Abstract
The determination of length of time from the last drinking is critical for cases like drunk driving, sexual assault victims, and also postmortem suspected poisoning cases. The study was aimed to established a method of estimating the time of last drinking through the pharmacokinetic study of conjugation metabolites of alcohol in blood after a single oral dose. Twenty-six volunteers (14 males) consumed alcohol with food at a fixed dose of 0.72 g/kg after fasting for 12 h. Five milliliters of blood were collected 120 h after the start of drinking, and all samples were analyzed with headspace-gas chromatography and high-performance liquid chromatography–tandem mass spectrometry. The time point of last drinking was estimated through the relationship between the concentration ratio of ethyl glucuronide to ethyl sulphate and the length of time after drinking. Pharmacokinetic parameters were analyzed by a pharmacokinetic software DAS according to the non-compartment model. A good correlation model was obtained from the relationship between concentration ratio of ethyl glucuronide to ethyl sulphate in blood and the time of alcohol use, and the margin of error was mostly lower than 10%. The time of maximum concentration, maximum concentration, and elimination half-life of ethyl glucuronide in blood were 4.12 ± 1.07 h, 0.31 ± 0.11 mg/L and 2.56 ± 0.89 h; the time of maximum concentration, maximum concentration, and elimination half-life of ethyl sulphate in blood were 3.02 ± 0.70 h, 0.17 ± 0.04 mg/L, and 2.04 ± 0.76 h. The study established a potential method to estimate the length of time after a moderate oral dose, and provided pharmacokinetic parameters of ethyl glucuronide and ethyl sulphate in Chinese population.
Similar content being viewed by others
Introduction
As a psychoactive substance with dependence-producing properties, alcohol has been one of the most widely abused drugs in the world. Due to the high prevalence of alcohol use in the general population, the number of alcohol-related accidents is increasing worldwide on the road, at work, and during acts of violence1, and the traffic accidents are the most common cases2. In most cases, however, we can no longer detect alcohol 6–8 h after drinking because of its rapid metabolism3, which makes it more complex to confirm drunk driving in a suspected hit-and-run accident4.
Alcohol is metabolized mainly through liver, and oxidized by alcohol dehydrogenases and aldehyde dehydrogenases eventually to acetyl CoA. Besides, there are other non-oxidative pathways of alcohol metabolism, such as conjugation reactions and fatty acyl synthases5. Ethyl glucuronide (EtG) and ethyl sulphate (EtS) are two major non-oxidative metabolites of alcohol produced by glucuronidation and sulfonation of alcohol. A very small amount (less than 1%) of the ethanol dose consumed is excreted in the urine as EtG and EtS6, which can be detected in many body fluids and tissues for an extended time after alcohol is eliminated from the body7. Therefore, EtG and EtS are expected to be sensitive and specific biomarkers for alcohol intake8,9,10.
The determination of recent alcohol use is critical for forensic purposes to evaluate cases such as drunk driving, sexual assault victims, and also postmortem suspected poisoning cases. The length of time from the last drinking is an important clue in some cases because it determines the nature of the case to some extent. Some methods have been reported to predict the time of last drinking10,11, and the concentration ratios of parent to its metabolites or the ratios of different metabolites were adopted in time estimation12,13, since the calculation of ratios can counteract the influence of dosage. However, the alcohol concentration is usually detectable within 8 h after ingestion, and considered accurate when measured within 24 h after death and at a temperature lower than 20 °C14. Therefore, we must be careful with the application of alcohol concentration in the analysis of cases, and a more reliable method is needed to estimate the time of last drinking. As the non-oxidative metabolites of alcohol, EtG and EtS have not only been reported higher concentrations and longer detection windows, which enable the retrospective assessment of alcohol intake even when alcohol itself was no longer present in the body15,16, but have been proved that they can not be produced after death9,14, and are stable at low temperature17. Consequently, the concentration ratio of EtG to EtS can be considered to estimate the time of last drinking.
The study aimed to established a method of estimating the time of last drinking through the pharmacokinetic study of EtG and EtS. Blood is the most commonly used matrix in alcohol-related cases. Compared with urine, analyte concentration in blood is rarely affected by the amount of water consumed, and its collection can not be easy to fake as well. Therefore, in this study, we investigated the pharmacokinetics of EtG and EtS in blood of 26 volunteers following a single dose of 0.72 g alcohol/kg to estimate the time of last drinking.
Pharmacokinetics of alcohol and its metabolites, especially the conjugation metabolites, are useful for the detection of alcohol consumption or relapse of alcoholics. Although that EtG and EtS have been reported longer detection windows, few studies about the pharmacokinetic parameters have been calculated9,18. The study is not only expected to establish a method of estimating the length of time after drinking, but also can provide pharmacokinetic parameters of EtG and EtS in Chinese population after a moderate oral dose.
Materials and methods
Chemicals and reagents
Alcohol (10 mg/mL) was obtained from AccuStandard, USA. Tertiary butanol (AR, ≥ 99.0%) was obtained from Aladdin, Shanghai. EtG (100 mg/mL) and two internal standards (IS, EtG-D5 1 mg/mL and EtS-D5 1 mg/mL) were obtained from Cerilliant, USA; EtS-Na (98%) was purchased from TSI, Japan. Methanol (HPLC grade) and acetonitrile (HPLC grade) were from Merke, USA; formic acid (LC/MS grade) was from J&K Chemical, China; ultrapure water was obtained from a water purification system (Milli-Q Academic, USA).
Participants and study design
A total of 26 adults, including 14 males and 12 females without histories of somatic or psychiatric illness, drinking, or medication use, participated in the study and provided informed consent to the Committee of Medical Ethics of Shanxi Medical University (2018LL349). Their median age is 24.5 years (ranging from 22 to 27) and the average body mass index is 20.9 kg/m2 (ranging from 16.8 to 34.6). All participants resided in a secure clinical research unit for at least 24 h afterward, and they were medically evaluated during alcohol administration and 3 days later for the sake of safety. All participants got paid for their time and efforts.
After 12 h of fasting, the participants received Fenjiu, a local liquor containing 40% alcohol, proportionately to their weight (0.72 g/kg) accompanied by food within 30 min. Five millilitres of blood were drawn each time from an indwelling venous catheter in the arm before drinking and at the time points of 0.5, 1.5, 2, 3, 5, 8, 12, 24, 36, 48, 120 h after the start of drinking, respectively. All samples were stored at − 20 °C until analysis.
Sample preparation
Alcohol
The preparation and detection methods were performed according to those used in our preliminary research19, and alcohol concentration was determined via the internal standard method using headspace-gas chromatography, with which tertiary butanol was the internal standard.
Briefly, 1 mL blood and 1 mL tertiary butanol (IS, 87 mg/mL) were added in a headspace bottle, next, the mixture was sealed after being diluted with 3 mL ultrapure water and then analyzed with headspace-gas chromatography.
EtG and EtS
Two internal standards (EtG-D5 and EtS-D5, 1 µg/mL, 100 µL) were added to 100 µL of blood to improve the identification and quantification of the metabolites, EtG and EtS. Proteins were precipitated with 800 µL of 80% acetonitrile in methanol for 10 min at 0 °C. After centrifugation (13,000 rpm, 5 min), the supernatant was removed and dried at 35 °C with nitrogen. The residues were redissolved with 400 µL of 5% acetonitrile in water, and centrifuged again at 13,000 rpm for 5 min. From the newly prepared solution, 3 µL was taken and injected into Liquid Chromatography tandem mass spectrometry (LC–MS/MS) for analysis.
LC–MS/MS analysis
Chromatographic separation was performed with an Inertsil ODS-3 column (2.1 × 100 mm, 3 µm) through a LC-20A system (Shimadzu, Japan). The mobile phase was a mixture of solvent A (0.1% formic acid in ultrapure water) and solvent B (0.1% formic acid in acetonitrile). The chromatographic column was held at 35 °C and eluted for 14.0 min in total at a flow rate of 0.2 mL/min with a gradient of 5% B (0–2.0 min), 90% B (2.0–6.0 min), 90% B (6.0–8.0 min), 5% (8.0–8.5 min), and 5% (8.5–14.0 min), respectively. Mass spectrometry was performed on a mass spectrometer (TRAP 4000, Sciex, AB). All analytes were ionized by electrospray in negative mode, and tandem MS analysis was performed in multiple reaction monitoring (MRM) mode. The ionspray voltage was − 4000 V, and the temperature was 500 °C. The curtain gas, Gas1, and Gas2 were 40 psi, 50 psi, and 35 psi, respectively. Other specific MRM parameters for each analyte are shown as follows in Table 1.
Estimation of the time of last drinking
The current study used the relationship between concentration ratios of EtG to EtS in blood and time to estimate the time of last drinking, and the errors between observed and actual time of last drinking were calculated with (|observed value − actual value|/actual value) × 100%.
Statistics
The pharmacokinetics parameters were calculated with the software of DAS 3.0 according to the non-compartmental method. All data were summarized with descriptive statistics. Arithmetic means and standard deviations of key data (concentrations and detection time points) and pharmacokinetic parameters were provided. All statistical analyses were performed with version 13.0 of IBM SPSS® Software (SPSS Inc., Chicago, IL, USA).
Ethics approval
All experiments were performed in accordance with the current China legislation and approved by the Committee of Medical Ethics of Shanxi Medical University (2018LL349).
Informed consent
All subjects provided written informed consent prior to screening.
Results
Method validation
All analytes including alcohol, EtG, EtS, EtG-D5 and EtS-D5 were well separated, no endogenous peak was observed to be coeluted with analytes, and the methods were fully validated as shown in Tables 2 and 3. The limit of detection (LOD) and limit of quantitation (LOQ) of EtG and EtS in blood were 0.02 µg/mL and 0.05 µg/mL, respectively. We redissolved the residues with 100 µL of 5% acetonitrile in water to quantitate the concentrations below the LOQ.
Estimation of the time of last drinking
Based on the mean concentrations of EtG and EtS in blood showed in Table 4, we calculated the mean concentration ratios of EtG to EtS, and analyzed the relationships between the ratios and last usage after single oral dose. It was found that the interval time only correlated well using binomial function (y = 1.646x2 − 0.9599x + 0.0878, x represented ratio, y represented time, R2 = 0.9904), and the errors between observed and actual values [(|observed value − actual value|/actual value) × 100%] were mostly lower than 10% within 8 h, as shown in Table 7.
Pharmacokinetic analysis
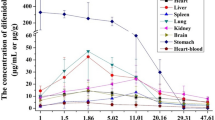
Data on concentrations at each time point and detection limits of alcohol and EtG, EtS are shown in Tables 4 and 5. It was showed that after the volunteers’ consumption of 0.72 g alcohol/kg, alcohol concentration reached the highest level of 0.41 ± 0.11 mg/mL at 1.5 h and then declined gradually, and the detection window time was 3–8 h. The peak blood levels (maximum observed value) of EtG (0.29 ± 0.12 µg/mL) and EtS (0.16 ± 0.04 µg/mL) were observed at 5 h and 3 h, respectively, and the detection window were 8–12 h and 5–12 h. Additionally, as shown in Fig. 1, it was found that the concentrations of EtG were always higher than those of EtS through the process of study.
Based on the non-compartment model, the pharmacokinetic parameters of alcohol and EtG, EtS after oral administration of 0.72 g alcohol/kg were calculated and are shown in Table 6. It was found that alcohol could reach its peak concentration in blood (441.65 ± 113.86 mg/L (0.44 ± 0.11 mg/mL)) at 2.02 ± 0.54 h, and the metabolites, EtG and EtS reached their peak concentrations (obtained from the pharmacokinetic model) (0.31 ± 0.11 mg/L and 0.17 ± 0.04 mg/L) at 4.12 ± 1.07 h and 3.02 ± 0.70 h, respectively. The t1/2z of alcohol and EtG, EtS were 1.24 ± 1.09 h and 2.56 ± 0.89 h, 2.04 ± 0.76 h, respectively. The CLz/F of alcohol was 0.49 ± 0.33 L/h; however, CLz/F of the metabolites of alcohol (EtG and EtS) could not been calculated accurately because their initial dose was different to estimate.
Discussion
The analytical method developed in this study has proved to be sensitive and accurate for the analysis of EtG and EtS. The lower LOD (0.02 µg/mL) and LOQ (0.05 µg/mL) achieved are particularly useful for quantifying the lower concentrations of EtG and EtS present in blood during pharmacokinetic investigation of EtG and EtS. Also, it is illegal in China to drive with a blood alcohol concentration (BAC) higher than 0.2 mg/mL, and Cmax of BAC (0.22–0.66 mg/mL) at 0.72 g/kg dose of alcohol used in the study is close to that, suggesting that the method might be suitable for monitoring most cases of drunk driving in China.
This study has focused on the concentration–time-curves of alcohol, EtG and EtS in blood of 26 volunteers following a single dose of 0.72 g alcohol/kg, and aimed to establish a method of estimating the time of last drinking. It was found that the time of post-alcohol use could be estimated using the relative concentrations of EtG and EtS. In the preciously studies, Zhao et al.10 once proposed predicting the time of last drinking using the serum concentration ratio of alcohol to EtG. While alcohol is usually metabolized quickly in living body, and the alcohol concentration after death is subject to change due to postmortem redistribution20 and postmortem production21. Therefore, the application of concentration ratios of alcohol to metabolites has great limitations, and as reported in the literature, our study also showed a poor correlation between the concentration ratio of alcohol to its metabolites and time of last drinking. While, despite great individual differences, a good correlation model was obtained from the mean concentration ratio of EtG to EtS in blood and the time of alcohol use, and most of the prediction errors were less than 10%. This would be useful in forensic investigation such as in the case of driving under the influence of alcohol.
Pharmacokinetic parameters of alcohol and EtG, EtS in blood were calculated based on the non-compartment model. For alcohol, the study found that it reached the Cmax of 441.65 ± 113.86 mg/L (0.44 ± 0.11 mg/mL) at 2.02 ± 0.54 h, and compared with the previous studies11, it showed a longer absorption phase. In addition, we found that alcohol in blood of the participants could be detected within 8 h (3–8 h), and the mean elimination half-life of alcohol was 1.24 ± 1.09 h (0.30–4.23 h), with individual differences. For EtG and EtS, in view of their longer detection window, we investigated the concentrations of analytes in blood up to 120 h after drinking, and it was the first time that pharmacokinetics of EtG and EtS in blood were evaluated in a larger number of Chinese population. Compared with EtS, EtG was discovered early and has been most studied10,22,23,24. It was reported that the detection windows of EtG in both serum and urine were longer than those of alcohol25,26,27, and we confirmed that EtG did metabolize slower than alcohol, and the elimination half-life of EtG in blood was 2.56 ± 0.89 h. Additionally, the detection time limit for urinary EtG was reported to depend weakly on the breath ethanol concentrations27, and our study showed no correlation between initial alcohol concentrations and detection limits of EtG, based on the CORREL function, suggesting that the lower alcohol consumption might not affect the detection limit of EtG. EtS was another non-oxidative metabolite of alcohol, and its concentration–time curve was found similar to that of EtG8,18. Georg Schmitt et al.18 once reported that the Cmax of EtS ranged from 0.09 µg/mL to 0.72 µg/mL at 0.52 ± 0.17 g/kg dosage of alcohol, and the Tmax was about 2.94 h, while in our study, the Cmax of EtS was 0.17 µg/mL (ranging from 0.08 µg/mL to 0.28 µg/mL) at 0.72 g/kg dosage, and the Tmax was 3.02 h, indicating interethnic differences. In addition, our study found that both the detection window and Cmax of EtS were lower than those of EtG. However, EtS has been reported to be stable and not susceptible to bacteria28,29, suggesting that EtS could provide complementary data in the identification of alcohol ingestion.
Alcohol metabolism is influenced by many factors including the amount of alcohol consumption, age, gender, race, and genetic variability30, among which genetic difference between individuals has been considered a major contributor to the pharmacokinetic variation of alcohol. Gudrun31 and Lostia32 reported that the concentrations of alcohol, EtG, and EtS would increase as the dosage of alcohol intake increases, and differ in individuals with the same dosage of alcohol. A homogenous sample was obtained in our study, since the 26 Chinese Han people recruited were young and healthy, and all of them were free from somatic or psychiatric illness, alcohol drinking, and regular medication. Although effects of these parameters can not be ruled out, the results obtained in this study do suggest the association of the diversified pharmacokinetics of alcohol in Chinese population with genetic difference between individuals. To further elucidate the mechanism underlying the observed differences, we need to investigate the metabolic enzymes phenotyping of the 26 Chinese participants in future studies.
Race is another important element affecting the result of alcohol pharmacokinetics. Alcohol dehydrogenase 2 (ADH2), aldehyde dehydrogenase 2 (ALDH2) and CYP2E1 are three major ethanol-metabolizing enzymes. It was reported that the allele frequencies in Chinese populations (76.7%, 15.6%, and 28.9% respectively) were obsevably higher than those in European groups (0%, 0%, and 5.1% respectively)33, and a strongly protective variant in ALDH2 is essentially only found in Asians34. Uridine diphosphate-glucuronosyltransferases (UGT) and sulfotransferases (SULT) are two enzymes responsible for EtG and EtS formation. It was reported that genes coding for these enzymes have considerable polymorphism35, while few studies reported the interethnic difference of the allele frequencies of UGT and SULT. Apart from the dosage, here results showed a possible influence of race on the formation of EtG and EtS. Further studies on the influence of race on the glucuronidation and sulfonation of alcohol should be considered in the next studies.
Factors affecting the metabolism of alcohol might affect the ratio of EtG/EtS, and then affect the outcome of time estimation. In this study, we estimated the drinking time of volunteers based on the individual value of EtG/EtS at each time point (data was not showed here), and it was found that there was still great individual difference, especially for the application of extreme values like min and max EtG/EtS. Generally, the calculation of ratios can counteract the influence of dosage, but this is not the case when the dosage is too large, which is due to the report that sulphation is more saturable than glucuronidation at higher concentrations of substrate. And our study also showed an influence of dosage on the time estimation, especially when the metabolic ability was also relatively poor or strong. As shown in Table 7, the min values of observed time were obtained from a volunteer with the lowest dosage of alcohol due to his lighter weight, at the same time, the volunteer had not only a poor ability of alcohol metabolism (tmax = 3 h), but a lower level of EtG (Cmax = 0.18 μg/mL) and higher level of EtS (Cmax = 0.20 μg/mL). Conversely, this was also true for the max values of observed time. Here the estimated model to calculate the period of time after drinking was only based on a unique dosage of 0.72 g/kg, and the facts affecting the metabolism of alcohol, such as genotypes of metabolic enzyme, were also not considered, therefore, further studies on the influence of these factors affecting alcohol metabolism on the time estimation could also be needed.
Additionally, cumulative effects caused by drinking cumulatively can also affect the calculation of last drinking. Here we simulated the drinking pattern at a normal meal of Chinese, namely, all volunteers were required to finish drinking within half an hour. In fact, drinking back and forth for more than half an hour is a rather normative drinking situation for most recreational alcohol drinkers. In this condition, there should be a cumulative addition of EtG and EtS concentrations in blood originating from these different drinking periods, and it is not possible to use the proposed model. Therefore, more studies on the impact of this for the calculation of last drinking should be also done in the next step.
In summary, the current study established a method of estimating the time of last drinking using the relationship between concentration ratio of EtG to EtS in blood and the time of alcohol use, and once further validated, this novel discovery will provide a useful analytical tool for monitoring alcohol use by Chinese motorists on the road. Additionally, we investigated the pharmacokinetics of alcohol and EtG, EtS in blood of Chinese population, and obtained the pharmacokinetic parameters of the targets. The sensitive LC–MS/MS approach developed and validated in the study can be applied in drink driving and other forensic cases when alcohol is involved, and the long detection windows of EtG and EtS support their use as useful markers for the detection of alcohol consumption.
Data availability
All data generated during the study appear in the submitted article.
References
Goullé, J. P. & Guerbet, M. Éthanol: Pharmacocinétique, métabolisme et méthodes analytiques. Ann. Pharm. Fr. 73, 313–322 (2015).
Abramovici, F. Medicine and driving: Alcohol and other toxins. Presse Med. 44, 1048–1054 (2015).
Zhuo, X. et al. Study on the elimination rate of blood alcohol and estimation of blood alcohol concentration. Chin. J. Forensic Sci. 01, 23–26 (2003).
Mei, B. et al. Research on the problems related to human alcohol content detection in traffic law enforcement. J. Transp. Eng. 04, 52–55 (2007).
Cederbaum, A. I. Alcohol metabolism. Clin. Liver Dis. 16, 667–685 (2012).
Walsham, N. E. & Sherwood, R. A. Ethyl glucuronide and ethyl sulfate. Adv. Clin. Chem. 67, 47–71 (2014).
Kummer, N., Lambert, W. E., Samyn, N. & Stove, C. P. Alternative sampling strategies for the assessment of alcohol intake of living persons. Clin. Biochem. 49, 1078–1091 (2016).
Dresen, S., Weinmann, W. & Wurst, F. M. Forensic confirmatory analysis of ethyl sulfate—A new marker for alcohol consumption—By liquid-chromatography/electrospray ionization/tandem mass spectrometry. J. Am. Soc. Mass Spectrom. 15, 1644–1648 (2004).
Høiseth, G. et al. A pharmacokinetic study of ethyl glucuronide in blood and urine: Applications to forensic toxicology. Forensic Sci. Int. 172, 119–124 (2007).
Zhao, H., Zhuo, X. & Shen, B. Detection and application of ethyl glucuronide in forensic toxicology. J. Forensic Med. 25, 63–67 (2009).
Lai, J. & Hu, B. Study of alcohol pharmacokinetics in human body. Chin. J. Forensic Med. 01, 1–5 (1996).
Wang, L. et al. Study on the pharmacokinetics of diazepam and its metabolites in blood of Chinese people. Eur. J. Drug Metab. Pharmacokinet. 45, 477–485 (2020).
Huestis, M. A. Estimating the time of last cannabis use from plasma 9-tetrahydrocannabinol and 11-nor-9-carboxy-9-tetrahydrocannabinol concentrations. Clin. Chem. 51, 2289–2295 (2005).
Liu, L. Forensic Toxicology (People’s Medical Publishing House, 2009).
Woźniak, M. K., Wiergowski, M., Namieśnik, J. & Biziuk, M. Biomarkers of alcohol consumption in body fluids—Possibilities and limitations of application in toxicological analysis. Curr. Med. Chem. 26, 177–196 (2019).
Heier, C., Xie, H. & Zimmermann, R. Nonoxidative ethanol metabolism in humans-from biomarkers to bioactive lipids. IUBMB Life 68, 916–923 (2016).
Liu, Y. et al. Stability of ethyl glucuronide, ethyl sulfate, phosphatidylethanols and fatty acid ethyl esters in postmortem human blood. J. Anal. Toxicol. 42, 346–352 (2018).
Schmitt, G., Halter, C. C., Aderjan, R., Auwaerter, V. & Weinmann, W. Computer assisted modeling of ethyl sulfate pharmacokinetics. Forensic Sci. Int. 194, 34–38 (2010).
Liu, X. et al. Study on self-generation alcohol in preserved dog corpses. Chin. J. Forensic Sci. 01, 26–29 (2010).
Yun, K. Postmortem redistribution of forensic toxicants. In The 3th Congress of Toxicants and Drugs Analysis, 300.
Maria, J. Q. et al. Postmortem in vitro ethanol production—It could be more common than we think. Forensic Sci Int. 274, 113–116 (2017).
Wurst, F. M. et al. On sensitivity, specificity, and the influence of various parameters on ethyl glucuronide levels in urine—Results from the WHO/ISBRA Study. Alcohol. Clin. Exp. Res. 28, 1220–1228 (2006).
Sarkola, T. Urinary ethyl glucuronide and 5-hydroxytryptophol levels during repeated ethanol ingestion in healthy human subjects. Alcohol Alcohol. 38, 347–351 (2003).
Nishikawa, M. et al. Determination of ethyl glucuronide, a minor metabolite of ethanol, in human serum by liquid chromatography-electrospray ionization mass spectrometry. J. Chromatogr. B Biomed. Sci. Appl. 726, 105–110 (1999).
Janda, I. & Alt, A. Improvement of ethyl glucuronide determination in human urine and serum samples by solid-phase extraction. J. Chromatogr. B Biomed. Sci. Appl. 758, 229–234 (2001).
Wurst, F. M., Vogel, R., Jachau, K., Varga, A. & Skipper, G. E. Ethyl glucuronide discloses recent covert alcohol use not detected by standard testing in forensic psychiatric inpatients. Alcohol. Clin. Exp. Res. 27, 471–476 (2003).
Helander, A., Bottcher, M., Fehr, C., Dahmen, N. & Beck, O. Detection times for urinary ethyl glucuronide and ethyl sulfate in heavy drinkers during alcohol detoxification. Alcohol Alcohol. 44, 55–61 (2008).
Baranowski, S. et al. In vitro study of bacterial degradation of ethyl glucuronide and ethyl sulphate. Int. J. Legal Med. 122, 389–393 (2008).
Helander, A. & Dahl, H. Urinary tract infection: A risk factor for false-negative urinary ethyl glucuronide but not ethyl sulfate in the detection of recent alcohol consumption. Clin. Chem. 51, 1728–1730 (2005).
Yun, K. The introduction of forensic toxicokinetics. Chin. J. Forensic Med. 6, 361–365 (2008).
Gudrun, H. et al. Ethyl glucuronide concentrations in oral fluid, blood, and urine after volunteers drank 0.5 and 1.0 g/kg doses of ethanol. J. Anal. Toxicol. 34, 319–324 (2010).
Maria, L. A., Lobo, V. J. & Cowan, D. A. Measurement of ethyl glucuronide, ethyl sulphate and their ratio in the urine and serum of healthy volunteers after two doses of alcohol. Alcohol Alcohol. 48, 74–82 (2012).
Kang, T. S., Woo, S. W., Park, H. J., Lee, Y. & Roh, J. Comparison of genetic polymorphisms of CYP2E1, ADH2, and ALDH2 genes involved in alcohol metabolism in Koreans and four other ethnic groups. J. Clin. Pharm. Ther. 34, 225–230 (2009).
Edenberg, H. J. & McClintick, J. N. Alcohol dehydrogenases, aldehyde dehydrogenases, and alcohol use disorders: A critical review. Alcohol Clin. Exp. Res. 42, 2281–2297 (2018).
Lostia, A. M., Vicente, J. L. & Cowan, D. A. Measurement of ethyl glucuronide, ethyl sulphate and their ratio in the urine and serum of healthy volunteers after two doses of alcohol. Alcohol Alcohol. 48, 74–82 (2013).
Acknowledgements
The authors thank Dr. Li for her help in language editing. This work was supported by funding from National Science and Technology Special Project Work (2015FY111400) and National Key R&D Project (2017YEC0803504, 2018YFC0 807403).
Author information
Authors and Affiliations
Contributions
D.Z., Z.W., W.Z., K.Y. and Z.G. designed the research; W.Z., R.W. and Y.G. performed most of the experiments and conducted the studies; L.W., M.H. and C.Z. prepared the manuscript and edited the paper. All authors read and approved the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, L., Zhang, W., Wang, R. et al. Estimating the time of last drinking from blood ethyl glucuronide and ethyl sulphate concentrations. Sci Rep 12, 14262 (2022). https://doi.org/10.1038/s41598-022-18527-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-18527-8
This article is cited by
-
The metabolic clock of ketamine abuse in rats by a machine learning model
Scientific Reports (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.