise, and income in addition to model 2; model 4 was adjusted for DM, hypertension, dyslipidemia, CKD, and BMI in addition to model 3; and model 5 was adjusted for glaucoma and RVO in addition to model 4.
Additionally, subgroup analyses were performed according to the following confounding factors: age, sex, BMI, DM, hypertension, dyslipidemia, smoking, CKD, drinking, exercise, low income, sex and age, RVO, and glaucoma. The Bonferroni correction was used for multiple comparisons in the subgroups. The cataract-free survival curve was estimated using the log-rank test. Statistical significance was defined as two-sided P < 0.05. All statistical analyses were performed using SAS (version 9.4, SAS Institute Inc., Cary, NC, USA).
Data availability
The datasets generated during and/or analyzed during the present study are available from the corresponding author on reasonable request.
References
Aw, M., Penn, J., Gauvreau, G. M., Lima, H. & Sehmi, R. Atopic march: Collegium internationale Allergologicum update 2020. Int. Arch. Allergy Immunol. 181, 1–10 (2020).
Pietruszyńska, M. et al. Ophthalmic manifestations of atopic dermatitis. Postepy Dermatol. Alergol. 37, 174–179 (2020).
Yamamoto, N. et al. Mechanism of atopic cataract caused by eosinophil granule major basic protein. Med. Mol. Morphol. 53, 94–103 (2020).
Jeon, H. S. et al. Association of pediatric atopic dermatitis and cataract development and surgery. JAMA Ophthalmol. 136, 912–918 (2018).
Barry, L. E. et al. Age and sex associations with systemic corticosteroid-induced morbidity in asthma. J. Allergy Clin. Immunol. Pract. 6, 2014-2023.e2 (2018).
Price, D. B. et al. Adverse outcomes from initiation of systemic corticosteroids for asthma: Long-term observational study. J. Asthma Allergy 11, 193–204 (2018).
Valenzuela, C. V. et al. Intranasal corticosteroids do not lead to ocular changes: A systematic review and meta-analysis. Laryngoscope 129, 6–12 (2019).
Lee, S. H., Lee, S. H., Lee, S. H. & Park, Y. L. Cataract, glaucoma, and dry eye disease in adults with atopic dermatitis: A nationwide cross-sectional study from the Republic of Korea. Ann. Dermatol. 31, 37–43 (2019).
Lee, Y. B. et al. Association between allergic diseases and ophthalmologic diseases, including cataracts and glaucoma, using the Korean National Health and Nutrition Examination survey 2010–2012: A STROBE-compliant article. J. Dermatol. 45, 463–467 (2018).
Bair, B., Dodd, J., Heidelberg, K. & Krach, K. Cataracts in atopic dermatitis: A case presentation and review of the literature. Arch. Dermatol. 147, 585–588 (2011).
Chen, C. C., Huang, J. L., Yang, K. D. & Chen, H. J. Atopic cataracts in a child with atopic dermatitis: A case report and review of the literature. Asian Pac. J. Allergy Immunol. 18, 69–71 (2000).
Mondzelewski, L., Hagan, C. & White, A. A. An 18-year-old male with severe bilateral cataracts and atopic dermatitis—a case report and review of the literature. Pediatr. Dermatol. 26, 583–586 (2009).
Niedelman, M. L. Bilateral matured cataracts complicating atopic dermatitis. Arch. Derm. Syphilol. 53, 663 (1946).
Asbell, P. A. et al. Age-related cataract. Lancet 365, 599–609 (2005).
Chylack, L. T. Jr. et al. The lens opacities classification system III The longitudinal study of cataract study group. Arch. Ophthalmol. 111, 831–836 (1993).
Kirwan, J. F., Venter, L., Stulting, A. A. & Murdoch, I. E. LOCS III examination at the slit lamp, do settings matter?. Ophthal. Epidemiol. 10, 259–266 (2003).
Tan, A. C., Loon, S. C., Choi, H. & Thean, L. Lens Opacities Classification System III: Cataract grading variability between junior and senior staff at a Singapore hospital. J. Cataract Refract. Surg. 34, 1948–1952 (2008).
Drucker, A. M., Qureshi, A. A., Dummer, T. J. B., Parker, L. & Li, W. Q. Atopic dermatitis and risk of hypertension, type 2 diabetes, myocardial infarction and stroke in a cross-sectional analysis from the Canadian Partnership for Tomorrow Project. Br. J. Dermatol. 177, 1043–1051 (2017).
Wang, L., Gao, S., Yu, M., Sheng, Z. & Tan, W. Association of asthma with coronary heart disease: A meta-analysis of 11 trials. PLoS ONE 12, e0179335 (2017).
Lee, D. S. et al. The gender-dependent association between obesity and age-related cataracts in middle-aged Korean adults. PLoS ONE 10, e0124262 (2015).
Lindblad, B. E., Håkansson, N. & Wolk, A. Metabolic syndrome and some of its components in relation to risk of cataract extraction. A prospective cohort study of men. Acta Ophthalmol. 97, 409–414 (2019).
Matsuo, T., Saito, H. & Matsuo, N. Cataract and aqueous flare levels in patients with atopic dermatitis. Am. J. Ophthalmol. 124, 36–39 (1997).
Yokoi, N. et al. Association of eosinophil granule major basic protein with atopic cataract. Am. J. Ophthalmol. 122, 825–829 (1996).
Brandonisio, T. M., Bachman, J. A. & Sears, J. M. Atopic dermatitis: A case report and current clinical review of systemic and ocular manifestations. Optometry 72, 94–102 (2001).
Nagaki, Y., Hayasaka, S. & Kadoi, C. Cataract progression in patients with atopic dermatitis. J. Cataract Refract. Surg. 25, 96–99 (1999).
Barbarot, S. et al. Epidemiology of atopic dermatitis in adults: Results from an international survey. Allergy 73, 1284–1293 (2018).
Ridolo, E. et al. Sex in respiratory and skin allergies. Clin. Rev. Allergy Immunol. 56, 322–332 (2019).
Nam, S. W. et al. Risk factors of presenile nuclear cataract in health screening study. BMC Ophthalmol. 18, 263 (2018).
Strzelak, A., Ratajczak, A., Adamiec, A. & Feleszko, W. Tobacco Smoke induces and alters immune responses in the lung triggering inflammation, allergy, asthma and other lung diseases: A mechanistic review. Int. J. Environ. Res. Public Health 15, 1033 (2018).
Ye, J. et al. Smoking and risk of age-related cataract: A meta-analysis. Invest. Ophthalmol. Vis. Sci. 53, 3885–3895 (2012).
Yoo, S. et al. Data resource profile: The allergic disease database of the Korean National Health Insurance Service. Epidemiol. Health 43, e2021010 (2021).
Na, K. S., Park, Y. G., Han, K., Mok, J. W. & Joo, C. K. Prevalence of and risk factors for age-related and anterior polar cataracts in a Korean population. PLoS ONE 9, e96461 (2014).
Choi, Y. J. et al. Increased risk of atrial fibrillation in patients with atopic triad: A nationwide population-based study. J. Allergy Clin. Immunol. Pract. 9, 3422-3430.e5 (2021).
Acknowledgements
This study was supported by a grant from the National Research Foundation of Korea (NRF) (2019R1G1A1100659, 2022R1A2C2006109) and by a grant from the Catholic University Yeouido St. Mary’s Hospital in the program year of 2022.
Author information
Authors and Affiliations
Contributions
Study conception and design: J.P., Y.H.C. and K.N.; analysis and interpretation of the data: J.P., K.H. and K.N.; acquisition of data: K.H., G.N., H.S.H. and S.-K.P.; revising or reviewing the manuscript: J.P., G.N., S.-K.P., H.S.H., Y.H.C. and K.N. All authors were involved in drafting the article or revising it critically for important intellectual content and approved the final version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Paik, JS., Han, K., Nam, G. et al. Increased risk of cataract surgery in patients with allergic disease: a population based cohort study. Sci Rep 12, 21258 (2022). https://doi.org/10.1038/s41598-022-25589-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-25589-1
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.