Abstract
We determined how the in vivo mobility of the first tarsometatarsal (TMT) joint can be quantified during gait. Twenty-five healthy participants (12 females) with no history of foot disorders were included. Non-invasive ultrasound (US) with a three-dimensional motion analysis (MA) system was used to evaluate the kinematic characteristics of first TMT joint during stance phase of gait. US probe was positioned longitudinally above the first TMT joint and adjusted to its proximal dorsal prominence. Gait analysis was conducted by the MA system starting with the activation of B-mode US video at 80 frames per second and 60-mm depth for simultaneous capture. During stance phase, the first metatarsal was translated dorsally with respect to the medial cuneiform, returning to a neutral level at toe-off in all subjects. During middle stance phase, the medial cuneiform was stable in males but displaced in the plantar direction in females and was the primary contributor to the differences in sagittal mobility observed between groups. Quantitatively measuring sagittal mobility of the first TMT joint could be useful for the early detection of foot abnormalities. The dynamic characteristics of the medial cuneiform during gait in healthy females may be associated with a high prevalence of hallux valgus.
Similar content being viewed by others
Introduction
Hallux valgus (HV) is a common foot deformity, with a prevalence of 23% in adults aged 18–65 years and 35.7% in adults aged > 65 years1. Several intrinsic factors are associated with the pathogenesis of HV, including female sex, age, metatarsal morphology, and first-ray hypermobility2. Hypermobility between the first metatarsal and medial cuneiform is one cause of HV, due to the laxity of the Lisfranc joint ligament and decreased plantar arch height3. Studies have reported that instability of the first TMT joint was identified in 94%–96% of patients with HV4,5. Hypermobility of the first TMT joint is correlated with the severity of HV and is compounded by repetitive downward movements of the metatarsals during weight bearing6,7. Biomechanically, excessive first metatarsal extension during the stance phase of gait leads to ligamentous laxity in the metatarsals and subtalar joints, reducing foot stiffness during the terminal stance and adversely affecting push-off mechanics6.
However, the hypermobility of isolated sagittal planes of the first TMT joint has not yet been shown as a definitive cause of HV8.
The mobility of the first ray and TMT joint in sagittal plane has been evaluated using several methods, such as manual examination9, a metal ruler10, a modified ankle–foot-orthosis with an adjustable micrometer11, lateral weight-bearing radiographs12, and three-dimensional computed tomography images with weight-bearing13. The accuracy of the manual test for the assessment of first-ray mobility is controversial, as the subjective results of the manual test are not quantifiable14. A few studies have reported the mobility of the first TMT joint using original devices4,10. However, their quantitative evaluations were limited, as the measurements were obtained manually with the feet immobilized, yielding only static observations. The average standard value of the first TMT joint mobility is 3.6–4.7 mm; however, these values are based on static measurements10. The mobility of the first TMT joint has been evaluated in several cadaveric studies15. In the study of Coughlin MJ et al., the first TMT joint was simulated in three-dimensional space; however, ligaments and other soft tissues were different from those in vivo, possibly affecting joint mobility. The in vivo dynamic gait assessment was performed using a digital fluoroscopic-based method for the rotational and translational movements of the first metatarsal, medial cuneiform, navicular, and talus during the stance phase of gait16. Particularly concerning are the patient’s radiation exposure and unclear images due to a frequency of 25 frames per second. Additionally, the angle of the first TMT joint during gait was evaluated using a three-dimensional MA system17; however, detailed observations for joint movements of the foot are limited. Thus, in vivo quantitative evaluation of the first TMT joint during gait has been challenging previously.
This study aimed to establish a method to quantitatively evaluate the mobility of the first TMT joint in vivo during the stance phase. A novel combination of ultrasound (US) imaging and a three-dimensional MA system was applied to assess first TMT joint mobility during gait in healthy participants. Further, HV is more prevalent in females, due to the differences in bone structure, joint laxity, and their habit of wearing tight-fitting shoes2,18. Therefore, we investigated the differences in the first TMT joint mobility between females and males. We hypothesize that the mobilities of the first metatarsal and medial cuneiform during the stance phase are greater in females than in males.
Methods
Participants
Participants were 25 healthy, recreationally active individuals, including 12 females and 13 males. Recreationally active was defined as having participated in at least one exercise session weekly—but not performing structured exercise training—during the preceding 2 months. Participants were included if they had a foot posture index (FPI-6) score < 6 points, and a score ≥ 6 was used to exclude individuals due to pes planus alignment19. Participants with foot and ankle problems such as ligament injuries; plantar fasciitis; bursitis; a history of lower extremity trauma; or neurological conditions affecting balance were also excluded.
Foot deformities were evaluated using photographs of the participant’s leg (front side) from the knees to feet. The angle between the medial aspect of the hallux and the first metatarsal (HV angle) was measured using these images (Fig. 1)20.
This study was approved by the Ethical Committee for Epidemiology of Hiroshima University (Approval Number: E-2187) and conducted following the principles of the Declaration of Helsinki. All participants provided informed consent.
Experimental procedure
Assessment of first TMT joint mobility using B-mode US during gait
We used a B-mode US system (Art Us EXT-1H, Telemed, Vilnius, Lithuania) and a US probe (5–11 MHz, 60-mm field of view; Echoblaster, Telemed, Vilnius, Lithuania)21 to evaluate the joint motion of the first TMT joint in the sagittal plane during stance phase. The MA system was synchronized with a US system that captured B-mode US video at 80 frames/s and 60 mm depth22. To start and stop simultaneous captures, changes in the electrical signal edges produced by the activation/deactivation of the US switch were recognized by the MA system. Captured data samples within both systems were then put in relation according to their predefined frame rates. The US probe settings are shown in Fig. 2. The US videos were visually inspected for each gait test to ensure that the landmarks of the first metatarsal and medial cuneiform did not disappear. If the video was unclear or the probe misaligned, the measurement was performed again. To standardize the placement position of the probe, we marked each participant’s skin and checked for any deviations. Three US video trials were measured for each side.
Gait analysis using ultrasound and a three-dimensional motion analysis system. Ultrasound probe was attached at the tarsometatarsal joint on an ultrasound gel pad (a), and the first metatarsal and medial cuneiform were within the field of view (b). The vertical locations of the first metatarsal and medial cuneiform were defined as the vertical distance from the screen top to the dorsum of each bone.
Gait analysis
Each participant walked 6 m over eight force plates (OR-6, 1000 Hz: AMTI, USA). Gait was analyzed using the Vicon motion capture analysis system with 16 infrared cameras (100 Hz)23. Sixteen reflective markers were placed on the lower body of the participants, and the markers were applied by the same examiner. After acquiring the data in the static standing position, participants walked over the force plates at their natural speed; two practice trials were conducted before measurements were obtained. Data captions took an average of 3 s for all participants. The participants took two steps before walking on the force plates.
Data analysis
The first of the force plate data were processed using the Plug-in-Gait pipeline for Vicon Nexus ver. 1.8.5 software (Vicon Motion Systems, UK) to detect the gait phase. The phase from heel contact to toe-off of the foot attached to the US probe was defined as one stance phase. One stance phase was calculated for all three trials on each side. Tracker 5.1.5 software (Open Source Physics, https://www.compadre.org) was used to calculate the vertical translation of the metatarsal and medial cuneiform in the US video24. Temporal changes in the vertical location of the first TMT joint during one stance phase obtained from the Vicon software were calculated. Vertical locations of the first metatarsal and medial cuneiform were defined as the shortest distance from the top of the video screen to the top of each bone (Fig. 2b); their locations were calculated for all frames. The gap in the vertical location of the medial cuneiform relative to the first metatarsal was analyzed by defining the first frame as the neutral level. One stance phase for each participant was normalized to 100 frames using normalization software. The overall profile was analyzed based on previous activity phases during the gait cycle. Finally, each stride between heel contact and toe-off was analyzed separately for the three stance phases: early (0–33 frames), middle (34–66 frames), and terminal (67–100 frames)25.
Statistical analysis
Outcomes were confirmed using the Shapiro–Wilk test for normality. Student’s t-test was used to compare quantitative variables. Intra-rater reliability of vertical movement of the first TMT joint during the three stance phases was assessed with intraclass correlation coefficients (ICC1,1). ICC1,1 was regarded as excellent if > 0.74, good if 0.60–0.74, fair if 0.40–0.59, and poor if < 0.40. Additionally, the standard error of the measurements (SEM) was calculated for the US data at each stance phase for sexes to evaluate the accuracy of the measurements. A two-way repeated-measures analysis of variance was used to determine the differences in US values between sexes as a between-subject factor and stance phase as a within-participant factor. When interaction effects were detected, post-hoc comparisons were conducted using the Tukey method to test the differences in movement variables of the first metatarsal and medial cuneiform between females and males. Partial η2 values were used to measure effect size. The post-hoc observed power based on partial η2 was generated using G*Power 3.1 software (Kiel University, Germany). The sample size of 24 feet in the female group and 26 feet in the male group was employed for statistical power analysis. The results of the post-hoc analysis had a large effect size (d = 0.8), an alpha level of p < 0.05, and showed a statistical power of 0.873, indicating adequate power. Statistical significance was set at p < 0.05. Analyses were done using SPSS version 23.0 for Windows (SPSS Inc, Chicago, Illinois, USA).
Results
The participants’ demographics are shown in Table 1. Mean age (p = 0.007), height (p < 0.001), body weight (p < 0.001), and body mass index (BMI) (p = 0.020) were significantly lower in females than in males. No significant differences in HV angle and FPI-6 scores were found between the two groups.
Intra-rater reliability for US vertical movement of the first TMT joint during the stance phase was considered excellent in the location of the metatarsals and medial cuneiform, and good to excellent in the gap of the first metatarsal and medial cuneiform (Table 2).
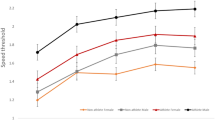
The changes in the ankle angle in dorsiflexion-plantar flexion during stance phase with and without the probe were not significantly different (Supplemental Fig. 1). The first metatarsal gradually displaced in the dorsal direction during the early stance phase and maintained the position during the middle stance. In the late phase, the first metatarsal shifted back in the plantar direction. In addition, a more plantar location was observed in females than in males during the early and middle stance phases (Fig. 3a; p = 0.038, p = 0.042, respectively). The position of the medial cuneiform was stable during the entire stance phase, compared with the first metatarsal, which was located more plantar in females than in males during the middle stance phase (Fig. 3b; p = 0.034). The gap of the vertical location of the first metatarsal and medial cuneiform in females tended to be large during the middle stance, compared with males; however, no statistical differences were identified (Fig. 3c).
Gender differences in first tarsometatarsal joint movement during one stance phase of gait. Temporal changes in the vertical location of the first metatarsal (a), medial cuneiform (b), and displacement of the two (c) are shown for males and females. Box plots comparing the vertical locations during the early, middle, and terminal stance phases are shown. *p < 0.01. Significant plantar displacement was observed in the vertical location of the first metatarsal in early and middle stance and in the vertical location of the medial cuneiform in middle stance in female compared to male.
Participant sex significantly affected the vertical locations of the medial cuneiform during the stance phase (p = 0.025). Gait phase had a significant effect on the first metatarsal, medial cuneiform, and the gap between them (p < 0.001, p = 0.001, p < 0.001, respectively; Table 3).
Discussion
This is the first study to quantify the mobility of first TMT joint in sagittal plane during gait using a synchronized US and MA system. The first metatarsal was located dorsally compared to the medial cuneiform during most of the stance phase, returning to neutral level at toe-off. Mobility of the first metatarsal and medial cuneiform differed in females and males, with the medial cuneiform being stable in males and displaced in the plantar direction in females, especially in the middle stance phase. Our US/MA system captured the vertical location and motion of the first metatarsal and medial cuneiform, allowing the assessment of the first TMT joint dynamics during gait.
The TMT joint is vital in maintaining the lateral and longitudinal stability of the midfoot26. Midfoot stability is associated with ankle, knee, and hip movement during gait27, and hypermobility of the first TMT can lead to collapsing foot arches, which may reduce adaptive abilities during gait. The quantification of the physiological mobility and pathological instability of the first metatarsal and medial cuneiform remains unclear. In this study, we performed a kinematic examination using a novel combination of the US and gait MA during the dynamic rollover phase to further evaluate the detailed biomechanical characteristics of first metatarsal and medial cuneiform during the stance phase.
Significant differences in the movements of the first metatarsal and medial cuneiform during the stance phase were observed between females and males. A study reported that females had more joint mobility of foot and laxity of ligaments supporting the foot arch than males28. The prevalence of HV is greater in females and may be related to differences in footwear, osseous anatomy, and ligamentous laxity2. Recently, the three-dimensional mobility of first ray, including the talonavicular, cuneonavicular, and first TMT joints, was evaluated using weight-bearing computed tomography images13. The first metatarsal showed a mean dorsiflexion angle of 2.0° ± 1.3°, mean inversion angle of 2.6° ± 1.4°, and mean adduction (relative to the medial cuneiform) angle of 1.1° ± 0.7° under loading in middle-aged, healthy volunteers13. These mobility values—determined with patients in static standing postures—were significantly larger in HV patients than in individuals with normal feet. This study evaluated the mobility of the first TMT joint in dynamic postures and indicated that the medial cuneiform is displaced in the plantar direction during the middle stance phase in healthy females. This finding suggests more laxity of the naviculocuneiform or intercuneiform 1–2 joints. A cadaveric study demonstrated that the naviculocuneiform, first TMT, and talonavicular joints contributed an average of 50%, 41%, and 9%, respectively, to the total first-ray sagittal plane range of motion29. The three-dimensional analysis using weight-bearing computed tomography images revealed greater mobility of the intercuneiform 1–2 joints in individuals with HV than in those with normal feet. A significant increase in dorsiflexion and inversion displacement of the intermediate cuneiform relative to the medial cuneiform has been reported30. Plantar displacement of the medial cuneiform in the stance phase might be induced by the hypermobility of the naviculocuneiform, intercuneiform 1–2 joint. These dynamics can lead to subsequent hypermobility of the first TMT joint, and long-term progression of HV and its higher prevalence among females. Thus, future studies investigating the relationship between the first-ray mobility and onset of HV in healthy participants are warranted. Our results can help improve the prognoses and quality of treatment for patients with foot deformities, including HV. It may also aid in developing a new evaluation method for the early detection of abnormalities in the first TMT joint or improving the progression of early-stage foot deformities.
This study has several limitations. First, the participants in this study were younger than the general age group in which foot deformities are observed. Second, our US measurements only observed the vertical mobility of the first TMT joint during gait. Future research should address the multi-directional analysis of the foot joint, and technological progress is essential to resolve this issue. Finally, the mobility of the naviculocuneiform joint could not be evaluated, as probe positioning would interfere with ankle joint movement during gait. The attachment of a reflective marker on the second metatarsal head and the US probe to the foot was not believed to have affected ankle joint movement during gait, as there was no significant difference in the ankle joint during gait with and without attachment of US probe (Supplemental Fig. 1). Moreover, we may use a cast system to avoid the probe movement; however, it would likely inhibit foot or ankle joint movement. Therefore, the US/MA system is appropriate for quantitatively measuring first TMT joint mobility.
In conclusion, mobility of the first TMT joint in the sagittal plane during the stance phase was quantified using a synchronized US/MA system. The medial cuneiform is displaced in plantar direction during middle stance phase in healthy females without foot disorders than in males. This US/MA system can be used to investigate the pathogenesis of foot disorders, such as the hallux valgus, in future studies.
Data availability
The datasets for this study are available upon request from the corresponding author.
References
Nix, S., Smith, M. & Vicenzino, B. Prevalence of hallux valgus in the general population: A systematic review and meta-analysis. J. Foot Ankle Res. 3, 21. https://doi.org/10.1186/1757-1146-3-21 (2010).
Perera, A. M., Mason, L. & Stephens, M. M. The pathogenesis of hallux valgus. J. Bone Joint Surg. Am. 93, 1650–1661. https://doi.org/10.2106/JBJS.H.01630 (2011).
Glasoe, W. M., Nuckley, D. J. & Ludewig, P. M. Hallux valgus and the first metatarsal arch segment: A theoretical biomechanical perspective. Phys. Ther. 90, 110–120. https://doi.org/10.2522/ptj.20080298 (2010).
Faber, F. W., Kleinrensink, G. J., Mulder, P. G. & Verhaar, J. A. Mobility of the first tarsometatarsal joint in hallux valgus patients: A radiographic analysis. Foot Ankle Int. 22, 965–969. https://doi.org/10.1177/107110070102201207 (2001).
Ellington, J. K., Myerson, M. S., Coetzee, J. C. & Stone, R. M. The use of the Lapidus procedure for recurrent hallux valgus. Foot Ankle Int. 32, 674–680. https://doi.org/10.3113/FAI.2011.0674 (2011).
Allen, M. K. et al. Relationship between static mobility of the first ray and first ray, midfoot, and hindfoot motion during gait. Foot Ankle Int. 25, 391–396. https://doi.org/10.1177/107110070402500605 (2004).
Glasoe, W. M. & Coughlin, M. J. A critical analysis of Dudley Morton’s concept of disordered foot function. J. Foot Ankle Surg. 45, 147–155. https://doi.org/10.1053/j.jfas.2006.02.008 (2006).
Van Beek, C. & Greisberg, J. Mobility of the first ray: Review article. Foot Ankle Int. 32, 917–922. https://doi.org/10.3113/FAI.2011.0917 (2011).
Shibuya, N., Roukis, T. S. & Jupiter, D. C. Mobility of the first ray in patients with or without hallux valgus deformity: Systematic review and meta-analysis. J. Foot Ankle Surg. 56, 1070–1075. https://doi.org/10.1053/j.jfas.2017.05.021 (2017).
Greisberg, J., Sperber, L. & Prince, D. E. Mobility of the first ray in various foot disorders. Foot Ankle Int. 33, 44–49. https://doi.org/10.3113/FAI.2012.0044 (2012).
Klaue, K., Hansen, S. T. & Masquelet, A. C. Clinical, quantitative assessment of first tarsometatarsal mobility in the sagittal plane and its relation to hallux valgus deformity. Foot Ankle Int. 15, 9–13. https://doi.org/10.1177/107110079401500103 (1994).
King, D. M. & Toolan, B. C. Associated deformities and hypermobility in hallux valgus: An investigation with weightbearing radiographs. Foot Ankle Int. 25, 251–255. https://doi.org/10.1177/107110070402500410 (2004).
Kimura, T. et al. Evaluation of first-ray mobility in patients with hallux valgus using weight-bearing CT and a 3-D analysis system: A comparison with normal feet. J. Bone Joint Surg. Am. 99, 247–255. https://doi.org/10.2106/JBJS.16.00542 (2017).
Cornwall, M. W. et al. The influence of first ray mobility on forefoot plantar pressure and hindfoot kinematics during walking. Foot Ankle Int. 27, 539–547. https://doi.org/10.1177/107110070602700710 (2006).
Coughlin, M. J. & Jones, C. P. Hallux valgus and first ray mobility: A prospective study. J. Bone Joint Surg. Am. 89, 1887–1898. https://doi.org/10.2106/JBJS.F.01139 (2007).
Martin, H. et al. Investigation of first ray mobility during gait by kinematic fluoroscopic imaging-a novel method. BMC Musculoskelet. Disord. 13, 14. https://doi.org/10.1186/1471-2474-13-14 (2012).
Lundgren, P. et al. Invasive in vivo measurement of rear-, mid-, and forefoot motion during walking. Gait Posture 28, 93–100 (2008).
Ferrari, J., Hopkinson, D. A. & Linney, A. D. Size and shape differences between male and female foot bones: Is the female foot predisposed to hallux abducto valgus deformity?. J. Am. Podiatr. Med. Assoc. 94, 434–452. https://doi.org/10.7547/0940434 (2004).
Redmond, A. C., Crosbie, J. & Ouvrier, R. A. Development and validation of a novel rating system for scoring standing foot posture: The Foot Posture Index. Clin. Biomech. 21, 89–98. https://doi.org/10.1016/j.clinbiomech.2005.08.002 (2006).
Shibuya, H. et al. New screening method for hallux valgus with using smartphone. Foot Ankle Orthop. https://doi.org/10.1177/2473011418S00242 (2018).
Rosa, L. G., Zia, J. S., Inan, O. T. & Sawicki, G. S. Machine learning to extract muscle fascicle length changes from dynamic ultrasound images in real-time. PLoS ONE 16, e0246611. https://doi.org/10.1371/journal.pone.0246611 (2021).
Telfer, S., Woodburn, J. & Turner, D. E. An ultrasound based non-invasive method for the measurement of intrinsic foot kinematics during gait. J. Biomech. 47, 1225–1228. https://doi.org/10.1016/j.jbiomech.2013.12.014 (2014).
Ishii, Y. et al. Dynamic ultrasonography of the medial meniscus during walking in knee osteoarthritis. Knee 27, 1256–1262. https://doi.org/10.1016/j.knee.2020.05.017 (2020).
Brown, D. & Cox, A. J. Innovative uses of video analysis. Phys. Teach. 47, 145–150. https://doi.org/10.1119/1.3081296 (2009).
Kim, E. J. et al. Inter-segmental foot kinematics during gait in elderly females according to the severity of hallux valgus. J. Orthop. Res. 38, 2409–2418. https://doi.org/10.1002/jor.24657 (2020).
Sripanich, Y. et al. Anatomy and biomechanics of the lisfranc ligamentous complex: A systematic literature review. J. Biomech. 119, 110287. https://doi.org/10.1016/j.jbiomech.2021.110287 (2021).
Cardoso, T. B. et al. Hip external rotation stiffness and midfoot passive mechanical resistance are associated with lower limb movement in the frontal and transverse planes during gait. Gait Posture 76, 305–310. https://doi.org/10.1016/j.gaitpost.2019.12.030 (2020).
Nagano, K., Okuyama, R., Taniguchi, N. & Yoshida, T. Gender difference in factors affecting the medial longitudinal arch height of the foot in healthy young adults. J. Phys. Ther. Sci. 30, 675–679. https://doi.org/10.1589/jpts.30.675 (2018).
Roling, B. A., Christensen, J. C. & Johnson, C. H. Biomechanics of the first ray. Part IV: The effect of selected medial column arthrodeses: A three-dimensional kinematic analysis in a cadaver model. J. Foot Ankle Surg. 41, 278–285. https://doi.org/10.1016/s1067-2516(02)80045-x (2002).
Kimura, T., Kubota, M., Suzuki, N., Hattori, A. & Marumo, K. Comparison of intercuneiform 1–2 joint mobility between hallux valgus and normal feet using weightbearing computed tomography and 3-dimensional analysis. Foot Ankle Int. 39, 355–360. https://doi.org/10.1177/1071100717744174 (2018).
Acknowledgements
We would like to thank the participants in this study, as well as Editage for English language editing.
Author information
Authors and Affiliations
Contributions
N.M. and Y.I.: Investigation, Resources, Writing original draft, Writing review & editing. T.T. and S.A.: Software, Visualization, Formal analysis. M.M.: Data curation, K.K. and H.I.: Formal analysis. T.N. and N.A.: Investigation, Resources, Writing original draft, Writing review & editing, Methodology. A.B. and Y.U.: Formal analysis, Data curation.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Maeda, N., Ikuta, Y., Tashiro, T. et al. Quantitative evaluation of the vertical mobility of the first tarsometatarsal joint during stance phase of gait. Sci Rep 12, 9246 (2022). https://doi.org/10.1038/s41598-022-13425-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-13425-5
This article is cited by
-
First tarsometatarsal joint mobility in hallux valgus during gait: A synchronized ultrasound and three-dimensional motion capture analysis
Journal of Medical Ultrasonics (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.