Abstract
Traumatic brain injury (TBI) is frequently associated with neuropsychiatric impairments such as symptoms of post-traumatic stress disorder (PTSD), which can be screened using self-report instruments such as the Post-Traumatic Stress Disorder Checklist for DSM-5 (PCL-5). The current study aims to inspect the factorial validity and cross-linguistic equivalence of the PCL-5 in individuals after TBI with differential severity. Data for six language groups (n ≥ 200; Dutch, English, Finnish, Italian, Norwegian, Spanish) were extracted from the CENTER-TBI study database. Factorial validity of PTSD was evaluated using confirmatory factor analyses (CFA), and compared between four concurrent structural models. A multi-group CFA approach was utilized to investigate the measurement invariance (MI) of the PCL-5 across languages. All structural models showed satisfactory goodness-of-fit with small between-model variation. The original DSM-5 model for PTSD provided solid evidence of MI across the language groups. The current study underlines the validity of the clinical DSM-5 conceptualization of PTSD and demonstrates the comparability of PCL-5 symptom scores between language versions in individuals after TBI. Future studies should apply MI methods to other sociodemographic (e.g., age, gender) and injury-related (e.g., TBI severity) characteristics to improve the monitoring and clinical care of individuals suffering from PTSD symptoms after TBI.
Similar content being viewed by others
Introduction
Traumatic brain injury (TBI) is characterized by an alteration in brain functions, or other cerebral pathology, resulting from an external force1. TBI poses a highly relevant challenge for health care systems worldwide with over 50 million prevalent cases globally2 and is associated with substantial societal costs as well as individual burden to patients and caregivers3,4. In Europe, the number of TBI-related deaths per year is estimated at about 82,0005 with incidental falls and road traffic accidents as the main causes of TBI6. Although the vast majority of TBI cases (70–90%) are classified as ‘mild’7, TBI is commonly associated with elevated rates of long-term neuropsychiatric and cognitive deficits8,9.
Post-traumatic stress disorder (PTSD) is among the most frequently reported psychiatric conditions associated with TBI10, mediated by various biological and psychological mechanisms11. According to the latest version of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5)12 PTSD manifests in symptoms of intrusion and hyperarousal among others that emerge after the exposure to actual or threatened death, serious injury, or sexual violence. PTSD prevalence rates range between 0.38% and 6.67% in general populations across Europe related to various trauma causes13. Importantly, a recent review by Conroy and colleagues (2020)14 noted that while affective disturbances in general are common comorbidities also in other neuropsychiatric diseases (i.e., stroke, Parkinson’s disease, multiple sclerosis), the relationship between PTSD and TBI is particularly distinct since both conditions are likely to emerge from a shared traumatic experience. Indeed, an elevated prevalence of comorbid PTSD (15.6%) can be observed in subjects after TBI, constituting a 73% higher risk of manifestation compared with individuals who exclusively sustained extracranial bodily injuries15. However, the emergence of PTSD may pass unnoticed in individuals after TBI due to the overlap in etiology, neuropsychiatric symptoms (e.g., headaches, hypersensitivity, sleep disturbances, impulsivity), and pathophysiological mechanisms between the two conditions16. As the treatment of PTSD is associated with major costs and burdens17,18, the implementation of valid instruments to evaluate PTSD symptoms is greatly important in order to ensure the appropriate therapy and thereby to substantially reduce the financial and social strain in the field of TBI.
The Post-Traumatic Stress Disorder Checklist (PCL)19 is a self-report screening tool for PTSD symptoms that can assist in identifying subjects in need of psychiatric treatment. Its most recent version (PCL-5)20 was updated based on the revised DSM-5 diagnostic criteria for PTSD, which propose the underlying disease dimensions following a traumatic experience (criterion A) to be intrusion (criterion B), avoidance (criterion C), negative alterations in cognition and mood (criterion D), and alterations in arousal and reactivity (criterion E). The PCL-5 assesses common symptoms contained in criteria B to E. However, the DSM-5 conceptualization of PTSD has been repeatedly challenged, as concurrent latent dimensions of psychopathology have been put forward by a broad range of factor analytic studies using the PCL-521. To date the debate about the characteristic factor structure of PTSD remains ongoing. In order to ensure valid psychopathological assessments, a thorough investigation of the factorial validity of PTSD measured using the PCL-5 is crucial.
Several language versions of the PCL-5 have been validated and have demonstrated good to excellent psychometric properties22,23,24,25,26,27,28,29,30. Recent work additionally demonstrated the validity of multiple PCL-5 translations in individuals after TBI and reported, for instance, a moderate to strong negative relationship of PTSD symptomatology with subjects’ functional recovery following TBI31. However, while instrument translation implies the equivalent assessment of the latent construct (i.e., PTSD) between language versions, empirical evidence for this assumption is required. The concept of measurement invariance (MI)32 describes the condition that equal item scores between subjects or groups should convey equal information, so that a lack of MI would result in a biased or misleading interpretation of individual symptomatology33. Thus, analyses of MI allow conclusions to be drawn as to whether group differences in mean scores are attributable to a ‘true’ variation in latent symptomatology rather than measurement error or bias. Prior research has demonstrated a lack of comprehensive MI in PTSD symptom scores assessed using a previous version of the PCL (i.e., PCL-C) when comparing military personnel with and without recent deployment34. This finding suggested that differences in symptom scores were extensively impacted by variables unrelated to the underlying latent PTSD psychopathology, prompting a further revision of the instrument. With regard to the PCL-5, initial evidence showed fundamental MI of the English and French versions in healthy individuals35. However, investigations of MI across multiple language versions of the PCL-5 in populations after TBI have not yet been conducted. Besides cross-linguistic comparisons, studies may utilize MI analyses to further enhance the understanding of PTSD symptomatology within or across the general population and specific clinical samples. First evidence in favor of MI of the PCL-5 in individuals who had experienced a single trauma or multiple trauma types was found36, while no evidence for MI in PTSD symptoms scores between trauma-exposed college students and military veterans was observed37. These results represent important steps towards the validation of the PCL-5 and its comparability in different populations but evidence across more clinical features is called for. The required data basis for bridging this gap is provided by large-scale international multicenter studies that assess a variety of psychopathological outcome parameters across a wide array of subject characteristics and language groups38,39.
The main aims of the current study were to understand the latent factor structure of PTSD in individuals after TBI and to investigate the equivalence of symptom assessments across multiple language versions of the PCL-5 applying MI procedures. Evidence in favor of MI would suggest that the PCL-5 can be used to assess one and the same latent construct of PTSD across all tested languages, allowing for data aggregation and direct comparisons of the PTSD symptomatology after TBI. Finally, MI analyses were conducted in individuals with different levels of recovery and severity of TBI in an effort to strengthen the applicability of the PCL-5 in TBI populations.
Results
Sociodemographic and injury-related data are presented in Table 1. The total sample comprised 1776 individuals within six language subgroups (Dutch: n = 586, English: n = 213, Finnish: n = 212, Italian: n = 261, Norwegian: n = 248, Spanish: n = 256). Notable variations were observed in the descriptive characteristics. Most prominently, the proportion of participants with a previous history of psychological problems in the English subsample (22.07%) was distinctly above the total average (12.27%). Moreover, reference of the PCL-5 to the TBI experience was reported only by a minority of Dutch-speaking individuals (39.08%) in contrast to the remaining language groups (72.30–84.77%). Pronounced PTSD symptomatology (i.e., PCL-5 ≥ 31) was present in 10.7% of all participants, with the lowest proportion in the Finnish (7.08%) and the highest rate in the Italian (17.24%) subsamples. Statistical analyses by means of ANOVA and Kruskal–Wallis tests showed that Dutch-speaking subjects were significantly older compared with most other language groups, Finnish individuals presented more favorable recovery and fewer extracranial injuries, and the Italian subsample suffered from more severe TBI and PTSD symptoms. However, the overall effect sizes of the observed differences were small (ds: 0.19–0.36) (Table A1 in Appendix). For an overview of the sociodemographic and injury-related characteristics in individuals after ‘ultra-mild’ or more severe TBI, see Table D1 in the Appendix.
Structural Validity
In all four candidate models the majority of items had high loadings (βs ≥ 0.80) on the respective proposed factors. No loadings below the cutoff (β < 0.50) were observed (Table 2). Goodness-of-fit parameters were satisfactory for all tested models (Table 3). The variation in the goodness-of-fit indices showed a slightly better fit for the concurrent models compared with the original DSM-5 model. However, overall differences in model fit were small. Since all candidate models showed a similarly satisfactory fit, subsequent MI analyses were conservatively based on the theory-driven DSM-5 conceptualization of PTSD.
Measurement invariance
Preparatory data inspection revealed that there were no subjects who used the response category 4 (‘extremely impaired’) with regard to a small number of PCL-5 items in the Finnish (i.e., Flashbacks, Reckless behavior, Cued physical reactions) and Norwegian (i.e., Dreams) subsamples. In keeping with the requirements of the MI approach the response categories 3 (‘quite a bit impaired’) and 4 (‘extremely impaired’) were collapsed for these items in all subsamples. Model fit statistics for the main MI analyses are presented in Table 4. Goodness-of-fit was excellent for all MI models. The variation in the descriptive fit indices was below the respective cutoff values and likelihood ratio tests suggested no significant fit differences between the MI models. Equal fit of all MI models was inferred, thus providing evidence for the structural equivalence of PTSD assessment across the total sample.
See Table C1 in the Appendix for the results of the complimentary analyses which retained the original response categories across all PCL-5 items in a subset of the total sample (N = 1316), excluding the Finnish and Norwegian subsamples due to their limited use of the response category 4 (‘extremely impaired’) in a few items. Goodness-of-fit was satisfactory for all MI models, the differences between the descriptive fit indices were minimal, and the likelihood ratio tests indicated no significant fit difference. Therefore, complimentary analysis using the original response format across all items underlined the main findings of equivalent PTSD assessment across the tested PCL-5 language versions in civilians after TBI.
With regard to comparisons of ‘ultra-mild’ with more severe TBI cases, data inspection revealed that in the ‘ultra-mild’ group no individuals indicated the response category 4 (‘extremely impaired’) in three items (i.e., Dreams, Irritability or aggressive behavior, Startle). Consequently, the response categories 3 (‘quite a bit impaired’) and 4 (‘extremely impaired’) were collapsed for these items across the ‘ultra-mild’ and more severely impaired individuals. The results of the subsequent MI analyses are presented in Table 5. Goodness-of-fit was excellent for all MI models, minimal differences between the descriptive fit parameters were observed, and the results of the likelihood ratio tests indicated no significant differences in model fit between MI models. Therefore, an equal fit across all MI models was concluded and evidence for the structurally equivalent assessment of PTSD symptoms using the PCL-5 between completely recovered individuals and those who sustained a more severe TBI was obtained.
Discussion
The current study aimed to examine the latent factorial structure and cross-linguistic invariance of the PCL-5 as an assessment tool for PTSD symptomatology using data collected in the CENTER-TBI study. Although validation has been available for several language versions of the PCL-522,31, this is the first study to evaluate whether measurements of PTSD symptoms were equivalent in six language groups (i.e., Dutch, English, Finnish, Italian, Norwegian, Spanish) of civilians after TBI. PTSD symptomatology was prevalent in all language subsamples with the proportions of highly affected individuals ranging between 7.08 and 17.24%, which is in line with previous reports15. Subsequent structural analyses resulted overall in a satisfactory fit for four structural models of PTSD, including the clinical DSM-5 conceptualization. Applying MI procedures conservatively based on the theory-driven DSM-5 model provided solid evidence for equivalent PCL-5 assessments. Therefore, symptom scores both across the tested language versions as well as between individuals after ‘ultra-mild’ or more severe TBI can be considered comparable. The presented evidence points towards the applicability of the PCL-5 in these populations.
In order to reduce the risk of substantial sampling bias when analyzing the generalizability of PTSD measurement across multiple language versions homogeneity of sociodemographic and injury-related variables across subsamples was desirable. The results of the descriptive analyses revealed sufficiently low variability in the current study. Although the injury characteristics differed significantly across language subsamples, the effect sizes were small and the risk of statistical artifacts was elevated by the relatively large subgroup sample size required for MI analyses40. Interestingly, individuals in the Dutch-speaking subsample were relatively old, had mostly experienced TBI resulting from incidental falls, often referred their answers in the PCL-5 to traumatic events other than the TBI experience, and showed rather mild symptoms of TBI and PTSD. Based on this observation, the relationship between functional outcomes and descriptive statistics including type, count, and timepoint of trauma needs further investigation. Previous studies have demonstrated the generalizability of PCL-5 assessments across descriptive strata such as gender41 or single- and multi-trauma types36. Future research should investigate equivalence across additional sociodemographic factors (e.g., age, education)42,43, injury-related characteristics (e.g., TBI severity, injury cause, healthy populations and non-TBI patients), and physical comorbidities (e.g., diabetes, cancer)44 in order to ensure a conclusive interpretation of symptom scores across subjects with diverse traits in clinical settings.
The current study reproduced previous findings on the structural validity of the PCL-5 in the Dutch subsample in CENTER-TBI45, extended the conclusions to five additional language subsamples and found satisfactory goodness-of-fit for the original DSM-5 model as well as concurrent models. As previously shown23,27,46,47, the concurrent models exhibited a better fit compared with the DSM-5 model. However, all concurrent models introduced structural factors that comprised fewer than three questionnaire items leading to reduced statistical robustness48. The higher number of latent factors in both the Anhedonia and the Hybrid models additionally led to increased model complexity. Thus, further statistical analyses were based conservatively on the theory-driven DSM-5 model which provided robust results that offer strong practical utility. Nonetheless, examinations of latent symptom dimensions add to the understanding of pathological factors central to PTSD and should be studied further to improve therapeutic treatment.
The current study exhibited a number of strengths. Firstly, results were based on high-quality multicenter data that representatively encompassed the complete TBI severity spectrum7. Due to this, it was possible to draw reliable conclusions for individuals after TBI. Furthermore, potential sources of bias in the descriptive characteristics across language subsamples were minimal and the factorial structure of the PCL-5 was verified. Finally, this is the first study to date that provides evidence for the comparability of PCL-5 scores across six language versions by applying robust statistical methods to test for MI. Therefore, the reported results uniquely validate comorbid PTSD assessments in the field of TBI.
The present investigation was limited by the inherent overlap of neuropsychiatric symptoms resulting from TBI experience and PTSD symptomatology, thereby posing a confounding effect in PCL-5 assessments16. However, while the extent to which scale scores represented expressions of PTSD as opposed to TBI symptomatology remains unclear, assessment of individuals after TBI increased the variance in the PCL-5 scores and prevented floor effects. Interestingly, we observed a lack of extreme impairment with regard to certain PTSD symptoms (i.e., Dreams, Flashbacks, Reckless behavior, Cued physical reactions) in the Finnish and Norwegian subsamples. Although overall differences in TBI severity were small across all language groups, the majority of Finnish and Norwegian individuals suffered from relatively mild TBI. Hence, the manifestation of these particular symptoms as PTSD-specific in contrast to injury-related in populations after TBI should be studied more extensively. Nonetheless, comparability of PCL-5 scores was established by adapting the response categories in the respective items and remained unchanged after the Finnish and Norwegian subsamples had been excluded. Moreover, the MI approach applied in the current study produced reasonable and durable results for the given dataset. Nonetheless, the application of alternative procedures for multi-group equivalence testing in differential data structures should be examined as well, for instance based on Item Response Theory49, Exploratory Structural Equation Modelling50, or Bifactor Models21. Moreover, we employed a previously proposed approach to identify a subset of ‘ultra-mild’ TBI cases51 which served as proxies for healthy individuals in the current analyses. However, since subjects in the ‘ultra-mild’ group were still TBI-affected to a certain degree, further investigations based on suitable datasets will be necessary to allow for robust conclusions on the comparability of the PCL-5 between general population samples and individuals after TBI. Finally, since the vast majority of TBI cases are classified as mild and may receive differential treatment of PTSD symptoms among other psychosocial disturbances depending on the inclusion in a specific clinical care pathway (i.e., emergency room, ward, intensive care), the characteristics of the recovery rates in individuals after mild TBI should be investigated further.
The reported results underline the validity of the DSM-5 structure of PTSD as well as the comparability of PCL-5 scores across all tested language versions and different levels of recovery and severity of TBI. Hence, differences in test scores can be attributed to underlying ‘true’ differences in PTSD symptomatology rather than systematic sampling bias or measurement error. Future studies should examine the equivalence of PTSD assessments in additional subject groups and should investigate factors impacting PTSD symptomatology following TBI.
Materials and methods
Data
All the analyses in the present investigation utilized data from the Collaborative European NeuroTrauma Effectiveness Research in Traumatic Brain Injury (CENTER-TBI) project, supported by the European Union (EU) Framework 7 program (EC grant 602,150; clinicaltrials.gov NCT02210221)38. This prospective observational cohort study aimed to improve the characterization and clinical care of subjects after TBI. Data was sampled from the CENTER-TBI core study which comprises information on 4509 individuals who participated at 63 institutional sites across 18 countries between December 2014 and December 2017. The inclusion criteria for participation were a clinical diagnosis of TBI, indication for a computed tomography (CT) scan and presentation to the study center within 24 h post injury. Individuals with severe pre-existing neurological disorders (e.g., epilepsy, cerebrovascular accident) were excluded52.
The CENTER-TBI study was conducted in accordance with all relevant laws of the EU which were directly applicable or had a direct effect, as well as all the relevant laws of the countries in which the recruiting sites were located, including but not limited to, the relevant privacy and data protection laws and regulations (‘Privacy Law’), the relevant laws and regulations on the use of human materials, and all relevant guidelines relating to clinical studies including, but not limited to, the ICH Harmonized Tripartite Guideline for Good Clinical Practice (CPMP/ICH/135/95) (‘ICH GCP’) and the World Medical Association Declaration of Helsinki entitled ‘Ethical Principles for Medical Research Involving Human Subjects’. Ethical approval was attained for each recruitment site. Informed consent was obtained for all subjects recruited in the CENTER-TBI core study with documentation in electronic case report forms (e-CRF, QuesGen Systems Incorporated, Burlingame, CA, USA).
All methods employed in the current study were carried out in accordance with relevant guidelines and regulations. Furthermore, the experimental protocol of this study was approved by the management committee of CENTER-TBI: proposal #70, https://www.center-tbi.eu/data/approved-proposals.
Ethical approval
The list of sites, ethics committees, approval numbers, and approval dates can be found on the official website of the CENTER-TBI project: www.center-tbi.eu/project/ethical-approval. The CENTER-TBI study received clearance from the following ethics committees: Ethikkommission der Medizinischen Universität Wien, Austria (1646/2014); Ethikkommission der Medizinischen Universität Innsbruck, Austria (AN2014-0,336,343/4.22); Centraal Ethisch Comité—Ethisch Comité Universitair Ziekenhuis Antwerpen en de Universiteit Antwerpen, Belgium (B300201422714); Comité d'Ethique Liège 412, Belgium (1427); Comité d'Ethique hospitalo-facultaire niversitaire de Liège 707, Belgium (B707201422102/2014–244); Comissie Medische Ethiek UZ KU Leuven, Belgium (B322201523981/S57019; ML11365); De Videnskabsetiske Komitéer for Region Syddanmark Odense/Copenhagen, Denmark (S-20140215); Varsinais suomen sairaanhoitopiirin kuntayhtyma—Eettinen Toimikunta Turku/Helsinki, Finland (95/1801/2014); Agence Nationale de Sécurité du Médicament et des Produits de Santé ANSM Paris/Besançon/Lille/Grenoble/Nancy/Poitiers, France (141421B-31); Ethikkommission Medizinsche Fakultät Heidelberg/Ludwigsburg, Germany (S-435/2014); Ethikkommission an der Medizinsche Fakultät Berlin, Germany (1098/15); Ethikkommission an der Medizinsche Fakultät Aachen, Germany (EK 174/15); ETT TUKEB Egészségügyi Tudományos Tanács Pecs/Szeged, Hungary (42,558–3/2014/EKU); Pécsi Tudományegyetem Pecs, Hungary (5421); Szegedi Tudományegyetem Szeged, Hungary (3803); Helsinki Committee, Rambam Health Care Campus Haifa, Israel (RMB 373-14); Hadassah Medical Organization IRB Jerusalem, Israel (0590-16 HMO); Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico—Direzione Scientifica Comitato Etico Milan, Italy (542/2014); Comitato Etico—Ospedale San Raffaele Milan/Padova, Italy (217/2014); Comitato Etico Interaziendale A.O.U. Città della Salute e della Scienza di Torino—A.O. Ordine Mauriziano—A.S.L. Torino, Italy (0,015,269); Comitato Etico IRST IRCCS AVR Cesena, Italy (1675/2015 I.5/207); Comitato Etico Della Provincia Monza Brianza Monza, Italy (1978/2014); Comitato Etico Interaziendale A.O.U. ‘Maggiore della Carità’ Novara, Italy (CE 46/15); Comitato Etico—Ospedale Niguarda Ca’ Granda Milan, Italy (636–122,015); Ethics Commiitee for Clinical Research at Pauls Stradins Clinical University Hospital Development Society Riga/Rezekne, Latvia (171,215-1E); VILNIAUS REGIONINIS BIOMEDICININIŲ TYRIMŲ ETIKOS KOMITETAS Vilnius, Lithuania (158,200-15-801-323); KAUNO REGIONINIS BIOMEDICININIŲ TYRIMŲ ETIKOS KOMITETAS Kaunas, Lithuania (BE-2-6); Leids Universitair Centrum—Commissie Medische Ethiek Leiden/Rotterdam/the Hague/Nijmegen/Tilburg/Groningen, Netherlands (P14.222/NV/nv); Regional komité for medisinsk og helsefaglig Tromso/Trondheim/Oslo, Norway (2014/1454); Comitetului de Etica a Spitalului Clinic Judeteam de Urgenta Timisoara, Romania (16-OCT-2014); Etidkog odbora Klinidkog centra Vojvodine Novi Sad, Serbia (00-08/332); Comité Etico de Investigacion Clinica del Hospital Universitario 12 de Octubre Madrid, Spain (14/262); Comité ético de investigación clínica y comisión de proyectos de investigación del hospital universitari Vall d'Hebron Barcelona, Spain (ID-RTF080); Comité Etico de Investigacion Clinica de Euskadi Bilbao, Spain (PI2014158); Comité Etico de Investigacion Clinica del Clínico Universitario de Valencia, Spain (F-CE-GEva-15); EPN (Regionala Etikprövningsnämnden i Stockholm) Stockholm/Umea, Sweden (2014/1473-31/4); La Commission cantonale (VD) d’éthique de la recherche sur l'être humain (CER-VD) Lausanne, Switzerland (473/11); NHS HRA Birmingham/Cambridge/Southampton/Sheffield/London/Salford/Liverpool/Bristol, United Kingdom (14/SC/1370); UHB Research Governance Office—Queen Elizabeth Hospital Birmingham, United Kingdom (RRK5224); Research and Development Department—Cambridge University Hospital NHS Foundation Trust Cambridge, United Kingdom (AO93184); Research Governance Office—University Hospitals Southhampton NHS Trust Southampton, United Kingdom (RHM CRI0294); Research and Development Department—Sheffield Teaching Hospitals NHS Foundation Trust Sheffield, United Kingdom (STH18187); Research & Innovation Office—Kings college London NHS Foundation Trust London, United Kingdom (KCH15-204); Research and Development Department—Salford Royal Hospital NHS Foundation Trust Salford, United Kingdom (2015/025ET); Research & Innovation Office—The Walton centre NHS Foundation Trust Liverpool, United Kingdom (RG154-15); Research & Innovation—North Bristol NHS Trust Bristol, United Kingdom (3427); NHS Scotland Edinburgh, United Kingdom/Scotland (14/SS/1086); Research and Development Department—University Hospitals Division NHS Lothian Edinburgh, United Kingdom/Scotland (2015/0171).
Study population
Data were extracted for adult subjects (age ≥ 16 years) who had completed psychopathological assessments at 6 months (− 1/ + 2 months) post injury. Subjects across the entire TBI severity spectrum were included in this study. Sociodemographic information was acquired at the time of enrollment into the CENTER-TBI study and included the subjects’ age, gender, marital status, education, occupation, self-reported pre-TBI history of psychiatric disorders, and cause of injury.
Participant data were aggregated by native language, further details can be found elsewhere31 and the application of MI analyses required the selection of language groups with a suitable sample size of n ≥ 20040. For details on the sample attrition in the current study, see Fig. 1.
Injury-related variables
Extracranial injury severity was assessed using the Injury Severity Score (ISS) derived from the Abbreviated Injury Scale score53,54. ISS values can range from 0 to 75 with higher scores indicating greater impairment and the threshold for clinical impairment at 16. TBI severity was assessed at baseline by applying the Glasgow Coma Scale (GCS)55. GCS scores from 13 to 15 indicate mild, 9 to 12 moderate, and 3 to 6 severe TBI. Mild TBI can be further differentiated into complicated (GCS ≥ 13 with CT abnormalities) and uncomplicated (GCS ≥ 13 without CT abnormalities)52. Moreover, the Glasgow Outcome Scale Extended (GOSE)56 was administered as a clinician-reported measure of functional recovery at six months following TBI and was scored on an eight-point scale (1 = dead, 2 = vegetative state, 3/4 = lower/upper severe disability, 5/6 = lower/upper moderate disability, 7/8 = lower/upper good recovery). More details on GOSE data extraction are provided elsewhere31. Finally, in accordance with a recently reported procedure51 we considered individuals who had a complete recovery (GOSE = 8) from the mildest degree of TBI (GCS = 15) without any CT abnormalities as ‘ultra-mild’ cases in the TBI severity spectrum. This classification was used to determine whether the PCL-5 is able to capture PTSD symptomatology in the same way in those completely recovered compared to more severely injured subjects.
PTSD symptoms
PTSD severity was evaluated using the PCL-520,23. The PCL-5 is a self-report questionnaire comprising 20 PTSD symptoms which correspond to four diagnostic criteria proposed in the DSM-5 (i.e., criterion B: intrusion, criterion C: avoidance, criterion D: negative alterations in cognition and mood, criterion E: alterations in arousal and impulsivity)12. Individuals reported their impairment during the past month on a Likert scale ranging from 0 (not at all) to 4 (extremely). Total scores can range from 0 to 80 with higher values indicating greater symptom severity and can be used to screen for clinical levels of PTSD symptomatology with cutoffs of 31 to 33 in civilian populations35,57. In accordance with previous research in the field of TBI45, a screening cutoff of 31 was applied in the current study. Finally, to examine the nature of the traumatic experience (criterion A) associated with the PTSD symptoms, subjects were surveyed whether they completed the PCL-5 in reference to the TBI event (‘When you responded to the questions in this questionnaire were your answers in reference to the stressful experience which caused your traumatic brain injury?’).
The original version of the PCL-5 is openly available from the website of the National Center for PTSD: https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp (last accessed on 17.11.2021). For the CENTER-TBI study the PCL-5 was translated and linguistically validated following a standardized protocol (for details, see58) as well as psychometrically tested31. All language versions can be retrieved from the CENTER-TBI website: https://www.center-tbi.eu/project/validated-translations-outcome-instruments (last accessed on 23.11.2021).
Statistical analyses
Descriptive statistics are presented for sociodemographic characteristics as well as injury-related variables in the total sample and the language subsamples. Detailed information on the psychometric properties of the PCL-5 language versions in CENTER-TBI, both at the item level as well as at the scale level, can be found elsewhere31. Differences between language groups with respect to age were examined using an ANOVA and post-hoc Tukey HSD tests accounting for multiple comparisons. Differences in injury-related variables (i.e., GOSE, GCS, ISS, PCL-5) were tested via Kruskal–Wallis tests with post-hoc pairwise Mann–Whitney-U-tests and corrected for multiple comparisons (see Table A1). Effect sizes were determined by calculating Cohen’s d statistics59, whereby ds ≥ 0.2 indicate small, ds ≥ 0.5 moderate, and ds ≥ 0.8 large effects60.
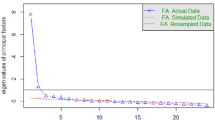
The latent structure of the PCL-5 was investigated within the framework of confirmatory factor analyses (CFA) with robust weighted least square mean and variance (WLSMV) estimator for ordinal variables61. Fit analyses were conducted for the following candidate models: the original four-factor DSM-5 model of PTSD12, the four-factor Dysphoria model27,46, the six-factor Anhedonia model23,62, and the seven-factor Hybrid model47,63,64. Models were defined by mapping items to the respective proposed latent factors, including a common second-order factor to represent PTSD. Item mappings to the respective factors as proposed in these structural models are provided (Table B1 in Appendix). Standardized factors loadings were evaluated with a cutoff of β > 0.50. Model fit was evaluated based on multiple descriptive goodness-of-fit indices, namely the overall chi-square statistic, Comparative Fit Index (CFI), Tucker-Lewis Index (TLI), standardized root mean square residual (SRMR), and root mean square error of approximation (RMSEA) with a 90% confidence interval. Desirable fit was determined for CFI and TLI above 0.95, RMSEA below 0.06, and SRMR less than 0.0865. However, since these cutoff values were not originally proposed for WLSMV estimation of ordinal data, results should be interpreted cautiously66. We therefore evaluated structural validity for the candidate models considering all fit indices simultaneously.
The cross-linguistic equivalence of the PCL-5 assessments was investigated by applying multi-group CFA with a WLSMV estimator for ordinal data based on recommendations by Wu and Estabrook (2016)67 and adapted from Svetina, Rutkowski, and Rutkowski (2020)68. Three nested MI models were set up with increasingly constrained structural parameters: (1) configural model, (2) thresholds model, (3) loadings model. Models were defined by mapping items to the proposed latent factors and including between-factor covariances. Again, model fit was evaluated based on the previously described goodness-of-fit indices (i.e., chi-square, CFI, TLI, SRMR, RMSEA with 90% CI) in conjunction with the respective cutoffs. Likelihood ratio statistics of the relative model fit were examined using scaled chi-square difference tests with the Satorra-Bentler approximation69 and significance levels at α = 0.05. Significant differences would indicate rejection of the null hypothesis of equal model fit. However, since chi-square difference tests may overestimate effects in studies with large samples sizes70, changes in descriptive goodness-of-fit indices were evaluated as well. Based on previous recommendations71,72, between-model non-invariance was assumed for ΔCFI and ΔTLI ≥ 0.010, as well as ΔSRMR and ΔRMSEA ≥ 0.015. Final evaluations of the comparative model fit, and thus MI, were based on all relevant parameters concurrently.
Finally, MI analyses between individuals after ‘ultra-mild’ and more severe TBI were carried out in similar fashion as described above by employing increasingly constrained nested MI models and evaluated based on the same difference tests and model indices alongside the respective cutoffs.
The reported results are based on the ‘CENTER core 2.1’ dataset retrieved from the Neurobot platform of CENTER-TBI: https://center-tbi.incf.org (last accessed on 09.07.2021). All analyses were conducted in R 3.6.373 using the packages ‘psych 2.0.12’74, ‘lavaan 0.6–8’75, and ‘semTools 0.5–4’76. For statistical tests, p < 0.05 was considered significant.
Informed consent
Informed consent was obtained from all subjects involved in the study.
Data availability
All relevant data are available upon request from CENTER-TBI, and the authors are not legally allowed to share it publicly. The authors confirm that they received no special access privileges to the data. CENTER-TBI is committed to data sharing and in particular to responsible further use of the data. Hereto, we have a data sharing statement in place: https://www.center-tbi.eu/data/sharing. The CENTER-TBI Management Committee, in collaboration with the General Assembly, established the Data Sharing policy, and Publication and Authorship Guidelines to assure correct and appropriate use of the data as the dataset is hugely complex and requires help of experts from the Data Curation Team or Bio- Statistical Team for correct use. This means that we encourage researchers to contact the CENTER-TBI team for any research plans and the Data Curation Team for any help in appropriate use of the data, including sharing of scripts. Requests for data access can be submitted online: https://www.center-tbi.eu/data. The complete Manual for data access is also available online: https://www.center-tbi.eu/files/SOP-Manual-DAPR-20181101.pdf.
Abbreviations
- TBI:
-
Traumatic brain injury
- PTSD:
-
Post-traumatic stress disorder
- DSM-5:
-
Diagnostic and statistical manual of mental disorders 5th edition
- PCL-5:
-
Post-traumatic stress disorder checklist for DSM-5
- CFA:
-
Confirmatory factor analysis
- MI:
-
Measurement invariance
- CENTER-TBI:
-
Collaborative European NeuroTrauma Effectiveness Research in TBI project
- ISS:
-
Injury severity score
- GCS:
-
Glasgow coma scale
- GOSE:
-
Glasgow outcome scale-extended
- WLSMV:
-
Weighted least square mean and variance estimator
- CFI:
-
Comparative fit index
- TLI:
-
Tucker-Lewis index
- SRMR:
-
Standardized root mean square residual
- RMSEA:
-
Root mean square error of approximation
- RTA:
-
Road traffic accidents
- ER:
-
Emergency room
- ADM:
-
Admission to ward
- ICU:
-
Intensive care unit
References
Menon, D. K., Schwab, K., Wright, D. W. & Maas, A. I. Position statement: Definition of traumatic brain injury. Arch. Phys. Med. Rehabil. 91, 1637–1640 (2010).
James, S. L. et al. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990–2016: A systematic analysis for the global burden of disease study 2016. Lancet Neurol. 18, 56–87 (2019).
Malec, J. F., Van Houtven, C. H., Tanielian, T., Atizado, A. & Dorn, M. C. Impact of TBI on caregivers of veterans with TBI: Burden and interventions. Brain Inj. 31, 1235–1245 (2017).
van Dijck, J. T. J. M. et al. In-hospital costs after severe traumatic brain injury: A systematic review and quality assessment. PLoS ONE 14, e0216743 (2019).
Majdan, M. et al. Epidemiology of traumatic brain injuries in Europe: A cross-sectional analysis. Lancet Public Health 1, e76–e83 (2016).
Peeters, W. et al. Epidemiology of traumatic brain injury in Europe. Acta Neurochir. (Wien) 157, 1683–1696 (2015).
Maas, A. I. R. et al. Traumatic brain injury: Integrated approaches to improve prevention, clinical care, and research. Lancet Neurol. 16, 987–1048 (2017).
Rogers, J. M. & Read, C. A. Psychiatric comorbidity following traumatic brain injury. Brain Inj. 21, 1321–1333 (2007).
Rabinowitz, A. R. & Levin, H. S. Cognitive sequelae of traumatic brain injury. Psychiatr. Clin. North Am. 37, 1–11 (2014).
Tanev, K. S., Pentel, K. Z., Kredlow, M. A. & Charney, M. E. PTSD and TBI co-morbidity: Scope, clinical presentation and treatment options. Brain Inj. 28, 261–270 (2014).
McMillan, T. M., Williams, W. H. & Bryant, R. Post-traumatic stress disorder and traumatic brain injury: A review of causal mechanisms, assessment, and treatment. Neuropsychol. Rehabil. 13, 149–164 (2003).
Diagnostic and statistical manual of mental disorders: DSM-5. (American Psychiatric Publishing, 2013).
Burri, A. & Maercker, A. Differences in prevalence rates of PTSD in various European countries explained by war exposure, other trauma and cultural value orientation. BMC Res. Notes 7, 407 (2014).
Conroy, S. K., Brownlowe, K. B. & McAllister, T. W. Depression comorbid with stroke, traumatic brain injury, Parkinson’s disease, and multiple sclerosis: Diagnosis and treatment. Focus 18, 150–161 (2020).
Van Praag, D. L. G., Cnossen, M. C., Polinder, S., Wilson, L. & Maas, A. I. R. Post-traumatic stress disorder after civilian traumatic brain injury: A systematic review and meta-analysis of prevalence rates. J. Neurotrauma 36, 3220–3232 (2019).
Hendrickson, R. C., Schindler, A. G. & Pagulayan, K. F. Untangling PTSD and TBI: Challenges and strategies in clinical care and research. Curr. Neurol. Neurosci. Rep. 18, 106 (2018).
Kessler, R. C. Posttraumatic stress disorder: The burden to the individual and to society. J. Clin. Psychiatr. 61, 4–44 (2000).
McGowan, I. The economic burden of PTSD. A brief review of salient literature. Int. J. Psychiatry Ment. Health 1, 20–26 (2019).
Weathers, F., Litz, B., Herman, D., Huska, J. & Keane, T. The PTSD checklist (PCL): Reliability, validity, and diagnostic utility. Annu. Conv. Int. Soc. Trauma. Stress Stud. (1993).
Weathers, F. et al. The PTSD checklist for DSM-5 (PCL-5). Publ. Online (2013).
Schmitt, T. A., Sass, D. A., Chappelle, W. & Thompson, W. Selecting the “Best” factor structure and moving measurement validation forward: An illustration. J. Pers. Assess. 100, 345–362 (2018).
Liu, P. et al. The underlying dimensions of DSM-5 posttraumatic stress disorder symptoms in an epidemiological sample of Chinese earthquake survivors. J. Anxiety Disord. 28, 345–351 (2014).
Blevins, C. A., Weathers, F. W., Davis, M. T., Witte, T. K. & Domino, J. L. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. J. Trauma. Stress 28, 489–498 (2015).
de Lima, E. P. et al. Cross-cultural adaptation of the posttraumatic stress disorder checklist 5 (PCL-5) and life events checklist 5 (LEC-5) for the Brazilian context. Trends Psychiatry Psychother. 38, 207–215 (2016).
Sveen, J., Bondjers, K. & Willebrand, M. Psychometric properties of the PTSD checklist for DSM-5: A pilot study. Eur. J. Psychotraumatol. 7., 30165 (2016).
Boysan, M. et al. Psychometric properties of the Turkish version of the PTSD checklist for diagnostic and statistical manual of mental disorders, fifth edition (PCL-5). Psychiatry Clin. Psychopharmacol. 27, 300–310 (2017).
Krüger-Gottschalk, A. et al. The German version of the posttraumatic stress disorder checklist for DSM-5 (PCL-5): Psychometric properties and diagnostic utility. BMC Psychiatry 17, 379 (2017).
Ibrahim, H., Ertl, V., Catani, C., Ismail, A. A. & Neuner, F. The validity of posttraumatic stress disorder checklist for DSM-5 (PCL-5) as screening instrument with Kurdish and Arab displaced populations living in the Kurdistan region of Iraq. BMC Psychiatry 18, 259 (2018).
Ito, M., Takebayashi, Y., Suzuki, Y. & Horikoshi, M. Posttraumatic stress disorder checklist for DSM-5: Psychometric properties in a Japanese population. J. Affect. Disord. 247, 11–19 (2019).
Martínez-Levy, G. A. et al. After a disaster: Validation of PTSD checklist for DSM-5 and the four- and eight-item abbreviated versions in mental health service users. Psychiatry Res. 305, 114197 (2021).
von Steinbuechel, N. et al. Psychometric characteristics of the patient-reported outcome measures applied in the CENTER-TBI study. J. Clin. Med. 10, 2396 (2021).
Gregorich, S. E. Do self-report instruments allow meaningful comparisons across diverse population groups? Testing measurement invariance using the confirmatory factor analysis framework. Med. Care 44, S78–S94 (2006).
Edwards, M. C., Houts, C. R. & Wirth, R. J. Measurement invariance, the lack thereof, and modeling change. Qual. Life Res. 27, 1735–1743 (2018).
Mansfield, A. J., Williams, J., Hourani, L. L. & Babeu, L. A. Measurement invariance of posttraumatic stress disorder symptoms among U.S. military personnel: Measurement invariance of PTSD Symptoms. J. Trauma. Stress 23, 91–99 (2010).
Ashbaugh, A. R., Houle-Johnson, S., Herbert, C., El-Hage, W. & Brunet, A. Psychometric validation of the English and French versions of the posttraumatic stress disorder checklist for DSM-5 (PCL-5). PLoS ONE 11, e0161645 (2016).
Contractor, A. A., Caldas, S. V., Dolan, M., Lagdon, S. & Armour, C. PTSD’s factor structure and measurement invariance across subgroups with differing count of trauma types. Psychiatry Res. 264, 76–84 (2018).
Eddinger, J. R. & McDevitt-Murphy, M. E. A confirmatory factor analysis of the PTSD checklist 5 in veteran and college student samples. Psychiatry Res. 255, 219–224 (2017).
Maas, A. I. R. et al. Collaborative European NeuroTrauma Effectiveness Research in traumatic brain injury (CENTER-TBI): A prospective longitudinal observational study. Neurosurgery 76, 67–80 (2015).
Yue, J. K. et al. Transforming research and clinical knowledge in traumatic brain injury pilot: Multicenter implementation of the common data elements for traumatic brain injury. J. Neurotrauma 30, 1831–1844 (2013).
Koh, K. & Zumbo, B. Multi-group confirmatory factor analysis for testing measurement Invariance in mixed item format data. J. Mod. Appl. Stat. Methods 7, 12 (2008).
Cao, X., Wang, L., Cao, C., Zhang, J. & Elhai, J. D. DSM-5 posttraumatic stress disorder symptom structure in disaster-exposed adolescents: Stability across gender and relation to behavioral problems. J. Abnorm. Child Psychol. 45, 803–814 (2017).
Galenkamp, H., Stronks, K., Mokkink, L. B. & Derks, E. M. Measurement invariance of the SF-12 among different demographic groups: The HELIUS study. PLoS ONE 13, e0203483 (2018).
González-Blanch, C. et al. Factor structure and measurement invariance across various demographic groups and over time for the PHQ-9 in primary care patients in Spain. PLoS ONE 13, e0193356 (2018).
Martínez-Soto, J., Torres, C. E. C. & de la Chiapas, J. M. R. Invarianza factorial de la escala Perfil de Estados de Ánimo (POMS) en adultos mexicanos. Rev. Psicol. Cienc Comport. Unidad Acad. Cienc. Juríd. Soc. 13, 45–60 (2022).
Van Praag, D. L. G., Fardzadeh, H. E., Covic, A., Maas, A. I. R. & von Steinbüchel, N. Preliminary validation of the Dutch version of the posttraumatic stress disorder checklist for DSM-5 (PCL-5) after traumatic brain injury in a civilian population. PLoS ONE 15, e0231857 (2020).
Biehn, T. L. et al. Underlying dimensions of DSM-5 posttraumatic stress disorder and major depressive disorder symptoms. Psychol. Inj. Law 6, 290–298 (2013).
Caldas, S. V., Contractor, A. A., Koh, S. & Wang, L. Factor structure and multi-group measurement invariance of posttraumatic stress disorder symptoms assessed by the PCL-5. J. Psychopathol. Behav. Assess. 42, 364–376 (2020).
Kline, R. B. Principles and Practice of Structural Equation Modeling 4th edn. (Guilford Publications, 2015).
Teymoori, A. et al. Measurement invariance of assessments of depression (PHQ-9) and anxiety (GAD-7) across sex, strata and linguistic backgrounds in a European-wide sample of patients after traumatic brain injury. J. Affect. Disord. 262, 278–285 (2020).
Thielmann, I. et al. The HEXACO–100 across 16 languages: A large-scale test of measurement invariance. J. Pers. Assess. 102, 714–726 (2020).
Wilson, L. et al. Understanding the relationship between cognitive performance and function in daily life after traumatic brain injury. J. Neurol. Neurosurg. Psychiatry 92, 407–417 (2021).
Steyerberg, E. W. et al. Case-mix, care pathways, and outcomes in patients with traumatic brain injury in CENTER-TBI: A European prospective, multicentre, longitudinal, cohort study. Lancet Neurol. 18, 923–934 (2019).
Copes, W. S. et al. The injury severity score revisited. J. Trauma Inj. Infect. Crit. Care 28, 69–77 (1988).
Gennarelli, T. A. & Wodzin, E. AIS 2005: A contemporary injury scale. Injury 37, 1083–1091 (2006).
Teasdale, G. & Jennett, B. Assessment of coma and impaired consciousness A practical scale. The Lancet 304, 81–84 (1974).
Wilson, J. T. L., Pettigrew, L. E. L. & Teasdale, G. Structured interviews for the Glasgow outcome scale and the extended Glasgow outcome scale: Guidelines for their use. J. Neurotrauma 15, 573–585 (1998).
Stein, M. B. et al. Risk of posttraumatic stress disorder and major depression in civilian patients after mild traumatic brain injury: A TRACK-TBI study. JAMA Psychiatry 76, 249 (2019).
von Steinbuechel, N. et al. Translation and linguistic validation of outcome instruments for traumatic brain injury research and clinical practice: A step-by-step approach within the observational CENTER-TBI study. J. Clin. Med. 10, 2863 (2021).
Lenhard, W. & Lenhard, A. Calculation of effect sizes. Dettelbach (Germany): Psychometric https://www.psychometrica.de/effect_size.html (2021).
Cohen, J. Statistical Power Analysis for the Behavioral Sciences (L. Erlbaum Associates, 1988).
Hancock, G. R. & Mueller, R. O. Structural Equation Modeling: A Second Course 2nd edn. (IAP, 2013).
Shevlin, M., Hyland, P., Karatzias, T., Bisson, J. I. & Roberts, N. P. Examining the disconnect between psychometric models and clinical reality of posttraumatic stress disorder. J. Anxiety Disord. 47, 54–59 (2017).
Armour, C. et al. Dimensional structure of DSM-5 posttraumatic stress symptoms: Support for a hybrid anhedonia and externalizing behaviors model. J. Psychiatr. Res. 61, 106–113 (2015).
Armour, C., Contractor, A., Shea, T., Elhai, J. D. & Pietrzak, R. H. Factor structure of the PTSD checklist for DSM-5: Relationships among symptom clusters, anger, and impulsivity. J. Nerv. Ment. Dis. 204, 108–115 (2016).
Hu, L. & Bentler, P. M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. Multidiscip. J. 6, 1–55 (1999).
Xia, Y. & Yang, Y. RMSEA, CFI, and TLI in structural equation modeling with ordered categorical data: The story they tell depends on the estimation methods. Behav. Res. Methods 51, 409–428 (2019).
Wu, H. & Estabrook, R. Identification of confirmatory factor analysis models of different levels of invariance for ordered categorical outcomes. Psychometrika 81, 1014–1045 (2016).
Svetina, D., Rutkowski, L. & Rutkowski, D. Multiple-group invariance with categorical outcomes using updated guidelines: An illustration using mplus and the lavaan/semtools packages. Struct. Equ. Model. Multidiscip. J. 27, 111–130 (2020).
Satorra, A. & Bentler, P. M. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika 66, 507–514 (2001).
Shi, D., DiStefano, C., McDaniel, H. L. & Jiang, Z. Examining chi-square test statistics under conditions of large model size and ordinal data. Struct. Equ. Model. Multidiscip. J. 25, 924–945 (2018).
Cheung, G. W. & Rensvold, R. B. Evaluating goodness-of-fit indexes for testing measurement invariance. Struct. Equ. Model. Multidiscip. J. 9, 233–255 (2002).
Chen, F. F. Sensitivity of goodness of fit indexes to lack of measurement invariance. Struct. Equ. Model. Multidiscip. J. 14, 464–504 (2007).
The R Foundation. R: The R Project for Statistical Computing. R-project.org. Published online https://www.r-project.org/ (2019).
Revelle, W. psych: Procedures for Personality and Psychological Research (Northwestern University, 2019).
Rosseel, Y. lavaan: An R package for structural equation modeling. J. Stat. Softw. 48, 1–36 (2012).
Jorgensen, T. D., Pornprasertmanit, S., Schoemann, A. M. & Rosseel, Y. semTools: Useful tools for structural equation modeling. (2021).
Acknowledgements
We gratefully thank all CENTER-TBI participants and investigators. We are immensely grateful to our patients with TBI for helping us in our efforts to improve care and outcome for TBI. The full list of the CENTER-TBI participants and investigators is provided in the Online Supplement.
Funding
Open Access funding enabled and organized by Projekt DEAL. CENTER-TBI was supported by the European Union 7th Framework programme (EC Grant 602150). Additional funding was obtained from the Hannelore Kohl Stiftung (Germany), from OneMind (USA), and from Integra LifeSciences Corporation (USA). The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Author information
Authors and Affiliations
Consortia
Contributions
Conceptualization: F.B., M.Z., K.C., and N.vS.; methodology: F.B., M.Z., K.C., and N.vS.; software: F.B.; validation: F.B., and M.Z.; formal analysis: F.B.; resources: N.vS.; data curation: F.B., and M.Z.; writing—original draft preparation: F.B.; writing—review and editing: F.B., M.Z., K.C., D.V.P., M.V., T.B., Y.H., and N.vS.; visualization: F.B.; supervision: N.vS., T.B., and Y.H.; project administration: N.vS.; funding acquisition: N.vS. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bockhop, F., Zeldovich, M., Cunitz, K. et al. Measurement invariance of six language versions of the post-traumatic stress disorder checklist for DSM-5 in civilians after traumatic brain injury. Sci Rep 12, 16571 (2022). https://doi.org/10.1038/s41598-022-20170-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-20170-2
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.